Abstract
Severe acute respiratory virus syndrome 2 (SARS-CoV-2) has led to a worldwide pandemic. Early studies in solid organ transplant (SOT) recipients suggested a wide variety of presentations, however, there remains a paucity of robust data in this population. We conducted a systematic review and meta-analysis of SOT recipients with SARS-CoV-2 infection from January 1st t October 9th, 2020. Pooled incidence of symptoms, treatments and outcomes were assessed. Two hundred and fifteen studies were included for systematic review and 60 for meta-analysis. We identified 2,772 unique SOT recipients including 1,500 kidney, 505 liver, 141 heart and 97 lung. Most common presenting symptoms were fever and cough in 70.2% and 63.8% respectively. Majority (81%) required hospital admission. Immunosuppressive medications, especially antimetabolites, were decreased in 76.2%. Hydroxychloroquine and interleukin six antagonists were administered in59.5% and 14.9% respectively, while only few patients received remdesivir and convalescent plasma. Intensive care unit admission was 29% from amongst hospitalized patients. Only few studies reported secondary infections. Overall mortality was 18.6%. Our analysis shows a high incidence of hospital admission in SOT recipients with SARS-CoV-2 infection. As management of SARS-CoV-2 continues to evolve, long-term outcomes among SOT recipients should be assessed in future studies.
Keywords: Solid organ transplant, COVID-19, SARS-CoV-2, Immunosuppression, Systematic review, Meta-analysis
Abbreviation: AKI, Acute kidney injury; CI, Confidence interval; CNI, Calcineurin inhibitor; COVID-19, Coronavirus disease 2019; CRP, C-Reactive Protein; FEM, Fixed Effect Model; HSCT, Hematopoietic Stem Cell Transplant; ICU, Intensive Care Unit; IL-6, Interleukin Six; MERS, Middle East Respiratory Syndrome; NP, Nasopharyngeal; PRESS, Peer Review for Electronic Search Strategies; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; REM, Random Effect Model; RT-PCR, Reverse Transcriptase-Polymerase Chain Reaction; SARS, Severe Acute Respiratory Syndrome Coronavirus 1; SARS- CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2; SOT, Solid organ transplant
1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for the coronavirus disease 2019 (COVID-19), has been an unmitigated worldwide pandemic, since the first case was reported in December 2019 [1,2]. Due to the high rate of transmissibility in the asymptomatic phase, the virus has continued to spread globally with catastrophic outcomes and has been a great challenge for clinicians all over the world [2,3]. Even though it causes mild disease in certain populations, to date it has led to 228,998 and 1,178,475 deaths in the U.S and worldwide, respectively [3].
Solid organ transplant (SOT) recipients are known to be vulnerable to several respiratory virus infections, such as influenza [4] due to a weakened T-cell mediated immune response [5]. The Centers for Disease Control and Prevention include SOT recipients amongst patients at increased risk for severe illness from SARS-CoV-2 [6]. Due to the novelty of this virus, there is still a paucity of data regarding many aspects including its natural course within immunocompromised hosts, the utility of current treatment regimens employed in non-transplant individuals for SOT recipients, the effect of immunosuppression on the course of the disease, and much more [7,8]. Even though presence of comorbidities, such as obesity, have been reported as risk factors for severe disease [9], an immunocompromised state has not yet been proven to have a worse clinical outcome with SARS-CoV-2 infection. Furthermore, as Vishnevetsky correctly points out, viruses that belong to the same coronavirus family such as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome Coronavirus 1 (SARS) have not shown an increased risk of infection or worse outcome in immunocompromised patients [[10], [11], [12]]. Lai et. al. also published their systematic review comparing disease outcomes among the three major coronavirus diseases with preliminary data [13]. Furthermore, immunosuppression in the setting of hyperinflammation may even be beneficial, by blunting excessive cytokine release, which is still left to be established [14].
Since the first report of COVID-19 in SOT recipient from China was published in early 2020 [15], researchers from all over the world, have published their own experiences, especially from epidemic centers [[16], [17], [18]] to try and bridge the gap in knowledge, including several recently published registries [[19], [20], [21], [22]]. COVID-19 presentation amongst SOT recipients has ranged from mild upper respiratory infection to severe acute respiratory distress and death [23,24]. Studies in the general population so far suggest a higher prevalence and severity of disease among middle-aged patients and in those with underlying comorbidities such as hypertension and obesity, however, data in SOT recipients is still lacking [25]. The wide variety in clinical presentation among SOT recipients is still not fully understood. Fung and Bebik recently published their narrative review that included SOT recipients and their manuscript broadly covered this area but did not assess present data quantitatively [24].
We performed a systematic review and meta-analysis of the existing literature to help expand our current limited knowledge base regarding COVID-19 in SOT recipients, especially looking at clinical presentations, treatment modalities and outcomes, with the aim to provide transplant physicians worldwide with important decision-making tools to manage these critically ill patients during this time of crisis.
2. Materials and methods
Our review was conducted according to the Methodological Expectations for Cochrane Intervention Reviews [26] and reported following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [27].
2.1. Search methods
We conducted a comprehensive literature database search to find all relevant literature, published from January 1st to October 9th, 2020, on SARS-CoV-2 and SOT. The database search strategy was developed by an academic health science librarian (J.R.) in consultation with the project leader (Y.N.) and was reviewed using the Peer Review for Electronic Search Strategies (PRESS) tool through the PRESS forum [28].
We searched Ovid Medline (including Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily), Embase (Elsevier Embase.com), Scopus (Elsevier), Web of Science (Clarivate Analytics, using Science Citation Index Expanded, Social Sciences Citation Index, Arts & Humanities Citation Index, Conference Proceedings Citation Index- Science, Conference Proceedings Citation Index- Social Science & Humanities, Emerging Sources Citation Index, BIOSIS Citation Index, KCI-Korean Journal Database, Russian Science Citation Index, SciELO Citation Index, and Zoological Record), and LitCovid (National Center for Biotechnology Information, U.S. National Library of Medicine, without date restrictions). We searched clinical trial registries with Clinicaltrials.gov and the World Health Organization International Clinical Trials Registry Platform for clinical trials with reported results. In lieu of handsearching, we also searched the online tables of contents of seven journals: American Journal of Transplantation, Journal of Heart and Lung Transplantation, Liver Transplantation, Pediatric Transplantation, Transplant Infectious Disease, Transplant International, and Transplantation. Databases and registries were searched between June 11th and June 15th, 2020, and individual journals were searched on June 19th, 2020. The database and journal site searches were updated on July 13th, 15th, August 20th, October 5th, as well as October 8th and again on October 9th 2020. The research team also monitored social media for new studies up to August 23rd, 2020. The search strategy was initially based on terms from 36 articles found by the research team prior to the comprehensive database search, and by refining, expanding, and adding to COVID-19 specific search strategies by Ellen Aaronson at the Mayo Clinic [29], and Michelle Volesko Brewer and Pieter van der Houwen, at Wolters Kluwer/Ovid [30].
The search strategy was written for Ovid Medline and translated using each database's syntax, controlled vocabulary, and search fields. MeSH terms, EMTREE terms, and text words were used for the search concepts of Covid-19/SARS-Cov-2 and solid organ transplantation and their synonyms. No language, study type, or publication type limits were applied at the search phase. Animal studies were excluded. Except for LitCovid, searches were limited by date from January 1, 2020 to the present to allow for broader search terms while still focusing on SARS-Cov-2.
For full search strategies, see Appendix 1. All database records were downloaded to EndNote X9, then uploaded to Covidence web-based software for deduplication, screening, and data extraction. We contacted several authors whose cases potentially can be used several times in the different articles. Two reviewers (MAM and APV) independently assessed all studies for risk of bias. Any discrepancies in data extraction were resolved with discussion with the third and fourth reviewers (M.R. and Y.N.). After study selection, one author (J.R.) checked for retractions at The Retraction Watch Database and individual journal websites.
2.2. Inclusion and exclusion criteria
We included all randomized controlled trials, cohort studies, case reports, and letters to the editor that included targeted data in SOT and reverse transcriptase-polymerase chain reaction (RT-PCR) or antibody testing confirmed SARS-CoV-2 infection. As previously mentioned, animal studies and articles where the main topic was other than COVID-19 in SOT patients were excluded. We excluded studies dealing with patients with suspected infection (eg. chest imaging abnormality and symptoms), without positive RT-PCR or antibody testing. We also excluded other non-SARS-CoV-2 coronavirus related studies such as MERS and SARS. If the study subject was published more than once, we entered in the analysis only once using all available sources. For the meta-analysis, we only included articles with 5 or more patients to minimize small study effect. From included studies, the following variables were collected: number of subjects, organ transplant types, symptoms, laboratory data, treatment modalities used, type of immunosuppression, modification to the immunosuppression, graft loss, follow up period, duration from first positivity to negativity of nasopharyngeal (NP) swab RT-PCR, and all-cause mortality. After obtaining these results we excluded studies for hospital admission, intensive care unit (ICU) admission, mechanical ventilation, and all-cause mortality, for studies dealing only with critically ill patients, to avoid selection bias and avoid heterogeneity.
2.3. Data analysis
We conducted this data analysis using STATA/IC 14.0 (StataCorp LP,College Station, TX, USA). Dichotomous data were shown as relative risk ratio (RR, event/total) and their confidence interval (CI), where relevant. Pooled incidence was calculated with either random effect model or fixed-effect model, wherever appropriate. Heterogeneity among studies was graphically shown and checked with I2 values, which show the variation among studies that are not due to chance. I2 values of 75%, 50%, and 25% correspond to a high, medium, and low level of heterogeneity. Fixed-effect model (FEM) was used if I2 was less than 50%, otherwise random effect model (REM) was used. To visually inspect the publication bias, we created both forest and funnel plots.
