Abstract
Objective:
Exposure to a traumatic event is common among US adults, yet only a small fraction develops post-traumatic stress disorder (PTSD). Higher pain after a traumatic injury has been associated with higher PTSD symptomology and thus may be a risk factor. However, few studies have examined how pain during the period immediately after a trauma, referred to as the acute post trauma period, relates to later to PTSD outcomes.
Methods:
A sample of (n = 87) individuals who had experienced a traumatic injury assessed their pain through daily mobile assessments for the first month after injury. PTSD, depression, and functional impairment were assessed at time of trauma and 1, and 3 months later.
Results:
Using latent class growth analysis (LCGA), three trajectories of pain were identified: low pain (41.3%), decreasing pain (43.7%), and high pain (14.9%). At baseline, the high pain class reported higher levels of depression and functional impairment than the low pain group. From baseline to 3 months, the low pain class experienced a reduction in PTSD, depression, and functional impairment whereas the high pain class experienced an increase in PTSD symptoms, and persistent depression, and functional impairment.
Conclusions:
These results demonstrate that there are distinct trajectories of pain after a traumatic injury. Persistent elevated pain is associated with more severe psychopathology in the period immediately following a traumatic injury.
Keywords: pain, traumatic injury, post-traumatic stress disorder, trajectories
The overwhelming majority of adults (89.7%) in the US will experience a traumatic event in their lifetime (1). A significant portion (8.3%) will develop posttraumatic stress disorder (PTSD) (1). PTSD is associated with several negative outcomes—including an inability to work, impaired social relationships, dependence on others, and the onset of comorbid conditions (2). Thus, preventing PTSD is of great public health importance. An important first step in understanding how to prevent PTSD is to identify the factors that contribute to its development. One such factor that is posited to be highly relevant is pain (3,4).
Prior work has shown pain at the time of a trauma is related to PTSD symptoms in both adults and children (5–7). Elevated pain within the weeks after a traumatic injury was associated with greater posttraumatic stress symptoms at 6 months (6). Additionally, elevated pain 24 to 48 hours after a traumatic injury increased the odds of developing PTSD four months later by more than fivefold and eight months later by almost sevenfold (7). Similarly, pain intensity at hospital discharge was significantly correlated with depressive and PTSD symptoms one year after a traumatic injury (5). Therefore, the experience of pain in the aftermath of the trauma is associated with subsequent symptoms of psychopathology.
The mutual maintenance model explains the high comorbidity between pain and PTSD (8–11). This model proposes that PTSD and chronic pain contribute to and are the result of several common factors including attentional biases toward experiencing pain or trauma, anxiety sensitivity, pain as a reminder of trauma, avoidant coping, depression, elevated anxiety, and catastrophizing (10). Prior work has supported this model as well. In a sample of veterans in rehabilitation for a spinal cord injury, 31% had both PTSD and pain, while 25% had pain without PTSD and 14% had PTSD without pain (11). In a study of patients after a traumatic injury, higher levels of pain at one week after trauma predicted higher arousal symptoms at 3 months, and elevated arousal at 3 months predicted higher pain at 12 months. Further, higher pain at 3 months was associated with higher re-experiencing, arousal and avoidance symptoms at 12 months (9). Therefore, pain and PTSD affect each other’s development over time.
The majority of the work on the association between pain and mental health outcomes after a trauma has focused on a single measurement of pain. Although pain is often present after an injury, its intensity varies during this period (12,13). These variations may be important in determining the onset and severity of subsequent mental health outcomes. Those who experience elevated pain for weeks after a trauma may be at greater risk for maladaptive outcomes such as PTSD, comorbid mental health conditions such as depression, and the functional impairment associated with these conditions than those whose pain quickly declines after the trauma (5,7,14,15). Examining pain longitudinally also determines how pain resolution may be associated with such outcomes. For example, a study that administered daily pain assessments to a sample of patients the first week after discharge from the emergency room identified two different trajectories of pain (12). Almost 80% of patients showed a negative slope, or pain reduction, while about 20% of patients had constant or worsening pain. The association between pain resolution after a trauma and mental health outcome has not yet been thoroughly examined.
Only one prior study has examined the trajectory of pain after an injury as it relates to mental health outcomes. In a sample that experienced a mild traumatic brain injury (mTBI), trajectories of headache pain were examined (16). Four trajectories throughout the first year after injury were identified: Chronic, Worsening, Improving, and Resolved. None of the individuals in the resolved and improving pain trajectories developed PTSD at 1 year. However, a substantial portion of the chronic (25%) and of the worsening (7%) groups met criteria for PTSD at 1-year follow-up (16). These results suggest that low and resolving pain after a traumatic injury may lead to better outcomes and higher pain trajectories may lead to higher PTSD symptomology. This study focused exclusively on headache pain following a mTBI, which may not generalize to the relationship between pain trajectories from other injuries and mental health outcomes. It is possible that concussion resulting from an mTBI could contribute to PTSD (17). Furthermore, this study examined pain trajectories during a 12-month period, and only assessed pain at baseline, 3, 6 and 12 months, which does not capture trajectories shortly after the trauma. Specifically, the experience of pain can be highly variable within the immediate aftermath of a traumatic event. Identifying different pain trajectories during this acute period may prove useful in understanding the association between pain and later mental health and functional outcomes.
