Abstract
This article describes supplementary tables and figures associated with the research paper entitled “Impact of referral bias on prognostic studies outcomes: insights from a population-based cohort study on infective endocarditis”. The aforementioned paper is a secondary analysis of data from the EI 2008 cohort on infective endocarditis and aimed at characterising referral bias. A total of 497 patients diagnosed with definite infective endocarditis between January 1st and December 31st 2008 were included in EI 2008. Data were collected from hospital medical records by trained clinical research assistants. Patients were divided into three groups: admitted to a tertiary hospital (group T), admitted to a non-tertiary hospital and referred secondarily to a tertiary hospital (group NTT) or admitted to a non-tertiary hospital and not referred (group NT). The pooled (NTT+T) group mimicked studies recruiting patients in tertiary hospitals only. Two different starting points were considered for follow up: date of first hospital admission and date of first admission to a tertiary hospital if any (hereinafter referred to as “referral time”). Referral bias is a type of selection bias which can occur due to recruitment of patients in tertiary hospitals only (excluding those who are admitted to non-tertiary hospitals and not referred to tertiary hospitals). This bias may impact the description of patients’ characteristics, survival estimates as well as prognostic factors identification. The six tables presented in this paper illustrate how patients’ selection (population-based sample [pooled (NT+NTT+T) group] versus recruitment in tertiary hospitals only [pooled (NTT+T) group]) might impact Hazards Ratios values for prognostic factors. Crude and adjusted Cox regression analyses were first performed to identify prognostic factors associated with 3-month and 1-year mortality in the whole sample using inclusion as the starting point. Analyses were then performed in the pooled (NTT+T) group first using inclusion as the starting point and finally using referral time as the starting point. Figures 1 to 3 illustrate how HR increase with time for covariates that were considered as time-varying covariates (covariate*time interaction).
Keywords: Infective endocarditis, Referral bias, Tertiary hospitals, Prognostic factors, Survival, Selection bias
Specifications Table
| Subject | Medicine |
| Specific subject area | Epidemiology; Infectious Diseases |
| Type of data | Tables and figures |
| How data were acquired | Secondary analysis of data from the EI 2008 cohort on infective endocarditis |
| Data format | Analysed |
| Parameters for data collection | Patients presenting with a diagnosis of definite infective endocarditis (Duke criteria modified by Li) and admitted to a hospital between January 1st 2008 and December 31st 2008 in one of the seven participating French regions were included in the EI 2008 cohort. All the patients included in EI 2008 were considered for our analyses. |
| Description of data collection | Baseline and follow-up data were collected from hospital medical records by trained clinical research assistants and a standardized case report form was completed. Vital status was collected from hospitals medical records, general practitioners’ records or civil registry one year after inclusion in the EI 2008 cohort. |
| Data source location | Institution: CHRU Nancy City/Town/Region: Nancy Country: France Latitude and longitude for collected samples/data: 46.2276° N, 2.2137° E |
| Data accessibility | The datasets generated during and/or analysed during the current study are not publicly available due to restrictions pertaining to the French law, but are available from the corresponding author upon reasonable request. |
| Related research article | Collonnaz M, Erpelding M-L, Alla F, Goehringer F, Delahaye F, Iung B, et al. Impact of referral bias on prognostic studies outcomes: insights from a population-based cohort study on infective endocarditis. Annals of Epidemiology [Internet]. 2020 Sep; Available from: https://doi.org/10.1016/j.annepidem.2020.09.008[1] |
Value of the Data
-
•
Studies recruiting patients in tertiary hospitals only are subject to referral bias. The results presented in the tables are part of a comprehensive analysis of the impact of this bias. They illustrate how referral bias can impact the assessment of the prognostic value of factors associated with 3-month and 1-year mortality from infective endocarditis.
-
•
Practitioners involved in infective endocarditis management as well as public health researchers and epidemiologists may benefit from these data. In addition, any researcher considering an observational study of a rare disease prone to be managed in non-tertiary hospitals at some point may benefit from these data.
-
•
These data may be useful for researchers aiming at characterising the impact of referral bias in studies on infective endocarditis or on other rare diseases. They can also be useful for future research on infective endocarditis as we highlighted the importance on a population-based recruitment of patients.
1. Data Description
The tables are supplementary data associated with the research paper entitled “Impact of referral bias on prognostic studies outcomes: insights from a population-based cohort study on infective endocarditis” [1]. The aforementioned paper is a secondary analysis of data from the EI 2008 cohort and aimed at characterising referral bias.
Tables 1 to 3 refer to the identification of prognostic factors associated with 3-month mortality from infective endocarditis (IE). Tables 4 to 6 refer to the identification of prognostic factors associated with to 1-year mortality.
Table 1.
