Rheumatology key message
The clinician needs to consider the overlapping pathophysiological mechanisms of SLE, APS and coronavirus disease 2019.
Dear Editor, The multiorgan and systemic manifestations of coronavirus disease 2019 (COVID-19) share features in common with SLE and APS. They are all associated with complement activation and microvascular injury, which can cause gastrointestinal symptoms creating a diagnostic challenge for the clinician. The severe acute respiratory distress syndrome coronavirus 2 (SARS-CoV-2) was identified in Wuhan, China as the aetiologic agent of a novel respiratory illness [1]. In addition to acute respiratory failure, extrapulmonary manifestations include haematologic abnormalities resulting in systemic coagulopathy manifest as pulmonary embolisms, deep vein thrombosis, microvascular injury and gastrointestinal abnormalities [1–3]. Histopathologic studies have shown microvascular injury in the heart, lungs, skin, kidney and small bowel [2, 4]. There is evidence this is in part driven by lectin pathway complement activation, with reports of deposition of C5b-9, C4d and mannose-binding lectin serine protease 2 (MASP2) in the microvasculature, which can produce a catastrophic microvascular injury syndrome [4]. Additionally, there are reports of aPL occurring in COVID-19 patients [5].
SLE is an autoimmune disease, characterized by immune dysregulation resulting in activation of the innate immune system with increased type 1 IFN, production of autoantibodies, generation of circulating immune complexes and episodic activation of the complement system. Lupus enteritis is a rare manifestation characterized clinically by abdominal pain, diarrhoea and vomiting, and radiographically by bowel wall oedema [6]. A subset of SLE patients develop aPL and are at risk for thrombotic events [7]. The occurrence of small-vessel occlusion is uncommon, but is a well-documented APS phenomenon that can occur in skin, liver, kidney and bowel [6, 7].
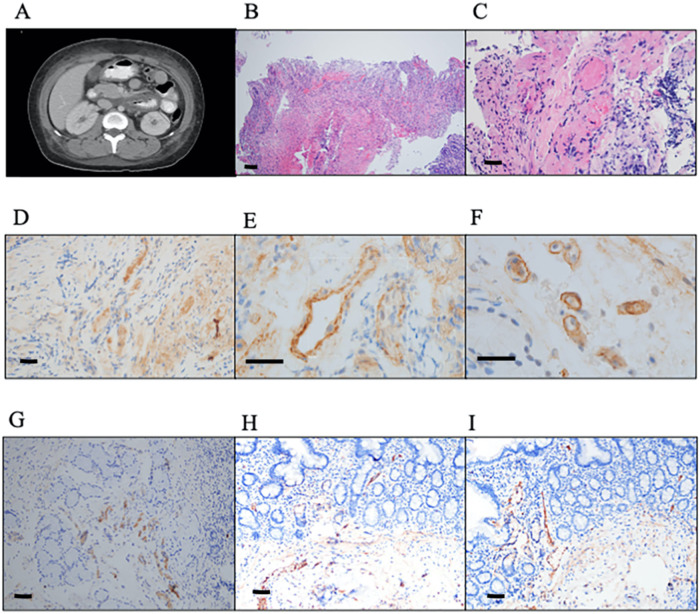
We report a case of a 27-year-old woman presenting with acute onset nausea, vomiting and non-bloody diarrhoea. Four years prior to admission she was diagnosed with SLE after developing immune thrombocytopenic purpura. Her SLE manifestations include malar rash, arthritis, ANA, anti-dsDNA, anti-Ro, persistently low C3 and C4, and a positive LA, which on subsequent testing was negative along with absent aCL and beta 2 glycoprotein antibodies. At physical exam on hospital day 1, she was afebrile, normotensive, with a heart rate 97 b.p.m., oxygenating 98%, with clear lungs, a diffusely tender abdomen without rebound and skin without rash. A nasopharyngeal swab analysed by PCR confirmed SARS-CoV-2 infection. Laboratory tests revealed C3 and C4 at her usual baseline levels at 74 and 4 mg/dl, respectively, and anti-dsDNA antibody of 161 IU/ml, slightly elevated compared with baseline. Her D-dimer increased from 2872 ng/ml on day 1 to 5446 ng/ml on day 3. aPL testing revealed newly present aCL IgG and IgM at 24.2 GPL and 21.4 MPL, respectively. CT of her abdomen showed diffuse small bowel oedema (Fig. 1A). On day 2, biopsies obtained during esophagogastroduodenoscopy revealed platelet/fibrin-rich thrombi in the microvasculature of her duodenal lamina propria and submucosa associated with ischaemic mucosal necrosis (Fig. 1B and C). The patient was treated with enoxaparin with concurrent decrease in her D-dimer level and resolution of her abdominal pain, diarrhoea and anorexia. Apixaban was initiated on hospital discharge.
Fig. 1.
Radiographic and histology findings
(A) CT abdomen with oedema of the small bowel wall. (B) Mucosal necrosis with microvascular thrombi and fibrin extravasation in lamina propria, consistent with thrombogenic vasculopathy (haematoxylin and eosin). (C) Occlusive luminal thrombi and mural fibrin (haematoxylin and eosin). (D–I) In situ deposition of components of complement activation, namely C3d, C4d, C5b-9 and MASP2, the latter a protein formed as a sequelae of the mannose-lectin binding activation were conducted on 4-μm sections procured from formalin-fixed paraffin-embedded tissue. Immunohistochemical assessment of SARS-CoV-2-associated envelope and spike glycoprotein was also conducted, as previously described [4]. (D) MASP2 staining, (E) C4d staining in thrombosed and (F) non-thrombosed capillaries and venules (diaminobenzidine), and (G) C5b-9 staining of (H) SARS-CoV-2 membrane and (I) spike glycoprotein throughout the microvasculature ( diaminobenzidine). MASP2: mannose-binding lectin serine protease 2 SARS-CoV-2: severe acute respiratory distress syndrome coronavirus 2. Scale bar = 100 μm.
