Abstract
Laryngocele is an uncommon benign cystic dilatation of the laryngeal saccule that communicates with the laryngeal lumen and contains air. On the basis of its localization, it can be traditionally classified in internal, external, or mixed. Usually unilateral and rarely bilateral, it may be congenital or acquired. It most often appears later in life without important symptoms except for cervical swelling. Here, together with a review of literature, we report the case of a 72-year-old man, smoker but without other specific risk factors, who presented laryngeal dyspnea for about one year. Neck CT scan performed during a previous hospitalization for respiratory failure revealed a left mixed laryngocele that was later surgically removed with cervicotomic access. The patient was discharged after one week. One month after surgery, we confirmed the absence of disease with video laryngoscopy.
Keywords: Laryngocele, Mixed laryngocele, Laryngopyocele, Neck mass, Case report
Highlights
-
•
Laryngocele is a rare benign cystic dilatation of laryngeal saccule.
-
•
Conditions increasing intraluminal laryngeal pressure are the main risk factors.
-
•
The diagnosis of laryngocele is essentially clinic, based on symptoms.
-
•
In some cases it can present with acute respiratory failure as pulmonary pathology.
-
•
Treatment is surgical excision, microlaryngoscopic, external or combined.
1. Introduction
Laryngocele is a rare benign cystic dilatation of the laryngeal saccule, a small mucosal pouch situated in the upper part of the ventricle of Morgagni between the ventricular folds, the base of epiglottis, and the inner surface of the thyroid cartilage [1]. Being in communication with the laryngeal lumen, it normally contains air, but may be filled with pus in severe cases; thus, it is termed laryngopyocele [2]. According to the traditional classification, laryngocele can be described as internal (within the larynx), external (outside the larynx), or mixed (both) [1]; however, many authors currently prefer to reduce this classification to only internal and mixed laryngocele [3]. Usually unilateral, laryngocele recognizes several etiologies including congenital, increased intralaryngeal pressure, and mechanical obstruction; it is often asymptomatic and found incidentally on imaging [2]. The treatment of choice is surgical excision [1,3], microlaryngoscopic, external or combined, depending on the laryngocele characteristics.
Here, in line with the SCARE criteria [4], we describe the case of a 72-year-old man smoker but without other specific risk factors, with laryngeal dyspnea for about one year to whom a neck CT-scan performed during a previous hospitalization for respiratory failure showed a left mixed laryngocele; this was further confirmed by video rhinofibrolaryngoscopy. The peculiarities of the case are the absence of any risk factor for laryngocele previously described in literature and its clinical presentation as acute respiratory failure simulating a pulmonary pathology. In addition, we also review the literature about this condition.
2. Case report
A 72-year-old man presented to our attention with a history of laryngeal dyspnea for about one year during hospitalization in another department for respiratory failure. In the context of this hospitalization, a neck CT-scan was performed revealing a left mixed laryngocele (Fig. 1). The patient was a farmer and currently retired; he was a smoker but had a negative history of alcohol consumption. He denied other risk factors for laryngocele. He suffered from high blood pressure and COPD, had already undergone gastroresection for gastric ulcer about 30 years ago and at time of clinic evaluation he denied other symptoms besides dyspnea.
Fig. 1.
Coronal neck-CT scan, showing the mixed left laryngocele.
On examination, he presented a left submandibular mobile mass not painful on palpation that was covered with normal skin (Fig. 2). Video rhinofibrolaryngoscopy showed a smooth-walled cystic swelling occupying the left portion of the supraglottic larynx, from the ariepiglottic fold to the ventricular folds and ventricle of Morgagni. A neck MRI was performed to confirm the diagnosis and better establish the boundaries of the mass: it showed how the laryngocele reached the infero-medial pole of the left submandibular gland causing an extrinsic compression of laryngeal vestibule and a right shift of the glottic lumen (Fig. 3).
Fig. 2.
Left submandibular swelling presented by the patient.
Fig. 3.
Coronal (a) and axial (b) neck-MRI confirming the diagnosis.
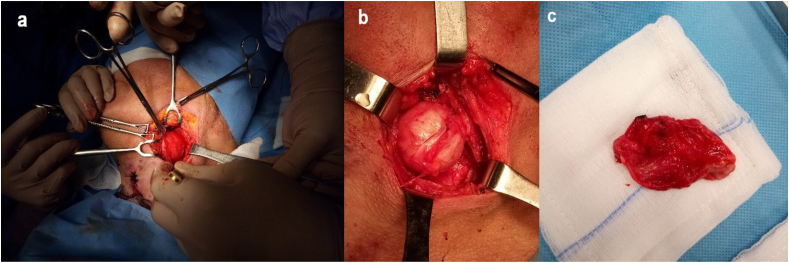
Three days after admission to the otolaryngology department, after adequate written informed consent, surgery was used to excise the laryngocele via cervicotomic access under general anesthesia. The first time consisted of tracheotomy under local anesthesia in order to facilitate the next phase; subsequently, the left submandibular region over the swelling was incised under general anesthesia, dissecting until reaching the thyrohyoid membrane where the laryngocele was isolated and removed entirely (Fig. 4).