Factors associated with 3-month mortality in the whole sample (pooled (NT+NTT+T) group) (Starting point=inclusion)
| Whole sample (N=460) |
|||||||
|---|---|---|---|---|---|---|---|
| Crude association |
Adjusted association* |
||||||
| n | HR | 95% CI | p | HR | 95% CI | p | |
| Socio-demographic | |||||||
| Age | <0.001 | <0.001 | |||||
| < 70 | 280 | ref | - | ref | - | ||
| ≥70 | 180 | 2.212 | 1.495-3.274 | 2.350 | 1.535-3.597 | ||
| Sex | 0.226 | ||||||
| Female | 117 | ref | - | ||||
| Male | 343 | 0.771 | 0.505-1.175 | ||||
| Medical history | |||||||
| Charlson Comorbidity index | <0.001 | 0.009 | |||||
| <2 | 248 | ref | - | ref | - | ||
| ≥ 2 | 212 | 2.196 | 1.466-3.288 | 1.760 | 1.150-2.695 | ||
| High blood pressure | 0.006 | ||||||
| No | 242 | ref | - | ||||
| Yes | 218 | 1.741 | 1.172-2.587 | ||||
| Injection drug use | 0.242 | ||||||
| No | 435 | ref | - | ||||
| Yes | 25 | 0.504 | 0.160-1.588 | ||||
| Underlying heart disease (HD) | 0.491 | ||||||
| No previously known HD | 236 | ref | - | ||||
| Previously known HD without prosthetic valve | 125 | 0.818 | 0.505-1.326 | ||||
| Prosthetic valve | 99 | 1.148 | 0.714-1.847 | ||||
| Previous IE | 0.119 | ||||||
| No | 430 | ref | - | ||||
| Yes | 30 | 0.401 | 0.127-1.264 | ||||
| Cardiac implantable electronic device | 0.464 | ||||||
| No | 399 | ref | - | ||||
| Yes | 61 | 1.221 | 0.716-2.082 | ||||
| IE profile | |||||||
| Clinical characteristics | |||||||
| Suspected source of infection | 0.071 | ||||||
| Community | 344 | ref | - | ||||
| Healthcare-related, acquired in hospital | 103 | 1.510 | 0.982-2.323 | ||||
| Healthcare-related, not acquired in hospital | 13 | 2.096 | 0.845-5.201 | ||||
| Left heart endocarditis | 0.390 | ||||||
| No | 90 | ref | - | ||||
| Yes | 370 | 1.257 | 0.747-2.115 | ||||
| Fever | 0.586 | ||||||
| No | 65 | ref | - | ||||
| Yes | 395 | 1.175 | 0.657-2.103 | ||||
| Heart failure | 0.043 | ||||||
| No | 303 | ref | - | ||||
| Yes | 157 | 1.499 | 1.013-2.218 | ||||
| Microbiological characteristics | |||||||
| Staphylococcal IE | <0.001 | 0.010 | |||||
| No | 293 | ref | - | ref | - | ||
| Yes | 167 | 2.500 | 1.691-3.697 | 1.695 | 1.132-2.539 | ||
| Echocardiographic characteristics | |||||||
| Vegetation | 0.625 | ||||||
| No vegetation | 59 | ref | - | ||||
| ≤15mm | 204 | 0.856 | 0.459-1.597 | ||||
| >15mm | 117 | 1.176 | 0.613-2.254 | ||||
| Unknown size of vegetation | 80 | 0.997 | 0.488-2.034 | ||||
| Perforation | 0.445 | ||||||
| No | 375 | ref | - | ||||
| Yes | 85 | 0.812 | 0.476-1.385 | ||||
| IE complications | |||||||
| Cardiac abscess⁎⁎ | 0.048 | ||||||
| No | 361 | ref | - | ||||
| Yes | 99 | 1.677 | 1.005-2.799 | ||||
| Septic shock⁎⁎ | <0.001 | <0.001 | |||||
| No | 385 | ref | - | ref | - | ||
| Yes | 75 | 5.463 | 3.647-8.183 | 3.873 | 2.480-6.049 | ||
| Cerebral haemorrhage⁎⁎ | 0.002 | ||||||
| No | 427 | ref | - | ||||
| Yes | 33 | 2.584 | 1.414-4.724 | ||||
| Cerebral embolism⁎⁎ | <0.001 | <0.001 | |||||
| No | 363 | ref | - | ref | - | ||
| Yes | 97 | 2.619 | 1.721-3.988 | 2.490 | 1.556-3.884 | ||
| Vascular phenomena | 0.083 | ||||||
| No | 242 | ref | - | ||||
| Yes | 218 | 1.412 | 0.956-2.085 | ||||
| Immunologic phenomena | 0.893 | ||||||
| No | 405 | ref | - | ||||
| Yes | 55 | 0.960 | 0.525-1.752 | ||||
| Persistent sepsis despite treatment | 0.085 | ||||||
| No | 410 | ref | - | ||||
| Yes | 50 | 1.599 | 0.938-2.727 | ||||
| Serum creatinine level ≥180 µmol/L | <0.001 | <0.001 | |||||
| No | 327 | ref | - | ref | - | ||
| Yes | 133 | 4.857 | 3.254-7.248 | 3.160 | 2.081-4.797 | ||
Crude and adjusted Cox regressions were performed.
Stepwise selection, sle=0.20, sls=0.05
Time dependent covariate
6 patients from group NTT were excluded from this analysis because they were not referred yet at 3 months.
Table 3.
Factors associated with 3-month mortality in patients who were managed in a tertiary hospital (Pooled (NTT+T) group) (Starting point=referral time)
| Pooled (NTT+T) group (N=410) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Crude association |
Adjusted association+ |
Adjusted association* |
||||||||
| n | HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |
| Socio-demographic | ||||||||||
| Age | 0.001 | <0.001 | <0.001 | |||||||
| < 70 | 261 | ref | - | ref | - | ref | - | |||
| ≥ 70 | 149 | 2.108 | 1.376-3.228 | 2.316 | 1.463-3.666 | 2.316 | 1.463-3.666 | |||
| Sex | ||||||||||
| Female | 100 | ref | - | 0.335 | ||||||
| Male | 310 | 0.793 | 0.494-1.271 | |||||||
| Medical history | ||||||||||
| Charlson Comorbidity index | 0.001 | 0.029 | 0.029 | |||||||
| <2 | 230 | ref | - | ref | - | ref | - | |||
| ≥ 2 | 180 | 2.038 | 1.320-3.145 | 1.662 | 1.054-2.621 | 1.662 | 1.054-2.621 | |||
| High blood pressure | 0.005 | |||||||||
| No | 225 | ref | - | |||||||
| Yes | 185 | 1.857 | 1.206-2.861 | |||||||
| Injection drug use | 0.359 | |||||||||
| No | 386 | ref | - | |||||||
| Yes | 24 | 0.583 | 0.184-1.845 | |||||||
| Underlying heart disease (HD) | 0.399 | |||||||||
| No previously known HD | 212 | ref | - | |||||||
| Previously known HD without prosthetic valve | 107 | 0.762 | 0.441-1.316 | |||||||
| Prosthetic valve | 91 | 1.168 | 0.701-1.945 | |||||||
| Previous IE | 0.196 | |||||||||
| No | 382 | ref | - | |||||||
| Yes | 28 | 0.467 | 0.148-1.479 | |||||||
| Cardiac implantable electronic device | 0.599 | |||||||||
| No | 3511 | ref | - | |||||||
| Yes | 59 | 1.166 | 0.658-2.069 | |||||||
