Abstract
Homelessness in the United States is often examined using cross-sectional, point-in-time samples. Any experience of homelessness is a risk factor for adverse outcomes, so it is also useful to understand the incidence of homelessness over longer periods. We estimate the lifetime prevalence of homelessness among members of the Baby Boom cohort (n = 6,545) using the 2012 and 2014 waves of the Health and Retirement Study (HRS), a nationally representative survey of older Americans. Our analysis indicates that 6.2 % of respondents had a period of homelessness at some point in their lives. We also identify dramatic disparities in lifetime incidence of homelessness by racial and ethnic subgroups. Rates of homelessness were higher for non-Hispanic blacks (16.8 %) or Hispanics of any race (8.1 %) than for non-Hispanic whites (4.8 %; all differences significant with p < .05). The black-white gap, but not the Hispanic-white gap, remained significant after adjustment for covariates such as education, veteran status, and geographic region.
Keywords: homelessness, racial and ethnic disparities, Health and Retirement Study
Introduction
Public officials and professional organizations recognize homelessness as a major public health and social welfare problem in the United States (Donovan and Shinseki 2013; Larkin et al. 2016). Our understanding of homelessness is limited by the data typically available, however. The main source of homelessness statistics in the United States, the Annual Homeless Assessment Report (AHAR), relies on point-in-time counts of sheltered and unsheltered individuals and annual counts of homelessness services users (U.S. Department of Housing and Urban Development 2017). Any period of homelessness is associated with adverse health consequences (Oppenheimer et al. 2016), so lifetime prevalence—that is, the fraction of individuals who have ever experienced homelessness—is also a useful indicator of the size of the affected population. Further, although AHAR data indicate substantial racial and ethnic disparities in the prevalence of homelessness (Henry et al. 2016), these estimates do not control for other characteristics. Outside AHAR, most studies of homelessness have used nonrepresentative samples to study specific subpopulations, such as Veteran’s Affairs services clients (Montgomery et al. 2015), or have large standard errors that make inferences about subgroups difficult (Link et al. 1994; Shelton et al. 2009).
We use recent, nationally representative data from the Health and Retirement Study (HRS) to estimate the lifetime prevalence of homelessness at late midlife both overall and for subgroups defined by race and ethnicity. We find that approximately 6 % of all American adults from the Baby Boom generation have experienced at least one spell of homelessness as measured by the HRS survey question. Our results also show dramatic, significant disparities in the lifetime prevalence of homelessness for non-Hispanic blacks compared with non-Hispanic whites that are not explained by differences in characteristics such as education, veteran status, and geographic region. One in six non-Hispanic black Baby Boomers reported having been homeless at some point, more than three times the rate for non-Hispanic whites. Hispanics of all races report a significantly higher lifetime prevalence of homelessness than non-Hispanic whites, but this disparity is largely explained by other characteristics.
Background
Homelessness is associated with a range of poor physical and mental health outcomes, including premature death (Barrow et al. 1999; Fazel et al. 2014; Montgomery et al. 2016; O’Connell 2005). These patterns are found even in studies able to account for characteristics, such as adverse childhood experiences, that increase the risk of both homelessness and health problems (Oppenheimer et al. 2016). As a consequence, homelessness incurs substantial public costs (Culhane 2008). Gauging the scope and identifying correlates of homelessness, though, is inherently difficult because even defining homelessness prompts debate (Hopper 1995; Lee et al. 2010). Even with consensus about who is considered homeless, actually counting these individuals presents serious challenges given that they may be “hidden” in easily overlooked or hard-to-access places (Hopper et al. 2008; Link et al. 1994, 1995; Wright and Devine 1995). Nationally representative surveys such as the Current Population Survey (CPS) that rely on a housing unit–based sampling frame will by design omit individuals experiencing a spell of current homelessness.
