Abstract
Different opinions about the reconstructive choice for upper limb are described in literature: advancement or rotation flaps, regional flaps and free flaps are the most common reconstructive options. Local and regional flaps can be used to cover small defects while large wounds require the use of free flaps or distant pedicled flaps. The coverage of large wounds opens a discussion about when to use free flaps and when distant pedicled flaps. This review will describe the different methods used for the coverage of soft tissues injuries affecting hand and/or forearm (excluding fingers). The aim is to show all flap reconstructive options in order to support the inexperienced surgeon during the management of traumatic injuries of the upper limb.
Keywords: Upper limb reconstruction, Upper limb trauma, Advancement and rotation flaps, Regional flaps, Free flaps
Highlights
-
•
Traumatic injuries of the upper limbs can represent serious and challenging wounds.
-
•
The main challenge for a hand surgeon is to offer a stable, long lasting and aesthetically acceptable coverage.
-
•
Advancement or rotation flaps, regional flaps and free flaps are the most common reconstructive options of the upper limb.
-
•
Knowledge gleaned from the wide experience of surgeons is fundamental for the decision-making process.
1. Introduction
Traumatic injuries of the upper limbs often result in serious and challenging wounds involving multiple compartments such as skin, bone, tendons and neurovascular structures. Limb function could be compromised. Complex wounds are generally caused by road traffic accidents, work-related or domestic accidents, thermal, electrical or chemical burns, firearm injuries, etc.
The main challenge for a hand surgeon is to cover these wounds providing a stable, long lasting and aesthetically acceptable coverage that enables joints excursion in order to ensure patient return to work [1].
The complex functionality of the hand and the number of involved structures make it often difficult to obtain a functional restoration, therefore amputation is the chosen solution in challenging cases.
The choice of the right reconstructive technique depends on various factors such as patient's age, nature and duration of the trauma, characteristics of the wound and conditions of the surrounding tissues. The exposure of vital structures and the need for secondary procedures influence the reconstructive choice.
Hand defects are unique, and an optimal reconstruction should guarantee tendons and joints movement and be effective enough to allow heavy work but at the same time maintain the sensitivity of the hand.
The most common reconstructive options include advancement or rotation flaps, regional flaps and free flaps [2].
This review will consider the different methods described for the coverage of soft tissues injuries affecting hand and/or forearm (excluding fingers).
2. First step: debridement
Some considerations have to be done when facing a traumatic upper extremity before proceeding with reconstruction.
In case of the limb salvage is possible it is difficult to predict functional outcomes even if different scoring systems have been proposed [3,4].
In severe traumas it is mandatory to consider that the involved joints tend to stiffen and tendons to stick, moreover adjacent structures are generally indirectly involved [5].
First, based on the guidelines for open fractures, an antibiotic prophylaxis is needed [6] along with an overall assessment of the neurovascular status and exclusion of a compartmental syndrome [7].
The following questions must be asked: What prevents tendons from gliding? Or joints from stiffening? An insufficient debridement, the presence of dead space filled by hematoma, an unstable fixation and an inadequate coverage can contribute to this situation.
These factors cause scar tissue formation which leads to stiffness and functional impairment of the limb; for this reason, an adequate debridement and prevention of complications such as hematomas or formation of dead spaces have to be ensured [8].
Devitalized tissues are a nest for inflammatory response and create a wound bed that tends to heal due to fibrosis which results in scar tissue. Reducing devitalized tissues is essential for bone revascularization and tendon gliding [8].
It is therefore necessary to proceed with a precise and rapid debridement of the wound to identify structures suitable for repair. In this context it is good to perform, if demanded, a fasciotomy especially when prolonged ischemia occur [9].
A compartmental syndrome is always to be considered and it can occur with minimal symptoms and be difficult to diagnose [8] therefore, when a compartmental syndrome is suspected, fasciotomies must be performed.
More than one debridement is usually required for final demarcation of the wound and reduction of infectious risk [10].
3. Assessment of the wound with Negative Pressure Wound Therapy
Negative Pressure Wound Therapy (NPWT) is covered in a separate chapter as an advanced dressing between debridement or until the wound is ready for tissue coverage. NPWT reduces swelling, edema, mediators of inflammation and risk of infection by preserving a closed wound [11].
The use of vacuum assisted therapy is always to be discussed as it is a simple method for a temporary coverage of the wound and a useful aid to improving the wound bed.
