Abstract
In regions such as India, where one-to-one behavior-analytic intervention is not easily accessible, parents and service providers may advocate for children with disabilities better if they have foundational training in behavioral approaches to problem behavior. The purpose of this study was to evaluate a culturally adapted training delivered in an underresourced region of India. Ten parents and professionals from Chennai completed the training, and the researchers evaluated its effects using a multiple-baseline design. Participants showed improvements in correct responses on a structured form designed to capture skills involved in function-based assessment and intervention, as well as the fidelity of implementation of extinction and functional communication training. Moreover, participants rated the acceptability of training highly on measures of social validity. Guidelines for the education of parents and service providers in underresourced areas outside of the United States are discussed.
Electronic supplementary material
The online version of this article (10.1007/s40617-020-00489-w) contains supplementary material, which is available to authorized users.
Keywords: Cultural adaptations, Function-based treatment, India, Problem behavior, Training manual
For decades, addressing the problem behavior of individuals with developmental disabilities has involved a functional approach to assessment and treatment (Hanley, Iwata, & McCord, 2003; Horner, 1994; Iwata et al., 1994). Function-based procedures have been replicated, extended, and discussed across hundreds of studies and have strong empirical support. However, most research on their efficacy and adoption has been developed and conducted in North American settings (e.g., Special Issue on Functional Analysis, 2013). Given the differential outcomes of behavioral interventions across varied ethnic or demographic characteristics (Artiles & Trent, 1994; Sugai, O’Keeffe, & Fallon, 2012), a careful examination of culture is crucial to our implementation of and training on the functional approach to problem behavior worldwide. To maximize the outcomes and generality of these practices across populations (Baer, Wolf, & Risley, 1968), research must be conducted cross-culturally and cross-linguistically.
The prevalence of autism spectrum disorder (ASD) in South Asia is estimated at 1 in 93 children (Hossain et al., 2017) and that of intellectual disabilities in India has been quoted at 1% (McKenzie, Milton, Smith, & Ouelette-Kuntz, 2016). Further, problem behavior (e.g., aggression, disruption, self-injury) is commonly associated with ASD and other neurodevelopmental disorders (Brown, Brown, & Dibiasio, 2013; Horner, Carr, Strain, Todd, & Reed, 2002). To our knowledge, no studies have tested the effectiveness of function-based behavioral interventions in treating problem behavior in children with developmental disabilities in South Asian populations, particularly in India. Martin, Nosik, and Carr (2016) quantified the relative paucity of research published in the Journal of Applied Behavior Analysis from anywhere outside of the United States and noted several potential barriers to publication. We posit that there may be many barriers not only to publication, but also to application, of behavior-analytic assessment and intervention in countries like India.
Primarily, there is a wide gap between the number of children receiving these diagnoses and the availability of specialized one-to-one behavior-analytic intervention in this region. According to the BACB Registry, only 13 individuals residing in India are BCaBAs, 24 are BCBAs, and 3 are BCBA-Ds (BACB, 2020). Thus, this region is represented by only 0.6% of BCBAs worldwide, whereas India represents about 18% of the world’s population. The limited number of specialists in this area and lack of publicly funded services hinder accessibility to this type of individualized treatment. One way to bridge the gap is to provide parents and service providers working with such populations with educational opportunities that allow them to address some of the challenges they encounter and to seek consultations appropriately for those they cannot address alone. Training parents and practitioners to be behavior-change agents is a well-researched intervention that is cost-effective and also contributes to the child’s progress (Hamad, Serna, Morrison, & Fleming, 2010; Ingersoll & Berger, 2015; Salomone et al., 2019).
There is a range of practices commonly used to address problem behavior in children with developmental disabilities in India, including pharmacological interventions (Kaur & Roy, 2017; Nagaraj, Singhi, & Malhi, 2006); treatments such as Ayurveda, homeopathy, pranic healing, and reflexology (Daley, 2002); sensory integration (Kaur & Roy, 2017; Sengupta, Lobo, & Krishnamurthy, 2017); and speech-language pathology (e.g., Kaur & Roy, 2017). Treatments for problem behavior typically involve a combination of two or more of these interventions delivered by independent private practitioners. For example, in a sample consisting of 109 urban families in India, over 75% had used medication and more than 50% had used either Ayurveda, or homeopathy, or both for the treatment of symptoms associated with ASD (Daley, 2002). However, some of the practices are not considered evidence-based approaches according to recognized standards (e.g., National Autism Center, 2015), and there is a noticeable lack of reports of function-based intervention in research from this region. For these reasons, it seems imperative to expand the literature base on best practice for Indian children with ASD.
Two potential ways to increase the adoption of behavior-analytic and evidence-based practices include education and training. Many studies in the United States have established the efficacy of structured training and practice opportunities for parents and professionals (e.g., Mueller et al., 2003; Sarokoff & Sturmey, 2004; Schepis, Reid, Ownbey, & Parsons, 2001; Wallace, Doney, Mintz-Resudek, & Tarbox, 2004). Fewer studies exist on training parents and professionals internationally (see Antonsson, Graneheim, Isaksson, Åström, & Lundström, 2016, and Marleau, Lanovaz, Gendron, Higbee, & Morin, 2018, for examples). However, training individuals to adopt established, evidence-based treatment may receive unfavorable responses if the training or treatment itself lacks relevance to the cultural needs and preferences of a subgroup (Hall, Ibaraki, Huang, Marti, & Stice, 2016). The field of adapting behavior-analytic interventions to be culturally relevant is in its infancy (Fong, Catagnus, Brodhead, Quigley, & Field, 2016). Psychotherapy and cognitive-behavioral interventions have been adapted to specific cultural groups (e.g., Chinese Americans: Hwang, 2009; Haitian Americans: Nicolas, Arntz, Hirsch, & Schmiedigen, 2009; Latinos: Organista & Munoz, 1996; Pakistanis: Naeem, Waheed, Gobbi, Ayub, & Kingdon, 2011; Puerto Ricans: Malgady, Rogler, & Costantino, 1990). Although there is evidence that culture and context influence diagnosis and treatment, there is still considerable debate about how to adapt specific treatments. Bernal, Bonilla, and Bellido (1995) offered a framework that presents eight dimensions that can be the subject of culturally adapted interventions: (a) language of the intervention, (b) persons delivering the intervention, (c) metaphors or cultural expressions that might be used in the treatment, (d) content or cultural knowledge about the subgroup, (e) treatment concepts, (f) treatment goals, (g) method of treatment, and (h) context, which includes the social, economic, and political structure surrounding the person. Their framework has been used extensively to adapt psychological interventions (e.g., DeGarmo & Martinez, 2006; Grote et al., 2009; Kayrouz, Dear, Karin, Fogliati, & Titov, 2016).