3. Results
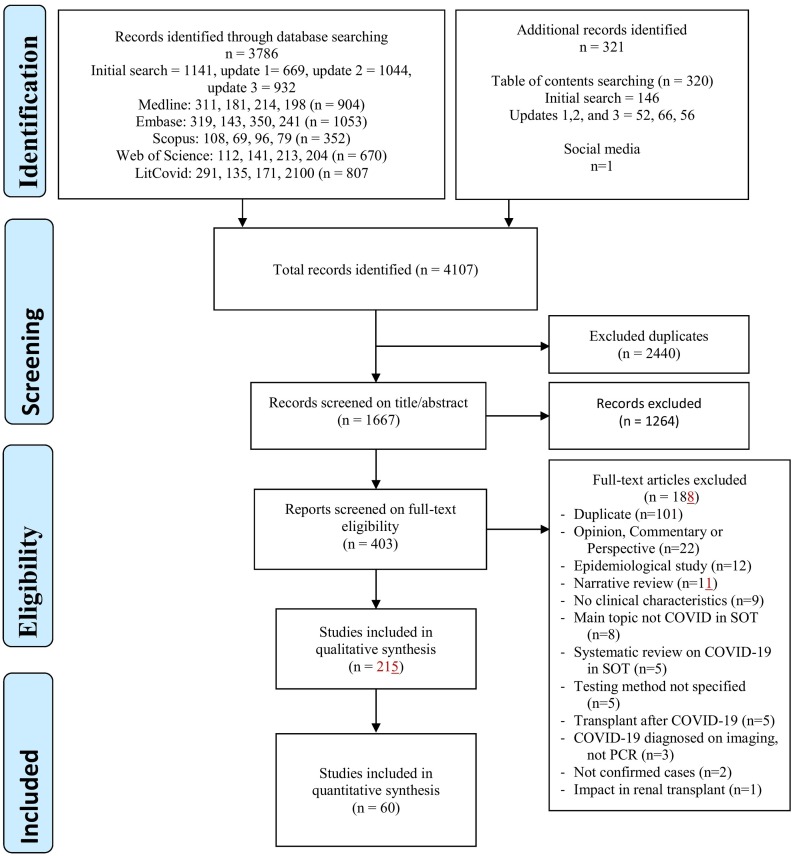
With this search strategy, we found 1,667 potential studies, after excluding the duplicates. Of these, 1,263 studies were excluded during the abstract and title review as they did not meet eligibility criteria. The most common reasons for exclusion were perspective or opinion commentaries regarding COVID-19 and articles reporting viruses other than COVID-19. As a result, we conducted a full-text review for 403 articles, of which 188 were excluded with reasons shown in Fig. 1 . Finally, a total of 215 studies were included in the systematic review [8,[15], [16], [17], [18], [19], [20], [21], [22], [23], [24],[31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99], [100], [101], [102], [103], [104], [105], [106], [107], [108], [109], [110], [111], [112], [113], [114], [115], [116], [117], [118], [119], [120], [121], [122], [123], [124], [125], [126], [127], [128], [129], [130], [131], [132], [133], [134], [135], [136], [137], [138], [139], [140], [141], [142], [143], [144], [145], [146], [147], [148], [149], [150], [151], [152], [153], [154], [155], [156], [157], [158], [159], [160], [161], [162], [163], [164], [165], [166], [167], [168], [169], [170], [171], [172], [173], [174], [175], [176], [177], [178], [179], [180], [181], [182], [183], [184], [185], [186], [187], [188], [189], [190], [191], [192], [193], [194], [195], [196], [197], [198], [199], [200], [201], [202], [203], [204], [205], [206], [207], [208], [209], [210], [211], [212], [213], [214], [215], [216], [217], [218], [219], [220], [221], [222], [223], [224], [225], [226], [227], [228], [229], [230], [231], [232], [233], [234], [235]], and 60 studies were included in a meta-analysis [16,18,21,22,24,31,32,38,40,43,50,51,55,59,60,65,69,70,79,81,85,88,96,100,102,108,114,117,128,133,135,136,[141], [142], [143],149,151,153,157,158,162,166,175,179,183,185,189,190,192,199,210,212,216,217,219,228,229,231].
Fig. 1.
Study selection flow. Majority of the cases were excluded due to opinion commentaries for COVID-19 or related to other viruses. Abbreviations: COVID; Coronavirus disease 2019, SOT; Solid organ transplant, RT-PCR; Reverse transcriptase-polymerase chain reaction.
3.1. Patient background
In total, 2,772 unique SOT recipients were identified including 1,500 kidney, 505 liver, 141 heart, 97 lung, 1 face and 43 unidentified combined transplants. One thousand seven hundred sixty four (63.63%) patients were male. Calcineurin inhibitor (CNI) and corticosteroids were used in the majority of the patients at the time of diagnosis, 91%, (95% Confidence Interval [CI], 87.6%-94.3%, REM, I2 86.4%) and 70.1%, (95% CI, 61.5%-78.7%, REM, I2 96.2%) respectively. Antimetabolite, such as azathioprine and mycophenolate mofetil, were used in 76.9% (95% CI, 71.3%-82.4%, REM, I2 87.6%). Time from transplant to diagnosis of SARS-CoV-2 widely varied from 4 days to 31 years. Of note, no donor derived SARS-2 COVID infection was reported.
3.2. Symptoms with COVID-19 in solid organ transplant recipients
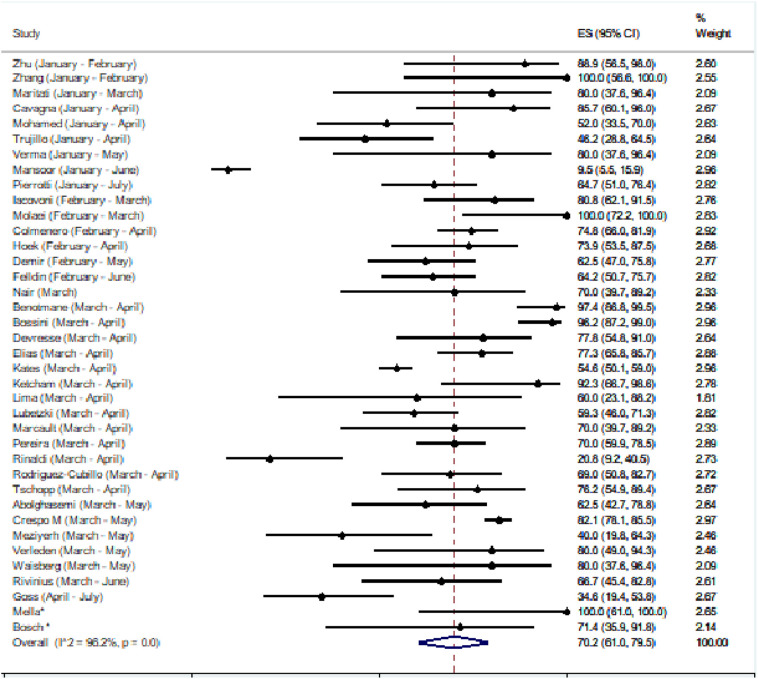
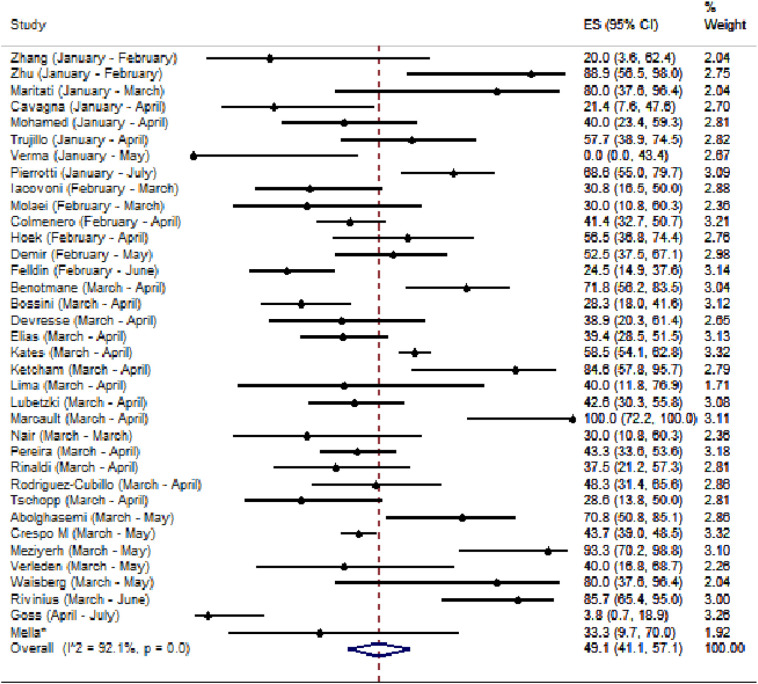
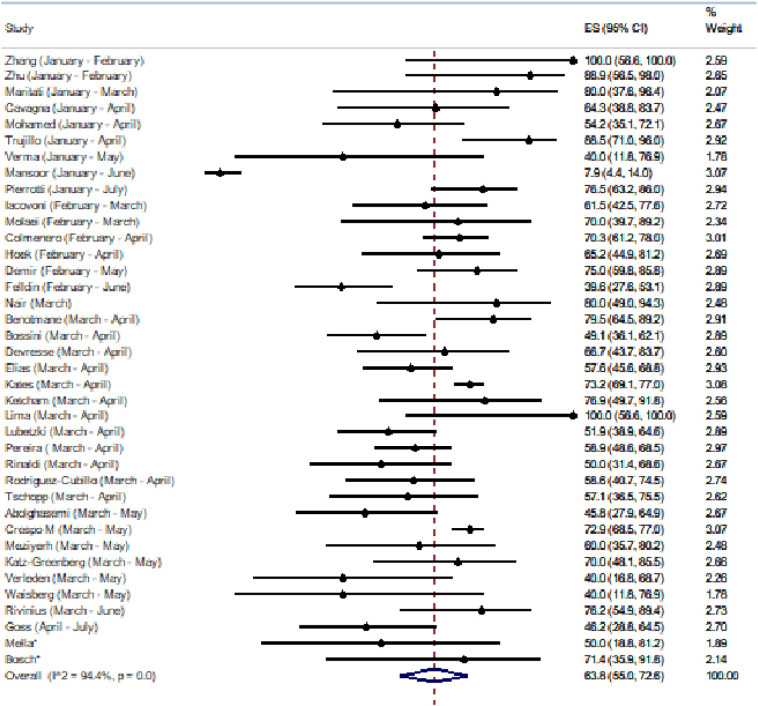
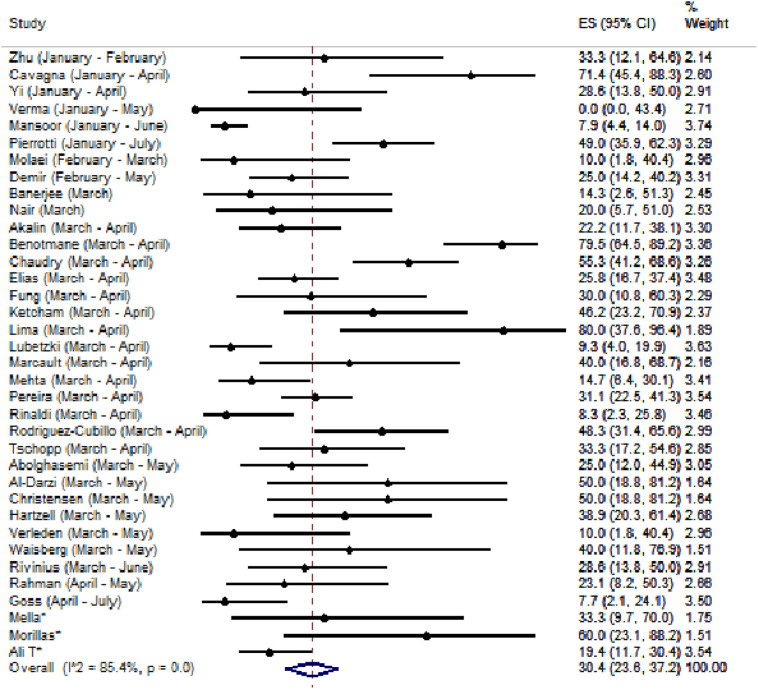
At first, we assessed the most common presenting symptoms among SOT recipients with COVID-19. A summary is shown in table 1 . Of note, pooled incidence of fever, shortness of breath, cough and diarrhea were 70.2% (95% CI, 61.0%-79.5%, REM, I2 96.2%), 49.1% (95% CI, 41.1%-57.1%, REM, I2 92.1%), 63.8% (95% CI, 55.0%-72.6%, REM, I2 94.4%) and 30.4% (95% CI, 23.6%-37.2%, REM, I2 85.4%), respectively (Fig. 2A, Fig. 2B, Fig. 2C, Fig. 2D ) [16,18,20,22,24,31,38,40,43,51,55,56,59,60,65,69,70,79,81,85,88,96,100,102,108,117,133,136,[141], [142], [143],149,151,152,156,158,162,166,179,185,189,190,192,210,212,216,217,219,228,229,231].
Table 1.
Summary of symptoms with COVID 19 in Solid Organ Transplant Recipients.
| Symptoms | No. of Studies | Model | Pooled incidence (%) (95% CI) | Heterogeneity (I2), p value |