The AHAR attempts to provide a nationally representative portrait of homelessness in the United States through an annual point-in-time (PIT) count from a single night in January and counts of shelter and transitional housing services users within a 12-month time frame. The PIT count relies on reports from local Continuums of Care (CoCs), planning coalitions that coordinate homeless services in a designated geographic area. CoCs develop their own count methods. Although the federal government provides technical assistance on effective techniques and must approve count plans (Buron et al. 2016), these varying methods raise serious issues of validity and reliability (Schneider et al. 2016). The annual counts use a management information system to gather reports on individuals served by emergency and transitional housing providers, excluding anyone not using such resources. Moreover, the AHAR counts provide limited information on other characteristics, making it impossible to isolate the contribution of different risk factors correlated with homelessness.
Even the most precise PIT estimates of homelessness understate the problem’s reach and bias our understanding (Phelan and Link 1999). A single spell of homelessness is associated with adverse outcomes (Oppenheim et al. 2016), so a PIT count captures only a fraction of those affected by homelessness. At least as important, from the perspectives of both population description and problem identification, is the group of individuals that have ever experienced homelessness. A lifetime estimate also addresses some of the measurement challenges intrinsic to PIT counts, such as the problem of hidden homelessness cited earlier (Hopper et al. 2008; Link et al. 1994, 1995). Counts may also overlook individuals in a spell of homelessness but not conforming to stereotypes, an issue Hopper and colleagues (2008) illuminated using decoy respondents during a count in New York City. Those who are currently in a period of homelessness may also hesitate to identify as such in a survey interview because of stigma (Link et al. 1994).
We are aware of two studies that have measured lifetime prevalence of homelessness in random samples of adults of different ages. Link and colleagues (1994) conducted a telephone survey of 1,507 randomly sampled adults across the continental United States, estimating that the lifetime prevalence of homelessness among adults was 14.0 % when including doubling up (staying “in a friend’s or relative’s home because you were homeless” (p. 1909)) and 7.4 % when restricted to literal homelessness (dwelling in a place not meant for human habitation or a temporary residence, such as a shelter). These data were collected in 1990 and are now dated, however. Shelton et al. (2009) examined lifetime experiences of homelessness using the National Longitudinal Study of Adolescent Health (Add Health), a large, nationally representative survey, finding that approximately 5 % of respondents had experienced homelessness.1 This analysis had a large sample size (n = 14,888); however, Add Health is limited to young adults (aged 18–28 in 2001, the survey wave used by the researchers) and thus reflects experiences of homelessness relatively early in the life course.
The studies by Link et al. (1994) and Shelton et al. (2009) also present a puzzle about the role of race and ethnicity as risk factors for homelessness. The AHAR identifies clear racial disparities in homelessness (Henry et al. 2016), as do other studies using more limited samples (Culhane and Metraux 1999; Fargo et al. 2012; Folsom et al. 2005; Montgomery et al. 2015). In contrast, Link and colleagues (1994) did not find a statistically significant relationship between race or ethnicity and homelessness. It is also unclear whether their estimate is from a bivariate model or a multivariate model that controls for other characteristics. Shelton et al. (2009) estimated multivariate models but found a statistically significant increase in risk of homelessness only for Native Americans. The researchers did not report bivariate correlations between race and homelessness for their sample. Thus, it remains unclear whether the discrepancy between the stark racial disparities in the AHAR and the insignificant racial disparities in existing estimates of lifetime prevalence can be explained by the lack of covariates in the AHAR data, the relatively small sample size in the Link et al. (1994) study, or the focus on young adults in Shelton et al. (2009). In the present study, we offer estimates of racial and ethnic disparities in the lifetime prevalence of homelessness both with and without covariates using a large, nationally representative sample of adults in late midlife, allowing us to resolve at least partially the apparent inconsistency between PIT and lifetime studies regarding racial and ethnic disparities in experiences of homelessness.
