Abstract
Background:
The inclusion of Z-codes for social determinants of health (SDOH) in the tenth revision of the International Classification of Diseases (ICD-10) may offer an opportunity to improve data collection of SDOH, but no characterization of their utilization exists on a national all-payer level.
Objective:
To examine the prevalence of SDOH Z-codes and compare characteristics of patients with and without Z-codes and hospitals that do and do not use Z-codes.
Research Design:
Retrospective cohort study using 2016 and 2017 National Inpatient Sample
Participants:
14,289,644 inpatient hospitalizations.
Measures:
Prevalence of SDOH Z-codes (codes Z55-Z65) and descriptive statistics of patients and hospitals.
Results:
Of admissions, 269,929 (1.9%) included SDOH Z-codes. Average monthly SDOH Z-code use increased across the study period by 0.01% per month (p<0.001). The cumulative number and proportion of hospitals that had ever used an SDOH Z-code also increased, from 1,895 hospitals (39%) in January 2016 to 4,188 hospitals (86%) in December 2017. Hospitals that coded at least 1 SDOH Z-code were larger, private not-for-profit, and urban teaching hospitals. Compared to admissions without an SDOH Z-code, admissions with them were for patients who were younger, more often male, Medicaid recipients or uninsured. A higher proportion of admissions with SDOH Z-codes were for mental health (44.0% versus 3.3%, p<0.001) and alcohol and substance use disorders (9.6% versus 1.1%, p<0.001) compared to those without.
Conclusions:
The uptake of SDOH Z-codes has been slow, and current coding is likely poorly reflective of the actual burden of social needs experienced by hospitalized patients.
Keywords: Z-codes, social determinants of health, ICD-10, social factors
Introduction
Social determinants of health (SDOH) are defined by the World Health Organization as the conditions in which people are born, grow, work, live, and age, as well as the broader forces and systems that shape these conditions.1 There has been growing interest in and research on the considerable impact of social factors on health risks and outcomes.2,3 Social determinants of health and related factors outside of clinical care have been found to account for over 60-80% of health outcomes2,3 and are increasingly emphasized as a public health priority. For example, the Centers for Disease Prevention and Control’s (CDC) Healthy People 2020 report underscores the importance of SDOH by setting the objective to “create social and physical environments that promote good health for all” as one of the four overarching goals for the decade.3
One barrier to understanding the prevalence and influence of SDOH has been a lack of standardized national data linked to health encounters. The tenth revision of the International Classification of Diseases (ICD-10) includes a new set of “Z-codes” to describe factors influencing health status and contact with the health system. A subset of the Z-codes, released in quarter four of 2015, addresses SDOH (Z55-Z65). The availability of SDOH Z-codes may offer an opportunity to elucidate the impact of these social factors more broadly than has been feasible in studies depending on in-person collection of specific SDOH data, for example on housing status, social support, or employment.
Despite their potential, utilization of these new codes is sparse. An initial study using Medicare data showed that Z-codes were coded in less than 1% of Medicare Fee-for-Service patients in 2017, and a report from the Missouri Hospital Association showed that such codes were used with increasing frequency in 2016 and 2017.4,5 However, to our knowledge, there has been no examination of the utilization of SDOH Z-codes and the characteristics of hospitals that use them on a national all-payer level, including data on uninsured individuals and those receiving Medicaid, who have a high prevalence of social risk factors.4
Therefore, our study had three objectives: (1) to quantify utilization of SDOH-Z codes during the 2 initial full years of their availability (2016-2017); (2) to compare characteristics of hospitals that utilized versus those that did not utilize SDOH-Z codes; and (3) to compare attributes of patients whose hospital admission record included SDOH-Z codes relative to those that did not.
Methods
Conceptual Framework
A theory that has been widely applied in the context of healthcare technology,6-8 called the “diffusion of innovation” theory, sets up a framework for the analysis of the early usage of SDOH Z-codes and accompanying data. Defined by Everett Rogers in his book Diffusion of Innovations in 1962, the process of diffusion of innovation can be divided into five successive stages characterized by the groups that successively adopt the new technology: innovators, early adopters, early majority, late majority, and laggards.9 We aimed to examine uptake across hospitals nationally with this framework in mind.