Depression is highly comorbid with PTSD such that these conditions may be develop together after a trauma. However, the association between pain and depression has received less attention in the literature than that between pain and PTSD. Results are mixed with the majority of evidence suggesting that pain may not be associated with subsequent depression and that depression may predict subsequent pain. In a large sample of individuals with chronic pain, depression was associated with pain and pain-related disability over time (18). However, pain was not associated with depression over time. Related work has suggested that significantly elevated depressive symptoms were associated with modest increases in knee pain over time, but reverse relation was not observed (19). However, another study in a sample of individuals being treated for chronic back, hip, and knee pain found evidence for a reciprocal relation over a 1 year period (20). Taken together, it is unclear how depression and pain are related and how this relation may manifest in the period of time immediately after a trauma.
Furthermore, there is a complex relationship between pain, depression, PTSD and functional impairment after a traumatic injury. In one study, pain and depression explained the relationship between post-traumatic stress symptoms and functional impairment 12 months after an injury (14). Additionally, chronic pain significantly contributed to functional impairment, and both pain and depression contributed to functional impairment one year after a traumatic injury (2,18,21). Thus, the relationship between pain in the first month after a trauma and functional impairment warrants further investigation.
The aim of the present study was to identify the trajectories of pain within the first month after a traumatic injury. The secondary goal was to determine how they relate to PTSD symptoms, depression symptoms, and functional impairment at 1 month and 3 months. It was hypothesized that three classes of pain would be identified: constant low level of pain, initial moderate and decreasing pain, and constant chronic pain. It was hypothesized that a worsening group would not be identified due to the limited assessment period and the presence of acute pain after the traumatic event. Furthermore, persistent elevated pain was hypothesized to be associated with greater PTSD, depression, and functional impairment whereas persistent low level and decreasing rate of pain was hypothesized to be associated with less PTSD, depression, and functional impairment.
Methods
Participants
Participants were 87 individuals who presented at a large northeastern acute and critical care service that experienced a traumatic injury (Table 1). Traumatic injury was defined as an injury that met criterion A for a diagnosis of PTSD. Participants had a mean age of 35.02 years (SD = 10.52). The majority of participants were male (62.5%) and self-identified as White (88.6%), 4.5% self-identified as African-American, 1.1% as Asian American, 1.1% as Pacific Islander, 2.3% as American Indian, and 2.3% as Biracial. The majority of the sample earn a household income below $50,000 (52.4%). The most common injury was from a motor vehicle crash (48.3%). The remaining types of injuries were fall from work related injury (23.0%), recreational accident (12.6%), burn (8.0%), crush injury (2.3%), assault (1.1%), and other trauma not specified (4.6%).
Table 1.
Descriptive information for each class.
| Low Pain | Decreasing Pain | High Pain | Overall | |
|---|---|---|---|---|
| Age | 34.11 (11.41) | 37.03 (10.12) | 30.85 (8.10) | 34.91 (10.53) |
| Female Sex | 12 (33.3) | 15 (39.5) | 6 (46.2) | 33 (37.9) |
| Income below $50,000 | 17 (47.2) | 20 (52.6) | 11 (84.6) | 48 (55.2) |
| White Race | 33 (91.67) | 32 (84.2) | 12 (92.3) | 77 (88.5) |
| Private Insurance | 22 (61.1) | 19 (50.0) | 6 (46.2) | 47 (54.0) |
| MVC | 17 (47.2) | 22 (57.9) | 6 (46.2) | 45 (51.7) |
| ISS Score | 17.18 (11.1) | 12.34 (10.21) | 13.8 (9.91) | 3.98 (10.46) |
Note: MVC = Motor Vehicle Crash. ISS = Injury Severity Score.
Measures
Standardized Trauma Interview (STI) (23).
The STI is a 41-item interview administered by trained research assistants, which assesses details of a participant’s traumatic experience. The STI was used in the present study to assess if participants’ traumatic experience met Criterion A.
Numeric Pain Rating Scale:
The Numeric Pain Rating Scale is a tool used to measure one’s level of pain. The scale ranges from 0 (no pain) to 10 (worst pain imaginable). For the purpose of this study, the measure was used to assess past day pain. This measure is widely used and has been tested against others to show validity (23).
PTSD Checklist for DSM-5 (PCL-5) (24):
The PCL-5 is a 20-item self-report measure that assesses PTSD symptoms according to DSM 5 criteria experienced over the last month. Responses were anchored to the current trauma. It assesses symptoms across 4 symptom clusters of PTSD (re-experiencing, negative mood, avoidance, and hyperarousal) on a 0-4 point Likert scale. Total scores range from 0-80. PCL-5 scores assessed at 1 month had an internal consistency of α = 0.94 and scores at 3 months had an internal consistency of α= 0.95.