Methods
Data are drawn from the 2012 and 2014 waves of the Health and Retirement Study (HRS 2012, 2014), a biennial, longitudinal survey of older Americans conducted since 1992 (Sonnega et al. 2014). The HRS is sponsored by the National Institute on Aging (Grant Number NIA U01AG009740) and is conducted by the University of Michigan. In 2012, a random half-sample of respondents were asked, “Have you ever been homeless or lived in a shelter?” The other half-sample received this question in 2014. The question as constructed does create uncertainties in interpretation, as we discuss later. We pool data from both years on individuals born in 1946–1964 for a total sample of 6,545 individuals aged 47 to 68 when surveyed. We compare the lifetime prevalence of homelessness as measured by the HRS for non-Hispanic whites (82 % of weighted sample), non-Hispanic blacks (10 %), and Hispanics of any race (8 %). To address the possibility that differences in homelessness are driven by factors other than race, we estimate Eq. (1):
| (1) |
The vector X includes the following covariates: education, female, age, veteran status, U.S.-born, census region, and urbanicity. We use the results from this model to calculate covariate-adjusted predicted probabilities of homelessness by race, with other covariates held constant at their means.
Results
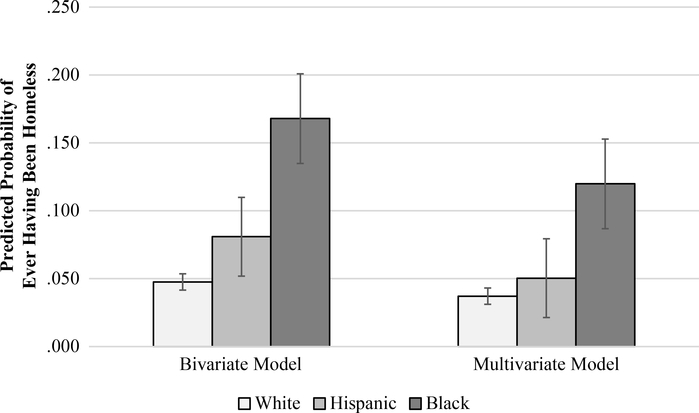
Overall, as measured by an affirmative response to the HRS homelessness question, 6.2 % of respondents had been homeless at some point (Table 1). Lifetime prevalence was significantly higher for minorities; 1 in 6 non-Hispanic blacks (16.8 %) and 1 in 12 Hispanics (8.1 %) had been homeless at some point, compared with 1 in 20 non-Hispanic whites (4.8 %). The covariate-adjusted predicted probabilities of homelessness from the multivariate model are reported in Table 1, and the full results of the model estimating Eq. (1) are reported in Table 2. Adjusting for the aforementioned covariates explains nearly all the Hispanic-white disparity. However, the black-white disparity remains large and statistically significant, with non-Hispanic blacks three times as likely as non-Hispanic whites to have experienced homelessness at some point during their lives (12.0 % vs. 3.7 %). Non-Hispanic blacks are more than twice as likely as Hispanics to have experienced homelessness (12.0 % vs. 5.0 %). Both the bivariate and the multivariate disparities are summarized graphically in Fig. 1.
Table 1.
Lifetime prevalence of homelessness at midlife, by race/ethnicity, for the Baby Boom cohort (birth years 1946–1963) observed at ages 51–68
| Total | Non-Hispanic White | Hispanic (any race) | Non-Hispanic Black | |
|---|---|---|---|---|
| Bivariate Results | ||||
| Prob(Ever homeless) | 0.062 (0.003) | 0.048 (0.003) | 0.081* (0.015) | 0.168** (0.017) |
| Multivariate Resultsa | ||||
| Prob(Ever homeless) | 0.056 (0.003) | 0.037 (0.003) | 0.050 (0.014) | 0.120** (0.015) |
| Mean Characteristics | ||||
| Age | 60.0 | 60.0 | 59.8 | 59.9 |
| Education | ||||
| Less than high school | 0.092 | 0.052 | 0.399** | 0.183** |
| High school | 0.279 | 0.279 | 0.262 | 0.293 |
| Some college | 0.458 | 0.479 | 0.265** | 0.446 |
| College degree or more | 0.170 | 0.191 | 0.073** | 0.078** |
| Female | 0.552 | 0.545 | 0.547 | 0.608** |
| Military veteran | 0.131 | 0.134 | 0.070** | 0.156 |
| U.S.-born | 0.925 | 0.968 | 0.473** | 0.932** |
| Unweighted n | 6,545 | 4,085 | 1,015 | 1,445 |
Note: Standard errors are shown in parentheses.