The more problematic and less studied questions are regarding how to identify the required adaptations. Hwang (2016) offered a model that involves generating knowledge about a culture by collaborating with stakeholders, integrating the generated information with empirical evidence in cultural literature, and subsequently adapting and testing the intervention. Some cultural aspects of Asian populations include a goal-driven approach, special importance placed on family values and relationships, a high emphasis on education as a means for improvement, hierarchical traditions, a therapist/medical professional taking on a directive-expert role, expectations of a personal connection with the professionals one works with, occasional distrust toward outsiders, reverence for experts or experienced people, and social etiquette such as offering food as a means to build relationships (Hwang, 2006; Lee, 1997; Lin, 2002; Nakamura, 1964; Roland, 1988; Sinha, Sinha, Verma, & Sinha, 2001).
Previous research on child-rearing practices has indicated that Indian parents tended to be more controlling than Euro-American parents and emphasized achievement more (Sahithya, Manohari, & Vijaya, 2019). It was also found that adults in India do not create learning situations for their children; rather, children have the responsibility to learn culturally valued behaviors and social norms by observing adults (Sharma, 1999). In a survey of 30 families in New Delhi, it was found that mothers believed that the behavior of a child must be person and context sensitive, and the child’s food and conduct were the most central concerns for the family (Tuli, 2012). Extended family members lived together and often helped in child-rearing. However, rapidly changing trends in the social milieu, economic heterogeneity, and diversity in the country advise against overgeneralizations.
The current gaps in research on adapting and applying behavior-analytic training outside of the United States are even more relevant given the BACB’s® recent decision to shift its international focus from a single global certificate to local, country-specific standards (BACB, 2019). Given the clear need for wider adoption of behavior analysis in India, we assessed the efficacy and social validity of a culturally adapted function-based behavioral assessment and interventions (FBAI) training program to support parents and professionals to address problem behavior in children with a developmental disability. Participants included lower resourced families who often experience barriers to access to care. We developed and manualized the training to include several relevant cultural adaptations using the models proposed by Bernal et al. (1995) and Hwang (2016).
Method
Participants and Setting
Ten individuals participated in our study: Swathi, Ishwari, Akhila, Madhu, Naureen, Bhanu, Lakshmi, Divya, Symi, and Rithika are pseudonyms. The participants were parents of children with a developmental disability (e.g., ASD, attention-deficit/hyperactivity disorder) or professionals (speech therapists, occupational therapists, and special educators) in Chennai, India, whom we recruited using flyers at a pediatrician’s office. Participation in the training was free. All professionals who participated in the study worked with a child with developmental delays or disabilities at the commencement of the study. Table 1 lists the characteristics of the participants in our study. All participants completed the training in a conference room equipped with a projector screen and speakers.
Table 1.
Demographic Information on Study Participants
| n = 10 | % | ||
|---|---|---|---|
| Gender | Male | 0 | 0 |
| Female | 10 | 100 | |
| Degree | Doctoral | 0 | 0 |
| Master’s | 2 | 20 | |
| Bachelor’s | 6 | 60 | |
| High school | 2 | 20 | |
| Role | Parent | 6 | 60 |
| Spl. educator | 1 | 10 | |
| SLP | 2 | 20 | |
| OT | 1 | 10 | |
| Other | 0 | 0 | |
| Additional certifications | 3 | 30 | |
| Child Diagnosis | ASD | 10 | 47 |
| ADHD | 2 | 10 | |
| ADD | 3 | 13 | |
| Asperger’s syndrome | 2 | 10 | |
| Communication disorder | 2 | 10 | |
| LD | 0 | 0 | |
| GDD | 2 | 10 | |
| Other | 0 | 0 | |
| Language | English | 6 | 60 |
| Tamil | 4 | 40 | |
| Hindi | 0 | 0 | |
| Other | 0 | 0 | |
| Knowledge About FA | Yes, used | 0 | 0 |
| Yes, read | 1 | 10 | |
| No | 9 | 90 | |
| Professionals Consulted | Self | 0 | 0 |
| Psychologist | 3 | 14 | |
| Doctor | 4 | 18 | |
| OT | 6 | 27 | |
| SLP/vision | 3 | 14 | |
| Teacher | 4 | 18 | |
| ABA | 2 | 9 | |
| Other | 0 | 0 | |
|
Dev./ implemented BIP |
Yes | 1 | 10 |
| No | 9 | 90 |
Note. Spl. = special; SLP = speech-language pathologist; OT = occupational therapist; ADHD = attention-deficit/hyperactivity disorder; ADD = attention-deficit disorder; LD = learning disability; GDD = global developmental delay; FA = functional analysis; Dev. developed; BIP = behavior intervention plan
Materials
FBAI Training Manual
The manual included all content covered in the face-to-face training (discussed later), as well as additional, self-guided practice opportunities. The manual was composed of six modules that covered (a) the basics of behavior and its functions; (b) a task analysis for designing a function-based behavior intervention plan; (c) procedures to teach functionally equivalent alternative behaviors; (d) proactive and reactive strategies to handle problematic behaviors maintained by attention, escape, access to tangibles, and automatic reinforcement; (e) tips on data collection; and (f) caveats about handling dangerous behaviors and methods to locate and seek professional guidance from a certified behavior analyst. The manual also included a note on the use of punishment, highlighting its ill effects and the ethical concerns involved. The manual was accompanied by a workbook to practice antecedent-behavior-consequence (ABC) data collection, behavioral function identification, and techniques to teach alternative appropriate behaviors. The printed manual was 20 pages long, and each module was 2 to 4 pages (M = 2.8) long. The training manual is available by request from the first author to individuals interested in conducting training in Chennai.
Test Videos
We created nine distinct videos consisting of three brief scenes (i.e., 30–40 s) each based on prepared scripts depicting each of three common social functions (attention, escape, and tangible; Beavers, Iwata, & Lerman, 2013). In total, we developed and filmed 27 brief scenes to allow for multiple exemplars during training and novel exemplars during assessments. The scenes showed two adult individuals role-playing as a parent and a child in the home setting in a variety of situations (e.g., snack time at a table, play with an iPad, and study time at a table). Each video contained three bouts of problem behavior with various social antecedents and consequences. For example, in one of the videos that showed study time at a table, the social antecedent included a demand being delivered (i.e., “Open your notebook and write your homework.”). The two social consequences included escape from the demand (i.e., there was no follow-through for the child to complete the instruction) and gaining attention (i.e., the actor playing the parent says, “That’s a very bad way to behave.”). The same individual played the role of the target child in all the test videos.