Patient Health Questionnaire-8 (PHQ-8) (25):
The PHQ-8 is an 8-item self-report measure that assesses depression symptoms experienced in the last two weeks. Responses were anchored to the current trauma. Ratings are made on a 0-3 point scale with regards to the frequency with which a symptom has been experienced. Scores range from 0-24, with higher scores indicating more severe depression. The PHQ-8 is adapted from the PHQ-9 and is identical except for the removal of an item on suicidal ideation. The internal consistency was α =0.88 for scores assessed at 1 month and α = 0.91 for scores assessed at 3 months.
Sheehan Disability Score (SDS) (26):
The SDS was developed as a global measure of the impact of mental illness on functioning. Responses were anchored to the current trauma. The SDS is a composite of three self-rated, 10-point Likert scale response items that aim to assess the level of the subjects’ impairment with regard to their work/school activities, family relationships, and social functioning over the past month. The internal consistency was α= 0.86 for scores assessed at 1 month and α = 0.86 for scores assessed at 3 months.
Procedure
This study was part of a larger study on the use of mobile applications to assess symptoms after trauma (28). Participants were recruited from the ED at a level 1 Trauma Center by a trained research assistant. Participants were included if they had experienced a trauma that met criterion A for a diagnosis of PTSD, which involved actual or threatened death, physical injury, or sexual violence (28). Electronic medical records (EMR) for the patient’s ED visit were reviewed by trained research assistants to determine if the individual experienced a criterion A event. Exclusion criteria included severe traumatic brain injury (TBI) and moderate TBI. Participants provided consent for inclusion in the study. Participants completed a battery of assessments and downloaded and installed a mobile application—Metricwire (Ontario, Canada)—on their mobile device. Every day for 30 days, participants received a notification to complete a mobile assessment of their current symptoms which included the Numeric Pain Rating Scale. Notifications were sent out between 7 PM and 8 PM, and participants were allowed to respond within that day. Participants then completed assessments of their PTSD, depression, and functional impairment at 1-month and 3 months post injury. Additional information about the current study is available is available elsewhere (29). Data collection occurred from 5/2015 to 5/2017. The Institutional Review Board of the University of Vermont approved all study procedures.
Data Analyses
Daily reports of pain symptoms were used to generate trajectories of pain in the acute post trauma period. The pain data was extracted from Metricwire and assessment dates were standardized to days after trauma. The pain scores were averaged across four-day periods to account for missing responses. The overall response rate was 61.1% and by aggregating across 4 days, a large majority of the sample (75.6%) were represented in each time point. This is a common practice in such studies (30). For these analyses, days of 5 to 40 post trauma were selected.
Latent class growth analysis (LCGA)—a type of growth mixture modeling which has shown to be an effective method to determine unknown classes of trajectories in prior psychological studies (32)—was used to identify classes of pain trajectories. First, a traditional growth curve (latent growth curve modeling or LGCM) was estimated. Goodness-of-fit was evaluated using the following fit statistics: the Bayesian, sample-size adjusted Bayesian and Aikaike information criterion (IC) indices; the root mean square error of approximation (RMSEA), the comparative fit index (CFI) and Tucker-Lewis index (TLI), and the standardized root mean residual (SRMR) (32). Next, latent class growth analysis (LCGA) was performed. Consistent with model recommendations, the hypothesized number of classes was tested in addition to one less and one more than expected: two, three and four class models were evaluated (32). In order to determine the appropriate model fit, the Bayesian, sample-size adjusted Bayesian and Aikaike information criterion (IC) indices, entropy values, the Vuong-Lo-Mendell Rubin (VLMR), the Bootstrapped Likelihood Ratio Test (BLRT), the Lo-Mendell-Rubin Likelihood Ratio Test (LMR-LRT) were compared. Analyses were conducted in Mplus (33).
Class membership was then used as a categorical variable to determine the extent that influenced change in PTSD, depression, and functional impairment in the three-month period since the trauma. These results were analyzed using a mixed effect model in which there were fixed effects for intercept, slope, class membership, and a slope x class membership interaction. Of interest was the significance of the effects for class membership and the interaction term. A random effect for intercept was included.
Results
The model fit indices suggested that a LGCM was not a good fit: χ2(df) = 103.150(40) p < 0.001; RMSEA = 0.135, 90% CI (0.103 – 0.167), CFI/TLI = 0.933/0.930, SRMR = 0.117. LCGA was performed for 2 through 4 class models (Table 2). The optimal model included 3-classes. The information criteria (AIC, BIC and SSABIC) for the 3-class model was lower than the 2 class but higher than the 4 class. Entropy was 0.928. The Likelihood-Ratio Tests were all statistically significant for the 3-class model with p values below 0.001. Figure 1 shows the optimal 3-class model for pain trajectories in the first month after trauma. The intercept (i) and slope (s) of each predicted class are as follows: low pain (i = 2.694; s = −0.249), decreasing pain (i = 6.108; s = −0.352), and persistent high pain (i = 8.400; s = −0.052).
Table 2.