Source: Health and Retirement Study, 2012 and 2014.
Average predicted probabilities from a multivariate logistic model, calculated with all covariates held constant at their mean values. Covariates in addition to race/ethnicity include age, education, gender, veteran status, U.S. nativity, region, and urbanicity.
Estimate is significantly different from the estimate for Non-Hispanic whites at p < .05
Estimate is significantly different from the estimate for Non-Hispanic whites at p < .01
Table 2.
Logistic regression results (dependent variable = 1 if ever homeless): Health and Retirement Study, 2012 and 2014 (n = 6,545)
| Odds Ratio | SE | |
|---|---|---|
| Race/Ethnicity | ||
| Non-Hispanic white (ref.) | ||
| Non-Hispanic black | 3.530** | 0.569 |
| Hispanic (any race) | 1.376 | 0.403 |
| Education | ||
| Less than high school (ref.) | ||
| High school | 0.288** | 0.052 |
| Some college | 0.306** | 0.054 |
| College or more | 0.168** | 0.052 |
| Other Demographic Characteristics | ||
| Age | 0.884** | 0.012 |
| = 1 if female | 0.845 | 0.111 |
| = 1 if military veteran | 2.278** | 0.413 |
| = 1 if U.S. native | 3.585** | 1.126 |
| Region | ||
| New England (ref.) | ||
| Mid-Atlantic | 1.659 | 0.655 |
| East North Central | 1.209 | 0.544 |
| West North Central | 1.177 | 0.557 |
| South Atlantic | 0.999 | 0.452 |
| East South Central | 1.583 | 0.770 |
| West South Central | 2.139 | 0.997 |
| Mountain | 1.764 | 0.742 |
| Pacific | 2.419† | 0.996 |
| Urbanicity | ||
| Urban (ref.) | ||
| Suburban | 1.150 | 0.203 |
| Ex-urban | 0.997 | 0.216 |
| Constant | 42.039 | 36.372 |
p < .10
p < .01
Fig. 1.
Lifetime prevalence of homelessness by race/ethnicity: Health and Retirement Study, 2012 and 2014
Beyond the racial and ethnic disparities of primary interest in this analysis, results from the control variables in the multivariate model warrant brief mention. Increases in education are associated with reduced risk of homelessness, with those completing high school, some college, or graduating college each having a significantly lower risk of homelessness than respondents without a high school diploma or equivalent. Increased age is also inversely associated with the probability of any experiences of homelessness (which may reflect selective mortality, an issue we discuss more in the next section). Military veterans and U.S. natives experienced homelessness at notably higher rates than nonveterans and immigrants, respectively. Geographic region is not a strong predictor of homelessness, with only the Pacific region having a significant association (at the .10 level) compared with New England, the base category. Neither suburban nor exurban respondents have a statistically significant difference in reported homelessness compared with their urban peers.