Structured FBAI Forms
We also developed structured FBAI forms, similar to those used by Scott, Lerman, and Luck (2018). An example of a structured form is available in the Appendix. For every test video, the form included a place to (a) indicate the target behavior observed, (b) select the best operational definition, (c) identify the antecedents and consequences of each of the three instances of target behavior, (d) identify a potential function of problem behavior, and (e) choose a functionally equivalent replacement behavior. Each question was designed in a multiple-choice format with one or more correct answers, and each question had four options. We designed distractors based on incorrect responses to open-ended questions in a pilot study that included 46 participants with similar demographic characteristics. Participants answered each question by placing a check mark in boxes next to each option. We included the option “none” so that participants were not forced to select among the listed options. However, this was never programmed as a correct response in any of the test videos. Prior to the study, the first author and second author independently completed a structured form for each test video. We compared the forms, and the interrater reliability (items with agreement divided by total items on the form) was 99%, with one disagreement in the consequences of one of the test videos, which we resolved through a discussion.
Dependent Variables
Our first dependent variable was responses on the structured FBAI form and was intended to approximate the development of a written plan. After participants viewed occurrences of problem behavior on the videos described previously, they completed the form by correctly identifying the target behavior, operational definitions, antecedents and consequences of problem behavior, potential function, and functionally equivalent replacement behavior from among several answer options. We summarized the percentage correct on the form for each test video by summing the number of items correct, dividing by the total number of items, and multiplying by 100. The total number of items per form was 10 (with antecedent and consequence data scored separately for each video).
Our second dependent variable was the fidelity of participants’ implementation of two function-based interventions: extinction and functional communication training. We assessed this measure by reviewing videotaped role-plays and scoring participant responses as correct or incorrect according to a rubric adapted from that described by Suess et al. (2014). The rubric outlined the critical steps to implementation, which included presenting the antecedent, blocking problem behavior, withholding consequences for problem behavior, prompting and delivering consequences for alternative behavior, and providing praise for alternative behavior. Implementation fidelity was summarized by dividing the number of correct steps by the total steps and multiplying by 100.
The social acceptability of the training procedure was measured 2 weeks after the training using a modified version of the Treatment Acceptability Rating Form–Revised (Reimers & Wacker, 1992; Wacker et al., 1998). The modified form contained 12 items (see Table 2) scored on a 5-point Likert-type scale from 1 (strongly disagree) to 5 (strongly agree). Questions were related to the acceptability of the training, length of the manual, ease of use, and the relevance of the information provided.
Table 2.
Participant Responses on the Social Validity Questionnaire
| Items | Mean (M) | Range |
|---|---|---|
| I found this training to be an acceptable way to acquire the skills necessary to address my child’s problem behavior. | 4.8 | 4–5 |
| I believe that the face-to-face training and the manual will likely be effective in helping me identify the factors causing my child’s behavior. | 4.8 | 4–5 |
| I liked the face-to-face training. | 4.7 | 4–5 |
| I found it easy to read the training manual. | 4.4 | 3–5 |
| The examples and videos provided with the manual were relevant to my child’s problems. | 4.8 | 4–5 |
| I experienced difficulty understanding the concepts covered in the manual. | 1.8 | 1–2 |
| I found the manual too lengthy. | 1.8 | 1–2 |
| I believe it would be acceptable to use this training with people who do not have access to one-on-one ABA intervention. | 4.8 | 4–5 |
| I believe that my training is likely to result in a permanent improvement in my child’s challenging behavior. | 4.7 | 4–5 |
| Overall, I had a positive reaction to this training. | 4.8 | 4–5 |
| The training helped me familiarize myself with ABA principles. | 4.8 | 4–5 |
| I am considering getting myself certified as a behavior analyst (RBT/BCaBA/BCBA). | 3.4 | 3–4 |
Note. All items were scored on a Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). In all practitioner forms, the words “my child’s” were replaced with “my student’s.” RBT = Registered Behavior Technician; BCaBA = Board Certified Assistant Behavior Analyst; BCBA = Board Certified Behavior Analyst
Interobserver Agreement (IOA)
Two independent observers scored the structured forms and videotapes of role-plays on 30% of all measures. IOA for correct responses on the structured form was calculated by dividing the number of agreements between the two observers by the total number of responses and multiplying the quotient by 100. Mean IOA across participants was 100% for this measure. IOA for the fidelity of implementation during role-plays was calculated by dividing the number of agreements between the two observers by the total number of steps and multiplying the quotient by 100. Mean IOA across participants was 95.8% (range 87.5%–100%) for the fidelity of implementation.
Procedure
All participants completed surveys describing their demographic details prior to baseline. The first author conducted identical trainings three times based on participant availability. Six participants were available for the first training (Swathi, Ishwari, Akhila, Madhu, Naureen, and Bhanu), two for the second (Lakshmi and Divya), and two for the third (Symi and Rithika). Participants viewed test videos chosen in a random order during baseline and posttraining assessments.
Baseline
Participants in the first, second, and third trainings viewed three, five, and seven test videos immediately prior to the onset of training. Each test video was played once, and participants had 10 s to identify the target behavior and the operational definition on the structured form. After this, the video was played a second time, and after each instance of the target behavior and its programmed consequences, the screen turned black and the participants had 10 s to record the antecedents and consequences. After the third instance of the problem behavior, participants had 20 s to identify the potential function and choose a functionally equivalent replacement behavior.
Fidelity of implementation was measured after completing the structured form for each test video. For this measure, we instructed participants to split into groups, in which one participant acted as the child and one acted as the parent/professional. Participants alternated the roles until all participants assumed each role at least once. Participants in the first, second, and third trainings completed 8, 10, and 13 videotaped role-plays respectively. We randomly selected one of the participants in the first (Akhila) and second (Divya) trainings to complete one additional baseline measure of videotaped role-plays. The experimenter provided the general instruction to the “children” to repeatedly engage in the problem behavior as they had seen on the test video; the experimenter provided the general instruction to the parents/professionals to react to the problem behavior and attempt to teach the alternate behavior(s) selected on the form. Prior to the first role-play, the experimenter stated that “there are no right or wrong answers; we just want to see what you normally do in such a situation.”
Training
Baseline was followed immediately by a 5-hr face-to-face training session delivered by the first author. All participants received the FBAI manual prior to the commencement of the training and had access to it throughout the training. The first author also used a PowerPoint slide deck to emphasize certain content in the training. The training involved in vivo and video demonstrations of concepts covered in the FBAI training manual: collecting ABC data, hypothesizing behavioral function, identifying and teaching alternative behaviors, and implementing differential reinforcement procedures. We designed 20 unique situations consisting of antecedent, behavior, and consequence events (five each for attention, escape, tangible, and nonsocial functions) for role-plays during the training. The participants formed pairs and completed two randomly assigned situations to practice the skills demonstrated. Intermittently, the trainer provided praise, descriptive feedback, and model prompts following errors.