Data
We utilized data from the 2016 and 2017 National Inpatient Sample (NIS) from the Healthcare Cost and Utilization Project (HCUP) Database. The NIS is the largest publicly available all-payer inpatient care database in the United States, containing data on hospital inpatient stays and discharges across all payer types, including Medicare, Medicaid, and private payers, as well as uninsured patients. It is a roughly 20% sample of all admissions from HCUP-participating hospitals, and amounts to approximately 7 million unweighted hospital stays per year.10 The 2016 and 2017 releases of the NIS include full 2016 and 2017 calendar year diagnosis and procedure codes data and was reported using ICD-10-CM. Hospitalizations missing a gender variable were excluded (n=5,140, or 0.036%).
Social determinant Z-codes
The primary variable of interest was the coding of a Z-code indicative of SDOH, specifically ICD-10 codes Z55 through Z65. These codes are used to characterize socioeconomic and psychosocial situations that could have an impact on health and outcomes. Such codes describe problems in education, unemployment, occupational risk exposure, housing, social environment, upbringing, primary support group, and other psychosocial situations.11 Detailed descriptions can be found in Supplemental Digital Content 1 (see Table of ICD-10 Z-Code Utilization).
Analyses
To evaluate the utilization of SDOH Z-codes in 2016 and 2017, we first calculated the average percent of discharges with SDOH Z-codes overall and as a weighted average of admissions at each hospital across each month of 2016 and 2017. Because the adoption of SDOH Z-codes at the hospital level appeared linear, we used linear regression to test for a change over time, using month as the predictor and the percent of hospitalizations with at least one SDOH Z code at the hospital level as the outcome. We also plotted the cumulative proportion of hospitals that used at least one Z-code by month over the study period.
Next, we characterized hospital characteristics of hospitals that used at least one SDOH Z-code by the end of 2017 versus non-adopter hospitals that did not. We examined hospital characteristics, including average total annual volume of admissions, hospital teaching status, urban-rural location, U.S. Census Bureau census division, hospital size, hospital ownership, hospital teaching status, hospital primary payer mix, and hospital patient population racial demographics. We used chi-square and t-tests to compare hospitals that had versus had not adopted SDOH Z-codes.
We then compared hospitalizations with an SDOH Z-code to those without Z-codes. We first calculated the overall presence of SDOH Z-codes, as well as the prevalence of each specific code Z55-Z65. We then quantified patient characteristics such as age, gender, race, insurance status, median zip code income, admission status, and Elixhauser comorbidities associated with each hospitalization, based on prior studies showing that SDOH are more prevalent among minorities, uninsured individuals, and low-income individuals, as well as those with a higher burden of medical and mental health comorbidities.3,12,13 We used logistic regression to determine which characteristics were statistically significantly associated with a higher odds of SDOH Z-codes, using hierarchical modeling accounting for clustering of hospitalizations within hospitals.
Finally, to further characterize hospitalizations with and without SDOH Z-codes in terms of the primary reason for hospitalization, we also determined the ten most common major diagnostic categories (MDCs) associated with admissions with and without an SDOH Z-code.
All analyses were conducted using Stata/IC version 15.1, StataCorp, College Station, TX. We considered a two-tailed p-value of less than 0.05 to be statistically significant. This project was determined to be non-human-subjects research due to the de-identified nature of the data by the Human Research Protection Office at Washington University in St. Louis.