The NPWT allows removal of blood and serum thus reducing edema and dead spaces, bacterial count and infectious potential and increasing microperfusion and neovascularization of the wound bed [2]. NPWT promotes granulation in soft tissue defects decreasing the amount of tissue required for final coverage and consequently decreasing the donor site morbidity.
Immediate reconstruction is contraindicated in unstable patients who cannot undergo long surgical procedures. Wounds with clear infection and in patients whom have undergone amputation and use of prosthesis can result in better functional outcomes than reconstruction [12] even if an early reconstruction seems to reduce hospitalization time and hospital costs [13].
Negative pressure therapy addresses the disadvantages of open wounds before they are covered with flaps, but it cannot be considered as an alternative to surgical debridement [14].
4. Flap choice: fasciocutaneous Vs muscle flaps
The next step is to consider the type of flap to use for wound coverage.
The aims of proper coverage are to obliterate dead spaces (in the context of infectious risk), promotion of wound healing with restoration of venous and lymphatic circles [15] and to provide a gliding coverage for tendons and muscles [16].
Fascial or fasciocutaneous flaps, compared to muscular flaps, provide a better cover for tendons sliding, moreover they are easier to rise in case of a second surgical step [17] due to less scars.
Another advantage of fasciocutaneous flaps compared to muscle flaps is the restoration of sensitivity which is extremely important in the functional outcome of the hand [18].
Fasciocutaneous flaps provide adequate tissue coverage with different possible orientations of the flap during the insetting, offer a gliding surface for tendons sliding and do not cause functional deficits [19].
There are many fascial or fasciocutaneous flaps available, but radial forearm flap (RFF), lateral arm flap (LAF), scapular flap (SF), temporoparietal fascial free flaps (TPF) and anterolateral thigh flap (ALT) are the most commonly used [20].
The ALT is one of the primary flaps for the reconstruction of large defects. ALT has a reliable cutaneous paddle and its volume can be adjusted by trimming and thinning the flap allowing greater application for reconstruction of the forearm and the thenar area; however, its anatomical variations and the learning curve are considered as disadvantages [21].
The muscle flaps can be trimmed, stretched along the fibers and apply to fill dead spaces [18].
Muscle flaps could be preferred in complex contaminated wounds because, on experimental studies, they have been shown to bring greater blood flow, antimicrobial activity and biological contribution to bone healing [22,23]. They are ideal for functional transfer combined with wound coverage [24].
Among the muscular flaps the choice is mainly based on the experience of the surgeon, but latissimus dorsi and rectus abdominis are the workhorses for large soft tissues defects; smaller defects can be covered with smaller portions of these muscles or with smaller muscles such as serratus anterior or gracilis flap [20]. The pedicled or free latissimus dorsi flap and the free gracilis flaps are the most used for functional transfers [24].
5. Locoregional pedicled flaps
Different locoregional pedicled flaps were described for hand reconstruction.
The Posterior Interosseous Artery Flap (PIAF) and the Reverse Radial Forearm Flap (RRFF) are well known for reconstruction of the hand, wrist and the first web space [25].
Among the advantages of these flaps are the single stage procedure that requires only one operating field and a rapid post-operative mobilization, furthermore the donor site can be closed by first intention for small defects.
On the other hand, the tedious dissection and the risk of venous congestion are the disadvantages [26], even if both flaps have a high success rate [27].
The RRFF can be used to cover defects of the wrist, palm and dorsum of the hand, proximal fingers and thumb, but the sacrifice of the radial artery makes it contraindicated in patients with inadequate ulnar artery inflow [2].
This flap can be harvested as an osteocutaneous flap and be considered in the reconstruction of the thumb for patients with contraindication to toe transfer [28].
The vascularization of the posterior interosseous artery was described by Manchot in 1989, but the island flap was described in 1986 [29].