Fit indices for 2, 3 and 4 class latent class growth analyses (LCGA).
| Fit Indices | 2 Class (n = 87) |
3 Class (n = 87) |
4 Class (n = 87) |
|---|---|---|---|
| Class Proportions | 52.9% | 14.9% | 17.2% |
| 47.1% | 41.4% | 34.7% | |
| -- | 43.7% | 16.4% | |
| -- | -- | 31.8% | |
| AIC | 2252.804 | 1965.588 | 1901.754 |
| BIC | 2287.327 | 2007.509 | 1951.072 |
| SSABIC | 2243.152 | 1953.868 | 1887.966 |
| Entropy | 0.918 | 0.928 | 0.882 |
| VLMR LRT | 0.0938 | 0.0004 | 0.1998 |
| p value | |||
| LMR LRT p value | 0.1056 | 0.0007 | 0.2226 |
| Bootstrap LRT p value | 0.000 | 0.0000 | 0.0000 |
Note. AIC: Aikaike Information Criteria, BIC: Bayesian Information Criteria, SSABIC: sample-size adjusted Bayesian Information Criteria; VLMR LRT: Vuong-Lo-Mendell Rubin Likelihood Ratio Test; LMR LRT: Lo-Mendell-Rubin Likelihood Ratio Test; Bootstrap Likelihood Ratio Test
Figure 1.
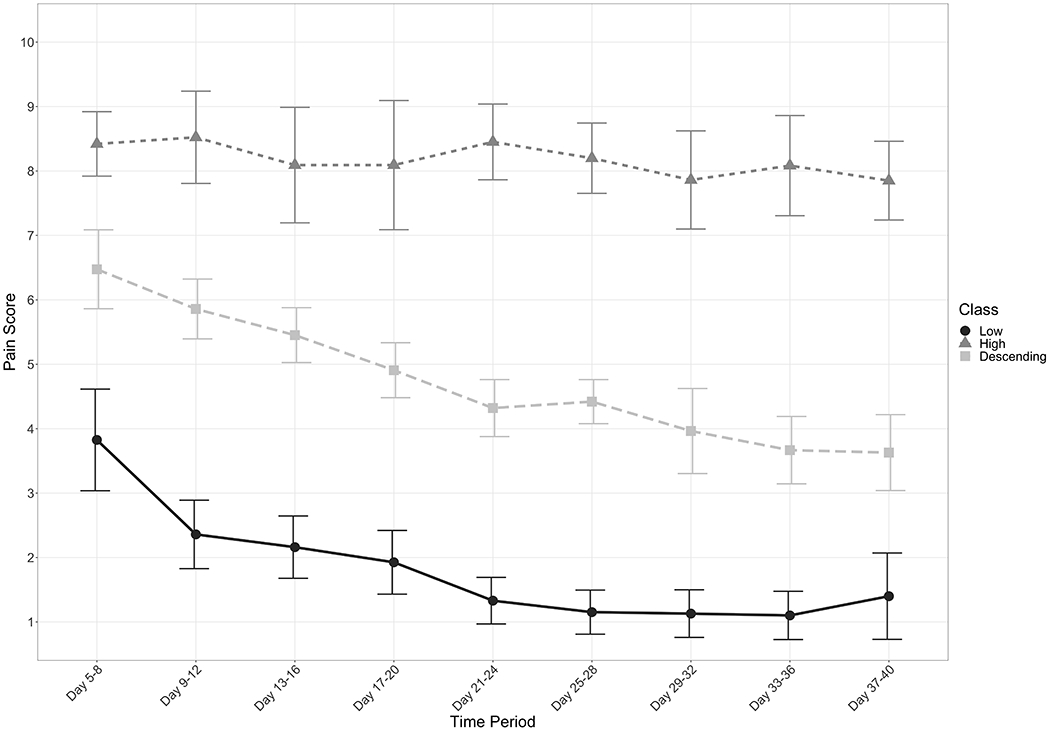
Latent class growth analysis pain trajectories across the acute post-trauma period.
The extent that Pain Class membership was associated with PTSD, depression, and functional impairment were then evaluated using mixed effect models (Table 3). The Low Pain class was used as the reference group. There were no differences the classes across demographic characteristics (p’s > .167). For PTSD, there was a significant negative slope (b = −4.27, SE = 1.04, p < .001), which suggested that there was a significant decrease in PTSD for the Low Pain Class. The interaction between slope and the High Pain Class was significant (b = 4.70, SE = 2.34, p = 0.046), suggesting that those in this class had PTSD symptoms that remained relatively stable over the three-month period post trauma. There was no significant fixed effect or interaction effect for time and Decreasing Class membership (p’s > .130). These findings suggest that the High Pain Class saw an increase in PTSD symptoms whereas the Low and Decreasing Classes experienced a decrease in such symptoms.
Table 3.