|---|---|---|---|---|
| Fever | 38 | REM | 70.2 (61.0-79.5) | 96.2, p<0.01 |
| Cough | 38 | REM | 63.8 (55.0-72.6) | 94.4, p<0.01 |
| Shortness of breath | 36 | REM | 49.1 (41.1-57.1) | 92.1, p<0.01 |
| Diarrhea | 36 | REM | 30.4 (23.6-37.2) | 85.4, p<0.01 |
Abbreviations: CI, confidence interval, REM, random effect model
Fig. 2A.
Pooled incidence of fever showing the absolute risk and 95% confidence intervals of each study (n=38) [18,20,22,31,56,59,60,65,70,79,81,85,88,96,102,108,117,133,136,[141], [142], [143],151,152,156,158,166,179,189,190,192,210,212,216,217,219,229,231]. Abbreviations. ES; Effect Size, CI; Confidence Interval, *=study period not defined.
Fig. 2B.
Pooled incidence of shortness of breath showing the absolute risk and 95% confidence intervals of each study (n=36) [18,20,22,31,55,60,65,70,79,81,85,88,96,102,108,117,133,136,142,143,151,152,156,158,166,179,189,190,192,210,212,216,217,219,229,231] Abbreviations. ES; Effect Size, CI; Confidence Interval, *=study period not defined.
Fig. 2C.
Pooled incidence of cough showing the absolute risk and 95% confidence intervals of each study (n=38) [18,20,22,31,55,59,60,65,70,79,81,85,88,96,102,108,114,117,133,136,141,143,151,152,156,158,166,179,189,190,192,210,212,216,217,219,229,231]. Abbreviations. ES; Effect Size, CI; Confidence Interval, *=study period not defined.
Fig. 2D.
Pooled incidence of diarrhea showing the absolute risk and 95% confidence intervals of each study (n=36) [16,18,24,31,38,40,43,51,55,65,69,79,85,96,100,117,133,136,141,142,149,151,158,162,166,179,185,189,190,192,212,216,217,219,228,231]. Abbreviations. ES; Effect Size, CI; Confidence Interval, *=study period not defined.
3.3. Laboratory results and radiologic findings
We then analyzed laboratory results at and after diagnosis of COVID-19. Leukopenia (white blood cell count <4000/mm3) was noted in 19 studies with pooled incidence of 17.8% (95% CI 10.7%-24.8%, REM, I2 57.2%) [24,31,40,51,88,96,108,133,135,143,151,152,158,162,166,216,217,219,229]. C-reactive protein (CRP) level was documented in 161 studies [8,14,[16], [17], [18], [19],21,[23], [24], [25],[31], [32], [33], [34], [35], [36], [37], [38],40,[42], [43], [44], [45], [46], [47], [48],[50], [51], [52],55,56,59,60,62,63,[66], [67], [68], [69],[71], [72], [73],[76], [77], [78], [79], [80], [81], [82],[84], [85], [86], [87], [88], [89],[92], [93], [94], [95], [96], [97], [98],[100], [101], [102], [103], [104],106,[108], [109], [110],112,115,116,[118], [119], [120], [121],[124], [125], [126], [127], [128], [129], [130],[133], [134], [135], [136], [137], [138], [139],141,143,146,147,[151], [152], [153], [154], [155], [156],158,159,[161], [162], [163], [164], [165], [166], [167],169,171,174,[177], [178], [179],185,[187], [188], [189], [190], [191], [192],194,[196], [197], [198], [199], [200],203,204,206,207,[210], [211], [212], [213], [214],216,[218], [219], [220], [221],[224], [225], [226],[228], [229], [230], [231], [232],[234], [235], [236], [237], [238], [239], [240]]. Cravedi et. al. reported a median CRP level of 41.0 (interquartile range 11.5-125.3) mg/L amongst 144 patients [19], while Pereira et. al. reported a median CRP level of 68.5 (interquartile range 15.4-126) mg/L from among 90 patients [18].
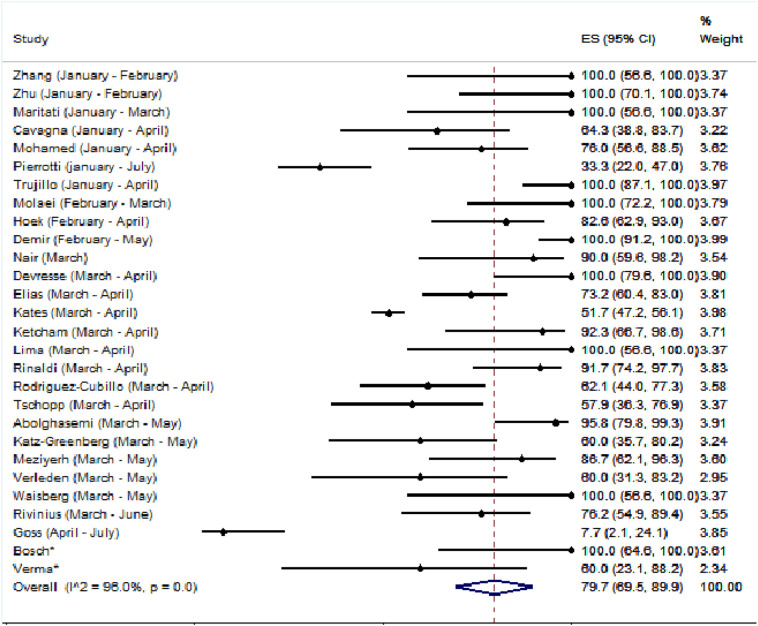
Radiological abnormalities on chest imaging, either radiography or computerized tomography, was found in 28 studies with pooled incidence of 79.7% (95% CI 69.5%-89.9%, REM, I2 96.0%) [22,31,59,65,79,81,85,96,102,114,117,133,143,152,156,158,166,179,189,190,192,210,212,216,217,219,229,231] (Fig. 3 ).
Fig. 3.
Pooled incidence of abnormal chest imaging (either radiography or computerized tomography) in solid organ transplant recipients and COVID-19, showing the absolute risk and 95% confidence intervals of each study (n=28)[22,31,59,65,79,81,85,96,102,114,117,133,143,152,156,158,166,179,189,190,192,210,212,216,217,219,229,231]. Abbreviations. ES; Effect Size, CI; Confidence Interval, *=study period not defined.