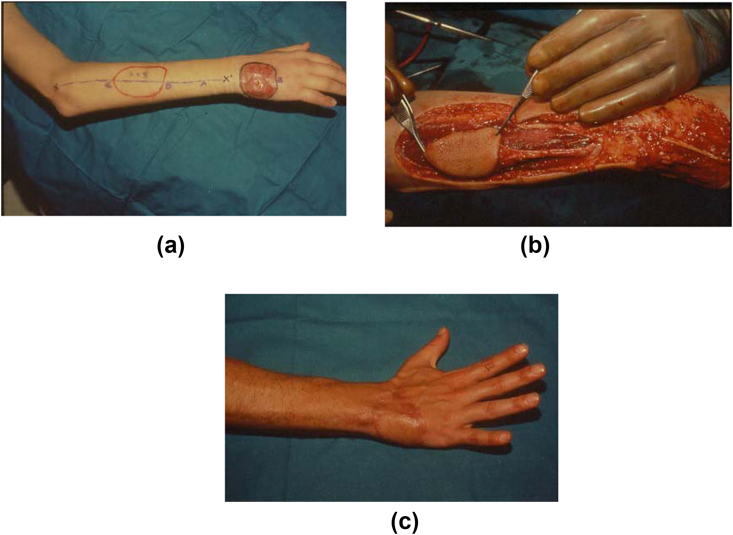
The PIAF can provide a pliable and thin cover for the defects of the dorsum, the wrist, the thumb and the first web space; it fits well the 3D defects, does not sacrifice a major artery and can provide a gliding surface for tendons (See Fig. 1).
Fig. 1.
Hand defect of the dorsum (Fig. 1a); Posterior Interosseous Artery Flap Harvest (Fig. 1b); Post-operative result (Fig. 1c).
The distal pedicle forearm flap based on the ulnar artery is a thin and reliable flap and can be a good option for defects of the wrist, palm, dorsum and proximal fingers [2].
The donor site morbidity is to be considered in these flaps, especially in relation to the aesthetics and the visibility of the hand [20].
In the immediate postoperative period, patients are generally concerned about injuries in hand reconstruction, but over time their concern is with the donor site and the aesthetic appearance.
Various options were proposed to improve the appearance of donor site and the lowest associated morbidity is when radial forearm flap is used [30].
Some authors found that RRFF can be used for wider therapeutic indications than PIAF and has better aesthetic results, however, considering the vascular pattern, the PIAF would be preferable because it does not sacrifice any major vessel [27].
RRFF is technically simpler and faster to rise than PIAF. PIAF has a major risk of venous congestion, which is the most frequent cause of partial or total flap necrosis [31].
6. Abdominal pedicled flaps
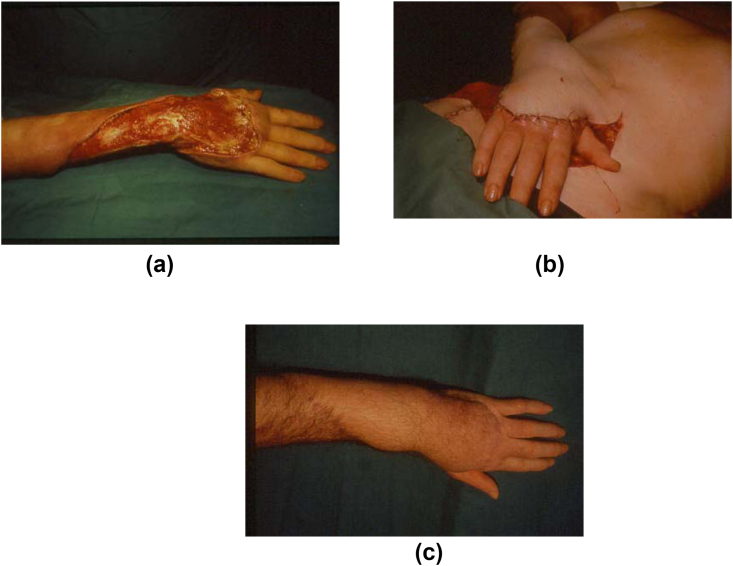
Among the distant pedicled flaps, abdominal flaps are still used for some reconstructions of the upper limb. There are four abdominal flaps: The groin flap based on the Superficial Circumflex Iliac Artery (SCIA), the Superficial External Pudendal Artery (SEPA) flap supplied by the homonymous artery, the Superficial Inferior Epigastric Artery (SIEA) flap and the paraumbilical perforators (PUP) flap supplied by perforators of the deep inferior epigastric artery (See Fig. 2).
Fig. 2.
Wide hand defect of the dorsal region (Fig. 2a); Distant abdominal pedicle flap (Fig. 2b); Post-operative result (Fig. 2c).
Groin flap was described by Mc Gregor and Jackson and it is certainly the most used among the abdominal flaps [32].
Saving time with reconstruction in one surgical step and avoid scarring for tendon sliding are the main advantages of these flaps and the surgical time is shorter compared to free flaps.