Results
Utilization of SDOH Z-codes over Time
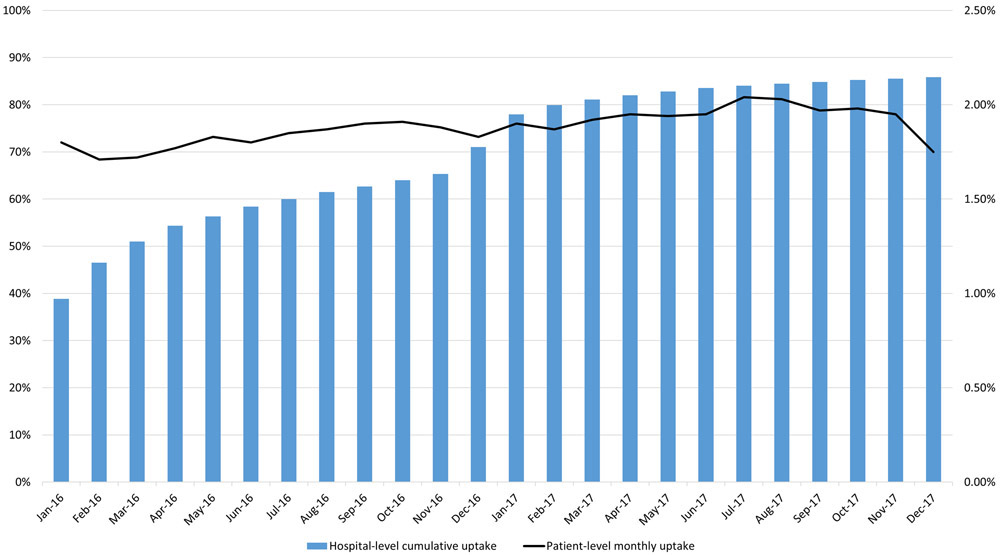
Out of 14,289,644 admissions in the 2016 and 2017 National Inpatient Sample (NIS), 269,929 (1.9%) had an associated SDOH Z-code (see Table, Supplemental Digital Content 1, which shows a more granular breakdown of SDOH Z-codes). The most common broad SDOH Z-code categories used were Z59 (“Problems related to housing and economic circumstances”), Z62 (“Problems related to upbringing”), Z63 (“Other problems related to primary support group, including family circumstances”), Z56 (“Problems related to employment and unemployment”), and Z60 (“Problems related to social environment”) (Figure 1). There were 320,874 unique SDOH Z-codes, demonstrating that some hospitalizations had more than one such Z-code applied, though the majority of hospitalizations (226,741, or 84.0%) had only one (see Table, Supplemental Digital Content 2, which shows the SDOH Z-codes per patient). The proportion of hospitalizations with at least one SDOH Z-code increased from 2016 to 2017, increasing on average 0.01% monthly (p<0.001) (Figure 2).
Figure 1. Distribution of SDOH Z-Codes.
SDOH=social determinants of health
Figure 2. Uptake of SDOH Z-Codes at the Hospital and Admission Level.
Left axis and bars represent the cumulative proportion of hospitals that coded at least one SDOH Z-code, by month. Right axis and line represent the monthly percent of hospitalizations (patient-level) that had at least one SDOH Z-code applied to their admission. Average monthly change was 0.01%, p<0.001. SDOH=social determinants of health.
Hospital Characteristics
The cumulative number and proportion of hospitals that had ever used an SDOH Z-code increased across the study period, from 1,895 hospitals (39%) in January 2016 to 4,190 hospitals (86%) in December 2017 (Figure 2). Compared to hospitals that did not use SDOH Z-codes, hospitals that did were more likely to be large, private not-for-profit, urban teaching hospitals (Table 1). There was also significant geographic variability in the likelihood of coding at least one SDOH Z-code, with the South Atlantic, Pacific, and Mid-Atlantic regions over-represented in the group of hospitals that had coded at least one SDOH Z-code.
Table 1.
Characteristics of Hospitals with versus without SDOH Z-Code Use
| Characteristic | Hospitals With SDOH Z-code Use N = 4,190 (85.9%) |
Hospitals Without SDOH Z-code Use N = 690 (14.1%) |
p-value |
|---|---|---|---|
| Hospital Size | <0.001 | ||
| Large | 26.4% | 7.0% | |
| Medium | 27.0% | 8.3% | |
| Small | 46.6% | 84.8% | |
| Hospital Ownership | <0.001 | ||
| Private, not-for-profit (voluntary) | 66.4% | 46.8% | |
| Government, nonfederal (public) | 17.0% | 35.5% | |
| Private, investor owned (proprietary) | 16.7% | 17.7% | |
| Hospital Teaching status and location | <0.001 | ||
| Urban - Teaching hospital | 37.8% | 6.2% | |
| Urban – Non-teaching hospital | 29.0% | 28.6% | |
| Rural | 33.2% | 65.2% | |
| U.S Census Bureau Census Divisions | <0.001 | ||
| Division 5: South Atlantic | 16.5% | 5.1% | |
| Division 9: Pacific | 12.6% | 1.5% | |
| Division 2: Mid-Atlantic | 10.4% | 2.2% | |
| Division 3: East North Central | 16.2% | 10.6% | |
| Division 8: Mountain | 8.0% | 7.5% | |
| Division 4: West North Central | 10.7% | 33.9% | |
| Division 7: West South Central | 14.5% | 26.5% | |
| Division 1: New England | 4.0% | 1.0% | |
| Division 6: East South Central | 7.0% | 11.7% |
Hospitals with SDOH Z-codes were defined as having at least 1 SDOH Z-code used in the 2016 or 2017 National Inpatient Sample.