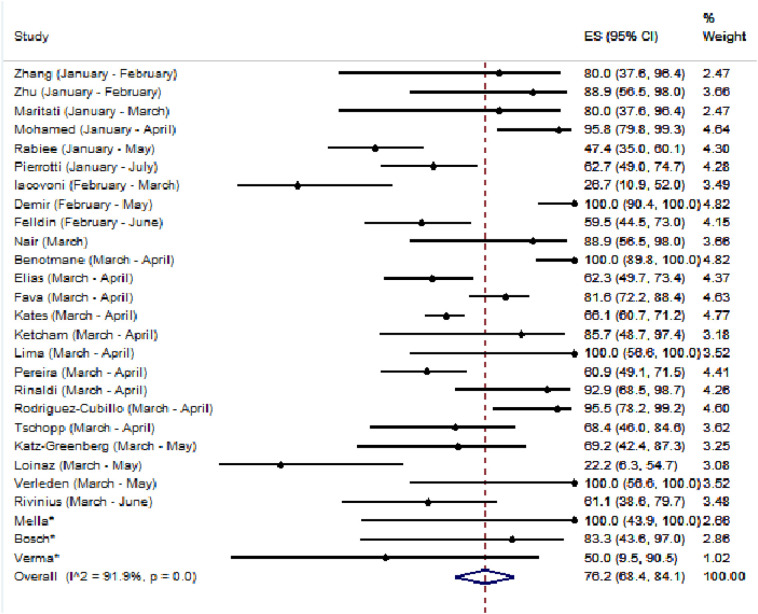
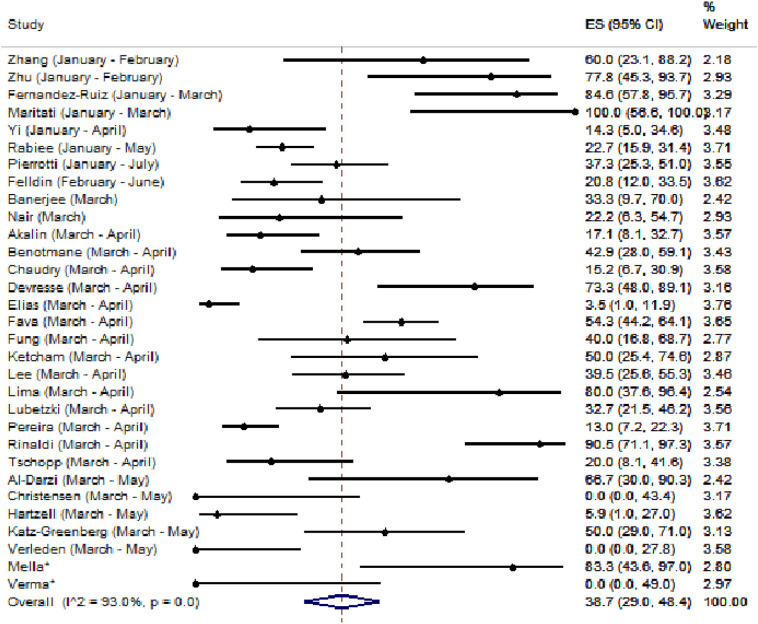
3.4. Treatment method
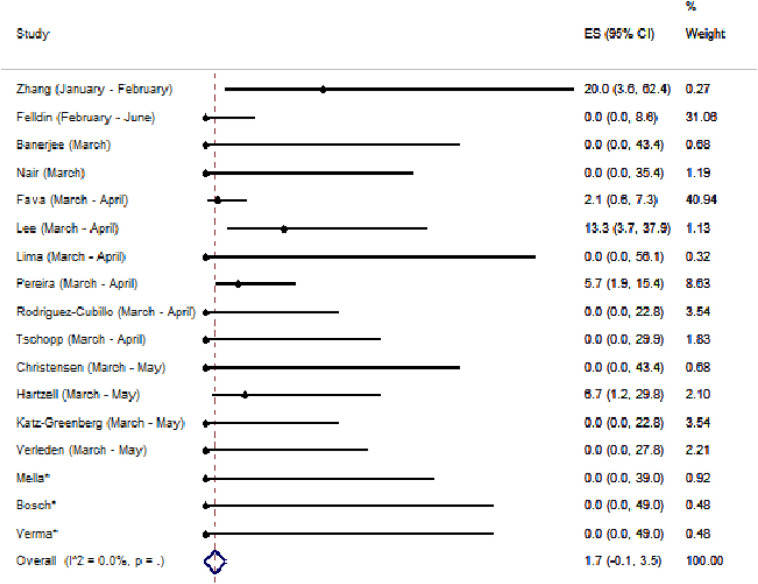
We also analyzed the different treatment modalities used in SOT patients with COVID 19 and findings are summarized in table 2 [18,20,22,24,31,55,59,60,65,70,79,81,85,88,96,102,108,114,117,133,136,142,143,151,156,158,166,179,183,189,192,210,212,216,219,231]. Immunosuppressive medications, especially antimetabolites, were decreased in 76.2% (95% CI, 68.4%-84.1%, REM, I2 91.9% ,Fig. 4A ) [18,21,22,55,59,79,85,88,108,114,117,133,135,143,151,156,166,179,183,189,190,192,212,216,217,229,231]. On the other hand, reduction in CNI highly varied from 0%-100% with pooled incidence of 38.7% (95% CI, 29.0%-48.4%, REM, I2 93.0, Fig. 4B ) [16,18,21,23,24,38,40,51,55,69,81,85,88,100,114,117,128,133,136,143,151,166,179,183,189,212,216,217,228,229,231]. Corticosteroids were very seldom reduced in 1.7% (95% CI, 0.1%-3.5%, FEM, I2 0.0%, Fig. 4C ) [18,21,51,59,69,88,100,114,128,133,151,166,192,212,216,217,229].
Table 2.
Summary of treatment modalities with COVID 19 in Solid Organ Transplant Recipients.
| Treatment Modalities | No. of Studies | Model | Pooled incidence (%) (95% CI) | Heterogeneity (I2), p value |
|---|---|---|---|---|
| Hydroxychloroquine | 30 | REM | 59.5 (45.0-74.0) | 98.7, p<0.01 |
| Azithromycin | 21 | REM | 48.6 (35.2-62.0) | 97.4, p<0.01 |
| IL-6 antagonist | 15 | REM | 14.9 (9.9-19.9) | 86.7, p<0.01 |
| Protease inhibitors | 11 | REM | 28.8 (19.1-38.5) | 82.8, p<0.01 |
| Steroids | 19 | REM | 38.9 (27.9-49.8) | 97.0, p<0.01 |
Abbreviations: CI, confidence interval, REM, random effects model, IL-6, interleukin six
Fig. 4A.
Pooled incidence of reduction in anti-metabolite showing the absolute risk and 95% confidence intervals of each study (n=27)[18,[20], [21], [22], [23],55,59,79,81,108,117,133,135,143,156,166,175,[189], [190], [191], [192],212,216,229,231]. Abbreviations. ES; Effect Size, CI; Confidence Interval, *=study period not defined.
Fig. 4B.
Pooled incidence of reduction in calcineurin inhibitor showing the absolute risk and 95% confidence intervals of each study (n=31)[16,18,20,21,23,24,38,51,55,79,81,117,128,133,143,151,166,175,189,191,212,216,228,229,231]. Abbreviations. ES; Effect Size, CI; Confidence Interval, *=study period not defined.
Fig. 4C.
Pooled incidence of reduction in steroid showing the absolute risk and 95% confidence intervals of each study (n=17)[18,21,23,51,81,100,128,151,166,191,192,212,216,229]. Abbreviations. ES; Effect Size, CI; Confidence Interval, *=study period not defined.
Majority of cases were treated with hydroxychloroquine (59.5% 95% CI, 45.0%-74.0%, REM, I2 98.7%, supplemental Fig. A) [18,20,22,31,55,59,60,65,70,81,85,88,96,102,108,114,117,133,143,151,158,166,183,189,190,192,210,212,216,219]. Forty eight percent of cases were also placed on azithromycin (95%CI, 35.2%-62.0%, REM, I2 97.4%, supplemental Fig. B) [18,20,22,55,59,60,65,70,88,96,102,114,158,166,179,183,189,190,210,216,219]. Interleukin Six (IL-6) antagonists were used in 14.9% (95% CI, 9.9%-19.9%, REM, I2 86.7% supplemental Fig. C) [18,20,22,55,60,70,79,85,88,117,133,136,189,192,210]. Protease inhibitors were used in 28.8% (95% CI, 19.1%-38.5%, REM, I2 82.8% supplemental Fig. D) [20,24,31,56,70,108,143,151,189,210,212]. Use of high dose steroids, [defined as prednisone at least 1mg/kg, hydrocortisone at least 100mg/day, methylprednisolone at least 200mg/daily, dexamethasone (>2mg/day)], was reported in 19 studies with a pooled incidence of 38.9% (95% CI, 27.9%-49.8%, REM, I2 97.0% ,supplemental Fig. E) [18,20,22,55,60,70,81,108,117,133,142,156,158,179,183,189,192,210,231]. Concurrent antibiotic use was seen in 69.4% (95% CI, 58.9%-79.9%, REM, I2 94.9%) [16,24,32,40,50,51,55,60,79,81,102,108,136,151,162,166,179,185,190,199,210,212,216,219,229].