Their main disadvantage is the immobilization of the limb for three weeks which can lead to joint stiffness.
In the microsurgery era, pedicled flaps are often overlooked, however they are extremely versatile and can be used in different ways to fill large soft tissue defects of the arm [33]. When all the pedicles of abdominal flaps are included, a 30 × 15 cm flap can be raised without a delay and can cover an area that extends from the elbow to the metacarpophalangeal joints.
The distal part of these flaps generally acts as a random flap and it is supplied exclusively by the dermal plexus, so that it can be thinned [34].
The groin flap is thinner than other flaps such as the ALT or the lateral arm flap, and in combination with the primary thinning technique it results in a thin flap even in obese patients [34].
For many authors the abdominal pedicled flaps remain the workhorses for reconstruction of the upper limb thanks to some tricks that make the patient's position more comfortable: keeping a narrow base rather than tubing it and an adequate length of the pedicle allows a movement of the flap in the postoperative period facilitating physiotherapy [34]. These refinements, in the opinion of some authors, give better outcomes than free flaps.
Concerning joint stiffness, some authors respond with a dedicated post-operative rehabilitation therapy that is able to obtain normal functional results. Ravikiran et al. found no shoulder or elbow stiffness in a three-week immobilization [25].
Furthermore, the pedicled distant flaps do not require microsurgical skills and are practical options when patient factors do not allow long surgical times [8].
Although the advent of free flaps has overtaken the use of pedicled flaps, these are still used in many microsurgical centers especially with these refinements that allow better comfort and better aesthetic outcomes.
7. Free flaps
Size of the flap, length and size of the pedicle, texture, thickness, color and whether sensitivity is required, have to be considered when choosing a free flap. Other parameters are morbidity of the donor site, need for further surgeries and surgeon's preference [35].
Among fasciocutaneous flaps the radial forearm flap, the lateral arm, the scapular, the temporoparieral fascial free flaps and ALT are the most commonly used in the reconstruction of the upper limb; latissimus dorsi, rectus abdominis, serratus anterior or gracilis among the muscle flaps [20].
Free flaps are an excellent treatment option in a single stage procedure: allow rapid post-operative mobilization, discharge and return to work [36] with less hospitalization and lower general costs [16].
One of the advantages is the orthoplastic approach: raising flaps as composite or chimeric and obtain a functional neurovascular and osteotendinous reconstruction in only one surgical time [37].
According to some studies, free flaps provide the best coverage in cases of severe injury to the upper limb by providing healthy tissues and promoting vascular growth: the blood supply has the advantage to improve bone healing and resistance to infections [18].
Indications for free flaps are when local flaps cannot be raised (referring to reconstructive ladder) or for extensive defects involving vital structures such as bones, tendons, nerves and vessels. Major indications include coverage after tumors resection or soft tissue infections.
However, early coverage with a free flap is not always possible and patients with comorbidities such as cardiovascular, neurosurgical, renal and hemodynamic function problems must be optimized before proceeding to major surgical procedures [21].
Reconstruction with free flaps is indicated whenever receiving vessels are outside the injury area, otherwise local or distant pedicled flaps could be valid options [24].
Rehabilitation after free flap usually starts 24 h after surgery before the muscles lose strength and excursion [24].
8. Local and perforators flaps
Pedicled transposition or rotation flaps are simple to raise and bring local skin with good color and texture match to the wound, however, their rotation arc is generally restricted to 90° and their use is limited to the area of skin laxity. These flaps often leave dog ears and require revisions [38].
A perforator-based propeller flap for the upper limb reconstruction combines the advantages of local pedicled flaps (good tissue match), regional pedicled flaps (180° of rotation), distant pedicled flaps (reliable) and free flaps (tissue outside the injury area) [39] achieving better aesthetic outcomes because tissues are covered with like to like [40].
Improvements in perforator flaps allow surgeons to harvest thin, pliable and well vascularized skin flaps, preserve the underlying muscle and, for small defects, close the donor site without skin grafting, moreover they can be used as pedicled or free flaps.
Pedicled perforators can be raised from the forearm without sacrificing vessels, are sturdy and can be harvested as fasciocutaneous or adipofascial flaps. Surgical time is less than free flaps and morbidity is limited [41].
These flaps are not even dependent on the facility. Their main disadvantage is the aesthetics outcome of the donor site, but they certainly have a role in the upper extremity reconstruction especially in countries with few resources [39].