| IE profile | ||||||||||
| Clinical characteristics | ||||||||||
| Suspected source of infection | 0.090 | |||||||||
| Community | 304 | ref | - | |||||||
| Healthcare-related, acquired in hospital | 95 | 1.559 | 0.978-2.486 | |||||||
| Healthcare-related, not acquired in hospital | 11 | 2.082 | 0.754-5.746 | |||||||
| Left heart endocarditis | 0.354 | |||||||||
| No | 82 | ref | - | |||||||
| Yes | 328 | 1.311 | 0.739-2.336 | |||||||
| Fever | 0.374 | |||||||||
| No | 55 | ref | - | |||||||
| Yes | 355 | 1.368 | 0.686-2.730 | |||||||
| Heart failure | 0.085 | |||||||||
| No | 266 | ref | - | |||||||
| Yes | 144 | 1.458 | 0.950-2.239 | |||||||
| Microbiological characteristics | ||||||||||
| Staphylococcal IE | <0.001 | 0.007 | 0.007 | |||||||
| No | 263 | ref | - | ref | - | ref | - | |||
| Yes | 147 | 2.732 | 1.776-4.202 | 1.854 | 1.186-2.899 | 1.854 | 1.186-2.899 | |||
| Echocardiographic characteristics | ||||||||||
| Vegetation | 0.544 | |||||||||
| No vegetation | 52 | ref | - | |||||||
| ≤15mm | 176 | 0.968 | 0.477-1.963 | |||||||
| >15mm | 106 | 1.387 | 0.671-2.866 | |||||||
| Unknown size of vegetation | 76 | 1.036 | 0.465-2.306 | |||||||
| Perforation | 0.443 | |||||||||
| No | 330 | ref | - | |||||||
| Yes | 80 | 0.799 | 0.451-1.418 | |||||||
| IE complications | ||||||||||
| Cardiac abscess⁎⁎ | 0.060 | |||||||||
| No | 315 | ref | - | |||||||
| Yes | 95 | 1. 669 | 0.979-2.846 | |||||||
| Septic shock⁎⁎ | <0.001 | <0.001 | <0.001 | |||||||
| No | 345 | ref | . | ref | - | ref | - | |||
| Yes | 65 | 5.057 | 3.239-7.894 | 3.462 | 2.119-5.657 | 3.462 | 2.119-5.657 | |||
| Cerebral haemorrhage⁎⁎ | 0.001 | |||||||||
| No | 381 | ref | - | |||||||
| Yes | 29 | 2.830 | 1.500-5.336 | |||||||
| Cerebral embolism⁎⁎ | <0.001 | <0.001 | <0.001 | |||||||
| No | 321 | ref | - | ref | - | ref | - | |||
| Yes | 89 | 2.579 | 1.638-4.061 | 2.518 | 1.544-4.105 | 2.518 | 1.544-4.105 | |||
| Vascular phenomena | 0.181 | |||||||||
| No | 214 | ref | - | |||||||
| Yes | 196 | 1.338 | 0.874-2.051 | |||||||
| Immunologic phenomena | 0.674 | |||||||||
| No | 359 | ref | - | |||||||
| Yes | 51 | 1.140 | 0.619-2.099 | |||||||
| Persistent sepsis despite treatment | 0.160 | |||||||||
| No | 364 | ref | . | |||||||
| Yes | 46 | 1.528 | 0.846-2.758 | |||||||
| Serum creatinine level ≥180 µmol/L | <0.001 | <0.001 | <0.001 | |||||||
| No | 291 | ref | - | ref | - | ref | - | |||
| Yes | 119 | 4.683 | 3.024-7.251 | 3.133 | 1.990-4.932 | 3.133 | 1.990-4.932 | |||
Crude and adjusted Cox regressions were performed.
Stepwise selection, sle=0.20, sls=0.05
Covariates resulting from the selection process in the whole sample were forced into the model
Time dependent covariate
Table 4.
Factors associated with 1-year mortality in the whole sample (pooled (NT+NTT+T) group) (Starting point=inclusion)
| Whole sample (N=466) |
|||||||
|---|---|---|---|---|---|---|---|
| Crude association |
Adjusted association* |
||||||
| n | HR | 95% CI | p | HR | 95% CI | p | |
| Socio-demographic | |||||||
| Age | <0.001 | <0.001 | |||||
| < 70 | 285 | ref | - | ref | - | ||
| ≥70 | 181 | 2.495 | 1.764-3.529 | 2.402 | 1.653-3.489 | ||
| Sex | 0.103 | ||||||
| Female | 118 | ref | - | ||||
| Male | 348 | 0.736 | 0.509-1.064 | ||||
| Medical history | |||||||
| Charlson Comorbidity index⁎⁎⁎ | <0.001 | 0.001 | |||||
| <2 | 252 | ref | - | ref | - | ||
| ≥ 2 | 214 | 1.011 | 1.006-1.016 | 1.008 | 1.003-1.013 | ||
| High blood pressure⁎⁎⁎ | <0.001 | 0.006 | |||||
| No | 245 | ref | - | ref | - | ||
| Yes | 221 | 1.008 | 1.004-1.012 | 1.006 | 1.002-1.010 | ||
| Injection drug use | 0.079 | ||||||
| No | 440 | ref | - | ||||
| Yes | 26 | 0.358 | 0.114-1.125 | ||||
| Underlying heart disease (HD) | 0.806 | ||||||
| No previously known HD | 240 | ref | - | ||||
| Previously known HD without prosthetic valve | 126 | 0.887 | 0.588-1.338 | ||||
| Prosthetic valve | 100 | 1.029 | 0.667-1.587 | ||||
| Previous IE | 0.078 | ||||||
| No | 436 | ref | - | ||||
| Yes | 30 | 0.408 | 0.151-1.105 | ||||
| Cardiac implantable electronic device | 0.276 | ||||||
| No | 403 | ref | - | ||||
| Yes | 63 | 1.289 | 0.816-2.038 | ||||
| IE profile | |||||||
| Clinical characteristics | |||||||
| Suspected source of infection | 0.033 | ||||||
| Community | 348 | ref | - | ||||
| Healthcare-related, acquired in hospital | 105 | 1.540 | 1.055-2.246 | ||||
| Healthcare-related, not acquired in hospital | 13 | 2.010 | 0.879-4.599 | ||||
| Left heart endocarditis | 0.471 | ||||||
| No | 93 | ref | - | ||||
| Yes | 373 | 1.177 | 0.756-1.831 | ||||
| Fever | 0.559 | ||||||
| No | 66 | ref | - | ||||
| Yes | 400 | 1.164 | 0.699-1.937 | ||||
| Heart failure⁎⁎⁎ | 0.001 | 0.027 | |||||
| No | 307 | ref | - | ref | - | ||
| Yes | 159 | 1.006 | 1.002-1.009 | 1.004 | 1.000-1.007 | ||
| Microbiological characteristics | |||||||
| Staphylococcal IE | <0.001 | 0.004 | |||||
| No | 297 | ref | - | ref | - | ||
| Yes | 169 | 2.179 | 1.548-3.067 | 1.679 | 1.177-2.395 | ||
| Echocardiographic characteristics | |||||||
| Vegetation | 0.885 | ||||||
| No vegetation | 59 | ref | - | ||||
| ≤15mm | 207 | 1.051 | 0.596-1.855 | ||||
| >15mm | 119 | 1.221 | 0.669-2.231 | ||||
| Unknown size of vegetation | 81 | 1.099 | 0.573-2.106 | ||||
| Perforation | 0.143 | 0.020 | |||||
| No | 381 | ref | - | ref | - | ||
| Yes | 85 | 0.690 | 0.420-1.134 | 0.545 | 0.327-0.909 | ||
| IE complications | |||||||
| Cardiac abscess⁎⁎ | 0.283 | ||||||