Fourteen studies, excluding potential duplicates, documented use of remdesivir with a total of 36 unique patients [18,22,50,69,70,114,127,133,136,165,183,217,228,240], of which 9 studies documented mortality with 2 deaths amongst 14 patients [ 50 , 69 , 114 , 127 , 133 , 136 , 165 , 217 , 228 ]. Thirteen studies, excluding potential duplicates, mentioned use of convalescent plasma with a total of 33 unique patients [24,33,46,69,90,110,114,133,136,165,185,199,228], of which 11 studies documented about mortality with a total of 4 deaths from among 31 patients [24,33,46,69,90,110,114,133,165,185,228].
3.5. Outcomes
Finally, we analyzed outcomes in SOT recipients post COVID-19 infection.
Twenty two studies showed 81.0% pooled incidence of hospital admission (95% CI 75.2%-86.7%, REM, I2 91.4%) [18,20,22,55,60,65,70,79,81,85,88,96,102,108,114,136,141,156,166,190,212,216], while 30 studies showed a 29.3% pooled incidence (95% CI 22.6%-36.1%, REM, I2 89.2%) of admission to the ICU from amongst hospital admissions [18,20,22,31,59,60,70,79,81,85,88,96,102,108,114,117,133,143,151,152,158,166,179,183,189,190,210,212,216,229]. Overall, 25.9% of patients required mechanical ventilation (95% CI 20.1%-31.8%, REM, I2 74.4%) from among hospital admissions [18,20,22,31,59,60,65,70,79,81,85,88,96,102,108,114,117,133,142,143,151,152,158,166,179,183,190,192,212,216,217,219,229,231].
Thirty-four studies addressed secondary or co-infections [22,24,50,51,89,91,92,96,105,106,110,127,133,143,145,151,157,158,162,163,165,166,177,182,185,[189], [190], [191],194,199,200,212,217,219]. The majority of reported cases were bacterial urinary tract infection in kidney transplant recipients [89,96,151,165,166,212] Of note, Nair et. al documented that 3 recipients, out of 10 kidney transplant patients, developed positive urine culture (Enterococcus, Klebsiella and E.coli) [166] and while Goss et. al report a culture with Group B streptococcus [96]. Respiratory secondary bacterial infections due to gram negative bacteria, including Eschericia coli, Pseudomonas aeruginosa, Acinetobacter baumanni, Klebsiella pneumoniae, Morganella morganii, Stenotrophomonas maltophilia, as well as gram positive bacteria, including Enterococcus faecalis, Staphylococcus aureus, Streptococcus haemolyticus were also noted [22,50,92,127,157,169,177,185,219][22,50]. Bacteremia was reported in 4 cases with different pathogens [50,91,133,143]: 2 patients with Klebsiella pneumoniae, Staphylococcus epidermidis and two patients with Staphylococcus aureus [143]. Clostridium difficile colitis was reported in three patients [177,185].
Regarding viral secondary infection we six reports of Cytomegalovirus infection [50,51,143,158,177,190]. Molaei et. al reports four patients having COVID-19 and CMV co-infection with a viremia of 412-592 IU/mL [158], on the other hand, Pereira et. al also reports five patients with CMV with a median of 1469 (1326-8994) IU/mL [177] while Pierroti et. al reports 9 patients with CMV viremia [179]. Only one case of Influenza A co-infection was reported [200]. Two other patients had co-infections with HHV-6 and EBV [177]. There is also a report on a patient with a recent history of slight BK viremia that largely increased after COVID-19 infection [145].
Fungal secondary infections were also reported. Candidemia was reported in 1 liver transplant recipient [106] and other solid organ transplant patients with Candida glabrata candidemia [177] and Candida krusei bacteremia [185] while Rinaldi et al. reported 3 invasive candidiasis as well as 12 pulmonary aspergillosis [189]. Morlacchi et. al. reported on 4 lung transplant recipients with a bronchoalveolar lavage from 1 patient with Aspergillus fumigatus [163] while Pereira et. al reported another solid organ transplant recipient with aspergillus infection [177]. Also, Roberts et. al. reported 2 fungal infections with Aspergillus versicolor and severe cutaneous candidiasis [191]. Finally, Kates et. al. reported a pneumonia due to cryptococcus species as well as a patient with Pneumocystis pneumonia [22].
There are 62 studies documented about the duration of viral shedding and time to negativity of RT-PCR on NP specimens [1,15,24,35,36,39,45,47,55,60,61,66,67,70,72,75,80,91,92,[96], [97], [98],105,106,110,113,115,[118], [119], [120], [121], [122],125,130,134,[136], [137], [138],140,147,148,[161], [162], [163], [164],170,174,176,180,182,197,198,200,207,213,218,220,221,226,229,230,232,241] Majority of patients achieved negativity around 3 to 5 weeks from the initial positive result. The NP swab RT-PCR methods varied from study to study and the time from onset of symptoms to first positive RT-PCR result was not assessed. However, we identified that SOT recipients achieved RT-PCR negativity on day 5 at the earliest [170] and day 56 at the latest [182] in this systematic review. No studies were found documenting viral culture of SARS-CoV-2 among SOT recipients.
Also, 52 articles documented about rejection after COVID-19 [18,[22], [23], [24],31,40,43,50,65,69,70,81,84,88,92,98,101,[103], [104], [105],108,114,116,118,120,123,125,130,[133], [134], [135],143,145,154,165,171,173,175,179,183,186,191,192,199,201,205,207,210,220,224,230,231][18,[22], [23], [24],65,81,84,92,98,101,[103], [104], [105],108,116,118,120,123,125,130,[133], [134], [135],143,173,175,186,191,192,199,201,210,224,230,231]. During the follow up period, the pooled incidence of rejection was calculated only at 1.0% (95% CI, 0.2%-1.7%, FEM, I2 0.0%) [22,23,65,81,88,108,114,133,135,143,179,183,192,210,231].
Finally, we assessed all-cause mortality after COVID-19 in SOT recipients. We identified 37 articles and 18.6% died from any cause (95% CI, 14.8%-22.3%, REM, I2 72.4%) during their follow-up period [18,20,22,31,55,59,60,65,70,79,81,85,88,96,102,108,114,117,133,[141], [142], [143],151,152,156,158,166,179,189,190,192,210,212,216,219,229,231]
3.6. Kidney transplant recipients
We conducted the same analysis for the subset of kidney transplant recipients [16,18,[20], [21], [22], [23], [24],31,32,38,43,51,55,60,65,79,81,85,88,96,100,102,114,136,142,143,149,151,152,156,158,166,179,185,189,192,210,212,228,229,231]. Fever, cough, and shortness of breath were seen in 70.3% (95% CI, 62.5%-78.2%, REM, I2 90.6%), 65.3% (95% CI, 58.9%-71.7%, REM, I2 74.3%), and 49.3% (95% CI, 40.5%-58.2%, REM, I2 87.8%), respectively. Of note, acute kidney injury (AKI) in this group was seen in 45.4% (95% CI, 35.7%-55.1%, REM, I2 85.5%) [21,24,40,43,51,60,81,85,100,114,136,149,156,166,179,189,192,210,229,231] during entire follow-up. Anti-metabolites were reduced in 85.5% (95% CI, 79.4%-91.6%, REM, I2 84.0%), while change in CNI were seen in 48.2% (95% CI, 31.4%-65.0%, REM, I2 95.5%), and steroids only among 1.8% 95% CI, 0.6%-4.1%, FEM, I2 0.0%), In regards to treatment modalities, majority of cases were treated with hydroxychloroquine in 75.6% (95% CI, 62.3%-88.8%, REM, I2 97.1%), with azithromycin use among 50.8% (95% CI, 38.7%-62.8%, REM, I2 89.0%). IL-6 antagonists were used in 17.3% (95% CI, 10.0%-24.6%, REM, I2 88.1%), protease inhibitors in 37.7% (95% CI, 23.2%-52.2%, REM, I2 89.1%), with high dose steroids in 44.4% (95% CI, 27.3%-61.4%, REM, I2 96.5%). All-cause mortality in the subset of kidney transplant recipients was noted to be 22.0% (95% CI, 19.5%-24.4%, FEM, I2 47.1%).
3.7. Non-kidney solid organ transplant recipients
We also looked at similar outcomes in non-kidney transplant recipients. However, due to small sample size, stratification per organ type was difficult. In terms of all-cause mortality, a pooled incidence of 11.8% (95% CI, 4.2%-19.3%, REM, I2 73.4%) among liver transplant recipients [43,50,70,96,128,141,212,219] and a pooled incidence of 15.6% (95% CI, 8.5%-22.7, FEM, I2 48.5%) among heart transplant recipients was seen [40,65,96,108,117,133,190,199].
4. Discussion
This is the first full systematic review and meta-analysis regarding COVID-19 in SOT recipients during the first wave of the pandemic in terms of symptoms, treatment strategy (including reduction in immunosuppression), and short-term outcomes. First, one fifth of this vulnerable population died after COVID-19 in a short term. Next, fever was common and reported in 70.2% but respiratory symptoms (cough and shortness of breath) were found in 63.8% and 49.1% respectively. Non-respiratory symptoms such as diarrhea were also seen in 30.4%. Also, we found that in the majority of SOT recipients, antimetabolites were either reduced or stopped completely.
In the general population, risk factors for severe COVID-19 infection have been well documented, such as hypertension, older age, and diabetes mellitus. Immunosuppressive medications have been thought to be a risk factor for severe illness from COVID-19 [6]. Even our meta-analysis showed a significantly higher admission rate (81.0%) as compared to the general population, which may not entirely reflect disease severity but rather the management strategy as employed by treating physicians who may prefer closer inpatient monitoring. Our meta-analysis showed incidence of lower respiratory tract infection (based on abnormal imaging), ICU admission rate and mortality of 79.7%, 29%, and 18.6% respectively, which are all comparable to the large published data in non-SOT, general population [242]. Even though T-cell immunity against respiratory viruses in SOT recipients is thought to be lower than the general population, viral clearance for SARS-CoV-2 in SOT recipients was around a median of 3-5 weeks, which again, is almost comparable to general population [242].