However, the upper limb perforator arteries are generally shorter compared to those of the lower limb and it affects the rotation arc. Some authors prefer to avoid these flaps on extremities when a large trauma with associated fractures has occurred; in any case the decision is intraoperatively evaluated in relation to the flap viability [42].
Perforator-based propeller flaps are a valid option to cover small and medium-sized defects in selected patients, however the complication rate remains high, especially when compared to free flaps in well-specialized centers [42].
9. Discussion
The choice of the type of coverage in the losses of substance of the upper limb is the subject of persistent debates and argumentations. The existence of a wide range of options even very different from each other, and the lack of strict guidelines, inevitably leaves the greater freedom of application by the surgeon based on his knowledge and skills [1,2].
Over time, various algorithms have been proposed to guide the surgical choices in a more sharable way [3,4]. Many elements were taken into consideration including patient's characteristics, type and localization of wound. Some authors have paid particular attention to skin similarity and reduced morbidity at the donor site, therefore preferring fasciocutaneous and perforating flaps [16].
The fascial and fasciocutaneous flaps are optimal for protecting tendon sliding, and allow to provide also for the sensitive component, especially important for the hand [[18], [19], [20]]. The perforating flaps also permit to avoid the sacrifice of vessels but, due to the shortness of their pedicle, they can only adapt to reduced losses of substance [40]. If the area to be covered is deeper, muscular flaps are necessary to avoid leaving dead spaces that could easily favor the formation of hematomas [41].
In general, it is believed that local or loco-regional flaps may be sufficient for small defects, while for major wounds free or distant pedicled flaps are more suitable to avoid further damage near the injury site [42].
The choice between free and distant pedicled flaps imply important considerations. Free flaps allows healthy multi-tissutal transfers with indisputable advantages in terms of blood supply, potential for healing and resistance to infections [20]. The possibility of a single-stage reconstruction followed by early rehabilitation reduces the risks of adhesions and stiffness, allowing a better and faster potential recovery [16,37]. The difficulty of execution lies in the need for adequate microsurgical skills and therefore they are burdened with a higher failure rate [21]. Distant pedicled flaps (such as the abdominals) have always been considered reliable, especially in patients with comorbidities which cannot be subjected to long and complex surgical operations, in case of extensive vascular damage (burns, scars, smokers…) or if considered part of a more articulated surgical strategy as a preparation for subsequent further transfers such as toe-to-thumb or vascularized fibula [[25], [26], [27], [28]]. Their main disadvantages are the need for a two-stage approach, the adaptation to the extension and position of the wound to be covered, the potential for limb stiffness and consequent prolonged rehabilitation, the frequent recourse to the subsequent debulking [30].
Beyond all these considerations, surgical choices are still largely linked to the personal experience and technical ability, besides to the resources available in the different hospitals.
10. Conclusion
Discordant opinions on the reconstructive choice for upper limb are found in literature: whether to use pedicled flaps (regional or distant) or free flaps.
In general, although local and regional flaps can be used to cover small defects, large wounds require the use of free flaps or distant pedicled flaps [16].
The greatest discussion arises from large wounds, when to use free flaps and when distant pedicled flaps.
Local flaps have limited applications for large defects considering the poverty of an expandable donor site, especially in the hand where the flap's range of motion is reduced. Furthermore, damage to adjacent tissues, in case of trauma, can compromise the vitality of the transfer [18].
Several algorithms have been proposed, but it seems that the tendency is to choose based on surgeons’ experiences [16]. Evidence-based advice from experts and their thoughts gleaned from the wide experience are fundamental for the decision-making process [[43], [44], [45], [46], [47], [48]].
Provenance and peer review
Not commissioned, externally peer reviewed.
Ethical approval
Nothing to declare.
Consent
The study is a review of the literature.
Registration of research studies
The research does not involve human participants but it is a review of the literature.
Sources of funding
Nothing to declare.
Author contribution
Elisa Benanti: study concept, data interpretation, writing the paper.
Giorgio De Santis: study concept, data interpretation, writing the paper.
Andrea Leti Acciaro: data collection.
Giulia Colzani: data collection.
Alessio Baccarani: data collection.
Marta Starnoni: study concept, data interpretation, writing the paper.
Guarantor
Elisa Benanti; Giorgio De Santis; Andrea Leti Acciaro; Giulia Colzani; Alessio Baccarani; Marta Starnoni.
Trial registry number
Nothing to declare.