Division 1 = New England (ME, NH, VT, MA, RI, CT); Division 2 = Mid-Atlantic (NY, PA, NJ); Division 3 = East North Central (WI, MI, IL, ID, OH) ; Division 4 = West North Central (MO, ND, SD, NE, KS, MN, IA); Division 5 = South Atlantic (DE, MD, DC, VA, WV, NC, SC, GA, FL) ; Division 6 = East South Central (KY, TN, MS, AL); Division 7 = West South Central (OK, TX, AK, LA); Division 8 = Mountain (ID, MT, WY, NV, UT, CO, AZ, NM); Division 9 = Pacific (AK, WA, OR, CA, HI)
Patient-Level Predictors of SDOH Z-Codes
There were also striking differences in the likelihood of having an SDOH Z-code applied across patient characteristics. Hospitalizations for children and older adults had lower odds of having at least one SDOH Z-code compared to hospitalizations for patients 18-34 years old (under 18 adjusted odds ratio (aOR) 0.45, 95% confidence interval [CI] [0.45-0.46]; 75+: aOR 0.31 [0.30-0.32]) (Table 2). Hospitalizations for women had lower odds of having at least one SDOH Z-code compared with hospitalizations for men (aOR 0.64 [0.63-0.65]). While hospitalizations for Black patients had higher unadjusted odds of an SDOH Z-code, this association was no longer significant after adjustment for the other factors examined. However, hospitalizations for Hispanic patients and patients of other or unknown race had lower odds of SDOH Z-codes compared to hospitalizations for white patients (Hispanic: aOR 0.59 [0.58-0.60], other/unknown race: aOR 0.78 [0.76-0.79]). Compared to hospitalizations for privately insured patients, hospitalizations for patients with all other insurance types including Medicare (aOR 1.96 [1.93-1.99]), Medicaid (aOR 2.74 [2.70-2.77]), self-pay/uninsured (aOR 2.91 [2.86-2.96]), no-charge (aOR 3.78 [3.62-3.95]), and other/missing (aOR 2.22 [2.17-2.27]) had higher odds of having an SDOH Z-code. Hospitalizations for patients missing information on ZIP code income also had higher odds of having an SDOH Z-code compared to hospitalizations with patients from the highest ZIP income quartile (aOR 4.91 [4.81-5.01]).
Table 2.
Characteristics of Admissions with versus without an SDOH Z-code
| Characteristic | With SDOH Z- code N = 269,929 (1.9%) |
Without SDOH Z- code N = 14,019,715 (98.1%) |
p-value | Odds Ratio | Lower 95% CI |
Upper 95% CI |
Adjusted Odds Ratio* |
Lower 95% CI |
Upper 95% CI |
|---|---|---|---|---|---|---|---|---|---|
| Age | < 0.001 | ||||||||
| 0-17 | 9.2% | 15.3% | 0.38 | 0.38 | 0.39 | 0.45 | 0.45 | 0.46 | |
| 18-34 | 25.3% | 16.0% | Ref | Ref | Ref | Ref | Ref | Ref | |
| 35-44 | 15.8% | 7.8% | 1.28 | 1.27 | 1.30 | 1.12 | 1.11 | 1.14 | |
| 45-54 | 20.0% | 9.8% | 1.30 | 1.28 | 1.31 | 1.12 | 1.10 | 1.13 | |