Discussion
Our estimate of the lifetime prevalence of homelessness, with approximately 6.2 % of Baby Boomer adults having experienced at least one episode, is consistent with the small body of existing research. Our figure is slightly higher than the estimate produced by Shelton et al.’s (2009) study of younger adults and slightly lower than the estimate of lifetime literal homelessness found by Link and colleagues (1994). Together with these earlier studies, our analysis confirms that homelessness is far more common than PIT studies capture. The 2016 AHAR PIT count, for example, estimated that 549,928 individuals experienced homelessness on a single night in January of that year, approximately 0.17 % of the U.S. population of 323 million (Henry et al. 2016). Homelessness is generally a temporary or a cyclical experience rather than a chronic condition (Kuhn and Culhane 1998), yet any experience of homelessness is a risk factor for adverse outcomes (Oppenheimer et al. 2016). Although a PIT count provides valuable information on trends in homelessness and cross-sectional description of those experiencing homelessness at one time, it cannot fully capture the size of the affected population given that only a fraction of that group will be currently homeless on any given day. Counts are also subject to extensive challenges posed by identifying individuals currently experiencing homelessness (Hopper et al. 2008; Link et al. 1995). A lifetime estimate provides a valuable complement by better estimating the scope of the population affected by—rather than currently experiencing—homelessness.
Our analysis also identifies striking and significant differences in lifetime experiences of homelessness by race: Non-Hispanic blacks are over three times more likely than non-Hispanic whites to have experienced at least one bout of homelessness, and this gap persists after adjustment for covariates. This result contrasts with insignificant estimates of racial disparities in earlier studies, raising the question of how homelessness relates to well-documented racial disparities in health (Williams 2005). Do experiences of homelessness contribute to racial disparities in health? Do health disparities contribute to differences in the prevalence of homelessness? Are the two mutually reinforcing, or do they covary as products of social discrimination or economic inequalities? Future research might aim to better understand these complex pathways. It should also seek to identify the factors, unobserved in this study, that increase the risk of homelessness for blacks given that observed social and economic characteristics largely explain the elevated risk of homelessness for Hispanics compared with non-Hispanic whites.
The analysis is subject to a number of limitations. Most critically, the survey question about homelessness provides limited guidance to the respondent, and inclusion of the phrase “or lived in a shelter” may compound respondents’ confusion about what should count as homelessness. Respondents likely have different conceptualizations of the issue, and the subsequent differences in survey answers at best are a source of random measurement error and at worst systematically bias our estimates of racial and ethnic disparities, if respondents from different racial/ethnic groups interpret this ambiguity dissimilarly. Homelessness is also not a homogenous experience, and researchers have developed multidimensional typologies to capture the extensive variation (McAllister et al. 2011). Link et al.’s (1994) earlier study on lifetime prevalence explicitly distinguished between experiences of “literal” and “doubled up” homelessness, and the precision of our estimates would undoubtedly benefit from such additional detail. Given that we are limited by the question in the HRS survey, however, we must acknowledge that its very general wording adds uncertainty and may be a source of bias. This limitation also points to an opportunity for other population-based surveys. Specifically, surveys might improve the quality of data on homelessness if they were to explicitly measure both “literal” and “doubled-up” experiences of homelessness while giving respondents guidance about how these are defined to help them answer accurately.
The study has two additional limitations worth noting. First, our estimate of homelessness may still be an undercount. The HRS will not capture currently homeless or institutionalized individuals in its baseline wave, and study participants who become homeless after the baseline interview may be less likely to respond to subsequent interviews. There may also be population attrition due to selective mortality. Given that homelessness is a risk factor for premature death, it is likely that a larger proportion of those that have experienced homelessness have died before reaching late midlife compared with those who have never experienced homelessness.2 Any of these factors will bias our estimate of the lifetime prevalence of homelessness toward 0 and may also have consequences for our estimates of racial disparities (Metraux et al. 2011). Second, homelessness may be especially common among the Baby Boom generation (Culhane et al. 2013). Whether and how the findings reported here apply to younger cohorts is unclear.
Despite these limitations, our analysis makes an important contribution to describing the population affected by homelessness in the United States. Our results indicate experiences of homelessness are far from rare: approximately 6.2 % of the population of Baby Boomer adults have experienced at least a single spell as measured by an affirmative response to the HRS survey question. This estimate is roughly similar to those provided by the small body of studies of lifetime prevalence. Unlike those analyses, however, we document clear and statistically significant racial and ethnic disparities in the lifetime risk of homelessness. We further find that the black-white disparity is robust to adjustment for observed covariates, such as educational attainment, whereas the Hispanic-white disparity is largely accounted for by these other characteristics. In the context of this finding, the relationship between homelessness and other racially patterned health and social disparities warrants continued investigation.