Similarly, as compared to oncology patients, which were also recognized as immunocompromised and high risk for severe COVID-19, our data showed comparable outcomes especially for hospital admission rate and mortality [243]. Even though this meta-analysis shows high incidence of mortality in SOT recipients when compared with the general population [242], it is important to note that these studies are not entirely comparable given the differences in associated comorbidities within the cohorts, such as incidence of diabetes or obesity.
On the other hand, hematopoietic stem cell transplant (HSCT) recipients are treated with immunosuppressive medications as well, and sometimes even at higher doses as compared to SOT recipients. Few reports have been published regarding COVID-19 in HSCT population and Malard et. al. documented a mortality of around 40%[244], which is significantly higher than SOT recipients.
In general, secondary infection was reported and found to be rare. In our study, some authors reported bacterial infection, especially urine culture positivity in kidney transplant recipients [89,151,165,166,212]. We cannot conclude if these infections occurred due to COVID-19 or were simply hospital acquired. Six reports of Cytomegalovirus infection were found in our study [50,51,143,158,177,190]. In general, Aspergillus co-infection was also reported, Rinaldi et. al reported twelve pulmonary aspergillosis [189], Pereira et.al reported also a patient with aspergillus infection [177], while other authors report a case of a lung transplant recipient with a positive bronchoalveolar lavage for Aspergillus fumigatus [163] and a case of Aspergillus versicolor [191]. Even though SOT recipients, especially lung transplant, are at highest risk for Aspergillosis, we found a relatively lower rate of Aspergillosis after COVID-19. This may be due to a short follow-up period or use of post-lung transplant anti-mold prophylaxis, even prior to COVID-19.
This systematic review and meta-analysis has several limitations. First, we found significant heterogeneity between studies. This may be in part due to a wide variety of different transplant types, immunosuppressive agents, and a lack of uniform treatment of COVID-19. Definition of certain clinical presentations, such as fever, also varied from study to study, giving rise to further heterogeneity. Even after factoring in heterogeneity into our analyses, we could not completely overcome it. Secondly, we could only perform analyses in the subset of kidney transplant recipients. Due to sample size limitations, we could not perform the same for other transplant types. Next, the follow-up period varied significantly from study to study and that prevented us from capturing certain outcomes, such as rate of rejection, allograft dysfunction, secondary infection, and even mortality. Finally, it is important to note that this systematic review and meta-analysis reflects our initial experience with this ever rapidly growing pandemic, and as treatment modalities and strategies evolve in the coming months, this is likely to change. Moreover, differences in the available resources, epidemiology and demographics, from country to country, also play an important factor when it comes to the management of these highly immunosuppressed patients.
In conclusion, we performed a systematic review and meta-analysis of COVID-19 in SOT recipients regarding symptoms, treatment options, and outcomes. Based on this review and meta-analysis, we conclude that a higher admission rate was noted but overall outcome was similar to the general population. Further studies are still required to assess the long-term outcomes including allograft rejection, secondary infections and mortality in this highly immunocompromised patient population.
Funding
The authors declare no-funding for this study.
Disclosure
Authors of this manuscript do not have any conflicts of interest to disclose.
Authorship
M.R, MAM, APV, J.R. and Y.N. performed the literature search. M.R., MAM, V.K. and Y.N. performed the data analysis. All authors were responsible for the study design, data interpretation, and writing.
Declaration of Competing Interest
The authors of this manuscript declare no competing conflicts of interest.
Acknowledgments
Acknowledgement
The authors would like to thank Tara Brigham, MLIS, from the Mayo Clinic Libraries in Jacksonville, FL, for peer review of the Medline database search strategy.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.trre.2020.100588.
Appendix A. Supplementary data
Supplementary material 1
Supplementary material 2
References
- 1.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China, Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coronavirus disease (COVID-19) World Health Organization; 2020. Situation Report. [Google Scholar]
- 4.Kumar D., Ferreira V.H., Blumberg E., Silveira F., Cordero E., Perez-Romero P. A 5-Year Prospective Multicenter Evaluation of Influenza Infection in Transplant Recipients. Clin Infect Dis. 2018;67:1322–1329. doi: 10.1093/cid/ciy294. [DOI] [PubMed] [Google Scholar]
- 5.L'Huillier A.G., Ferreira V.H., Hirzel C., Nellimarla S., Ku T., Natori Y. T-cell responses following Natural Influenza Infection or Vaccination in Solid Organ Transplant Recipients. Sci Rep. 2020;10:10104. doi: 10.1038/s41598-020-67172-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coronavirus Disease 2019 - People of Any Age with Underlying Medical Conditions, Centers for Disease Control and Prevention.
- 7.Cao X. COVID-19: immunopathology and its implications for therapy. Nat Rev Immunol. 2020;20:269–270. doi: 10.1038/s41577-020-0308-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guillen E., Pineiro G.J., Revuelta I., Rodriguez D., Bodro M., Moreno A. Case report of COVID-19 in a kidney transplant recipient: Does immunosuppression alter the clinical presentation? Am J Transplant. 2020;20:20. doi: 10.1111/ajt.15874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh A.K., Gillies C.L., Singh R., Singh A., Chudasama Y., Coles B. Prevalence of comorbidities and their association with mortality in patients with COVID-19: A Systematic Review and Meta-analysis. Diabetes Obes Metab. 2020 doi: 10.1111/dom.14124. (Online ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan J.W., Ng C.K., Chan Y.H., Mok T.Y., Lee S., Chu S.Y. Short term outcome and risk factors for adverse clinical outcomes in adults with severe acute respiratory syndrome (SARS) Thorax. 2003;58:686–689. doi: 10.1136/thorax.58.8.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park J.E., Jung S., Kim A., Park J.E. MERS transmission and risk factors: a systematic review. BMC Public Health. 2018;18:574. doi: 10.1186/s12889-018-5484-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vishnevetsky A., Levy M. Rethinking high-risk groups in COVID-19. Mult Scler Relat Disord. 2020;42:102139. doi: 10.1016/j.msard.2020.102139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lai Q., Spoletini G., Bianco G., Graceffa D., Agnes S., Rossi M. SARS-CoV2 and immunosuppression: A double-edged sword. Transpl Infect Dis. 2020:e13404. doi: 10.1111/tid.13404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhu L., Xu X., Ma K., Yang J., Guan H., Chen S. Successful recovery of COVID-19 pneumonia in a renal transplant recipient with long-term immunosuppression. Am J Transplant. 2020;17:17. doi: 10.1111/ajt.15869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chaudhry Z.S., Williams J.D., Vahia A., Fadel R., Acosta T.P., Prashar R. Clinical Characteristics and Outcomes of COVID-19 in Solid Organ Transplant Recipients: A Case-Control Study. Am J Transplant. 2020;20:3051–3060. doi: 10.1111/ajt.16188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gandolfini I., Delsante M., Fiaccadori E., Zaza G., Manenti L., Degli Antoni A. COVID-19 in kidney transplant recipients. Am J Transplant. 2020;31:31. doi: 10.1111/ajt.15891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.M.R. Pereira, S. Mohan, D.J. Cohen, S.A. Husain, G.K. Dube, L.E. Ratner, S. Arcasoy, M.M. Aversa, L.J. Benvenuto, D.M. Dadhania, S. Kapur, L.M. Dove, R.S. Brown Jr, R.E. Rosenblatt, B. Samstein, N. Uriel, M.A. Farr, M. Satlin, C.B. Small, T.J. Walsh, R.P. Kodiyanplakkal, B.A. Miko, J.G. Aaron, D.S. Tsapepas, J.C. Emond, E.C. Verna, COVID-19 in solid organ transplant recipients: Initial report from the US epicenter, Am J Transplant, (n/a). [DOI] [PMC free article] [PubMed]
- 19.P. Cravedi, S.M. Suraj, Y. Azzi, M. Haverly, S. Farouk, M.J. Pérez-Sáez, M.D. Redondo-Pachón, B. Murphy, S. Florman, L.G. Cyrino, M. Grafals, S. Venkataraman, X.S. Cheng, A.X. Wang, G. Zaza, A. Ranghino, L. Furian, J. Manrique, U. Maggiore, I. Gandolfini, N. Agrawal, H. Patel, E. Akalin, L.V. Riella, T.T.s. group, COVID-19 and Kidney Transplantation: Results from the TANGO International Transplant Consortium, Am J Transplant, (n/a). [DOI] [PMC free article] [PubMed]
- 20.M. Crespo, A. Mazuecos, E. Rodrigo, E. Gavela, F. Villanego, E. Sánchez-Alvarez, E. González-Monte, C. Jiménez-Martín, E. Melilli, F. Diekman, S. Zárraga, D. Hernández, J. Pascual, f.t.S.S.o.N.C.-. Group, Respiratory and Gastrointestinal COVID-19 Phenotypes in Kidney Transplant Recipients, Transplantation, (Online First (9000)). [DOI] [PubMed]
- 21.A. Favà, D. Cucchiari, N. Montero, N. Toapanta, J. Centellas, A. Vila-Santandreu, A. Coloma, M. Meneghini, A. Manonelles, J. Sellarés, I. Torres, R. Gelpi, I. Lorenzo, P. Ventura-Aguiar, F. Cofan, V. Torregrosa, M. Perelló, C. Facundo, D. Seron, F. Oppenheimer, O. Bestard, J. Cruzado, F. Moreso, E. Melilli, Clinical characteristics and risk factors for severe COVID-19 in hospitalized kidney transplant recipients: A multicentric cohort study, Am J Transplant, (n/a). [DOI] [PMC free article] [PubMed]
- 22.Kates O.S., Haydel B.M., Florman S.S., Rana M.M., Chaudhry Z.S., Ramesh M.S. COVID-19 in solid organ transplant: A multi-center cohort study. Clin Infect Dis. 2020 [Google Scholar]
- 23.Fernandez-Ruiz M., Andres A., Loinaz C., Delgado J.F., Lopez-Medrano F., San Juan R. COVID-19 in solid organ transplant recipients: A single-center case series from Spain. Am J Transplant. 2020;16:16. doi: 10.1111/ajt.15929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fung M., Chiu C.Y., DeVoe C., Doernberg S.B., Schwartz B.S., Langelier C. Clinical Outcomes and Serologic Response in Solid Organ Transplant Recipients with COVID-19: A Case Series from the United States. Am J Transplant. 2020;01:01. doi: 10.1111/ajt.16079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.TL J.C. Julian Higgins, Tovey David, Thomas James, Flemyng Ella, Churchill Rachel. Methodological Expectations of Cochrane Intervention Reviews (MECIR) Cochrane Methods. 2020 [Google Scholar]
- 27.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gotzsche P.C., Ioannidis J.P. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 28.McGowan J., Sampson M., Salzwedel D.M., Cogo E., Foerster V., Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;75:40–46. doi: 10.1016/j.jclinepi.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 29.L. Kristin, COVID-19 Literature Searches, in.