| 55-64 | 16.8% | 14.5% | 0.73 | 0.73 | 0.74 | 0.80 | 0.79 | 0.81 | |
| 65-74 | 6.8% | 15.8% | 0.27 | 0.27 | 0.28 | 0.39 | 0.38 | 0.39 | |
| 75+ | 6.1% | 20.8% | 0.19 | 0.18 | 0.19 | 0.31 | 0.30 | 0.32 | |
| Female | 42.1% | 56.8% | < 0.001 | 0.55 | 0.55 | 0.56 | 0.64 | 0.63 | 0.65 |
| Race | < 0.001 | ||||||||
| White | 59.0% | 62.1% | Ref | Ref | Ref | Ref | Ref | Ref | |
| Black | 20.0% | 14.4% | 1.46 | 1.44 | 1.47 | 0.99 | 0.98 | 1.00 | |
| Hispanic | 10.1% | 11.8% | 0.90 | 0.89 | 0.91 | 0.59 | 0.58 | 0.60 | |
| Other/Unknown | 10.9% | 11.6% | 0.99 | 0.98 | 1.00 | 0.78 | 0.76 | 0.79 | |
| Insurance | < 0.001 | ||||||||
| Medicare | 24.2% | 40.4% | 1.14 | 1.12 | 1.15 | 1.96 | 1.93 | 1.99 | |
| Medicaid | 45.4% | 22.7% | 3.80 | 3.76 | 3.84 | 2.74 | 2.70 | 2.77 | |
| Private Insurance | 15.7% | 29.9% | Ref | Ref | Ref | Ref | Ref | Ref | |
| Self-Pay/Uninsured | 9.0% | 3.8% | 4.54 | 4.47 | 4.61 | 2.91 | 2.86 | 2.96 | |
| No-Charge | 1.1% | 0.3% | 7.23 | 6.96 | 7.52 | 3.78 | 3.62 | 3.95 | |
| Other/Missing | 4.6% | 3.0% | 2.92 | 2.86 | 2.98 | 2.22 | 2.17 | 2.27 | |
| Median Household Incomea | < 0.001 | ||||||||
| Q1: $1 - 42,999 | 34.7% | 29.9% | 1.63 | 1.61 | 1.65 | 1.19 | 1.17 | 1.20 | |
| Q2: $43,000 - 53,999 | 23.3% | 25.6% | 1.28 | 1.27 | 1.30 | 1.03 | 1.02 | 1.05 | |
| Q3: $54,000 - 70,999 | 19.3% | 23.4% | 1.16 | 1.14 | 1.17 | 1.00 | 0.99 | 1.02 | |
| Q4: $71,000+ | 14.0% | 19.6% | Ref | Ref | Ref | Ref | Ref | Ref | |
| Missing | 8.8% | 1.5% | 8.09 | 7.96 | 8.23 | 4.91 | 4.81 | 5.01 |
SDOH = social determinants of health; Q1 = 1st quartile; Q2 = 2nd quartile; Q3 = 3rd quartile; Q4 = 4th quartile
Median Household Income of the patient’s reported home ZIP code
Odds ratio of having an SDOH Z-code applied to hospitalization.
Model adjusted for all variables listed in the table as well as age, gender, and clinical comorbidities
The hospitalizations with SDOH Z-codes were for a distinctly different set of major diagnostic categories (MDCs) than for hospitalizations without an SDOH Z-code. Out of the top 10 most common MDCs in hospitalizations with an SDOH Z-code, hospitalizations with an SDOH Z-code had markedly higher rates of MDC 19 (“Mental Diseases and Disorders”, 44.0% of hospitalizations versus 3.3%, p<0.001), MDC 20 (“Alcohol/Drug Use & Alcohol/Drug Induced Organic Mental Disorders”, 9.6% versus 1.1%, p<0.001), and MDC 21 (“Injuries, Poisonings & Toxic Effects of Drugs”, 3.4% versus 1.5%, p<0.001) than hospitalizations without an SDOH Z-code (Figure 3 and see Table, Supplemental Digital Content 3, which shows the most common MDCs in SDOH Z-Code patients).
Figure 3. Most Common Major Diagnostic Categories in Hospitalizations With versus Without an SDOH Z-Code.