Declaration of competing interest
The authors declares that there is no conflict of interest regarding the publication of this paper.
References
- 1.Alphonsus C.K. Principles in the management of a mangled hand. Indian J. Plast. Surg. 2011 May;44(2):219–226. doi: 10.4103/0970-0358.85343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bashir M.M., Sohail M., Shami H.B. Traumatic wounds of the upper extremity. Hand Clin. 2018 Feb;34(1):61–74. doi: 10.1016/j.hcl.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Durham R.M., Mistry B.M., Mazuski J.E., Shapiro M., Jacobs D. Outcome and utility of scoring systems in the management of the mangled extremity. Am. J. Surg. 1996 Nov;172(5):569–573. doi: 10.1016/S0002-9610(96)00245-0. [DOI] [PubMed] [Google Scholar]
- 4.Bray P.W., Bover M.I., Bowen C.V. Complex injuries of the forearm. Coverage considerations. Hand Clin. 1997 May;13(2):263–278. [PubMed] [Google Scholar]
- 5.Del Pinal F., Urrutia E., Klich M. Severe crush injury to the forearm and hand: the role of microsurgery. Clin. Plast. Surg. 2017 Apr;44(2):233–255. doi: 10.1016/j.cps.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Holtom P.D. Antibiotic prophylaxis:current recommendations. J. Am. Acad. Orthop. Surg. 2006;14(10 Spec No):S98eS100. doi: 10.5435/00124635-200600001-00023. [DOI] [PubMed] [Google Scholar]
- 7.Panattoni J.B., Ahmed M.M., Busel G.A. An ABC technical algorithm to treat the mangled upper extremity: systematic surgical approach. J Hand Surg Am. 2017 Nov;42(11):934. doi: 10.1016/j.jhsa.2017.08.017. e1-934.e10. [DOI] [PubMed] [Google Scholar]
- 8.Adkinson J.M., Chung K.C. Flap reconstruction of elbow and forearm: a case-based approach. Hand Clin. 2014 May;30(2):153–163. doi: 10.1016/j.hcl.2013.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Togawa S., Yamami N., Nakayama H., Mano Y., Ikegami K., Ozeki S. The validity of the mangled extremity severity score in the assessment of upper limb injuries. J Bone Joint Surg. Br. 2005 Nov;87(11):1516–1519. doi: 10.1302/0301-620X.87B11.16512. [DOI] [PubMed] [Google Scholar]
- 10.Lenarz C.J., Watson J.Y., Moed B.R., Israel H., Mullen J.D., Macdonald J.B. Timing of wound closure in open fractures based on cultures obtained after debridment. J Bone Joint Surg. Am. 2010 Aug;92(10):1921–1926. doi: 10.2106/JBJS.I.00547. 18. [DOI] [PubMed] [Google Scholar]
- 11.Gage M.J., Yoon R.S., Egol K.A., Liporace F.A. Uses of negative pressure wound therapy in orthopedic trauma. Orthop. Clin. N. Am. 2015 Apr;46(2):227–234. doi: 10.1016/j.ocl.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast. Reconstr. Surg. 1986 Sep;78(3):285–292. doi: 10.1097/00006534-198609000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Sundine M., Scheker L.R. A comparison of immediate and staged reconstruction of the dorsum of the hand. J Hand Surg Br. 1996 Apr;21(2):216–221. doi: 10.1016/s0266-7681(96)80102-1. [DOI] [PubMed] [Google Scholar]
- 14.Ali E., Raghuvanshi M. Treatment of open upper limb injuries with infection prevention and negative pressure wound therapy: a systematic review. J. Wound Care. 2017 Dec2;26(12):712–719. doi: 10.12968/jowc.2017.26.12.712. [DOI] [PubMed] [Google Scholar]
- 15.Slavin S.A., Upton J., Kaplan W.D., Van den Abbeele A.D. An investigation of lymphatic function following free-tissue transfer. Plast. Reconstr. Surg. 1997 Mar;99(3):730–741. doi: 10.1097/00006534-199703000-00020. [DOI] [PubMed] [Google Scholar]
- 16.Chim H., Ng Z.Y., Carlsen B.T., Mohan A.T., Saint-Cyr M. Soft tissue coverage of the upper extremity: an overview. Hand Clin. 2014 Nov;30(4):459–473. doi: 10.1016/j.hcl.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 17.Yazar S., Lin C.H., LinYT, Ulusal A.E., Wei F.C. Outcome comparison between free muscle and free fasciocutaneous flap for reconstruction of distal third and ankle traumatic open tibial fractures. Plast. Reconstr. Surg. 2006 Jun;117(7):2468–2475. doi: 10.1097/01.prs.0000224304.56885.c2. [DOI] [PubMed] [Google Scholar]