Descriptive Statistics on PTSD, Depression, and Functional Impairment at Time of Trauma, 1-month, and 3-month Follow-Up.
| High (H) | Decreasing (D) | Low (L) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | Cohen’s D (High - Decreasing) | M | SD | Cohen’s D (Decreasing - Low) | M | SD | Cohen’s D (High - Low) | |
| Baseline | |||||||||
| PTSD | 28.38 | 16.74 | 0.60 | 19.99 | 13.11 | 0.06 | 19.19 | 15.62 | 0.58 |
| Depression | 15.04 | 4.71 | 0.82 | 9.88 | 6.78 | 0.05 | 10.1 | 6.29 | 0.82 |
| Functional Impairment | 21.81 | 7.45 | 0.12 | 20.72 | 9.70 | 0.53 | 15.88 | 8.48 | 0.72 |
| 1-Month | |||||||||
| PTSD | 29.50 | 16.44 | 0.71 | 17.46 | 16.13 | 0.26 | 13.44 | 13.77 | 1.05 |
| Depression | 12.00 | 6.78 | 0.72 | 7.64 | 5.89 | 0.30 | 5.91 | 5.84 | 1.00 |
| Functional Impairment | 22.90 | 5.32 | 0.58 | 17.91 | 9.32 | 0.82 | 10.69 | 8.33 | 1.57 |
| 3-Month | |||||||||
| PTSD | 35.14 | 17.93 | 1.13 | 15.69 | 17.13 | 0.31 | 11.03 | 13.44 | 1.69 |
| Depression | 14.86 | 6.52 | 1.22 | 7.07 | 6.36 | 0.61 | 3.79 | 4.36 | 2.32 |
| Functional Impairment | 19.71 | 4.79 | 0.62 | 14.47 | 8.98 | 1.29 | 4.61 | 6.25 | 2.50 |
Note: M = Mean. SD = Standard Deviation
For depression, there was also a significant negative slope (b = −3.23, SE = 0.51, p < .001). There were significant fixed effects for the High Pain Class (b = 4.43, SE = 1.87, p = 0.019) and a slope by High Pain Class interaction (b = 2.56, SE = 1.13, p = 0.024). There was also a significant interaction for slope and Decreasing Pain Class (b = 1.59, SE = 0.73, p = .030). These results suggest that the Low Pain Class experienced an overall decrease in depression symptoms during the three-month period after the trauma. The Decreasing Pain Class also experienced a decrease during this period, albeit at a slower rate. The High Pain Class, however, remained relatively stable during this period.
For functional impairment, a similar pattern of results emerged. There was a significant negative fixed effect for slope (b = −5.57, SE = 0.82, p < .001). There were also significant fixed effects for the High Pain Class (b = 6.17, SE = 2.58, p = .018) and a significant slope by High Pain Class interaction (b = 4.72, SE = 1.80, p = .010). The same results were found for the Decreasing Pain Class with a significant fixed effect (b=. 4.77, SE = 1.84, p = .011) and a significant slope by Decreasing Pain Class interaction (b = 2.41, SE = 1.17, p = .040). These findings suggested that the Low Pain Class had significantly lower functional impairment at the time of trauma and experienced a sharper rate of improvement than the other classes. Furthermore, the High Pain Class experienced the slowest improvement in impairment while having the highest level at the time of the trauma.
Discussion
This study examined the experience of pain across the first month after a traumatic injury and the relationship between change in pain and psychopathology symptoms. Daily mobile assessments allowed for a comprehensive examination of the experience of pain throughout the first month after trauma, a critical period in the development of such impairments (35). Three distinct trajectories of pain were identified. The largest percentage of individuals experienced initial moderate pain that decreased over the first month after injury. The second largest class experienced low initial pain that decreased across the 1-month period. The third class experienced high initial pain that persisted over the first month.
Trajectory membership was related to mental health outcomes and functional impairment at baseline, 1 month and 3 months. At baseline, about five days after injury, the High Pain Class had higher levels of PTSD, and significantly higher depression and functional impairment than the low pain class. The High Pain Class experienced sustained PTSD, depression and functional impairment from baseline to 3 months whereas the Low Pain Class experienced a decrease in these domains. These results are consistent with prior work on mTBI in which only those in the chronic and increasing classes developed PTSD (16). Furthermore, the Decreasing Class reported a slower decrease in depression and disability than the Low Pain Class. Therefore, a trajectory characterized by persistent pain after a trauma may lead to worsening health outcomes, including higher levels of PTSD, depression, and injury-related functional impairment. Conversely, minimal pain after such an event is associated with better outcomes.Furthermore, the differences between trajectory outcomes became more pronounced at the 3-month follow-up. Thus, persistently high pain in the first month after a traumatic injury may be predictive of long-term adverse health outcomes.
The results of this study support the mutual maintenance model, which suggests that pain may exacerbate PTSD symptoms and PTSD may interfere with pain management (9,10). Pain may serve as a reminder of the traumatic event, enhancing reexperiencing symptoms of PTSD, and PTSD avoidance symptoms may hinder pain management (10). Therefore, higher levels of pain may serve as a reminder of the traumatic event that may exacerbate PTSD symptoms. Additionally, prior studies have shown that early PTSD symptoms—specifically arousal symptoms—may predict later pain after trauma (9). This relation should be further explored in subsequent studies. Specifically, future studies should investigate PTSD and pain symptoms simultaneously to examine how pain and PTSD symptoms affect each other over time.
