Abstract
We present a case of muscle-invasive bladder cancer arising in a man who had previously been diagnosed with prostate cancer. His prostate cancer diagnosis and subsequent treatment with external beam radiation therapy occurred over 20 years prior to being diagnosed with bladder cancer. Biopsies of the bladder mass revealed a high-grade urothelial carcinoma with prostatic invasion and MRI showed significant concern for invasion into the pelvic floor. Metastatic lesions on his right rib and left clavicle were discovered on bone scan.
Keywords: Lower urinary tract symptoms, Prostatic neoplasms, Radiotherapy, Urinary bladder neoplasms
1. Introduction
Radiation therapy (RT) has been used in the treatment of prostate cancer for over 50 years.1 While effective in its purpose of killing cancer cells, it is not without risk. Of the risks associated with RT, the development of a secondary malignancy is of most concern for the patient and physician. Recent advances in the technique/technology utilized in RT such as three-dimensional conformal radiotherapy (3D-CRT), intensity modulated radiotherapy (IMRT), and advances in dose escalation have touted better target localization and better outcomes and contemporary data suggests that the risk of secondary malignancy associated with RT is less than one percent.1,2
We present a case of treatment emergent, metastatic muscle-invasive bladder cancer occurring over 20 years after being treated for prostate cancer with external beam radiation therapy (ERBT).
2. Case presentation
A 76-year-old man with a history of prostate cancer in the late 90's and a 25 pack-year smoking history (quit in 2016) presented for pre-operative testing to undergo cystoscopy and lithotripsy of a bladder calculus. The SUNY Downstate Health Sciences University Urology Department was consulted to the ED for labs concerning for anemia (Hgb: 7.5 > 6.2 g/dL), hyperkalemia (K: 5.5 mmol/L), and AKI (BUN: 84, creatinine: 2.1 > 4.0 mg/dL). Urinalysis revealed >182 RBC's, >4000 WBC's, + leukocyte esterase, and was negative for nitrites. He was currently taking tamsulosin (0.4 mg/day) and finasteride (5 mg/day) with poor adherence.
He was treated with ERBT over 20 years prior, and throughout his follow-up, showed no signs of disease recurrence. His most recent PSA = 1.5 ng/mL, which was his baseline. On presentation, he complained of dysuria, difficulty urinating, frequency, and lower volume voids for 4–5 months. He denied hematuria, fever, chills, nausea, vomiting, abdominal pain, boney pain, and weight loss. CT abdomen/pelvis showed an asymmetric bladder wall thickening with layering calcifications and demonstrated radiographic concern for muscle invasion (Fig. 1). The patient was medically optimized and taken to the OR for cystoscopy, urethral dilation, cystolitholapaxy, and TURP.
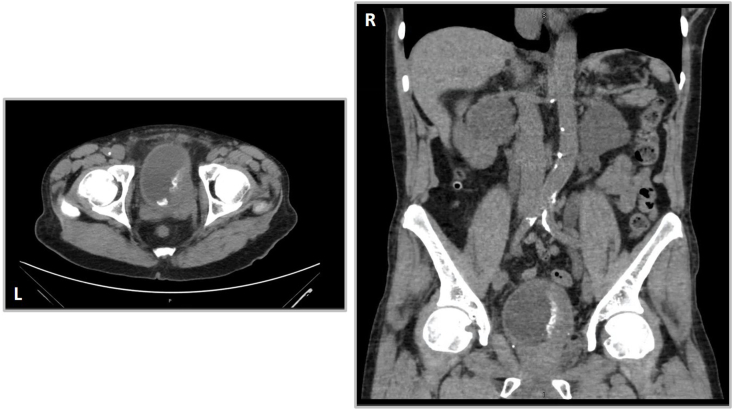
Fig. 1.
Abdominal/Pelvic CT scan without contrast.
Abnormal left superolateral bladder wall thickening with layering calcifications. Left: axial view. Right: coronal view.
During cystoscopy, the patient was noted to have a focus of calcification, which appeared to be a matrix upon necrotic debris. Biopsies of the calcification were obtained. Pathology from the initial biopsies revealed high grade urothelial carcinoma, invading the lamina propria. Pathology from the prostatic tissue obtained also revealed high grade urothelial carcinoma with similar morphology to that of the mass. A representative histologic specimen is shown in Fig. 2. Re-staging TURBT revealed necrotic, focally calcified tissue with markedly atypical cells. Subsequent MRI (Fig. 3) and bone scan revealed invasion of the adjacent pelvic floor musculature and metastatic lesions on the 7th right rib and left clavicle. At the time that this paper is being authored, the patient is still weighing his treatment options (RT vs diversion via ileal conduit).