- 18.Herter F., Ninkovic M., Ninkovic M. Rational flap selection and timing for coverage of complex upper extremity trauma. J. Plast. Reconstr. Aesthetic Surg. 2007;60(7):760–768. doi: 10.1016/j.bjps.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 19.Geddes C.R., Morris S.F., Neligan P.C. Perforator flaps: evolution, classification, and applications. Ann. Plast. Surg. 2003 Jan;50(1):90–99. doi: 10.1097/00000637-200301000-00016. [DOI] [PubMed] [Google Scholar]
- 20.William C. Pederson.Upper extremity microsurgery. Plast. Reconstr. Surg. 2001 May;17(6):1524–1536. [PubMed] [Google Scholar]
- 21.Spindler N., Al-Benna S., Ring A., Homann H., Steinstrasser L., Steinau H.U., Langer S. Free anterolateral thigh flaps for upper extremity soft tissue reconstruction. GMS Interdiscip Plast Reconstr Surg. DGPW. 2015 Feb 5:4. doi: 10.3205/iprs000064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu R., Schindeler A., Little D.G. The potential role of muscle in bone repair. J. Musculoskelet. Neuronal Interact. 2010 Mar;10(1):71–76. [PubMed] [Google Scholar]
- 23.Gosain A., Chang N., Mathes S., Hunt T.K., Vasconez L. A study of the relationship between blood flow and bacterial inoculation in musculocutaneous and fasciocutaneous flaps. Plast. Reconstr. Surg. 1990 Dec;86(6):1152–1162. [PubMed] [Google Scholar]
- 24.Schaverien M.V., Hart A.M. Free muscle flaps for reconstruction of upper limb defects. Hand Clin. 2014 May;30(2):165–183. doi: 10.1016/j.hcl.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 25.Naalla R., Chauhan S., Dave A., Singhal M. Reconstruction of post-traumatic upper extremity soft tissue defects with pedicled flaps: an algorithmic approach to clinical decision making. Chin. J. Traumatol. 2018 Dec;21(6):338–351. doi: 10.1016/j.cjtee.2018.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.El-Sabbagh A.H., Zeina A.A., El-Hadidy A.M., El-Din A.B. Reversed posterior interosseous flap: safe and easy method for hand reconstruction. J Hand Microsurg. 2011 Dec;3(2):66–72. doi: 10.1007/s12593-011-0042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Akdağ O., Yıldıran G., Sütçü M., Karameşe M. Posterior interosseous flap versus reverse adipofascial radial forearm flap for soft tissue reconstruction of dorsal hand defects. Ulus Travma Acil Cerrahi Derg. 2018 Jan;24(1):43–48. doi: 10.5505/tjtes.2017.41196. [DOI] [PubMed] [Google Scholar]
- 28.Biemer E., Stock W. Total thumb reconstruction: a one-stage reconstruction using an osteocutaneous forearm flap. Br. J. Plast. Surg. 1983 Jan;36(1):52–55. doi: 10.1016/0007-1226(83)90011-5. [DOI] [PubMed] [Google Scholar]
- 29.Zancolli E.A., Angrigiani C. Posterior interosseous island forearm flap. J Hand Surg. Br. 1988 May;13(2):130–135. doi: 10.1016/0266-7681_88_90121-0. [DOI] [PubMed] [Google Scholar]
- 30.Bardsley A.F., Soutar D.S., Elliot D., Batchelor A.G. Reducing morbidity in the radial forearm flap donor site. Plast. Reconstr. Surg. 1990 Aug;86(2):287–292. [PubMed] [Google Scholar]
- 31.Lu L.J., Gong X., Lu X.M., Wang K.L. The reverse posterior interosseous flap and its composite flap: experience with 201 flaps. J. Plast. Reconstr. Aesthetic Surg. 2007;60(8):876–882. doi: 10.1016/j.bjps.2006.11.024. [DOI] [PubMed] [Google Scholar]
- 32.McGregor IA, Jackson IT. The groin flap. Br. J. Plast. Surg. 192 Jan; 25(1):3-16. [DOI] [PubMed]
- 33.Miller E.A., Friedrich J. Soft tissue coverage of the hand and upper extremity: the reconstructive elevator. J. Hand Surg. Am. 2016 Jul;41(7):782–792. doi: 10.1016/j.jhsa.2016.04.020. [DOI] [PubMed] [Google Scholar]