Histopathological analysis demonstrated a pauci-inflammatory thrombogenic vasculopathy with marked endothelial cell injury. The case differed from conventional small vessel lymphocytic or neutrophil-rich vasculitis of SLE due to lack of vasocentric inflammation (Fig. 1B and C). There was minimal endothelial staining for myxovirus resistance protein Apointing to lack of type I IFN activity, consistent with inactive SLE. Markers of mannose-binding lectin complement activation were demonstrated by extensive staining of capillaries and venules for MASP2 (Fig. 1D), C3d, C4d (Fig. 1E and F) and C5b-9 (Fig. 1G) present in thrombosed and non-thrombosed vessels, indicative of systemic complement activation. The endothelial complement staining pattern mirrored staining of SARS-CoV-2 membrane and spike glycoprotein expression (Fig. 1H and I).
While the majority of thrombotic occlusion in COVID-19 has been documented in the pulmonary vasculature, its occurrence in extrapulmonary organs including the skin and gastrointestinal tract has also been reported [1, 3, 4, 8]. A case series described severe small bowel ischaemia caused by multifocal microthrombi and mesenteric and portal vein thrombosis in three patients with COVID-19 presenting with acute abdomen [3].
On the other hand, lupus mesenteric vasculopathy can be broadly categorized as thrombotic or as inflammatory. Vasculitic patterns include a neutrophil-rich leukocytoclastic vasculitis attributable to an Arthus type III immune complex reaction, a lymphocytic vasculitis attributable to antibody targeting endothelium in concert with enhanced IFN expression, or as a result of C5a-mediated neutrophil endothelial cell homo- and heterotypic leukoaggregation [7]. Alternatively, the thrombotic patterns are typically linked to APS [7].
The myriad pathogenetic mechanisms responsible for the development of small intestinal microvascular thrombosis in an individual with newly diagnosed COVID-19 and longstanding SLE are complex, overlapping and largely inextricable. The absence of aPL titres >40 units conferring thrombogenic potential, SLE serological activity, myxovirus resistance protein A staining to suggest a role for type 1 IFN stimulated genes, and resolution of symptoms without steroids or immunomodulation argue against SLE exacerbation. Moreover, SARS-CoV-2 spike glycoprotein endothelial localization and activation of the lectin complement pathway generating C5a and C5b-9 can explain the observed enteric thrombotic vasculopathy. The localization of these viral proteins to endothelium demonstrate a critical trigger to the mannose-binding lectin pathway of complement activation. Finally, the pattern of MASP2 and SARS-CoV-2 endothelial staining mirrors that found in other cases of COVID-19-associated vascular thrombosis in which there were no complicating aPL [1, 5], suggesting the patient’s aPL were an epiphenomenon.
We report the first case of an SLE patient with COVID-19 infection and histological evidence of complement activation. Although the occurrence of COVID-19 infection in a well-established SLE patient is a coincidence, the development of symptomatic enteritis accompanied by thrombotic vasculopathy with histological evidence for lectin pathway complement activation mirroring viral protein deposition, and the presence of aPL, requires the clinician to consider the overlapping pathophysiological mechanisms of SLE, APS and COVID-19, which are important given their unique clinical courses and treatment.
Funding: No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this manuscript.
Disclosure statement: The authors have declared no conflicts of interest.
Data availability statement
All authors had access to the data and a role in writing the manuscript. The patient’s consent was obtained for publication.
Contributor Information
Rochelle Castillo, Department of Rheumatology.
Jonathan Melamed, Department of Pathology, New York University Langone Health.
Cynthia Magro, Department of Pathology and Laboratory Medicine, Weill Cornell Medicine, New York, NY, USA.
Pamela Rosenthal, Department of Rheumatology.
H Michael Belmont, Department of Rheumatology.
References
- 1. Guan W, Ni Z, Hu Y. et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gavriilaki E, Brodsky RA. Severe COVID‐19 infection and thrombotic microangiopathy: success does not come easily. Br J Haematol 2020;189:e227–30. [DOI] [PubMed] [Google Scholar]
- 3. Ignat M, Philouze G, Aussenac-Belle L. et al. Small bowel ischemia and SARS-CoV-2 infection: an underdiagnosed distinct clinical entity. Surgery 2020;168:14–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Magro C, Mulvey JJ, Berlin D. et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res 2020;220:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhang Y, Xiao M, Zhang S. et al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med 2020;382:e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kishimoto M, Nasir A, Mor A, Belmont H. Acute gastrointestinal distress syndrome in patients with systemic lupus erythematosus. Lupus 2007;16:137–41. [DOI] [PubMed] [Google Scholar]
- 7. Belmont HM, Abramson SB, Lie JT. Pathology and pathogenesis of vascular injury in systemic lupus erythematosus. Interactions of inflammatory cells and activated endothelium. Arthritis Rheum 1996;39:9–22. [DOI] [PubMed] [Google Scholar]
- 8. Mao R, Qiu Y, He J-S. et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2020;5:667–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All authors had access to the data and a role in writing the manuscript. The patient’s consent was obtained for publication.