We informed participants about the page numbers (or module numbers) in the FBAI manual for each concept that was covered during the training and of the availability of additional information in the manual. We provided sample demonstrations using the ABC data collection sheets and FBAI forms provided in the manual, and asked participants to use them at home or in the clinic. However, the research team did not monitor the participants’ use of the manual outside of the study.
Posttraining
We conducted posttraining sessions in the same manner as baseline, immediately after the face-to-face training. Similar to baseline, all participants completed the structured forms for two to three new test videos and also taped three to five new role-plays.
Follow-up Data
Four participants submitted a video of their implementation of the trained procedures 3 weeks posttraining and with an actual client (i.e., a child with a disability). The participants received the same instructions as they had during the role-play with an adult actor. For each video, the experimenters scored their fidelity of implementation as a preliminary measure of maintenance and generalization.
Cultural Adaptations
To maximize participation, efficacy, and social validity, we made small adaptations to the training structure, content, and delivery. The specific adaptations we made are outlined in Table 3 based on the framework described by Bernal et al. (1995). For example, the manual and training were developed based on a collaboration between a U.S.-based researcher (the second author) with expertise in functional analysis and a research-practitioner (the first author) who had owned and operated a behavioral agency in Chennai, India, for several years prior to the study. The authors developed all written materials in English and then had them translated into Tamil (the language native to the region) by a professional translator. The first author, who is fluent in both English and Tamil, proofread all translated materials prior to the study. The trainer (the first author) was a BCBA who was matched in ethnicity with the participants. The purpose of the face-to-face training was, in part, to introduce the concepts covered in the manual and also to indicate that the new information was being provided by an “insider” matched in ethnicity and language with the participants and familiar to the professionals who delivered other interventions (e.g., speech therapy, occupational therapy) in the region. In addition, the individuals, location, and situations depicted in the videos were native to the Chennai region. These videos were filmed in local households with confederates matched in ethnicity to the participants.
Table 3.
Cultural Adaptations Made to the Training Based on Bernal et al.’s (1995) Framework
| Parameter | Elements Added to Intervention |
|---|---|
| Language | The training manual was available in Tamil. |
| Persons | The trainer was matched in ethnicity with participants. |
| Metaphors |
1. Actors in video models were matched in ethnicity. 2. Role-play scenarios chosen were relevant to the area (e.g., academic writing tasks for very young children, joint family contexts with grandparents as caregivers, visits to the temple). 3. All illustrations in the manual included Indian names and situations typical to the region. |
| Content |
1. Specific training on the alternatives to positive punishment (commonly practiced in the region) was provided in the manual. 2. Specific strategies for conveying information regarding treatment to other family members (e.g., grandparents) were provided in the face-to-face training. 3. Examples of naturalistic (e.g., attention, breaks, setting up a preferred activity following a hard or nonpreferred task) reinforcers were provided in the manual and the face-to-face training due to the discomfort with edible and tangible reinforcers. 4. Easy data collection systems akin to the cards used to track milk purchases (used in every household in the region) were provided. |
| Concepts |
1. The trainer used the phrase “developmental delay” instead of “developmental disability” to minimize stigma. 2. The trainer provided ABA strategies as a treatment, in addition to the existing practices in the region. 3. Equivalent Tamil words for ABA terminology, including reinforcement, punishment, function of behavior, automatic reinforcement, extinction, resurgence, and so on, were created (available from the first author). |
| Goals |
1. Improvement in child behavior was stated as a means to remove unwanted negative attention on the child from the general public. 2. Training was viewed as a means of education for the participants to improve the child’s and the family’s quality of life, and ultimately for the child to be eligible to access regular schooling. |
| Methods |
1. Proactive strategies were prescribed as a general means of improving behavior in an attempt for the trainer to adopt a directive role in both the manual and during the training. 2. The participants in the training were recruited via flyers distributed at an office of a pediatrician, a role that is often revered for experience and expertise. 3. During the ABA information sessions conducted prior to the training, the trainer set aside time for all attendees to introduce themselves in an attempt to develop a personal relationship. 4. The trainer also provided personal information (educational and family background, area of residence, hobbies, marital status) about herself when this information was requested during the training. |
| Context |
1. Face-to-face training was conducted in a general education preschool to make it more accessible and less stigmatizing. 2. A snack and a beverage were offered during the face-to-face training consistent with social etiquette. |
The manual included a variety of hypothetical examples using individuals with Indian names in situations commonly encountered in the region. For instance, one example from the manual (translated into English here) described Meera, who goes to the temple with her grandparents every evening. They enter the main hall of the temple for the evening prayer, and Meera starts making loud noises. When this happens, her grandfather takes her outside the temple for a walk. After introducing this example, the manual describes the proactive strategy of asking Meera whether she wants to go inside the main hall or sit down near the flower store outside of the temple.
Participants did not have any prior knowledge of or experience with applied behavior analysis (ABA), so the trainer recruited via flyers in the offices of pediatricians, who are revered for their experience and expertise in this region. The trainer also conducted 30-min informational sessions prior to the study for all interested participants. In these sessions, the trainer introduced ABA as a scientific approach to understanding human behavior and emphasized its use in everyday situations in a classroom, at home, or in a neighborhood play area. This method was consistent with previous research conducted with individuals with no prior exposure to ABA (e.g., Denne, Thomas, Hastings, & Hughes, 2015).
Certain features of the training also expanded on the known activities of the participants. For example, many participants had no prior exposure to data collection on child behavior, but all participants had daily exposure to data collection on their family’s milk consumption. In Chennai, every family has a card to track milk consumption. This card is left for the vendor who delivers milk to the household each week. The ABC data sheet we developed for the training included certain visual characteristics of this milk card. Other features of the training emphasized certain strategies (e.g., using naturalistic reinforcers), and covered certain content (e.g., occupational therapy, punishment procedures), based on the participants’ perceived interest in and comfort level with these topics. We also provided strategies (e.g., giving a rationale, modeling) for our participants to convey this information to grandparents who were regularly involved in childcare activities in the region. Concepts such as “disability” that are associated with stigma in the region were replaced with acceptable alternatives (e.g., “delay”). We also capitalized on the emphasis that families in India place on education as a means for improvement. The FBAI training was proposed as a means for a child with problem behavior to potentially become eligible to access regular education.