Acknowledgements:
The HRS (Health and Retirement Study) is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan. The authors thank external reviewers and the editors for helpful comments and suggestions.
Footnotes
Add Health prompts respondents with criteria defining homelessness, including staying in a place not meant for sleeping, staying in a shelter, or lacking a fixed residence (Shelton et al. 2009).
Supplemental analysis of HRS data shows that individuals who have ever been homeless are in worse health than those who have not; they are twice as likely to be in fair or poor health and are significantly more likely to report heart disease, lung disease, or having ever had cancer or a stroke. These results hold both with and without adjustment for characteristics, including gender, race, ethnicity, education, and age.
References
- Barrow SM, Herman DB, Cordova P, & Struening EL (1999). Mortality among homeless shelter residents in New York City. American Journal of Public Health, 89, 529–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buron L, McCall T, & Solari CD (2016). The 2015 Annual Homeless Assessment Report (AHAR) to Congress, Part 2: Estimates of homelessness in the United States, data collection and analysis methodology. Washington, DC: U.S. Department of Housing and Urban Development, Office of Community Planning and Development. [Google Scholar]
- Culhane DP (2008). The cost of homelessness: A perspective from the United States. European Journal of Homelessness, 2, 97–114. [Google Scholar]
- Culhane DP, & Metraux S (1999). One-year rates of public shelter utilization by race/ethnicity, age, sex and poverty status for New York City (1990 and 1995) and Philadelphia (1995). Population Research and Policy Review, 18, 219–236. [Google Scholar]
- Culhane DP, Metraux S, Byrne T, Stino M, & Bainbridge J (2013). The age structure of contemporary homelessness: Evidence and implications for public policy. Analyses of Social Issues and Public Policy, 13, 228–244. 10.1111/asap.12004 [DOI] [Google Scholar]
- Donovan S, & Shinseki EK (2013). Homelessness is a public health issue. American Journal of Public Health, 103(S2), S210–S211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fargo J, Metraux S, Byrne T, Munley E, Montgomery AE, Jones H, … Culhane, D. (2012). Prevalence and risk of homelessness among US veterans. Preventing Chronic Disease, 9, E45 10.5888/pcd9.110112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel S, Geddes JR, & Kushel M (2014). The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet, 384, 1529–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folsom DP, Hawthorne W, Lindamer L, Gilmer T, Bailey A, Golshan S, … Jeste DV (2005). Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. American Journal of Psychiatry, 162, 370–376. [DOI] [PubMed] [Google Scholar]
- Health and Retirement Study (HRS 2012 Core Final Release) public use dataset. (2012). Produced and distributed by the University of Michigan with funding from the National Institute on Aging (Grant No. NIA U01AG009740). Ann Arbor: University of Michigan. [Google Scholar]
- Health and Retirement Study (HRS 2014 Core Final Release) public use dataset. (2014). Produced and distributed by the University of Michigan with funding from the National Institute on Aging (Grant No. NIA U01AG009740). Ann Arbor: University of Michigan. [Google Scholar]
- Henry M, Watt R, Rosenthal L, & Shivji A (2016). The 2016 Annual Homeless Assessment Report (AHAR) to Congress, Part 1: Point-in-time estimates of homelessness. Washington, DC: U.S. Department of Housing and Urban Development, Office of Community Planning and Development. [Google Scholar]
- Hopper K (1995). Definitional quandaries and other hazards in counting the homeless: An invited commentary. American Journal of Orthopsychiatry, 63, 340–346. [DOI] [PubMed] [Google Scholar]