The findings of the present study also contribute to the small body of literature suggesting there is an association between post-injury pain and depression. The high pain class had significantly elevated depression from the low pain trajectories at baseline, and that elevation was sustained at 1-month and 3-months post injury. This difference suggests that sustained elevated pain is associated with higher levels of depression whereas resolving and low pain is not. There are several mechanisms that may explain this relation. Using the findings from the current study, the elevated functional impairment associated with sustained pain may impair the number activities an individual can engage in, which in turn reduces their mood. This could be explained by the fear-avoidance model for chronic pain which suggests that pain can cause pain-related fear and prevent mobility and engagement in activities, which can increase levels of depression and perpetuate pain (35,36). Additionally, these relations may reflect a process that is not present in the first month but is by three months post injury. These associations, and other mechanisms, are only proposed at this stage and should be explored in future work.
These results have clinical implications for post injury care. First, treating pain after a traumatic injury may both reduce pain and reduce the likelihood of developing later psychopathology. For example, morphine administered to combat veterans after injury significantly reduced the incidence of PTSD (37). Amidst concern about opioid addiction, providers are advised to safely prescribe opioids and seek out other pain management strategies (38). As suggested by the current results, effective pain management after a traumatic injury is necessary to prevent chronic pain, depression, PTSD and functional impairment. A recent report provided suggestions for clinical management of acute pain after a musculoskeletal injury including recommendations for pharmacological and nonpharmacologic interventions to promote recovery (38). Patients with elevated or persistent acute pain may benefit from psychosocial interventions such as cognitive behavioral therapy which addresses comorbid depression and posttraumatic stress, and may produce pain relief (38). Therefore, pain-management strategies may also protect against the development of PTSD. Second, consideration of different pain trajectories may inform providers about the efficacy of pain management better than individual pain scores (39). Tracking change in pain could determine if and how pain management should proceed, and secondarily improve other outcomes.
The present study had several limitations. Trajectories of pain experience were identified and related to psychopathology outcomes. Prior research has suggested that injury severity, traumatic brain injury (TBI), and level of consciousness may influence the development of pain and PTSD (40,41). The predictive value of injury-related factors such as injury severity and type should be considered. Additionally, we found that those in the higher pain class had higher levels of PTSD, depression and impairment at the baseline assessment, about five days after injury. It is possible that these higher baseline symptoms may have originated from pre-injury symptoms contributing to higher post-injury pain. However, it was not possible to determine whether these higher baseline symptoms were due to pre- or post-injury factors or a combination and how they contributed to post-injury pain levels. The role of pain medications was not explored. Since pain management may lead to lower pain trajectories and lower PTSD symptomology, it is possible that pain medications taken in the hospital or throughout the first month may have affected the pain trajectories and subsequent PTSD outcome. Further, it would be useful to study the efficacy of in-hospital pain treatments on these trajectories as it could support the hypothesis that early pain treatment may improve recovery. The sample size was modest (n = 87) and consisted of a heterogeneous group of injuries – nearly half of the traumas were motor vehicle crashes. The results may not generalize to the physical and psychiatric outcomes of other traumas. Furthermore, there were no data available on the extent that participants were involved in litigation as a result of their PTE. The involvement in legal processes may have had an influence on the severity of pain and impairments (42). Finally, due to the timing of measurements, it is difficult to determine the temporal relation of pain and these outcomes.
The results of this study demonstrated that pain in the first month after a traumatic injury followed three trajectories which differentially related to later PTSD, depression and functional impairment. Having a low pain trajectory may reduce the risk of developing such conditions, while having a persistent high level of pain may increase risk. Providing early intervention that targets pain may thus have numerous benefits. Further study on the early experience of pain and its effect on PTSD development in the acute post trauma period is warranted.
Acknowledgments
Conflicts of Interest and Source of Funding: The authors have no conflicts of interest. This study was funded by UVM REACH Award, UVM Summer Undergraduate Research Fellowship Award, and NIMH - 1K08MH107661-01A1.
Acronyms used:
- PTE
potentially traumatic event
- PTSD
post-traumatic stress disorder
- LCGA
latent class growth analysis
- LGCM
latent growth class analysis
- ED
emergency department
- PCL-5
PTSD Checklist for DSM-5
- PHQ-8
Patient Health Questionnaire
- SDS
Sheehan Disability Score
- AIC
Aikaike Information Criteria
- BIC
Bayesian Information Criteria
- SSABIC
sample-size adjusted Bayesian Information Criteria
- VLMR LRT
Vuong-Lo-Mendell Rubin Likelihood Ratio Test
- LMR LRT
Lo-Mendell-Rubin Likelihood Ratio Test
- BLRT
Bootstrap Likelihood Ratio Test.