Finally, the setting of the training was in a general education preschool to avoid the stigma often associated with visiting special education schools in the region. A snack and beverage were offered during training, consistent with local social etiquette.
Experimental Design
We used a multiple-baseline across-participants design by conducting additional baseline measures for participants in the second training compared to the first training, and additional baseline measures for participants in the third training compared to the second.
Results
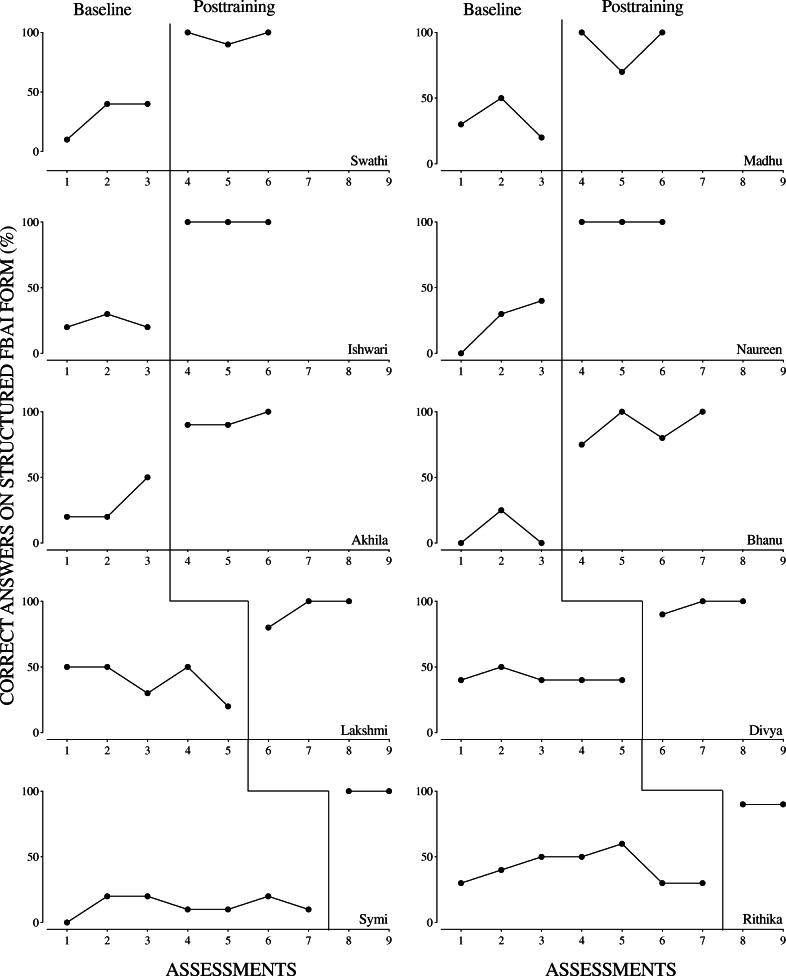
Figure 1 shows each participant’s score on the structured FBAI form. For all participants, baseline scores were consistently below 80% prior to training and consistently above 80% only after training was conducted. Further, all participants received 100% correct on the structured form on at least one posttraining assessment. Mean performance prior to training was 30% and following training was 95.4% across participants.
Fig. 1.
Participant scores on the structured FBAI form
Figure 2 shows participants’ scores on the videotaped role-plays of function-based intervention procedures. Participants also showed marked improvement on this measure following training. Mean performance prior to training was 29.2% and following training was 88.1% across participants. For only one participant, Divya, an increasing trend in baseline was evident. Thus, for all but Divya, these results suggest that the training effectively increased the participants’ fidelity of implementation of functional communication training and extinction procedures. Four participants submitted a video of their implementation of these same procedures with a child 3 weeks after training. Performance on the videotaped implementations with the child averaged 90% for these participants, providing preliminary support for the generality of changes in participant behavior.
Fig. 2.
Participant scores on the videotaped role-plays
Social validity data are shown in Table 2. In general, all participants rated the training very highly, and a few also indicated interest in obtaining certification in behavior analysis.
Discussion
To our knowledge, this is the first study to evaluate the efficacy and social validity of a manualized training for teaching behavior-analytic perspectives and skills to an Indian population. In regions such as India, where unsubstantiated treatments are often practiced, and several barriers exist to accessing behavior-analytic intervention, the present study produced successful preliminary outcomes in the education and training of parents and service providers. The study provided clear descriptions of the cultural adaptations made to all aspects of training procedures, from recruitment to delivery. Consideration of the culture, context, and ecology is crucial for the development of parent education and behavioral intervention programs for culturally diverse families (Bernal et al., 1995; Hwang, 2006; Santarelli, Koegel, Casas, & Koegel, 2001), and this is not a new idea in the literature (Albin, Lucyshyn, Horner, & Flannery, 1996; Bailey et al., 1990). However, the paucity of research being conducted outside of the United States with varied populations emphasizes the need for culturally sensitive trainings to be evaluated.
Our data suggest that the training was effective in teaching key skills involved in writing a behavioral assessment and intervention plan, but limitations of this measure must be considered alongside these promising results. The form was structured to guide participants to indicate specific information in predetermined areas; it remains unknown whether the participants would have included all pertinent information in the absence of this structure. In addition, the form required participants to assume functions based on ABC data and in the absence of a functional analysis. We used ABC data as a means for our participants to hypothesize the function of the behavior; however, previous research has shown that determining function based on ABC data alone can lead to erroneous conclusions (Camp, Iwata, Hammond, & Bloom, 2009). Nevertheless, we felt that considering potential functions based on ABC data was an improvement over participants’ common practice of intervening without any consideration of function or learning history.
Our data also suggest that the training was effective in improving participants’ direct implementation of evidence-based assessment and intervention procedures. However, the majority of these measures were obtained during role-plays with adult confederates who were also involved in the training. Obtaining measures with naïve confederates using scripted responses would provide a more rigorous measure of implementation fidelity; obtaining follow-up measures with actual children in a typical setting is optimal. Due to practical constraints, we obtained follow-up data for only a subset of our participants. Maintenance and generalization of training are key measures that may be impacted by the inclusion of cultural adaptations. Thus, measures of implementation with a child both prior to and following training should be included in future research in this area.
The results of this study provide several avenues for future research. If researcher-practitioner collaborations such as those in the present study are funded in the future, long-term investigations using randomized control trials of larger sample sizes can be performed. The training used in the current study introduced the behavior-analytic perspective and provided structured practice of its application, but more support is likely needed to maintain impactful outcomes at high integrity over time. Although we measured two distinct dependent variables in this study, we did not collect data on child behavior change or the long-term adoption of the strategies addressed during the training. In addition, we used multiple-choice options and role-plays as a convenient way to approximate relevant skills (i.e., writing behavior plans and direct implementation with a client). Studying the impact of training on these more complex dependent measures is an important next step.