- 30.MEDLINE® 2020 Database Guide, in.
- 31.S. Abolghasemi, M. Mardani, S. Sali, N. Honarvar, M. Baziboroun, COVID-19 and kidney transplant recipients, Transpl Infect Dis, (n/a e13413). [DOI] [PMC free article] [PubMed]
- 32.Abrishami A., Samavat S., Behnam B., Arab-Ahmadi M., Nafar M., Sanei Taheri M. Clinical Course, Imaging Features, and Outcomes of COVID-19 in Kidney Transplant Recipients. Eur Urol. 2020;06:06. doi: 10.1016/j.eururo.2020.04.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abuzeineh M., Muzaale A.D., Crews D.C., Avery R.K., Brotman D.J., Brennan D.C. Telemedicine in the Care of Kidney Transplant Recipients With Coronavirus Disease 2019: Case Reports. Transplant Proc. 2020;52(9):2620–2625. doi: 10.1016/j.transproceed.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adapa S., Konala V.M., Naramala S., Daggubati S.R., Koduri N.M., Gayam V. COVID-19 in Renal Transplant Patient Presenting With Active Typical Symptoms and Resolved Atypical Symptoms. J Investig Med High Impact Case Rep. 2020;8 doi: 10.1177/2324709620949307. (2324709620949307) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Adrogue A.H., Mithani F., Ibrahim H.N., Schwartz M.R., Gaber L., Hebert S.A. A Kidney Transplant Recipient With Coronavirus Disease 2019: Utility of a Prognostication Score. Transplant Proc. 2020;52:2620–2625. doi: 10.1016/j.transproceed.2020.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aiello P., Johnson S., Ramos Mercado A., Hussein S. Pneumatosis intestinalis in a patient with COVID-19. BMJ Case Rep. 2020;13 doi: 10.1136/bcr-2020-237564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aigner C., Dittmer U., Kamler M., Collaud S., Taube C. COVID-19 in a lung transplant recipient. J Heart Lung Transplant. 2020;39:610–611. doi: 10.1016/j.healun.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Akalin E., Azzi Y., Bartash R., Seethamraju H., Parides M., Hemmige V. Covid-19 and Kidney Transplantation. N Engl J Med. 2020;24:24. doi: 10.1056/NEJMc2011117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Akdur A., Karakaya E., Ayvazoglu Soy E.H., Alshalabi O., Kirnap M., Arslan H. Coronavirus Disease (COVID-19) in Kidney and Liver Transplant Patients: A Single-Center Experience. Exp Clin Transplant. 2020;18:270–274. doi: 10.6002/ect.2020.0193. [DOI] [PubMed] [Google Scholar]
- 40.Al-Darzi W., Aurora L., Michaels A., Cowger J., Grafton G., Selektor Y. Heart transplant recipients with confirmed 2019 novel coronavirus infection: The Detroit experience. Clin Transplant. 2020 doi: 10.1111/ctr.14091. [DOI] [PubMed] [Google Scholar]
- 41.Al-Makki A., Taber T. Neutropenic fever in COVID-19 in kidney transplant patient. Rev Med Virol. 2020 doi: 10.1002/rmv.2156. [DOI] [PubMed] [Google Scholar]
- 42.Alberici F., Delbarba E., Manenti C., Econimo L., Valerio F., Pola A. A single center observational study of the clinical characteristics and short-term outcome of 20 kidney transplant patients admitted for SARS-CoV2 pneumonia. Kidney Int. 2020;97:1083–1088. doi: 10.1016/j.kint.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ali T., Al-Ali A., Fajji L., Hammad E., Nazmi A., Alahmadi I. Coronavirus Disease-19: Disease Severity and Outcomes of Solid Organ Transplant Recipients: Different Spectrum of Disease in Different Populations? Transplantation. 2020 doi: 10.1097/TP.0000000000003433. [DOI] [PubMed] [Google Scholar]
- 44.Allam S.R., Dao A., Madhrira M.M., Antiporta P.B., Nair R.R., Guiteau J.J. Interleukin-6 receptor antagonist therapy to treat SARS-CoV-2 driven inflammatory syndrome in a kidney transplant recipient. Transpl Infect Dis. 2020 doi: 10.1111/tid.13326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ammirati E., Travi G., Orcese C., Sacco A., Auricchio S., Frigerio M. Heart-Kidney Transplanted patient affected by COVID-19 pneumonia treated with tocilizumab on top of immunosuppressive maintenance therapy. IJC Heart Vasc. 2020;29:100596. doi: 10.1016/j.ijcha.2020.100596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Antony S.J., Singh J., de Jesus M., Lance J. Early use of tocilizumab in respiratory failure associated with acute COVID -19 pneumonia in recipients with solid organ transplantation. IDCases. 2020;21 doi: 10.1016/j.idcr.2020.e00888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Araten D.J., Belmont H.M., Schaefer-Cutillo J., Iyengar A., Mattoo A., Reddy R. Mild Clinical Course of COVID-19 in 3 Patients Receiving Therapeutic Monoclonal Antibodies Targeting C5 Complement for Hematologic Disorders. Am J Case Rep. 2020;21 doi: 10.12659/AJCR.927418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Arenas M.D., Crespo M., Perez-Saez M.J., Collado S., Redondo-Pachon D., Llinas-Mallol L. Clinical Profiles in Renal Patients with COVID-19. J Clin Med. 2020;9 doi: 10.3390/jcm9082665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Arpali E., Akyollu B., Yelken B., Tekin S., Turkmen A., Kocak B. Case report: A kidney transplant patient with mild COVID-19. Transpl Infect Dis. 2020 doi: 10.1111/tid.13296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.M. Aversa, L. Benvenuto, M. Anderson, L. Shah, H. Robbins, M. Pereira, J. Scheffert, M. Carroll, J. Hum, M. Nolan, G. Reilly, P. Lemaitre, B.P. Stanifer, F. D’Ovidio, J. Sonett, S. Arcasoy, T.C.U.L.T. Program, COVID-19 in lung transplant recipients: A single center case series from New York City, Am J Transplant, (n/a). [DOI] [PMC free article] [PubMed]
- 51.Banerjee D., Popoola J., Shah S., Ster I.C., Quan V., Phanish M. COVID-19 infection in kidney transplant recipients. Kidney Int. 2020;97:1076–1082. doi: 10.1016/j.kint.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bartiromo M., Borchi B., Botta A., Bagala A., Lugli G., Tilli M. Threatening drug-drug interaction in a kidney transplant patient with Coronavirus Disease 2019 (COVID-19) Transpl Infect Dis. 2020;12:12. doi: 10.1111/tid.13286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Becchetti C., Zambelli M.F., Pasulo L., Donato M.F., Invernizzi F., Detry O. COVID-19 in an international European liver transplant recipient cohort. Gut. 2020 doi: 10.1136/gutjnl-2020-321923. (gutjnl-2020-321923) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Belli L.S., Duvoux C., Karam V., Adam R., Cuervas-Mons V., Pasulo L. COVID-19 in liver transplant recipients: preliminary data from the ELITA/ELTR registry. Lancet Gastroenterol Hepatol. 2020;04:04. doi: 10.1016/S2468-1253(20)30183-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.I. Benotmane, G. Gautier Vargas, M.-J. Wendling, P. Perrin, A. Velay, X. Bassand, D. Bedo, C. Baldacini, M. Sagnard, D. Bozman, M. Della Chiesa, M. Solis, F. Gallais, N. Cognard, J. Olagne, H. Delagreverie, L. Gontard, B. Panaget, D. Marx, F. Heibel, L. Braun, B. Moulin, S. Caillard, S. Fafi-Kremer, In-depth virological assessment of kidney transplant recipients with COVID-19, Am J Transplant, (n/a). [DOI] [PMC free article] [PubMed]
- 56.Benotmane I., Perrin P., Gautier Vargas G., Bassand X., Keller N., Lavaux T. Biomarkers of Cytokine Release Syndrome Predict Disease Severity and Mortality From COVID-19 in Kidney Transplant Recipients. Transplantation. 2020 doi: 10.1097/TP.0000000000003480. [DOI] [PubMed] [Google Scholar]
- 57.Bhoori S., Rossi R.E., Citterio D., Mazzaferro V. COVID-19 in long-term liver transplant patients: preliminary experience from an Italian transplant centre in Lombardy. Lancet Gastroenterol Hepatol. 2020;5:532–533. doi: 10.1016/S2468-1253(20)30116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Billah M., Santeusanio A., Delaney V., Cravedi P., Farouk S.S. A catabolic state in a kidney transplant recipient with COVID-19. Transpl Int. 2020;01:01. doi: 10.1111/tri.13635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.F. Bösch, N. Börner, S. Kemmner, C. Lampert, S. Jacob, D. Koliogiannis, M. Stangl, S. Michel, N. Kneidinger, C. Schneider, M. Fischereder, M. Irlbeck, G. Denk, J. Werner, M.K. Angele, M.O. Guba, Attenuated early inflammatory response in solid organ recipients with COVID-19, Clin Transplant, (n/a e14027). [DOI] [PMC free article] [PubMed]