References
- 1.Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National Estimates of Exposure to Traumatic Events and PTSD Prevalence Using DSM-IV and DSM-5 Criteria. J Trauma Stress. 2013. October 1;26(5):537–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O’Donnell ML, Varker T, Holmes AC, Ellen S, Wade D, Creamer M, Silove D, McFarlane A, Bryant RA. Disability After Injury: The Cumulative Burden of Physical and Mental Health. J Clin Psychiatry. 2013. February 15;74(02):e137–43. [DOI] [PubMed] [Google Scholar]
- 3.Asmundson GJ, Coons MJ, Taylor S, Katz J. PTSD and the Experience of Pain: Research and Clinical Implications of Shared Vulnerability and Mutual Maintenance Models. Can J Psychiatry. 2002. December 1;47(10):930–7. [DOI] [PubMed] [Google Scholar]
- 4.Qi W, Gevonden M, Shalev A. Prevention of Post-Traumatic Stress Disorder After Trauma: Current Evidence and Future Directions. Curr Psychiatry Rep. 2016. February;18(2):20–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Archer KR, Heins SE, Abraham CM, Obremskey WT, Wegener ST, Castillo RC. Clinical Significance of Pain at Hospital Discharge Following Traumatic Orthopedic Injury: General Health, Depression, and PTSD Outcomes at 1 Year. Clin J Pain. 2016. March;32(3):196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hildenbrand AK, Marsac ML, Daly BP, Chute D, Kassam-Adams N. Acute Pain and Posttraumatic Stress After Pediatric Injury. J Pediatr Psychol. 2016. January 1;41(1):98–107. [DOI] [PubMed] [Google Scholar]
- 7.Norman SB, Stein MB, Dimsdale JE, Hoyt DB. Pain in the aftermath of trauma is a risk factor for post-traumatic stress disorder. Psychol Med. 2008. April;38(4):533–42. [DOI] [PubMed] [Google Scholar]
- 8.Brennstuhl M-J, Tarquinio C, Montel S. Chronic Pain and PTSD: Evolving Views on Their Comorbidity. Perspect Psychiatr Care. 2015;51(4):295–304. [DOI] [PubMed] [Google Scholar]
- 9.Liedl A, Silove D, McFarlane A, Knaevelsrud C, Bryant RA. Support for the mutual maintenance of pain and post-traumatic stress disorder symptoms. Psychol Med. 2010. July;40(7):1215–23. [DOI] [PubMed] [Google Scholar]
- 10.Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: mutual maintenance? Clin Psychol Rev. 2001. August 1;21(6):857–77. [DOI] [PubMed] [Google Scholar]
- 11.Ullrich PM, Smith BM, Poggensee L, Evans CT, Stroupe KT, Weaver FM, Burns SP. Pain and Post-Traumatic Stress Disorder Symptoms During Inpatient Rehabilitation Among Operation Enduring Freedom/Operation Iraqi Freedom Veterans With Spinal Cord Injury. Arch Phys Med Rehabil. 2013. January;94(1):80–5. [DOI] [PubMed] [Google Scholar]
- 12.Chapman CR, Fosnocht D, Donaldson GW. Resolution of acute pain following discharge from the emergency department: the acute pain trajectory. J Pain Off J Am Pain Soc. 2012. March;13(3):235–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trevino C, deRoon-Cassini T, Szabo A, Brasel K. Acute longitudinal pain trajectories in the traumatically injured. SOJ Anesthesiol Pain Manag. 2015. September 27;2(3):1–7. [Google Scholar]
- 14.Giummarra MJ, Casey SL, Devlin A, Ioannou LJ, Gibson SJ, Georgiou-Karistianis N, Jennings PA, Cameron PA, Ponsford J. Co-occurrence of posttraumatic stress symptoms, pain, and disability 12 months after traumatic injury. Pain Rep. 2017. September;2(5):e622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bartoszek G, Hannan SM, Kamm J, Pamp B, Maieritsch KP. Trauma-Related Pain, Reexperiencing Symptoms, and Treatment of Posttraumatic Stress Disorder: A Longitudinal Study of Veterans: Trauma-Related Pain and Treatment of PTSD. J Trauma Stress. 2017. June;30(3):288–95. [DOI] [PubMed] [Google Scholar]
- 16.Sawyer K, Bell KR, Ehde DM, Temkin N, Dikmen S, Williams RM, Dillworth T, Hoffman JM. Longitudinal Study of Headache Trajectories in the Year After Mild Traumatic Brain Injury: Relation to Posttraumatic Stress Disorder Symptoms. Arch Phys Med Rehabil. 2015. November 1;96(11):2000–6. [DOI] [PubMed] [Google Scholar]
- 17.Yurgil KA, Barkauskas DA, Vasterling JJ, Nievergelt CM, Larson GE, Schork NJ, Litz BT, Nash WP, Baker DG. Association Between Traumatic Brain Injury and Risk of Posttraumatic Stress Disorder in Active-Duty Marines. JAMA Psychiatry. 2014. February 1;71(2):149–57. [DOI] [PubMed] [Google Scholar]
- 18.Lerman SF, Rudich Z, Brill S, Shalev H, Shahar G. Longitudinal Associations Between Depression, Anxiety, Pain, and Pain-Related Disability in Chronic Pain Patients. Psychosom Med. 2015. April;77(3):333–341. [DOI] [PubMed] [Google Scholar]