| No | 367 | ref | - | ||||
| Yes | 99 | 1.299 | 0.806-2.096 | ||||
| Septic shock⁎⁎ | <0.001 | <0.001 | |||||
| No | 390 | ref | - | ref | - | ||
| Yes | 76 | 4.129 | 2.840-6.003 | 3.360 | 2.211-5.104 | ||
| Cerebral haemorrhage⁎⁎ | 0.015 | ||||||
| No | 433 | ref | - | ||||
| Yes | 33 | 2.042 | 1.151-3.622 | ||||
| Cerebral embolism⁎⁎ | <0.001 | <0.001 | |||||
| No | 369 | ref | - | ref | - | ||
| Yes | 97 | 2.256 | 1.545-3.293 | 2.324 | 1.556-3.469 | ||
| Vascular phenomena⁎⁎⁎ | 0.182 | ||||||
| No | 246 | ref | - | ||||
| Yes | 220 | 0.998 | 0.094-1.001 | ||||
| Immunologic phenomena | 0.272 | ||||||
| No | 411 | ref | - | ||||
| Yes | 55 | 0.717 | 0.396-1.298 | ||||
| Persistent sepsis despite treatment | 0.091 | ||||||
| No | 416 | ref | - | ||||
| Yes | 50 | 1.521 | 0.936-2.474 | ||||
| Serum creatinine level ≥180 µmol/L | <0.001 | <0.001 | |||||
| No | 333 | ref | - | ref | - | ||
| Yes | 133 | 3.996 | 2.832-5.638 | 2.780 | 1.944-3.977 | ||
Crude and adjusted Cox regressions were performed.
Stepwise selection, sle=0.20, sls=0.05
Time dependent covariate
Time-varying covariate (interaction with time)
Table 6.
Factors associated with 1-year mortality in patients who were managed in a tertiary hospital (Pooled (NTT+T) group) (Starting point=referral time)
| Pooled (NTT+T) group (N=410) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Crude association |
Adjusted association+ |
Adjusted association* |
||||||||
| n | HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |
| Socio-demographic | ||||||||||
| Age | <0.001 | <0.001 | <0.001 | |||||||
| < 70 | 261 | ref | - | ref | - | ref | - | |||
| ≥ 70 | 149 | 2.343 | 1.586-3.462 | 2.310 | 1.520-3.511 | 2.317 | 1.526-3.518 | |||
| Sex | 0.261 | |||||||||
| Female | 100 | ref | - | |||||||
| Male | 310 | 0.781 | 0.508-1.201 | |||||||
| Medical history | ||||||||||
| Charlson Comorbidity index⁎⁎⁎ | 0.003 | 0.036 | 0.022 | |||||||
| <2 | 230 | ref | - | ref | - | ref | - | |||
| ≥ 2 | 180 | 1.008 | 1.003-1.013 | 1.005 | 1.000-1.010 | 1.006 | 1.001-1.011 | |||
| High blood pressure⁎⁎⁎ | 0.001 | 0.005 | 0.004 | |||||||
| No | 225 | ref | - | ref | - | ref | - | |||
| Yes | 185 | 1.011 | 1.005-1.018 | 1.009 | 1.003-1.016 | 1.009 | 1.003-1.016 | |||
| Injection drug use | 0.201 | |||||||||
| No | 386 | ref | - | |||||||
| Yes | 24 | 0.473 | 0.150-1.491 | |||||||
| Underlying heart disease (HD) | 0.453 | |||||||||
| No previously known HD | 212 | ref | - | |||||||
| Previously known HD without prosthetic valve | 107 | 0.823 | 0.505-1.343 | |||||||
| Prosthetic valve | 91 | 1.180 | 0.738-1.887 | |||||||
| Previous IE | 0.193 | |||||||||
| No | 382 | ref | - | |||||||
| Yes | 28 | 0.515 | 0.190-1.400 | |||||||
| Cardiac implantable electronic device | 0.507 | |||||||||
| No | 351 | ref | - | |||||||
| Yes | 59 | 1.193 | 0.709-2.008 | |||||||
| IE profile | ||||||||||
| Clinical characteristics | ||||||||||
| Suspected source of infection | 0.039 | |||||||||
| Community | 304 | ref | - | |||||||
| Healthcare-related, acquired in hospital | 95 | 1.581 | 1.031-2.422 | |||||||
| Healthcare-related, not acquired in hospital | 11 | 2.239 | 0.902-5.558 | |||||||
| Left heart endocarditis | 0.324 | |||||||||
| No | 82 | ref | - | |||||||
| Yes | 328 | 1.300 | 0.772-2.188 | |||||||
| Fever | 0.520 | |||||||||
| No | 55 | ref | - | |||||||
| Yes | 355 | 1.219 | 0.667-2.226 | |||||||
| Heart failure⁎⁎⁎ | 0.006 | 0.081 | ||||||||
| No | 266 | ref | - | ref | - | |||||
| Yes | 144 | 1.006 | 1.002-1.011 | 1.004 | 1.000-1.008 | |||||
| Microbiological characteristics | ||||||||||
| Staphylococcal IE | <0.001 | 0.020 | 0.017 | |||||||
| No | 263 | ref | - | ref | - | ref | - | |||
| Yes | 147 | 2.225 | 1.508-3.283 | 1.618 | 1.079-2.426 | 1.633 | 1.092-2.443 | |||
| Echocardiographic characteristics | ||||||||||
| Vegetation | 0.729 | |||||||||
| No vegetation | 52 | ref | - | |||||||
| ≤15mm | 176 | 1.153 | 0.594-2.235 | |||||||
| >15mm | 106 | 1.413 | 0.708-2.820 | |||||||
| Unknown size of vegetation | 76 | 1.131 | 0.534-2.394 | |||||||
| Perforation | 0.118 | 0.038 | ||||||||
| No | 330 | ref | - | ref | - | |||||
| Yes | 80 | 0.638 | 0.363-1.121 | 0.543 | 0.305-0.966 | |||||
| IE complications | ||||||||||
| Cardiac abscess⁎⁎ | 0.132 | |||||||||
| No | 315 | ref | - | |||||||
| Yes | 95 | 1.469 | 0.891-2.422 | |||||||
| Septic shock⁎⁎ | <0.001 | <0.001 | <0.001 | |||||||
| No | 345 | ref | - | ref | - | ref | - | |||
| Yes | 65 | 4.086 | 2.679-6.233 | 2.847 | 1.754-4.621 | 2.766 | 1.721-4.445 | |||
| Cerebral haemorrhage⁎⁎ | 0.003 | |||||||||
| No | 381 | ref | - | |||||||
| Yes | 29 | 2.494 | 1.364-4.558 | |||||||
| Cerebral embolism⁎⁎ | <0.001 | <0.001 | <0.001 | |||||||
| No | 321 | ref | - | ref | - | ref | - | |||
| Yes | 89 | 2.336 | 1.536-3.555 | 2.499 | 1.581-3.949 | 2.551 | 1.615-4.029 | |||
| Vascular phenomena⁎⁎⁎ | 0.168 | |||||||||
| No | 214 | ref | - | |||||||
| Yes | 196 | 0.997 | 0.993-1.001 | |||||||
| Immunologic phenomena | 0.810 | |||||||||
| No | 359 | ref | - | |||||||
| Yes | 51 | 0.929 | 0.509-1.697 | |||||||
| Persistent sepsis despite treatment | 0.171 | |||||||||
| No | 364 | ref | - | |||||||
| Yes | 46 | 1.466 | 0.848-2.536 | |||||||
| Serum creatinine level ≥180 µmol/L | <0.001 | <0.001 | <0.001 | |||||||
| No | 291 | ref | - | ref | - | ref | - | |||
| Yes | 119 | 4.113 | 2.776-6.095 | 3.085 | 2.053-4.634 | 3.055 | 2.031-4.594 | |||
Crude and adjusted Cox regressions were performed.