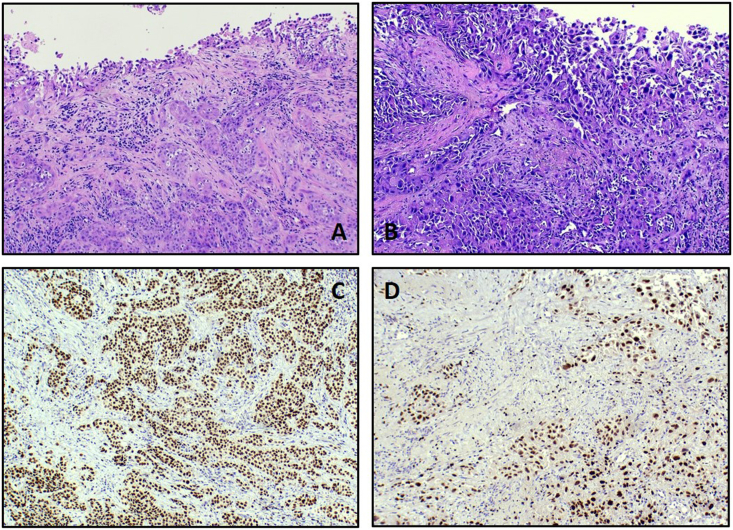
Fig. 2.
Bladder/Prostatic biopsy.
The bladder biopsy (A) shows nests of high-grade urothelial carcinoma invading the lamina propria in the background of extensive necrosis and inflammation. The specimen from prostate biopsy (B) also shows high grade invasive urothelial carcinoma that is morphologically similar to the tumor in bladder biopsy. Immunohistochemical studies on the bladder biopsy (C) and the prostate biopsy (D) demonstrate that the tumor cells are positive for GATA-3 and negative for PSA, supporting urothelial origin.
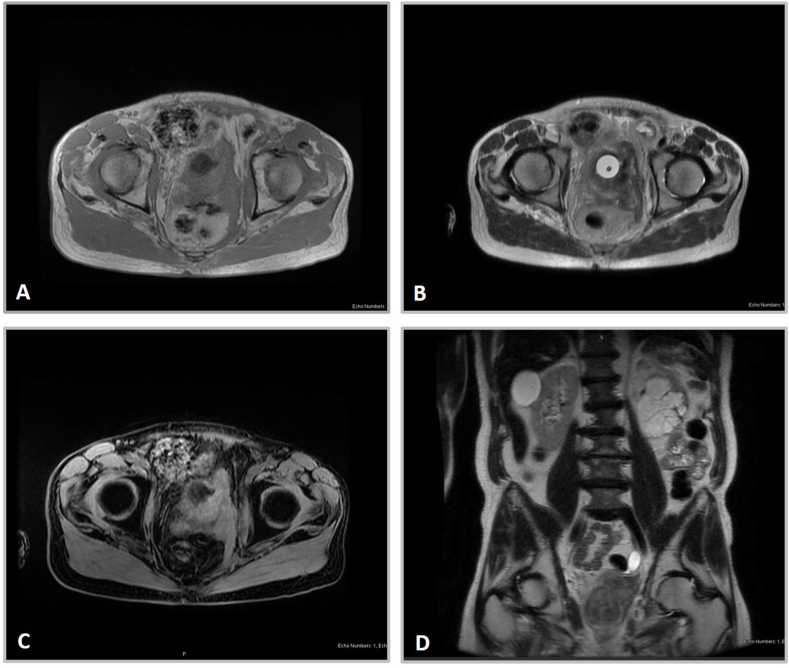
Fig. 3.
Abdominal/Pelvic MRI without contrast.
Infiltrative bladder mass insinuating into the left lateral and posterior lumen walls with apparent invasion of the adjacent left pelvic floor musculature. A: T1 weighted MRI, axial view. B: T2 weighted MRI, axial view. C: 3D water-selective MRI, axial view. D: T2 weighted MRI, coronal view.