One promising outcome of our study was the reported interest in obtaining certification following training from a few participants. Should more practitioners and parents in India seek avenues for certification, access to care for the treatment of problem behavior could greatly improve. Until then, future research should evaluate the impact of telehealth services that link behavioral experts with stakeholders worldwide (Barkaia, Stokes, & Mikiashvili, 2017; Barretto, Wacker, Harding, Lee, & Berg, 2006; Tsami, Lerman, & Toper-Korkmaz, 2019). We suggest that this outreach strategy will be most successful in collaboration with a culturally responsive training program like the one described herein. In light of the recent announcement proposing the development of local credentialing programs in behavior analysis (BACB, 2019), and the Behavior Analysis in Practice special issue on diversity and equity highlighting the need for culturally responsive interventions, practitioners and scientists may use the current training protocol as an initial framework to achieve buy-in and positive outcomes outside of the United States.
We close with some suggested guidelines for pursuing the international research and practice mentioned previously. Foremost, we encourage researchers to identify an area or population in particular need of our services (e.g., a region with a low BCBA-to-child ratio). The next step is to form partnerships with research-practitioners native to the region, because effective training requires proficiency in the participants’ native language; knowledge of cultural values, norms, and prejudices; and an understanding of the context of the training setting (Tekola et al., 2019). Such partnerships may arise out of informal discussions at international conferences (e.g., the European Association for Behavior Analysis conference served as the impetus of the partnership between the coauthors of this article), multicultural special interest groups, or online forums. Next, it is recommended that the generality and transferability of established interventions to previously untested target populations be assessed. Cultural modifications may be necessary to increase interest and participation in behavior-analytic research and moderate treatment outcomes. Consider seeking expertise in disciplines outside of behavior analysis for guidelines on completing this step. Despite limited research on necessary and sufficient modifications, cultural and linguistic considerations should be made and documented carefully to provide a baseline upon which such research can be conducted in the future. Subsequently, researchers may recruit participants from a region where the need for treatment has been established (e.g., using pilot surveys, advertisements, meetings with existing practitioners of allied fields). It is possible that obtaining the most robust measures of behavior change may not be feasible at first, but embracing less robust measures lays the groundwork for exploring culturally sensitive interventions in a more rigorous manner. Thus, we hope this study serves as a small step in a movement toward the type of international dissemination that our field has desired for decades.
Electronic supplementary material
(DOCX 18 kb)
Acknowledgements
We thank Rima Hamawe, Amanda Garcia, and the California State University, Northridge, Master of Science in Applied Behavior Analysis class of 2018 for their contributions to the training manual. We also thank Nanditha and Sadhasivam for translating the manual into Tamil.
Compliance with Ethical Standards
Funding
Funding for this study was obtained from the Behavior Analysis Certification Board (BACB) and the College of Social and Behavioral Sciences at California State University, Northridge.
Conflict of Interest
The authors declare no conflict of interest.
Ethical Approval
The study was approved by the Institutional Review Board of California State University, Northridge. All procedures performed in this study involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments.
Informed Consent
Informed consent was obtained from all individual participants in this study.
Footnotes
Research Highlights
• The education and training of parents and service providers in managing problem behavior are crucial in regions with few certified professionals.
• A manualized training was effective at increasing the written and videotaped implementation of functional assessment and function-based intervention procedures.
• We describe the cultural adaptations made to our training along eight dimensions defined by an existing framework.
• We describe guidelines for international dissemination and culturally responsive research based on our results.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Albin RW, Lucyshyn JM, Horner RH, Flannery KB. Contextual fit for behavioral support plans: A model for “goodness of fit.”. In: Koegel LK, Koegel RL, Dunlap G, editors. Positive behavioral support: Including people with difficult behaviors in the community. Baltimore, MD: Brookes; 1996. pp. 81–98. [Google Scholar]
- Antonsson H, Graneheim UH, Isaksson U, Åström S, Lundström MO. Evaluation of a web-based training program for professional carers working with people with learning disabilities and challenging behavior: A pilot study with SSED-design. Issues in Mental Health Nursing. 2016;37(10):734–743. doi: 10.1080/01612840.2016.1189636. [DOI] [PubMed] [Google Scholar]
- Artiles AJ, Trent SC. Overrepresentation of minority students in special education: A continuing debate. Journal of Special Education. 1994;27(4):410–437. doi: 10.1177/002246699402700404. [DOI] [Google Scholar]
- Baer DM, Wolf MM, Risley TR. Some current dimensions of applied behavior analysis. Journal of Applied Behavior Analysis. 1968;1:91–97. doi: 10.1901/jaba.1968.1-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey DB, Simeonsson RJ, Winton PJ, Huntington GS, Comfort M, Isbell P, et al. Family-focused interventions: A functional model for planning, implementing and evaluating individualized family services in early intervention. Journal of the Division for Early Childhood. 1990;10:156–171. doi: 10.1177/001440299806400302. [DOI] [Google Scholar]
- Barkaia A, Stokes TF, Mikiashvili T. Intercontinental telehealth coaching of therapists to improve verbalizations by children with autism. Journal of Applied Behavior Analysis. 2017;50:582–589. doi: 10.1002/jaba.391. [DOI] [PubMed] [Google Scholar]
- Barretto A, Wacker DP, Harding J, Lee J, Berg WK. Using telemedicine to conduct behavioral assessments. Journal of Applied Behavior Analysis. 2006;39:333–340. doi: 10.1901/jaba.2006.173-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beavers, G. A., Iwata, B. A., & Lerman, D. C. (2013). Special issue on functional analysis: Commemorating thirty years of research and practice. Journal of Applied Behavior Analysis, 46, 1–353. [DOI] [PubMed]