Fig. 4.
Phases of surgery: incision (a), isolation of laryngocele (b), removed laryngocele (c).
The subsequent post-operative course was regular and free of complications. The tracheal cannula was removed on day three. On the 7th post-operative day, the patient was discharged in good health and with final histological diagnosis of laryngocele. One month after surgery, the patient attended an outpatient hospital check-up visit in the context of which videoendoscopy established the absence of disease (Fig. 5).
Fig. 5.
Videolaryngoscopy one month after surgery.
3. Discussion
Laryngocele was first described by Larrey (a surgeon in Napoleon's army) in 1829 as “an air-filled tumor” and then by Virchow who gave it the name by which it is known today in 1887 [1]. It is an abnormal cystic dilation of laryngeal saccule [1,2], a small mucosal pouch situated in the upper part of ventricle of Morgagni between the ventricular folds, the base of epiglottis, and the inner surface of thyroid cartilage [1].
Being in communication with laryngeal lumen, laryngocele normally contains air, but by virtue of the presence of mucinous glands in the ventricle, it may contain mucus (laryngomucocele) or, in severe cases of infection, it may be filled with pus (laryngopyocele) [2].
With an incidence of 1 per 2.5 million people per year, laryngocele is a rare clinical entity, five times more common in men than women [5]. It may present at in any age from neonates to the elderly, but the reported peak incidence in the literature is between the fifth and sixth decade of life [1,5]. It is unilateral in about 85% of cases [6] and in more than 8% of cases it turns into a laryngopyocele [7], that is the main complication.
Laryngocele is historically classified as internal when inside the larynx, confined within the thyrohyoid membrane; external if outside the larynx, beyond the thyrohyoid membrane and extended to the subcutaneous tissues of the neck; mixed if it presents both components [2,8]. However, many modern authors prefer to reduce this classification only to internal and mixed laryngocele [2]: therefore, those laryngoceles medial to the thyrohyoid membrane are internal, and mixed those located beyond the membrane [9]. The latter are also the most common type of laryngocele, making up 50% of all [7].
Regarding its etiologies, laryngocele can be both congenital and acquired. It is most often congenital and related to a large ventricle appendix [10]. Among acquired causes, perhaps the most important are all those conditions that lead to an increased intraluminal laryngeal pressure for repeated and prolonged periods: thus, laryngocele is more common in glass blowers and wind instruments players [8]. From this point of view, also mechanical obstructions of the larynx that increase the endoluminal pressure can lead to laryngocele as in the case of laryngeal obstructive carcinoma, especially supraglottic, amyloidosis, chondroma, rheumatoid arthritis, or scleroderma [1,3]. However, adult patients at highest risk for development of laryngocele are usually those with congenitally dilated saccules [10]: in fact, in them also the Valsalva maneuver, that accosts true and false vocal folds increasing intralaryngeal pressure, might exacerbate the congenitally dilated saccule to result in a laryngocele [2]. Nevertheless, all these triggering conditions were absent in the patient subject of case report, for which it was not possible to recognize any known risk factors.
The diagnosis of laryngocele is essentially clinical: its most common symptoms are hoarseness and neck swelling, but it may also present with snoring, upper airway obstruction, increasing stridor, sore throat, cough, pain, globus sensation, and dysphagia [1,3,11]. In our case, patient presented dyspnea and acute respiratory failure like pulmonary pathology. Nevertheless, laryngoceles are very often asymptomatic and therefore diagnosed incidentally with imaging [8] especially CT, which is currently the most accurate imaging modality for their diagnosis [2,8] and in which laryngocele appears as an air-filled structure in the space near the laryngeal saccule. Another diagnostic possibility is MRI, which is useful to define boundaries of the dilatation and its relationship with thyrohyoid membrane, distinguishing internal from external and mixed laryngocele [1]; moreover, MRI can discriminate laryngocele from laryngomucocele, laryngopyocele, and even the eventual underlying laryngeal squamous cell carcinoma [10].
As previously mentioned, the main complication of laryngocele is pyocele, but other complications also include pathogens aspiration with subsequent bronchitis and pneumonia, rupture and following infection in the lateral larynx, and upper airway obstruction [6]: for this last reason, both laryngoceles and laryngopyoceles are possible causes of sudden death [7].
The treatment of choice is surgical excision [1,3] for which different approaches are possible depending on the characteristics of the lesion. For example, smaller internal laryngoceles are managed via microlaryngoscopy with a CO2 laser [1,9], which presents fewer complications and faster post-operative hospitalization [9], but with the disadvantages of limited surgical exposure, post-operative endolaryngeal scarring, and risk of incomplete resection [2,9]. On the contrary, larger or mixed laryngoceles are approached through external access on the lateral neck [1,2]. This last method is preferred for superior exposure, precision, and a low recurrence rate; however, it implies higher morbidity, more complications (edema and subsequent airway impairment, laryngocutaneous fistula, subcutaneous emphysema and nerve injury), longer surgery, and longer recovery time with subsequently increased cost [2]. The external approaches described in the contemporary literature include the transthyrohyoid membrane approach (most common), thyrotomy with resection of the upper 1/3 of thyroid cartilage, and V-shaped thyrotomy. The latter two both offer a superior visualization of the paraglottic space relative to the transthyrohyoid membrane approach [2,9]. To prevent the risk of respiratory distress, a tracheotomy is practiced as a surgical first step in many patients [1], as in our case.