- 34.Sabapathy S.R., Bajantri B. Indications, selection, and use of distant pedicled flap for upper limb reconstruction. Hand Clin. 2014 May;30(2):185–199. doi: 10.1016/j.hcl.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 35.Ninkovic M., Schoeller T., Wechselberger G., Otto A., Sperner G., Anderl H. Primary flap closure in complex limb injuries. J. Reconstr. Microsurg. 1997 Nov;13(8):575–583. doi: 10.1055/s-2007-1006440. [DOI] [PubMed] [Google Scholar]
- 36.King E.A., Ozer K. Free skin flap coverage of the upper extremity. Hand Clin. 2014 May;30(2):201–209. doi: 10.1016/j.hcl.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 37.Levin L.S. The reconstructive ladder. An orthoplastic approach. Orthop. Clin North Am. 1993 Jul;24(3):393–409. [PubMed] [Google Scholar]
- 38.Ono S., Sebastin S.J., Yazaki N., Hyakusoku H., Chung K.C. Clinical applications of perforator-based propeller flaps in upper limb soft tissue reconstruction. J. Hand Surg. Am. 2011 May;36(5):853–863. doi: 10.1016/j.jhsa.2010.12.021. [DOI] [PubMed] [Google Scholar]
- 39.Panse N., Sahasrabudhe P. Free style perforator based propeller flaps: simple solutions for upper extremity reconstruction! Indian J. Plast. Surg. 2014 Jan;47(1):77–84. doi: 10.4103/0970-0358.129628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ono S., Sebastin S.J., Ohi H., Chung K.C. Microsurgical flaps in repair and reconstruction of the hand. Hand Clin. 2017 Aug;33(3):425–441. doi: 10.1016/j.hcl.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 41.Samson D., Power D.M. The adipofascial radial artery perforator flap: a versatile reconstructive option in upper limb surgery. Hand Surg. 2015;20(2):266–272. doi: 10.1142/S0218810415500227. [DOI] [PubMed] [Google Scholar]
- 42.Vitse J., Bekara F., Bertheuil N., Sinna R., Chaput B., Herlin C. Perforator-based propeller flaps reliability in upper extremity soft tissue reconstruction: a systematic review. J Hand Surg. Eur. 2017 Feb;42(2):157–164. doi: 10.1177/1753193416669262. [DOI] [PubMed] [Google Scholar]
- 43.Baccarani A., Starnoni M., De Santis G. Ultrasonic cutting and coagulating device in implant-based breast reconstruction. Plast Reconstr Surg Glob Open. 2018;6(11) doi: 10.1097/GOX.0000000000002020. Published. 2018 Nov 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Starnoni M., Pinelli M., De Santis G. Surgical wound infections in plastic surgery: simplified, practical, and standardized selection of high-risk patients. Plast Reconstr Surg Glob Open. 2019;7(4) doi: 10.1097/GOX.0000000000002202. Published. 2019 Apr 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Starnoni M., De Santis G., Pinelli M. Fibula free flap elevation without tourniquet: are harmonic scalpel shears useful? Plast Reconstr Surg Glob Open. 2019;7(9) doi: 10.1097/GOX.0000000000002409. Published. 2019 Sep. 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Starnoni M., Pinelli M., De Santis G. Setting of helium plasma device (J-Plasma) in flap elevation. J Vasc Surg Cases Innov Tech. 2020 Jul 15;6(3):446. doi: 10.1016/j.jvscit.2020.07.008. PMID: 32875177; PMCID: PMC7451687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Benanti E., Starnoni M., Spaggiari A., Pinelli M., De Santis G. Objective selection criteria between ALT and radial forearm flap in oral soft tissues reconstruction. Indian J. Plast. Surg. 2019;52(2):166–170. doi: 10.1055/s-0039-1693504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Starnoni M., Baccarani A., Pinelli M., Pedone A., De Santis G. Tattooing of the nipple-areola complex: what not to do. A case series. Ann Med Surg (Lond). 2020;55:305–307. doi: 10.1016/j.amsu.2020.05.041. Published. 2020 May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]