MDC=major diagnostic category; SDOH=social determinants of health; lnjuries, Poisonings & Toxic Effects of Drugs: MDC 21; Musculoskeletal and Dermatological Disorders: MDC 8 = Diseases & Disorders of the Musculoskeletal System & Connective Tissue; MDC 9 = Diseases & Disorders of the Skin, Subcutaneous Tissue & Breast; Medical Disorders: MDC 5 = Diseases & Disorders of the Circulatory System; MDC 4 = Diseases & Disorders of the Respiratory System; MDC 18 = Infectious & Parasitic Diseases, Systemic or Unspecified Sites; MDC 1 = Diseases & Disorders of the Nervous System; MDC 10 = Diseases & Disorders of the Endocrine, Nutritional & Metabolic System; Alcohol/Drug Use & Alcohol/Drug Induced Organic Mental Disorders: MDC 20; Mental Diseases & Disorders: MDC 19;
Discussion
There is growing consensus that data on social determinants of health are crucial to the overall goal of improving population health. Defined in 2003 as the “health outcomes of a group of individuals, including the distribution of such outcomes within the group,”14 population health is critical as payers and systems take responsibility for groups of patients, are held liable for patients’ health status, and/or are reimbursed on a per-capita basis. If SDOH were reliably and broadly collected, these data could be used for population health efforts.15-17 In 2016, the Centers for Medicare & Medicaid Services (CMS) launched the Accountable Health Communities Model, based on evidence that addressing unmet health-related social needs through enhanced clinical-community linkages can improve outcomes and reduce costs.18,19 Thirty organizations are currently participating in the model, which incorporates an SDOH screening tool, social service referral networks, community service navigation assistance, and encouragement of clinical-community alignment to ensure services are available and appropriately responsive to community needs.19
Efforts to use SDOH Z-codes to drive interventions have also taken place at the payer and provider levels. For example, nonprofits and payers have released claim coding tools and education campaigns to promote SDOH coding among providers.20-22 Providers and health systems across the country have started to cross-walk the codes against their care models.23,24 Large hospital and physician groups like the American Hospital Association and the American Medical Association have offered webinars25 and started collaborations26 with payers to optimize uptake of SDOH Z-codes. Kaiser Permanente Northwest, an integrated health care delivery system, recently incorporated the use of SDOH Z-codes into their care model, in an effort to use standardized SDOH data to target specific community resources and process changes to meet identified patient needs.27 3M Corporation—a leader in health data analysis—is considering developing a composite SDOH score that includes the new Z-codes.28
Despite these potential benefits, our findings suggest that SDOH Z-codes are being vastly underutilized at the patient level, given that prior studies examining social risk factors in hospitalized patients show the prevalence of issues like poverty and unstable housing to be much higher than 1.8%.29 One possibility for why Z-codes are not being used widely is that non-adopter clinicians do not know how and when to code them. The CDC released preliminary guidelines for coding SDOH Z-codes in 2016,30 but there was confusion among healthcare providers over whether social factors needed to be explicitly be documented by a physician in order to be coded. The particular questions that the Z-codes are designed to capture have been the domain of social work in many settings, and clinicians are generally not specifically trained to do comprehensive SDOH assessments. While clarification in early 2018 suggested that these codes can be documented by any clinician involved in patient care,31 it is possible that confusion remains. Certain physicians or types of physicians may also be more attuned to coding SDOH Z-codes, which may explain why hospital-level uptake of these codes is high, but the patient-level uptake remains low. Another reason for the lack of greater use of Z-codes in non-adopters may be that no current national financial incentives exist to code SDOH Z-codes. They are not included in risk adjustment models for hospital performance evaluation or federal value-based payment programs, and therefore may not be the focus of documentation improvement efforts by billing departments and coding experts to the degree that clinical comorbidities have been.
Some have suggested that rich SDOH data may already exist in electronic health records (EHRs), and be an alternative way to access this information. However, EHR SDOH data are typically unstructured (i.e. recorded as unrestricted text rather than binary fields) and may be computationally difficult to mine in their current form. Documentation of SDOH and patient social histories is in most cases non-standardized and may vary significantly based on provider type and individual style. SDOH Z-codes could serve as a way to standardize documentation and allow for intervention at the population health level, or even more broadly for tracking and resource allocation by public health officials or policymakers.
There are limitations to this study. First, we used administrative data. While the NIS is considered nationally representative, not all hospitals participate and our findings may not generalize to specialty hospitals, psychiatric hospitals, and other facilities under-represented in this dataset. Second, we had limited information on hospitals’ identities, and could therefore not determine which hospitals participated in alternative payment models or other population health efforts. Third, we did not have information on clinician identity or type and could not determine if certain clinicians or certain types of clinicians were more likely to code SDOH Z-codes. The fact that the majority of hospitals adopted SDOH Z-codes relatively quickly, but the overall uptake remained quite low, suggests that clinicians and not hospitals may be the more relevant entity to study with regards to diffusion of innovation theory. Fourth, we had limited geographic data because HCUP does not report county or state-level data to ensure that data are not identifiable. Future work using geographically identified data could shed additional light on how state or local policies are associated with SDOH Z-code uptake. Finally, because of data limitations in the NIS, we cannot track patients longitudinally, and therefore are unable to determine whether the SDOH Z-codes are associated with long-term health outcomes such as readmission, long-term mortality, or health spending.