4. Conclusion
In conclusion, laryngocele is a rare condition that recognizes an increased intraluminal laryngeal pressure as main risk factor, absent in our patient. Although its main symptoms, if present, are dysphonia and/or dysphagia, it may also manifest in atypical way, with an acute respiratory failure simulating a pulmonary pathology, as reported in this clinical case. Nevertheless, laryngocele is an asymptomatic condition in most cases, discovered incidentally on imaging, especially on CT, and whose main treatment is surgical through external approaches for mixed laryngoceles and microlaryngoscopic for internal ones.
Informed consent of patient
Written informed consent about surgery and publication of this case report and accompanying images was obtained from the patient and it is on our possess. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer reviewed.
Sources of funding
The authors declare no sources of funding. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
For all procedures performed in case report “Left mixed laryngocele in absence of risk factors: a case report and review of literature”, formal consent of institution's ethics committee is not required.
Author contribution
Bisogno Antonella: data collection; literature review; writing the paper.
Cavaliere Matteo: data analysis and interpretation; correction of the manuscript; surgeon.
Scarpa Alfonso: data analysis and interpretation; correction of the manuscript; surgeon.
Cuofano Rossella: data analysis and interpretation; surgeon.
Troisi Donato: data collection; literature review; surgeon.
Iemma Maurizio: study concept and design; first surgeon; director of Otorhinolaryngology Department.
Registration of research studies
-
1.
Name of the registry:
-
2.
Unique Identifying number or registration ID:
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
Bisogno Antonella.
Declaration of competing interest
The authors declare no conflict of interest.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.amsu.2020.11.024.
Contributor Information
Antonella Bisogno, Email: a.bisogno91@gmail.com.
Matteo Cavaliere, Email: matorl@inwind.it.
Alfonso Scarpa, Email: alfonsoscarpa@yahoo.it.
Rossella Cuofano, Email: cuofanor@gmail.com.
Donato Troisi, Email: donatotroisi@gmail.com.
Maurizio Iemma, Email: iemmahno@gmail.com.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Juneja R., Arora N., Meher R., Mittal P., Passey J.C., Saxena A. Laryngocele: a rare case report and review of literature. Indian J. Otolaryngol. Head Neck Surg. 2019;71(Suppl 1):147–151. doi: 10.1007/s12070-017-1162-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Biswas S., Saran M. Blunt trauma to the neck presenting as dysphonia and dysphagia in a healthy young woman; A rare case of traumatic laryngocele. Bull Emerg Trauma. 2020;8(2):129–131. doi: 10.30476/BEAT.2020.46455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomé R., Thomé D.C., De La Cortina R.A. Lateral thyrotomy approach on the paraglottic space for laryngocele resection. Laryngoscope. 2000;110(3 Pt 1):447–450. doi: 10.1097/00005537-200003000-00023. [DOI] [PubMed] [Google Scholar]
- 4.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A.J., Orgill D.P., for the SCARE Group The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 5.Nikandish R., Zareizadeh A., Motazedian S., Zeraatian S., Zakeri H., Ghaffarpasand F. Bilateral vocal cord paralysis after anterior cervical discectomy following cervical spine injury: a case report. Bull Emerg Trauma. 2013;1(1):43–45. [PMC free article] [PubMed] [Google Scholar]
- 6.Felix J.A., Felix F., Mello L.F. Laryngocele: a cause of upper airway obstruction. Braz J Otorhinolaryngol. 2008;74(1):143–146. doi: 10.1016/s1808-8694(15)30765-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maweni R.M., Jr., Shirazi S., Chatzoudis D., Das S. Laryngopyocoele with contralateral laryngocoele: a rare cause of respiratory distress. BMJ Case Rep. 2018 doi: 10.1136/bcr-2018-225444. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kara İ., Kökoğlu K., Çağlı S., Yüce İ. Bilateral laryngocele causing epiglottic deformity and upper airway obstruction. Turk. Arch. Otolaryngol. 2019;57(2):99–101. doi: 10.5152/tao.2019.3949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zelenik K., Stanikova L., Smatanova K., Cerny M., Kominek P. Treatment of Laryngoceles: what is the progress over the last two decades? BioMed Res. Int. 2014;2014:819453. doi: 10.1155/2014/819453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prasad K.C., Vijayalakshmi S., Prasad S.C. Laryngoceles - presentations and management. Indian J. Otolaryngol. Head Neck Surg. 2008;60(4):303–308. doi: 10.1007/s12070-008-0108-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mobashir M.K., Basha W.M., Mohamed A.E., Hassaan M., Anany A.M. Laryngoceles: concepts of diagnosis and management. Ear Nose Throat J. 2017;96(3):133–138. doi: 10.1177/014556131709600313. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.