Stepwise selection, sle=0.20, sls=0.05
Covariates resulting from the selection process in the whole sample were forced into the model
Time dependent covariate
Time-varying covariate (interaction with time)
Tables 1 and 4 present absolute frequency, crude and adjusted Hazards Ratios (HR) when using the whole sample of patients (pooled (NT+NTT+T) group) and using the date of inclusion (date of first admission to hospital for IE) as the starting point for analyses.
Tables 2 and 5 present absolute frequency, crude and adjusted HRs obtained when performing analyses on a sample of patients recruited in tertiary hospitals only (pooled (NTT+T) group) using date of inclusion as the starting point.
Table 2.
Factors associated with 3-month mortality in patients who were managed in a tertiary hospital (Pooled (NTT+T) group) (Starting point=inclusion)
| Pooled (NTT+T) group (N=404) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Crude association |
Adjusted association+ |
Adjusted association* |
||||||||
| n | HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |
| Socio-demographic | ||||||||||
| Age | 0.001 | <0.001 | <0.001 | |||||||
| < 70 | 256 | ref | - | ref | - | ref | - | |||
| ≥ 70 | 148 | 2.085 | 1.361-3.193 | 2.368 | 1.494-3.755 | 2.368 | 1.494-3.755 | |||
| Sex | 0.391 | |||||||||
| Female | 99 | ref | - | |||||||
| Male | 305 | 0.813 | 0.507-1.304 | |||||||
| Medical history | ||||||||||
| Charlson Comorbidity index | 0.002 | 0.020 | 0.020 | |||||||
| <2 | 226 | ref | - | ref | - | ref | - | |||
| ≥ 2 | 178 | 2.011 | 1.303-3.105 | 1.712 | 1.087-2.699 | 1.712 | 1.087-2.699 | |||
| High blood pressure | 0.005 | |||||||||
| No | 222 | ref | - | |||||||
| Yes | 182 | 1.851 | 1.202-2.852 | |||||||
| Injection drug use | 0.362 | |||||||||
| No | 381 | ref | - | |||||||
| Yes | 23 | 0.585 | 0.185-1.851 | |||||||
| Underlying heart disease (HD) | 0.379 | |||||||||
| No previously known HD | 208 | ref | - | |||||||
| Previously known HD without prosthetic valve | 106 | 0.747 | 0.433-1.291 | |||||||
| Prosthetic valve | 90 | 1.157 | 0.695-1.926 | |||||||
| Previous IE | 0.182 | |||||||||
| No | 376 | ref | - | |||||||
| Yes | 28 | 0.457 | 0.144-1.445 | |||||||
| Cardiac implantable electronic device | 0.531 | |||||||||
| No | 347 | ref | - | |||||||
| Yes | 57 | 1.201 | 0.677-2.130 | |||||||
| IE profile | ||||||||||
| Clinical characteristics | ||||||||||
| Suspected source of infection | 0.100 | |||||||||
| Community | 300 | ref | - | |||||||
| Healthcare-related, acquired in hospital | 93 | 1.541 | 0.967-2.457 | |||||||
| Healthcare-related, not acquired in hospital | 11 | 2.061 | 0.747-5.687 | |||||||
| Left heart endocarditis | 0.384 | |||||||||
| No | 79 | ref | - | |||||||
| Yes | 325 | 1.290 | 0.727-2.288 | |||||||
| Fever | 0.361 | |||||||||
| No | 54 | ref | - | |||||||
| Yes | 350 | 1.380 | 0.692-2.754 | |||||||
| Heart failure | 0.088 | |||||||||
| No | 262 | ref | - | |||||||
| Yes | 142 | 1.452 | 0.946-2.229 | |||||||
| Microbiological characteristics | ||||||||||
| Staphylococcal IE | <0.001 | 0.006 | 0.006 | |||||||
| No | 259 | ref | - | ref | - | ref | - | |||
| Yes | 145 | 2.733 | 1.777-4.204 | 1.863 | 1.191-2.914 | 1.863 | 1.191-2.914 | |||
| Echocardiographic characteristics | ||||||||||
| Vegetation | 0.495 | |||||||||
| No vegetation | 52 | ref | - | |||||||
| ≤15mm | 173 | 0.965 | 0.476-1.958 | |||||||
| >15mm | 104 | 1.414 | 0.685-2.922 | |||||||
| Unknown size of vegetation | 75 | 1.045 | 0.470-2.326 | |||||||
| Perforation | 0.396 | |||||||||
| No | 324 | ref | - | |||||||
| Yes | 80 | 0.780 | 0.440-1.384 | |||||||
| IE complications | ||||||||||
| Cardiac abscess⁎⁎ | 0.022 | |||||||||
| No | 309 | ref | - | |||||||
| Yes | 95 | 1.869 | 1.094-3.193 | |||||||
| Septic shock⁎⁎ | <0.001 | <0.001 | <0.001 | |||||||
| No | 340 | ref | - | ref | - | ref | - | |||
| Yes | 64 | 5.288 | 3.387-8.254 | 3.622 | 2.209-5.937 | 3.622 | 2.209-5.937 | |||
| Cerebral haemorrhage⁎⁎ | 0.001 | |||||||||
| No | 375 | ref | - | |||||||
| Yes | 29 | 2.941 | 1.559-5.548 | |||||||
| Cerebral embolism⁎⁎ | <0.001 | <0.001 | <0.001 | |||||||
| No | 315 | ref | - | ref | - | ref | - | |||
| Yes | 89 | 2.618 | 1.662-4.125 | 2.563 | 1.567-4.190 | 2.563 | 1.567-4.190 | |||
| Vascular phenomena | 0.193 | |||||||||
| No | 210 | ref | - | |||||||
| Yes | 194 | 1.328 | 0.866-2.034 | |||||||
| Immunologic phenomena | 0.711 | |||||||||
| No | 353 | ref | - | |||||||
| Yes | 51 | 1.123 | 0.610-2.067 | |||||||
| Persistent sepsis despite treatment | 0.219 | |||||||||
| No | 358 | ref | - | |||||||
| Yes | 46 | 1.449 | 0.803-2.615 | |||||||
| Serum creatinine level ≥180 µmol/L | <0.001 | <0.001 | <0.001 | |||||||
| No | 285 | ref | - | ref | - | ref | - | |||
| Yes | 119 | 4.533 | 2.928-7.019 | 3.048 | 1.935-4.799 | 3.048 | 1.935-4.799 | |||
Crude and adjusted Cox regressions were performed.