Conclusions
Social determinants of health ICD-10 Z-codes were underutilized in 2016 and 2017, and coding is likely under-representative of the true burden of social risk in hospitalized patients. Increasing the utilization of Z-codes on a national level has potential for improving both the measurement of SDOH and for facilitating the development of programs aimed at addressing them.
Supplementary Material
Supplemental Digital Content 1. Social Determinants of Health ICD-10 Z-Code Utilization in the 2016 and 2017 CY National Inpatient Sample .doc
Supplemental Digital Content 2. SDOH Z-Codes Per Patient .doc
Supplemental Digital Content 3. Most Common MDCs in SDOH Z-Code Patients .doc
Acknowledgments
Financial Disclosures / Conflicts of Interest: Dr. Joynt Maddox receives research support from the National Heart, Lung, and Blood Institute (R01HL143421), National Institute on Aging (R01AG060935), and Commonwealth Fund, and previously did contract work for the US Department of Health and Human Services. Dr. Gmerice Hammond is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award number T32HL007081. Dr. Wadhera receives research support from the National Heart, Lung, and Blood Institute (K23HL148525-1). The other authors report no conflicts.
Funding Source: NIH #5T35HL007815. The funders played no role in the design or execution of the study, nor in the decision to submit it for publication.
References
- 1.World Health Organization. Social determinants of health. World Health Organization. 2018. Available at: https://www.who.int/social_determinants/en/. Accessed August 15, 2019.
- 2.Hood CM, Gennuso KP, Swain GR, Catlin BB. County Health Rankings: Relationships Between Determinant Factors and Health Outcomes. Am J Prev Med. 2016;50(2):129–135. [DOI] [PubMed] [Google Scholar]
- 3.Office of Disease Prevention and Health Promotion, Centers for Disease Control and Prevention. Social Determinants of Health ∣ Healthy People 2020. 2019. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. Accessed August 15, 2019.
- 4.Weeks WB, Cao SY, Lester CM, Weinstein JN, Morden NE. Use of Z-Codes to Record Social Determinants of Health Among Fee-for-service Medicare Beneficiaries in 2017. Journal of general internal medicine. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reidhead M Decoding Social Determinants of Health. Jefferson City, MO: Missouri Hospital Association;2018. [Google Scholar]
- 6.Dandu N, Zmistowski B, Chen AF, Chapman T, Howley M. How are Electronic Health Records Associated with Provider Productivity and Billing in Orthopaedic Surgery? Clin Orthop Relat Res. 2019;477(11):2443–2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jung HY, Unruh MA, Kaushal R, Vest JR. Growth Of New York Physician Participation In Meaningful Use Of Electronic Health Records Was Variable, 2011–12. Health Aff (Millwood). 2015;34(6):1035–1043. [DOI] [PubMed] [Google Scholar]
- 8.McCoy AB, Wright A, Eysenbach G, et al. State of the art in clinical informatics: evidence and examples. Yearb Med Inform. 2013;8:13–19. [PubMed] [Google Scholar]
- 9.Rogers EM. Diffusion of Innovations, 5th Edition. 5 ed: Simon and Schuster; 2003. [Google Scholar]
- 10.Healthcare Cost and Utilization Project (HCUP). HCUP-US NIS Overview. 2019. Available at: https://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed August 15, 2019.