- Beavers GA, Iwata BA, Lerman DC. Thirty years of research on the functional analysis of problem behavior. Journal of Applied Behavior Analysis. 2013;46:1–21. doi: 10.1002/jaba.30. [DOI] [PubMed] [Google Scholar]
- Beavers, G. A., Iwata, B. A., & Lerman, D. C. (2013). Special issue on functional analysis: Commemorating thirty years of research and practice. [DOI] [PubMed]
- Behavior Analyst Certification Board. (2019, December 31). Global certification [press release]. Retrieved from https://www.bacb.com/global-certification/
- Behavior Analyst Certification Board. (2020). BCBA/BCaBA registry. Retrieved May 12, 2020, from http://info.bacb.com
- Bernal G, Bonilla J, Bellido C. Ecological validity and cultural sensitivity for outcome research: Issues for the cultural adaptation and development of psychosocial treatments with Hispanics. Journal of Abnormal Child Psychology. 1995;23(1):67–82. doi: 10.1007/BF01447045. [DOI] [PubMed] [Google Scholar]
- Brown JF, Brown MZ, Dibiasio P. Treating individuals with intellectual disabilities and challenging behaviors with adapted dialectical behavior therapy. Journal of Mental Health Research in Intellectual Disabilities. 2013;6(4):280–303. doi: 10.1080/19315864.2012.700684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camp EM, Iwata BA, Hammond JL, Bloom SE. Antecedent versus consequent events as predictors of problem behavior. Journal of Applied Behavior Analysis. 2009;42:469–483. doi: 10.1901/jaba.2009.42-469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daley TC. The need for cross-cultural research on the pervasive developmental disorders. Transcultural Psychiatry. 2002;39(4):531–550. doi: 10.1177/136346150203900409. [DOI] [Google Scholar]
- Degarmo DS, Martinez CR. A culturally informed model of academic well-being for Latino youth: The importance of discriminatory experiences and social support. Family Relations. 2006;55(3):267–278. doi: 10.1111/j.1741-3729.2006.00401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denne L, Thomas E, Hastings R, Hughes C. Assessing competencies in applied behavior analysis for tutors working with children with autism in a school-based setting. Research in Autism Spectrum Disorders. 2015;20:67–77. doi: 10.1016/j.rasd.2015.08.008. [DOI] [Google Scholar]
- Fong EH, Catagnus RM, Brodhead MT, Quigley S, Field S. Developing the cultural awareness skills of behavior analysts. Behavior Analysis in Practice. 2016;9(1):84–94. doi: 10.1007/s40617-016-0111-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grote NK, Swartz HA, Geibel SL, Zuckoff A, Houck PR, Frank E. A randomized controlled trial of culturally relevant, brief interpersonal psychotherapy for perinatal depression. Psychiatric Services. 2009;60(3):313–321. doi: 10.1176/appi.ps.60.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall GN, Ibaraki AY, Huang ER, Marti CN, Stice E. A meta-analysis of cultural adaptations of psychological interventions. Behavior Therapy. 2016;47:993–1014. doi: 10.1016/j.beth.2016.09.005. [DOI] [PubMed] [Google Scholar]
- Hamad CD, Serna RW, Morrison L, Fleming R. Extending the reach of early intervention training for practitioners: A preliminary investigation of an online curriculum for teaching behavioral intervention knowledge in autism to families and service providers. Infants and Young Children. 2010;23:195. doi: 10.1097/IYC.0b013e3181e32d5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanley GP, Iwata BA, McCord BE. Functional analysis of problem behavior: A review. Journal of Applied Behavior Analysis. 2003;36:147–185. doi: 10.1901/jaba.2003.36-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horner RH. Functional assessment: Contributions and future directions. Journal of Applied Behavior Analysis. 1994;27:401–404. doi: 10.1901/jaba.1994.27-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horner RH, Carr EG, Strain PS, Todd AW, Reed HK. Problem behavior interventions for young children with autism: A research synthesis. Journal of Autism and Developmental Disorders. 2002;32(5):423–446. doi: 10.1023/A:1020593922901. [DOI] [PubMed] [Google Scholar]
- Hossain MD, Ahmed HU, Jalal Uddin MM, Chowdhury WA, Iqbal MS, Kabir RI, et al. Autism spectrum disorders (ASD) in South Asia: A systematic review. BMC Psychiatry. 2017;17:281. doi: 10.1186/s12888-017-1440-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang WC. The psychotherapy adaptation and modification framework: Application to Asian Americans. American Psychologist. 2006;61:702–715. doi: 10.1037/0003-066x.61.7.702. [DOI] [PubMed] [Google Scholar]
- Hwang WC. The formative method for adapting psychotherapy (FMAP): A community-based developmental approach to culturally adapting therapy. Professional Psychology: Research and Practice. 2009;40(4):369–377. doi: 10.1037/a0016240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang, W. C. (2016). Culturally adapting psychotherapy for Asian heritage populations. Claremont, CA: Academic Press.
- Ingersoll B, Berger N. Correction: Parent engagement with a telehealth-based parent-mediated intervention program for children with autism spectrum disorders: Predictors of program use and parent outcomes. Journal of Medical Internet Research. 2015;17:e257. doi: 10.2196/jmir.4913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwata BA, Pace GM, Dorsey MF, Zarcone JR, Vollmer TR, Smith RG, et al. The functions of self-injurious behavior: An experimental-epidemiological analysis. Journal of Applied Behavior Analysis. 1994;27:215–240. doi: 10.1901/jaba.1994.27-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur D, Roy S. Self-injurious behavior (SIB) of eye poking in a toddler with autism, neurofibromatosis and infantile spasm. ASEAN Journal of Psychiatry. 2017;18:99–102. [Google Scholar]
- Kayrouz R, Dear BF, Karin E, Fogliati VJ, Titov N. A pilot study of a clinician-guided Internet-delivered cognitive behavioural therapy for anxiety and depression among Arabs in Australia, presented in both English and Arabic languages. Internet Interventions. 2016;5:5–11. doi: 10.1016/j.invent.2016.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee E. Chinese American families. In: Lee E, editor. Working with Asian Americans: A guide for clinicians. New York, NY: Guilford Press; 1997. pp. 46–78. [Google Scholar]
- Lin YN. The application of cognitive behavioral therapy to counseling Chinese. American Journal of Psychotherapy. 2002;55(4):46–58. doi: 10.1176/appi.psychotherapy.2002.56.1.46. [DOI] [PubMed] [Google Scholar]
- Malgady RG, Rogler LH, Costantino G. Culturally sensitive psychotherapy for Puerto Rican children and adolescents: A program of treatment outcome research. Journal of Consulting and Clinical Psychology. 1990;58(6):704–712. doi: 10.1037//0022-006x.58.6.704. [DOI] [PubMed] [Google Scholar]
- Marleau, B., Lanovaz, M. J., Gendron, A., Higbee, T. S., & Morin, D. (2018). Using interactive web training to teach parents to select function-based interventions for challenging behaviour: A preliminary study. Journal of Intellectual & Developmental Disability. Advance online publication. 10.3109/13668250.2018.1464281.