Stepwise selection, sle=0.20, sls=0.05
Covariates resulting from the selection process in the whole sample were forced into the model
Time dependent covariate
6 patients from group NTT were excluded from this analysis because they were not referred yet at 3 months.
Table 5.
Factors associated with 1-year mortality in patients who were managed in a tertiary hospital (Pooled (NTT+T) group) (Starting point=inclusion)
| Pooled (NTT+T) group (N=410) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Crude association |
Adjusted association+ |
Adjusted association* | ||||||||
| n | HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |
| Socio-demographic | ||||||||||
| Age | <0.001 | <0.001 | <0.001 | |||||||
| < 70 | 261 | ref | - | ref | - | ref | - | |||
| ≥ 70 | 149 | 2.253 | 1.543-3.290 | 2.193 | 1.460-3.293 | 2.193 | 1.460-3.293 | |||
| Sex | 0.271 | |||||||||
| Female | 100 | ref | - | |||||||
| Male | 310 | 0.791 | 0.521-1.200 | |||||||
| Medical history | ||||||||||
| Charlson Comorbidity index⁎⁎⁎ | 0.005 | 0.005 | ||||||||
| <2 | 230 | ref | - | <0.001 | ref | - | ref | - | ||
| ≥ 2 | 180 | 1.009 | 1.005-1.014 | 1.007 | 1.002-1.012 | 1.007 | 1.002-1.012 | |||
| High blood pressure⁎⁎⁎ | 0.007 | 0.007 | ||||||||
| No | 225 | ref | - | <0.001 | ref | - | ref | - | ||
| Yes | 185 | 1.008 | 1.004-1.013 | 1.006 | 1.002-1.011 | 1.006 | 1.002-1.011 | |||
| Injection drug use | 0.144 | |||||||||
| No | 386 | ref | - | |||||||
| Yes | 24 | 0.425 | 0.135-1.340 | |||||||
| Underlying heart disease (HD) | 0.664 | |||||||||
| No previously known HD | 212 | ref | - | |||||||
| Previously known HD without prosthetic valve | 107 | 0.862 | 0.541-1.373 | |||||||
| Prosthetic valve | 91 | 1.106 | 0.694-1.760 | |||||||
| Previous IE | 0.149 | |||||||||
| No | 382 | ref | - | |||||||
| Yes | 28 | 0.479 | 0.177-1.302 | |||||||
| Cardiac implantable electronic device | 0.341 | |||||||||
| No | 351 | ref | - | |||||||
| Yes | 59 | 1.272 | 0.775-2.088 | |||||||
| IE profile | ||||||||||
| Clinical characteristics | ||||||||||
| Suspected source of infection | 0.075 | |||||||||
| Community | 304 | ref | - | |||||||
| Healthcare-related, acquired in hospital | 95 | 1.484 | 0.978-2.253 | |||||||
| Healthcare-related, not acquired in hospital | 11 | 2.071 | 0.836-5.129 | |||||||
| Left heart endocarditis | 0.268 | |||||||||
| No | 82 | ref | - | |||||||
| Yes | 328 | 1.331 | 0.802-2.208 | |||||||
| Fever | 0.362 | |||||||||
| No | 55 | ref | - | |||||||
| Yes | 355 | 1.322 | 0.725-2.408 | |||||||
| Heart failure⁎⁎⁎ | <0.001 | 0.017 | 0.017 | |||||||
| No | 266 | ref | - | ref | - | ref | - | |||
| Yes | 144 | 1.007 | 1.003-1.011 | 1.005 | 1.001-1.009 | 1.005 | 1.001-1.009 | |||
| Microbiological characteristics | ||||||||||
| Staphylococcal IE | <0.001 | 0.015 | 0.015 | |||||||
| No | 263 | ref | - | ref | - | ref | - | |||
| Yes | 147 | 2.153 | 1.476-3.141 | 1.634 | 1.102-2.423 | 1.634 | 1.102-2.423 | |||
| Echocardiographic characteristics | ||||||||||
| Vegetation | 0.607 | |||||||||
| No vegetation | 52 | ref | - | |||||||
| ≤15mm | 176 | 1.221 | 0.633-2.358 | |||||||
| >15mm | 106 | 1.523 | 0.768-3.022 | |||||||
| Unknown size of vegetation | 76 | 1.191 | 0.567-2.503 | |||||||
| Perforation | 0.178 | 0.047 | 0.047 | |||||||
| No | 330 | ref | - | ref | - | ref | - | |||
| Yes | 80 | 0.694 | 0.408-1.181 | 0.574 | 0.332-0.992 | 0.574 | 0.332-0.992 | |||
| IE complications | ||||||||||
| Cardiac abscess⁎⁎ | 0.116 | |||||||||
| No | 315 | ref | - | |||||||
| Yes | 95 | 1.491 | 0.906-2.455 | |||||||
| Septic shock⁎⁎ | <0.001 | <0.001 | <0.001 | |||||||
| No | 345 | ref | - | ref | - | ref | - | |||
| Yes | 65 | 3.962 | 2.610-6.013 | 2.991 | 1.874-4.773 | 2.991 | 1.874-4.773 | |||
| Cerebral haemorrhage⁎⁎ | 0.005 | |||||||||
| No | 381 | ref | - | |||||||
| Yes | 29 | 2.386 | 1.308-4.352 | |||||||
| Cerebral embolism⁎⁎ | <0.001 | <0.001 | <0.001 | |||||||
| No | 321 | ref | - | ref | - | ref | - | |||
| Yes | 89 | 2.184 | 1.443-3.307 | 2.266 | 1.452-3.535 | 2.266 | 1.452-3.535 | |||
| Vascular phenomena⁎⁎⁎ | 0.105 | |||||||||
| No | 214 | ref | - | |||||||
| Yes | 196 | 0.997 | 0.993-1.001 | |||||||
| Immunologic phenomena | 0.624 | |||||||||
| No | 359 | ref | - | |||||||
| Yes | 51 | 0.861 | 0.472-1.568 | |||||||
| Persistent sepsis despite treatment | 0.166 | |||||||||
| No | 364 | ref | - | |||||||
| Yes | 46 | 1.455 | 0.856-2.475 | |||||||
| Serum creatinine level ≥180 µmol/L | <0.001 | <0.001 | <0.001 | |||||||
| No | 291 | ref | - | ref | - | ref | - | |||
| Yes | 119 | 3.942 | 2.693-5.770 | 2.882 | 1.941-4.278 | 2.882 | 1.941-4.278 | |||
Crude and adjusted Cox regressions were performed.