- 11.American Hospital Association. ICD-10-CM Coding for Social Determinants of Health Washington, DC: 2018. [Google Scholar]
- 12.Lewis VA, Joynt Maddox KE, Gottlieb DJ, Bynum JPW. Developing and Validating a Measure to Predict Poverty in Medicare Administrative Data AcademyHealth Annual Research Meeting; 2018; Seattle, WA. [Google Scholar]
- 13.Johnston KJ, Wen H, Schootman M, Joynt Maddox KE. Association of Patient Social, Cognitive, and Functional Risk Factors with Preventable Hospitalizations: Implications for Physician Value-Based Payment. J Gen Intern Med. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kindig D, Stoddart G. What Is Population Health? American Journal of Public Health. 2003;93(3):380–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chaiyachati KH GD, Aysola J. Health Systems Tackling Social Determinants of Health: Promises, Pitfalls, and Opportunities of Current Policies. 2019. [PubMed] [Google Scholar]
- 16.Machledt D Addressing the Social Determinants of Health Through Medicaid Managed Care. Issue Brief (Commonw Fund);2017. 1558–6847. [PubMed] [Google Scholar]
- 17.Foundation RWJ. Medicaid’s Role in Addressing Social Determinants of Health. 2019.
- 18.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable Health Communities — Addressing Social Needs through Medicare and Medicaid. New England Journal of Medicine. 2016;374(1):8–11. [DOI] [PubMed] [Google Scholar]
- 19.Center for Medicare & Medicaid Innovation. Accountable Health Communities Model ∣ Center for Medicare & Medicaid Innovation. Centers for Medicare and Medicaid Services. 2019. Available at: https://innovation.cms.gov/initiatives/ahcm/. Accessed August 15, 2019. [Google Scholar]
- 20.eHealth Initiative. eHI Releases Tools Promoting the USe of ICD-10-CM Z Codes for Social Determinants of Health Data. 2019. Available at: https://www.ehidc.org/articles/ehi-releases-tools-promoting-use-icd-10-cm-z-codes-social-determinants-health-data. Accessed August 15, 2019..
- 21.Daniel-Robinson L, Moore JE. Innovation and Opportunities to Address Social Determinants of Health in Medicaid Managed Care. Institute for Medicaid Innovation;2019. [Google Scholar]
- 22.Louisiana Healthcare Connections. SDOH Center of Excellence to support providers in addressing social determinants of health. 2019. Available at: https://www.louisianahealthconnect.com/newsroom/sdoh-center-of-excellence-to-support-providers-in-addressing-sdo.html. Accessed August 15, 2019.
- 23.Schulman M, Thomas-Henkel C. Opportunities for Complex Care Programs to Address the Social Determinants of Health. Center for Health Care Strategies;2019. [Google Scholar]
- 24.Olson DP, Oldfield BJ, Navarro SM. Standardizing Social Determinants of Health Assessments. Health Affairs. 2019. Available at: https://www.healthaffairs.org/do/10.1377/hblog20190311.823116/full/. Accessed August 15, 2019. [Google Scholar]
- 25.American Hospital Association. ICD-10-CM Codes for the Social Determinants of Health. 2020. Available at: https://events-na12.adobeconnect.com/content/connect/c1/1295154209/en/events/event/shared/2638441025/event_landing.html?sco-id=2638597042&campaign-id=Partner. Accessed March 20, 2020
- 26.United Healthcare. UnitedHealthcare and the AMA Collaborate to Understand and Address Social Barriers Preventing People’s Access to Better Health. 2019. Available at: https://newsroom.uhc.com/content/uhc/newsroom/news-releases/AMA-announcement.html. Accessed March 20, 2020.
- 27.Friedman NL, Banegas MP. Toward Addressing Social Determinants of Health: A Health Care System Strategy. Perm J. 2018;22:18–095. [Google Scholar]
- 28.LaBrec PA, Butterfield R, 3M Corporation. The Development and Application of a Composite Score for Social Determinants of Health. [Google Scholar]
- 29.Joynt Maddox KE, Reidhead M, Hu J, et al. Adjusting for social risk factors impacts performance and penalties in the hospital readmissions reduction program. Health services research. 2019;54(2):327–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Medicare and Medicaid Services. ICD-10-CM Official Guidelines for Coding and Reporting, FY 2016. Baltimore, MD: 2016. [Google Scholar]
- 31.Center for Medicare and Medicaid Services. ICD-10-CM Official Guidelines for Coding and Reporting, FY 2018. Baltimore, MD: 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1. Social Determinants of Health ICD-10 Z-Code Utilization in the 2016 and 2017 CY National Inpatient Sample .doc
Supplemental Digital Content 2. SDOH Z-Codes Per Patient .doc
Supplemental Digital Content 3. Most Common MDCs in SDOH Z-Code Patients .doc