- Hopper K, Shinn M, Laska E, Meisner M, & Wanderling J (2008). Estimating the numbers of unsheltered homeless people through plant-capture and postcount survey methods. American Journal of Public Health, 98, 1438–1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn R, & Culhane DP (1998). Applying cluster analysis to test a typology of homelessness by pattern of shelter utilization: Results from the analysis of administrative data. American Journal of Community Psychology, 26, 207–232. [DOI] [PubMed] [Google Scholar]
- Larkin H, Henwood B, Fogel SJ, Aykanian A, Briar-Lawson KH, Donaldson LP, … Streeter CL (2016). Responding to the grand challenge to end homelessness: The national homelessness social work initiative. Families in Society, 97, 153–159. [Google Scholar]
- Lee BA, Tyler KA, & Wright JD (2010). The new homelessness revisited. Annual Review of Sociology, 36, 501–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan J, Bresnahan M Stueve, A., Moore, R., & Susser, E. (1995). Lifetime and five-year prevalence of homelessness in the United States: New evidence on an old debate. American Journal of Orthopsychiatry, 65, 347–354. [DOI] [PubMed] [Google Scholar]
- Link BG, Susser E, Stueve A, Phelan J, Moore RE, & Struening E (1994). Lifetime and five-year prevalence of homelessness in the United States. American Journal of Public Health, 84, 1907–1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAllister W, Lennon MC, & Kuang L (2011). Rethinking research on forming typologies of homelessness. American Journal of Public Health, 101, 596–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metraux S, Eng N, Bainbridge J, & Culhane DP (2011). The impact of shelter use and housing placement on mortality hazard for unaccompanied adults and adults in family households entering New York City shelters: 1990–2002. Journal of Urban Health, 88, 1091–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery AE, Dicter ME, Thomasson AM, Fu X, & Roberts CB (2015). Demographic characteristics associated with homelessness and risk among female and male veterans accessing VHA outpatient care. Women’s Health Issues, 25, 42–48. [DOI] [PubMed] [Google Scholar]
- Montgomery AE, Szymkowiak D, Marcus J, Howard P, & Culhane DP (2016). Homelessness, unsheltered status, and risk factors for mortality: Findings from the 100 000 homes campaign. Public Health Reports, 131(6), 765–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connell JJ (2005). Premature mortality in homeless populations: A review of the literature. Nashville, TN: National Health Care for the Homeless Council. [Google Scholar]
- Oppenheimer SC, Nurius PS, & Green S (2016). Homelessness history impacts on health outcomes and economic and risk behavior intermediaries: New insights from population data. Families in Society, 43, 576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan JC, & Link BG (1999). Who are “the homeless”? Reconsidering the stability and composition of the homeless population. American Journal of Public Health, 89, 1334–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider M, Brisson D, & Burnes D (2016). Do we really know how many are homeless? An analysis of the point-in-time homelessness count. Families in Society, 97, 321–329. [Google Scholar]
- Shelton KH, Taylor PJ, Bonner A, & van den Bree M (2009). Risk factors for homelessness: Evidence from a population-based study. Psychiatric Services, 60, 465–472. [DOI] [PubMed] [Google Scholar]
- Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, & Weir DR (2014). Cohort profile: The Health and Retirement Study (HRS). International Journal of Epidemiology, 43, 576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Housing and Urban Development. (2017). An introductory guide to the annual homeless assessment report. Washington, DC: U.S. Department of Housing and Urban Development; Retrieved from https://www.hudexchange.info/resources/documents/Introductory-Guide-to-the-2017-AHAR.pdf[ [Google Scholar]
- Williams DR (2005). The health of U.S. racial and ethnic populations. Journals of Gerontology: Series B, Psychological Sciences & Social Sciences, 60(Special Issue 2), S53–S62. [DOI] [PubMed] [Google Scholar]
- Wright JD, & Devine JA (1995). Housing dynamics of the homeless: Implications for a count. American Journal of Orthopsychiatry, 63, 320–329. [DOI] [PubMed] [Google Scholar]