- Martin NT, Nosik MR, Carr JE. International publication trends in the Journal of Applied Behavior Analysis: 2000–2014. Journal of Applied Behavior Analysis. 2016;49:416–420. doi: 10.1002/jaba.279. [DOI] [PubMed] [Google Scholar]
- McKenzie K, Milton M, Smith G, Ouelette-Kuntz H. Systematic review of the prevalence and incidence of intellectual disabilities: Current trends and issues. Current Developmental Disorders Reports. 2016;3:104. doi: 10.1007/s40474-016-0085-7. [DOI] [Google Scholar]
- Mueller MM, Piazza CC, Moore JW, Kelley ME, Bethke SA, Pruett AE, et al. Training parents to implement pediatric feeding protocols. Journal of Applied Behavior Analysis. 2003;36:545–562. doi: 10.1901/jaba.2003.36-545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naeem F, Waheed W, Gobbi M, Ayub M, Kingdon D. Preliminary evaluation of culturally sensitive CBT for depression in Pakistan: Findings from Developing Culturally-Sensitive CBT Project (DCCP) Behavioural and Cognitive Psychotherapy. 2011;39:165–173. doi: 10.1017/S1352465810000822. [DOI] [PubMed] [Google Scholar]
- Nagaraj R, Singhi P, Malhi P. Risperidone in children with autism: Randomized, placebo-controlled, double blind study. Journal of Child Neurology. 2006;21:450–455. doi: 10.1177/08830738060210060801. [DOI] [PubMed] [Google Scholar]
- Nakamura H. Ways of thinking of Eastern people: India, China, Tibet, and Japan. Honolulu, HI: East West Center Press; 1964. [Google Scholar]
- National Autism Center. (2015). Findings and conclusions: National standards project, phase 2. Randolph, MA: Author.
- Nicolas GM, Arntz DL, Hirsch B, Schmiedigen A. Cultural adaptation of a group treatment for Haitian American adolescents. Education and Psychological Studies. 2009;40(4):378–384. doi: 10.1037/a0016307. [DOI] [Google Scholar]
- Organista KC, Munoz RF. Cognitive behavioural therapy with Latinos. Cognitive and Behavioral Practice. 1996;2(3):255–270. doi: 10.1016/S1077-7229(96)80017-4. [DOI] [Google Scholar]
- Reimers TM, Wacker DP. Acceptability of behavioral treatments for children: Analog and naturalistic evaluations by parents. School Psychology Review. 1992;21:628–643. [Google Scholar]
- Roland A. In search of self in India and Japan: Towards a cross-cultural psychology. Princeton, NJ: Princeton University Press; 1988. [Google Scholar]
- Sahithya BR, Manohari SM, Vijaya R. Parenting styles and its impact on children: A cross cultural review with a focus on India. Mental Health, Religion & Culture. 2019;22:357–383. doi: 10.1080/13674676.2019.1594178. [DOI] [Google Scholar]
- Salomone E, Pacione L, Shire SY, Brown F, Reichow B, Servili C. Development of the WHO Caregiver Skills Training Programme for developmental disorders or delays. Frontiers in Psychiatry. 2019;10:1–9. doi: 10.3389/fpsyt.2019.00769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santarelli G, Koegel RL, Casas JM, Koegel LK. Culturally diverse families participating in behavior therapy parent education programs for children with developmental disabilities. Journal of Positive Behavior Interventions. 2001;3(2):120–123. doi: 10.1177/109830070100300209. [DOI] [Google Scholar]
- Sarokoff RA, Sturmey P. The effects of behavioral skills training on staff implementation of discrete-trial teaching. Journal of Applied Behavior Analysis. 2004;37:535–538. doi: 10.1901/jaba.2004.37-535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepis MM, Reid DH, Ownbey J, Parsons MB. Training support staff to embed teaching within natural routines of young children with disabilities in an inclusive preschool. Journal of Applied Behavior Analysis. 2001;34:313–327. doi: 10.1901/jaba.2001.34-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott J, Lerman DC, Luck K. Computer-based training to detect antecedents and consequences of problem behavior. Journal of Applied Behavior Analysis. 2018;51:784–801. doi: 10.1002/jaba.495. [DOI] [PubMed] [Google Scholar]
- Sengupta K, Lobo L, Krishnamurthy V. Educational and behavioral interventions in management of autism spectrum disorder. Indian Journal of Pediatrics. 2017;84:61–67. doi: 10.1007/s12098-015-1967-0. [DOI] [PubMed] [Google Scholar]
- Sharma N. Current trends in infant care: An Indian experience. Early Childhood Development and Care. 1999;68:71–79. [Google Scholar]
- Sinha JBP, Sinha TN, Verma J, Sinha RBN. Collectivism coexisting with individualism: An Indian scenario. Asian Journal of Social Psychology. 2001;4:133–145. doi: 10.1111/j.1467-839X.2001.00081.x. [DOI] [Google Scholar]
- Suess AN, Romani PW, Wacker DP, Dyson SM, Kulhe JM, Lee JF. Evaluating the treatment fidelity of parents who conduct in-home functional communication training with coaching via telehealth. Journal of Behavioral Education. 2014;23:34–59. doi: 10.1007/s10864-013-9183-3. [DOI] [Google Scholar]
- Sugai G, O’Keeffe BV, Fallon LM. A contextual consideration of culture and school-wide positive behavior support. Journal of Positive Behavioral Interventions. 2012;14:197–208. doi: 10.1177/1098300711426334. [DOI] [Google Scholar]
- Tekola, B., Girma, F., Kinfe, M., Abdurahman, R., Tesfaye, M., Yenus, Z., et al. (2019). Adapting and pre-testing the World Health Organization’s Caregiver Skills Training Programme for autism and other developmental disorders in a very low-resource setting: Findings from Ethiopia. Autism. Advance online publication. 10.1177/1362361319848532. [DOI] [PMC free article] [PubMed]
- Tsami L, Lerman D, Toper-Korkmaz O. Effectiveness and acceptability of parent training via telehealth among families around the world. Journal of Applied Behavior Analysis. 2019;52:1113–1129. doi: 10.1002/jaba.645. [DOI] [PubMed] [Google Scholar]
- Tuli M. Beliefs on parenting and childhood in India. Journal of Comparative Family Studies. 2012;43(1):81–91. doi: 10.3138/jcfs.43.1.81. [DOI] [Google Scholar]
- Wacker DP, Berg WK, Harding JW, Derby KM, Asmus JM, Healy A. Evaluation and long-term treatment of aberrant behavior displayed by young children with developmental disabilities. Developmental and Behavioral Pediatrics. 1998;19:260–266. doi: 10.1097/00004703-199808000-00004. [DOI] [PubMed] [Google Scholar]
- Wallace MD, Doney JK, Mintz-Resudek CM, Tarbox RS. Training educators to implement functional analyses. Journal of Applied Behavior Analysis. 2004;37:89–92. doi: 10.1901/jaba.2004.37-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 18 kb)