3. Discussion
Painless, gross hematuria is the most common presenting symptom seen in patients with bladder cancer however, persistent irritative voiding symptoms in the absence of hematuria can be an indication of an underlying malignancy. For men above the age of 70 years, lower urinary tract symptoms (LUTS) are common complaints, usually associated with benign prostatic hyperplasia (BPH). However, these symptoms may represent an underlying oncologic process, especially in patients with history of pelvic RT. Approximately eight percent of men diagnosed with bladder cancer after receiving RT for prostate cancer present with LUTS.3
Patients who have been treated with RT have been shown to have an increased risk of developing secondary malignancies in radiation exposed areas and throughout the body.4 Men who had received RT for prostate cancer have been shown to carry an increased risk for developing bladder cancer (BC). Brenner et al. found that RT was associated with a 34% increased risk for BC at 10 years.5 More contemporary studies have echoed these findings. Moon et al. calculated an odds ratio of 1.63 for BC in men who received ERBT for prostate cancer.4 Contemporary data demonstrates a median period of 5 years between RT and bladder cancer diagnosis.3,5
In addition to being at higher risk for BC in general, men who have received RT are at increased risk to have a high-grade tumor present at the time of diagnosis. Yee et al. found that 92% of patients previously treated with RT had a high tumor grade at diagnosis, compared to 77% of non-irradiated patients. They also found that men treated with RT had progression to higher grade disease compared to those who had not received RT. After adjusting for age and time between diagnoses, they calculated that men who received RT for prostate cancers were 2.7 times more likely to develop muscle invasive bladder tumors compared to those who had not received RT.3
Regarding location, radiation increases the risk of a tumor developing in the trigone or bladder neck and increases the risk of having prostatic invasion by malignant urothelium.3
It is worth noting that we could not find data regarding survival and risk beyond 15 years in patients who received RT for prostate cancer.
4. Conclusion
Men who have undergone RT for prostate cancer are at significantly increased risk for developing bladder cancer and for having higher grade tumors present at diagnosis. The case presented demonstrates, if only anecdotally, that the risk for bladder cancer following RT may remain elevated 20+ years after treatment. Further investigation into the risks associated with RT beyond 15–20 years is needed as they may become a more significant factor in therapeutic decision making. Most importantly, physicians should pay close attention to when a patient has a history of radiation therapy.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
Drafting of the manuscript: Jack Barnett; Revision of the manuscript: Jack Barnett, Matthew Bruha, Llewellyn Hyacinthe, Fatih Ozay; Supervision: Llewellyn Hyacinthe and Matthew Bruha. Pathologic image/description: Fatih Ozay. All authors have read and approved the final manuscript.
Declaration of competing interest
Jack Barnett – no conflicts of interest to report, Matthew Bruha – no conflicts of interest to report, Fatih Ozay – no conflicts to report, Llewellyn Hyacinthe – no conflicts of interest to report.
References
- 1.Mangar S.A., Huddart R.A., Parker C.C., Dearnaley D.P., Khoo V.S., Horwich A. Technological advances in radiotherapy for the treatment of localised prostate cancer. Eur J Canc. 2005;41(6):908–921. doi: 10.1016/j.ejca.2004.12.028. [DOI] [PubMed] [Google Scholar]
- 2.Turina M. Frequency and surgical management of chronic complications related to pelvic radiation. Arch Surg. 2008;143(1):46. doi: 10.1001/archsurg.2007.7. [DOI] [PubMed] [Google Scholar]
- 3.Yee D.S., Shariat S.F., Lowrance W.T. Impact of previous radiotherapy for prostate cancer on clinical outcomes of patients with bladder cancer. J Urol. 2010;183(5):1751–1756. doi: 10.1016/j.juro.2010.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moon K., Stukenborg G.J., Keim J., Theodorescu D. Cancer incidence after localized therapy for prostate cancer. Cancer. 2006;107(5):991–998. doi: 10.1002/cncr.22083. [DOI] [PubMed] [Google Scholar]
- 5.Brenner D.J., Curtis R.E., Hall E.J., Ron E. Second malignancies in prostate carcinoma patients after radiotherapy compared with surgery. Cancer. 2000;88(2):398–406. doi: 10.1002/(SICI)1097-0142(20000115)88:2<398::AID-CNCR22>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]