- 19.Riddle DL, Kong X, Fitzgerald GK. Psychological health impact on 2-year changes in pain and function in persons with knee pain: data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2011. September;19(9):1095–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kroenke K, Wu J, Bair MJ, Krebs EE, Damush TM, Tu W. Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. J Pain Off J Am Pain Soc. 2011. September;12(9):964–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kroenke K, Outcalt S, Krebs E, Bair MJ, Wu J, Chumbler N, Yu Z. Association between anxiety, health-related quality of life and functional impairment in primary care patients with chronic pain. Gen Hosp Psychiatry. 2013. July 1;35(4):359–65. [DOI] [PubMed] [Google Scholar]
- 22.Foa EB, Rothbaum BO. Treating the trauma of rape: Cognitive-behavioral therapy for PTSD. Guilford Press; 2001. [Google Scholar]
- 23.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011. November 1;63(S11):S240–52. [DOI] [PubMed] [Google Scholar]
- 24.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J Trauma Stress. 2015. December 1;28(6):489–98. [DOI] [PubMed] [Google Scholar]
- 25.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. J Gen Intern Med. 2001. September 1;16(9):606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sheehan D Sheehan disability scale. Handb Psychiatr Meas. 1983;2:100–2. [Google Scholar]
- 27.Price M, Legrand AC, Brier ZMF, Gratton J, Skalka C. The short-term dynamics of posttraumatic stress disorder symptoms during the acute posttrauma period. Depress Anxiety. 2019. November 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Psychiatric Association. Diagnostic and statistical manual of mental disorders [Internet]. 5th ed. Washington, DC; 2013. Available from: 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- 29.Price M, Van Stolk-Cooke K, Legrand AC, Brier ZMF, Ward HL, Connor JP, Gratton J, Freeman K, Skalka C. Implementing assessments via mobile during the acute posttrauma period: feasibility, acceptability and strategies to improve response rates. Eur J Psychotraumatology. 2018;9(Suppl 1):1500822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Price M, Van Stolk-Cooke K, Brier ZMF, Legrand AC. mHealth solutions for early interventions after trauma: improvements and considerations for assessment and intervention throughout the acute post-trauma period. MHealth. 2018;4:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.deRoon-Cassini TA, Mancini AD, Rusch MD, Bonanno GA. Psychopathology and resilience following traumatic injury: A latent growth mixture model analysis. Rehabil Psychol. 2010;55(1):1–11. [DOI] [PubMed] [Google Scholar]
- 32.Wickrama KAS, Lee TK, O’Neal CW, Lorenz FO. Higher-Order Growth Curves and Mixture Modeling with Mplus: A Practical Guide (Multivariate Applications Series). New York: Routledge; 2016. 326 p. [Google Scholar]
- 33.Muthén LK, Muthén BO. Mplus User’s Guide. Seventh Los Angeles, CA: Muthén & Muthén; 2015. [Google Scholar]
- 34.Whitman JB, North CS, Downs DL, Spitznagel EL. A prospective study of the onset of PTSD symptoms in the first month after trauma exposure. 2013. May 1;25(2):8E–17E. [PubMed] [Google Scholar]
- 35.Zale EL, Ditre JW. Pain-Related Fear, Disability, and the Fear-Avoidance Model of Chronic Pain. Curr Opin Psychol. 2015. October 1;5:24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000. April;85(3):317–32. [DOI] [PubMed] [Google Scholar]
- 37.Holbrook TL, Galarneau MR, Dye JL, Quinn K, Dougherty AL. Morphine Use after Combat Injury in Iraq and Post-Traumatic Stress Disorder. N Engl J Med. 2010. January 14;362(2):110–7. [DOI] [PubMed] [Google Scholar]
- 38.Hsu JR, Mir H, Wally MK, Seymour RB. Clinical Practice Guidelines for Pain Management in Acute Musculoskeletal Injury. J Orthop Trauma. 2019. May;33(5):e158–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chapman CR, Donaldson GW, Davis JJ, Bradshaw DH. Improving Individual Measurement of Postoperative Pain: The Pain Trajectory. J Pain Off J Am Pain Soc. 2011. February;12(2):257–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Delahanty DL, Raimonde AJ, Spoonster E, Cullado M. Injury severity, prior trauma history, urinary cortisol levels, and acute PTSD in motor vehicle accident victims. J Anxiety Disord. 2003;17(2):149–64. [DOI] [PubMed] [Google Scholar]
- 41.Melcer T, Walker J, Sechriest VF, Lebedda M, Quinn K, Galarneau M. Glasgow Coma Scores, Early Opioids, and Posttraumatic Stress Disorder Among Combat Amputees. J Trauma Stress. 2014. April 1;27(2):152–9. [DOI] [PubMed] [Google Scholar]
- 42.Heron-Delaney M, Kenardy J, Charlton E, Matsuoka Y. A systematic review of predictors of posttraumatic stress disorder (PTSD) for adult road traffic crash survivors. Injury. 2013. November;44(11):1413–22. [DOI] [PubMed] [Google Scholar]