Stepwise selection, sle=0.20, sls=0.05
Covariates resulting from the selection process in the whole sample were forced into the model
Time dependent covariate
Time-varying covariate (interaction with time)
Tables 3 and 6 present absolute frequency, crude and adjusted HRs obtained when recruiting patients in tertiary hospitals only (pooled (NTT+T) group) using referral time (the date of first admission to a tertiary hospital if any) as the starting point.
A total of six prognostic factors were associated with 3-month mortality (age ≥70, Charlson comorbidity index ≥2, Staphylococcal IE, septic shock, cerebral embolism, and serum creatinine level ≥18 μmol/L). The prognostic factors did not differ across groups; however, the values of HRs associated with these prognostic factors were influenced by sample and starting point selection.
When using the date of inclusion as the starting point, a total of nine prognostic factors were associated with 1-year mortality in the whole sample and in the pooled (NTT+T) group (age ≥70, Charlson comorbidity index ≥2*time, high blood pressure*time, heart failure*time, Staphylococcal IE, valve perforation, septic shock, cerebral embolism, and serum creatinine level ≥180 μmol/L). When using referral time as the starting point, heart failure and valve perforation were no longer identified as prognostic factors.
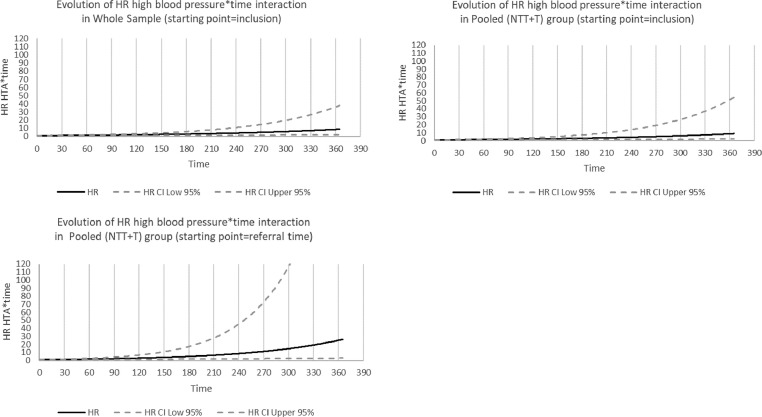
Figs. 1 to 3 represent the evolution of Hazard Ratios with time (in days) for the three covariates (Charlson comorbidity index ≥2, high blood pressure and heart failure) that did not meet the proportional hazard assumption and were included in 1-year survival models as time-varying covariates (considering covariate*time interaction). Figs. 1 to 3 show how HR for these covariates increased with time. For example, for Charlson comorbidity index ≥2, the risk of death from IE in the whole sample was multiplied by 1.27 [1.09–1.47] after one month and by 1.61 [1.20–2.17] after two months. Noteworthy, 95% confidence intervals width also increased with time, showing a loss of precision in HR estimates over time.
Fig. 2.
Evolution over time of Hazard Ratios for the association between high blood pressure and one-year mortality.
Fig. 1.
Evolution over time of Hazard Ratios for the association between Charlson comorbidity index ≥2 and one-year mortality.
Fig. 3.
Evolution over time of Hazard Ratios for the association between heart failure and one-year mortality.
2. Experimental Design, Materials and Methods
2.1. The EI 2008 cohort
2.1.1. Background
We used data from EI 2008, a one-year prospective, population based, cohort study of patients with IE [2]. Inclusion criteria in EI 2008 were: being over 18 years old, living in one of the seven participating French administrative areas (greater Paris, Lorraine, Rhône-Alpes, Franche-Comté, Marne, Ille-et-Villaine and Languedoc- Roussillon), and being admitted to hospital for IE between January 1st 2008 and December 31st 2008. Diagnosis of IE was adjudicated by a team of infectious diseases professionals. Definite cases of IE (Duke criteria modified by Li [3]) were included in the cohort. Patients were followed during one year after inclusion. Baseline and follow-up data were collected on a standardised case report form by trained clinical research assistants. Information on patients’ characteristics, IE profiles, treatment and complications were retrieved from hospital medical records. Vital status was assessed from hospital medical records, general practitioners’ records or civil registry office 1 year after inclusion, and date of death was collected when appropriate.
All the patients enrolled in the EI 2008 cohort (497 patients with a definite diagnosis of IE) were considered for our analyses.
2.1.2. Data collection
Patients were divided into three groups: patients admitted to a tertiary hospital (group T), patients admitted to a non-tertiary hospital and secondarily referred to a tertiary hospital (group NTT), and patients admitted to a non-tertiary hospital and not secondarily referred to a tertiary hospital (group NT).
Baseline data consisted of sociodemographic characteristics (age ≥70, sex) and medical history data (Charlson comorbidity index ≥2, high blood pressure, injection drug use, underlying heart disease, previous IE and implantable cardiac device). Data on IE profile and IE complications were collected during follow-up in hospital stay. IE profile data included clinical characteristics (suspected source of infection, left heart endocarditis, fever and heart failure), microbiological characteristics (Staphylococcal IE), and echocardiographic characteristics (vegetation and perforation). IE complications data consisted of cardiac abscess, septic shock, cerebral haemorrhage, cerebral embolism, vascular phenomena, immunologic phenomena, persistent sepsis despite treatment, and serum creatinine level ≥180 µmol/L.
2.2. Secondary analysis of EI 2008 data
2.2.1. Aim of the study
We used data from the EI 2008 cohort to provide a comprehensive characterisation of referral bias [1]. Referral bias is a type of selection bias that can occur in studies recruiting patients in tertiary hospitals only (mixing patients admitted directly to tertiary hospitals and those referred secondarily to tertiary hospitals, but excluding patients admitted to non-tertiary hospitals and not referred). Studies on rare diseases such as infective endocarditis are particularly prone to referral bias [4], [5], [6], a bias which may threaten the validity of prognostic studies’ results [7].
2.2.2. Data analyses
The whole sample (pooled (NT+NTT+T) group) represented a population-based recruitment of patients with IE. The pooled (NTT+T) group was used to mimic prognostic studies recruiting patients in tertiary hospitals.
Two different starting points were considered for the follow-up: inclusion (corresponding to the date of first hospital admission) and referral time (corresponding to the date of first admission to a tertiary hospital if any, i.e. used for groups T and NTT only to mimic prognostic studies based on patients recruited in tertiary hospitals only). Survival time was calculated from the starting point to the date of death or to the date of last follow-up.
All variables mentioned in data collection were evaluated for their potential prognostic impact. Patients with missing data for at least one of these potential prognostic factors were excluded from analyses (after checking that the characteristics of excluded patients did not differ significantly from those of included patients). One patient (patient number 560) was excluded from analyses due to a negative delay between hospital admission and septic shock (covariate introduced in Cox analyses as a time-dependent covariate). As a result, a total of 466 patients with infective endocarditis were included in the Cox analyses (274 in group T (58,8%), 136 in group NTT (29,2%) and 56 in group NT (12,0%)).
Data presented in tables 1 to 6 were obtained through crude and adjusted Cox modelling of 3-month and 1-year survival from IE. For both 3-months and 1-year survival, analyses were performed in five steps:
1/ In the pooled (NT+NTT+T) group, i.e. a population-based sample, using inclusion as the starting point, a stepwise selection (with a significance level for entry (sle) set at 0.20 and a significance level for staying in the model (sls) set at 0.05) was performed to identify prognostic factors
2/ In the pooled (NTT+T), using inclusion as the starting point, covariates identified as prognostic factors in Step 1 were forced into the multivariable model to identify an eventual difference in significance or in the magnitude of HRs
3/ In the pooled (NTT+T) group, using inclusion as the starting point, a stepwise selection (sle=0.20 and sls=0.05) was performed to naively identify prognostic factors
4/ In the pooled (NTT+T) group, using referral time as the starting point, covariates identified as prognostic factors in Step 1 were forced into the multivariable model to identify an eventual difference in the magnitude or significance of their effect
5/ In the pooled (NTT+T) group, using referral time as the starting point, a stepwise selection (sle=0.20 and sls=0.05) was performed to identify prognostic factors using a design prone to referral bias.
Cox models assumptions (Log-linearity assumption and proportional hazard assumption) were checked. In 1-year Cox analyses, high blood pressure, Charlson comorbidity index, heart failure, and vascular phenomena did not meet the proportional hazard assumption and were considered as time-varying covariates (covariate*time interaction). IE complications occurring during the hospital stay (septic shock, cardiac abscess, cerebral embolism, and cerebral haemorrhage) were introduced in the models as time-dependent covariates. Statistical analyses were performed using SAS 9.4 (SAS Institute, Inc., Cary, NC) software.
Ethics Statement
EI 2008 was conducted in accordance with the Declaration of Helsinki. Patients were informed of the study but their written individual consent was not required. EI 2008 was authorized by the Commission Nationale de l'Informatique et des Libertés (CNIL-DR-2010-219) and registered in ClinicalTrials.gov (NCT03295045).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships which have, or could be perceived to have, influenced the work reported in this article.
Acknowledgments
We thank all contributors of the AEPEI Study Group on Infective Endocarditis.
References
- 1.Collonnaz M, Erpelding M-L, Alla F, Goehringer F, Delahaye F, Iung B. Impact of referral bias on prognostic studies outcomes: insights from a population-based cohort study on infective endocarditis. Ann. Epidemiol. [Internet] 2020 Sep doi: 10.1016/j.annepidem.2020.09.008. Available from: [DOI] [PubMed] [Google Scholar]
- 2.Selton-Suty C, Célard M, Le Moing V, Doco-Lecompte T, Chirouze C, Iung B. Preeminence of Staphylococcus aureus in infective endocarditis: a 1-year population-based survey. Clin Infect Dis. 2012;54(May(9)):1230–1239. doi: 10.1093/cid/cis199. [DOI] [PubMed] [Google Scholar]
- 3.Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG, Ryan T. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30(April(4)):633–638. doi: 10.1086/313753. [DOI] [PubMed] [Google Scholar]
- 4.Steckelberg JM, Rouse MS, Wilson WR, Melton LJ, Ilstrup DM. Influence of referral bias on the apparent clinical spectrum of infective endocarditis. Am. J. Med. 1990;88(Jun 1(6)):582–588. doi: 10.1016/0002-9343(90)90521-e. [DOI] [PubMed] [Google Scholar]
- 5.Fernández‐Hidalgo N, Almirante B, Tornos P, González‐Alujas MT, Planes AM, Larrosa MN. Prognosis of left‐sided infective endocarditis in patients transferred to a tertiary‐care hospital—prospective analysis of referral bias and influence of inadequate antimicrobial treatment. Clin. Microbiol. Infect. 2011;17(May 1(5)):769–775. doi: 10.1111/j.1469-0691.2010.03314.x. [DOI] [PubMed] [Google Scholar]
- 6.Kanafani ZA, Kanj SS, Cabell CH, Cecchi E, de Oliveira Ramos A, Lejko-Zupanc T. Revisiting the effect of referral bias on the clinical spectrum of infective endocarditis in adults. Eur J Clin Microbiol Infect Dis. 2010;29(10):1203–1210. doi: 10.1007/s10096-010-0983-2. [DOI] [PubMed] [Google Scholar]
- 7.Rothman K, Greenland S, Lash T. Modern Epidemiology. 3rd ed. Lippincott Williams and Wilkins;; 2008. Validity in epidemiologic studies. [Google Scholar]