- 60.N. Bossini, F. Alberici, E. Delbarba, F. Valerio, C. Manenti, S. Possenti, L. Econimo, C. Maffei, A. Pola, V. Terlizzi, C. Salviani, M. Moscato, S. Pasquali, N. Zambetti, M. Tonoli, S. Affatato, P. Pecchini, F. Battista Viola, F. Malberti, G. Depetri, M. Gaggiotti, F. Scolari, T.B.R.C.t. force, Kidney transplant patients with SARS-CoV-2 infection: the brescia renal COVID task force experience, Am J Transplant, (n/a). [DOI] [PMC free article] [PubMed]
- 61.Buscemi V., De Carlis R., Lauterio A., Merli M., Puoti M., De Carlis L. Does interval time between liver transplant and COVID-19 infection make the difference? Dig Liver Dis. 2020 doi: 10.1016/j.dld.2020.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bush R., Johns F., Acharya R., Upadhyay K. Mild COVID-19 in a pediatric renal transplant recipient. Am J Transplant. 2020;13:13. doi: 10.1111/ajt.16003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bussalino E., De Maria A., Russo R., Paoletti E. Immunosuppressive therapy maintenance in a kidney transplant recipient with SARS-CoV-2 pneumonia: A case report. Am J Transplant. 2020;13:13. doi: 10.1111/ajt.15920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Carey S.A., Afzal A., Jamil A., Williams S., Gottlieb R.L. Outpatient COVID-19 surveillance testing in orthotopic heart transplant recipients. Clin Transplant. 2020 doi: 10.1111/ctr.14105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cavagna L., Seminari E., Zanframundo G., Gregorini M., Di Matteo A., Rampino T. Calcineurin Inhibitor-Based Immunosuppression and COVID-19: Results from a Multidisciplinary Cohort of Patients in Northern Italy. Microorganisms. 2020;8 doi: 10.3390/microorganisms8070977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen S., Yin Q., Shi H., Du D., Chang S., Ni L. A familial cluster, including a kidney transplant recipient, of Coronavirus Disease 2019 (COVID-19) in Wuhan, China. Am J Transplant. 2020;03:03. doi: 10.1111/ajt.15903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cheng D.R., Wen J.Q., Liu Z.Z., Lv T.F., Chen J.S. Coronavirus disease 2019 in renal transplant recipients: report of two cases. Transpl Infect Dis. 2020 doi: 10.1111/tid.13329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chenna A., Konala V.M., Gayam V., Naramala S., Adapa S. Coronavirus Disease 2019 (COVID-19) in a Renal Transplant Patient. Cureus. 2020;12 doi: 10.7759/cureus.8038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Christensen J., Kumar D., Moinuddin I., Bryson A., Kashi Z., Kimball P. Coronavirus Disease 2019 Viremia, Serologies, and Clinical Course in a Case Series of Transplant Recipients. Transplant Proc. 2020;52:2637–2641. doi: 10.1016/j.transproceed.2020.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.J. Colmenero, M. Rodríguez-Perálvarez, M. Salcedo, A. Arias-Milla, A. Muñoz-Serrano, J. Graus, J. Nuño, M. Gastaca, J. Bustamante-Schneider, A. Cachero, L. Lladó, A. Caballero, A. Fernández-Yunquera, C. Loinaz, I. Fernández, C. Fondevila, M. Navasa, M. Iñarrairaegui, L. Castells, S. Pascual, P. Ramírez, C. Vinaixa, M.L. González-Dieguez, R. González-Grande, L. Hierro, F. Nogueras, A. Otero, J.M. Álamo, G. Blanco-Fernández, E. Fábrega, F. García-Pajares, J.L. Montero, S. Tomé, G. De la Rosa, J.A. Pons, Epidemiological pattern, incidence and outcomes of COVID-19 in liver transplant patients, J Hepatol. [DOI] [PMC free article] [PubMed]
- 71.P. Columbia University Kidney Transplant, Early Description of Coronavirus 2019 Disease in Kidney Transplant Recipients in New York, J Am Soc Nephrol, 31 (2020) 1150-1156. [DOI] [PMC free article] [PubMed]
- 72.Cozzi E., Faccioli E., Marinello S., Loy M., Congedi S., Calabrese F. COVID-19 pneumonia in lung transplant recipients: report of two cases. Am J Transplant. 2020;12:12. doi: 10.1111/ajt.15993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Crespo M., Jose Perez-Saez M., Redondo-Pachon D., Llinas-Mallol L., Montero M.M., Villar J. COVID-19 in elderly kidney transplant recipients. Am J Transplant. 2020;29:29. doi: 10.1111/ajt.16096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dahl Mathiasen V., Jensen-Fangel S., Skov K., Leth S. Uneventful case of COVID-19 in a kidney transplant recipient. BMJ Case Rep. 2020;13 doi: 10.1136/bcr-2020-237427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dajti E., Cristini F., Tamanini G., Cescon M., Bazzoli F., Tame M. COVID-19 in a young liver transplant recipient: caution for drug-drug interactions. J Gastrointestin Liver Dis. 2020;29:470. doi: 10.15403/jgld-2672. [DOI] [PubMed] [Google Scholar]
- 76.De Francesco M.A., Alberici F., Bossini N., Scolari F., Pascucci F., Tomasoni G. Pneumocystis jirevocii and SARS-CoV-2 Co-Infection: A Common Feature in Transplant Recipients? Vaccines (Basel) 2020;8 doi: 10.3390/vaccines8030544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.De Gottardi A., Fratila C., Bertoli R., Cerny A., Magenta L., Gianella P. Clinical characteristics and management of a liver transplanted patient admitted with SARS-CoV-2 infection. Clin Res Hepatol Gastroenterol. 2020 doi: 10.1016/j.clinre.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Decker A., Welzel M., Laubner K., Grundmann S., Kochs G., Panning M. Prolonged SARS-CoV-2 shedding and mild course of COVID-19 in a patient after recent heart transplantation. Am J Transplant. 2020;09:09. doi: 10.1111/ajt.16133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.E. Demir, M. Uyar, E. Parmaksiz, A. Sinangil, B. Yelken, A.B. Dirim, O. Merhametsiz, S. Yadigar, Z. Atan Ucar, A.R. Ucar, M.E. Demir, M. Mese, E.B. Akin, N. Garayeva, S. Safak, O.A. Oto, H. Yazici, A. Turkmen, COVID-19 in kidney transplant recipients: A multicenter experience in Istanbul, Transpl Infect Dis, (n/a e13371). [DOI] [PMC free article] [PubMed]
- 80.N. Desmazes-Dufeu, B. Coltey, L. Amari, M. Gouitaa, C. Touzery, M. Reynaud-Gaubert, P. Chanez, N. Cassir, Discordant courses of COVID-19 in a cohabiting couple of lung transplant recipients, Transpl Infect Dis, (n/a e13410). [DOI] [PMC free article] [PubMed]
- 81.A. Devresse, L. Belkhir, B. Vo, B. Ghaye, A. Scohy, B. Kabamba, E. Goffin, J. De Greef, M. Mourad, M. De Meyer, J.-C. Yombi, N. Kanaan, COVID-19 Infection in Kidney Transplant Recipients: A Single-Center Case Series of 22 Cases From Belgium, Kidney Medicine [DOI] [PMC free article] [PubMed]
- 82.Dirim A.B., Demir E., Ucar A.R., Garayeva N., Safak S., Oto O.A. Fatal SARS-CoV-2 infection in a renal transplant recipient. CEN Case Reports. 2020:409–412. doi: 10.1007/s13730-020-00496-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Doevelaar A.A.N., Holzer B., Seibert F.S., Bauer F., Stervbo U., Rohn B.J. Lessons for the clinical nephrologist: recurrence of nephrotic syndrome induced by SARS-CoV-2. J Nephrol. 2020 doi: 10.1007/s40620-020-00855-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dube G.K., Husain S.A., McCune K.R., Sandoval P.R., Ratner L.E., Cohen D.J. COVID-19 infection in pancreas transplant recipients. Transpl Infect Dis. 2020 doi: 10.1111/tid.13359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Elias M., Pievani D., Randoux C., Louis K., Denis B., Delion A. COVID-19 Infection in Kidney Transplant Recipients: Disease Incidence and Clinical Outcomes. J Am Soc Nephrol. 2020;31:2413–2423. doi: 10.1681/ASN.2020050639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Faguer S., Del Bello A., Abravanel F., Nicolau-Travers M.L., Kamar N. Tocilizumab for Hemophagocytic Syndrome in a Kidney Transplant Recipient With COVID-19. Ann Intern Med. 2020;18:18. doi: 10.7326/L20-0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Farfour E., Picard C., Beaumont L., Lesprit P., Ballester M.C., Ackermann F. COVID-19 in lung-transplanted and cystic fibrosis patients: Be careful. J Cyst Fibros. 2020;10:10. doi: 10.1016/j.jcf.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Felldin M., Softeland J.M., Magnusson J., Ekberg J., Karason K., Schult A. Initial Report From a Swedish High-Volume Transplant Center After The First Wave of The COVID-19 Pandemic. Transplantation. 2020 doi: 10.1097/TP.0000000000003436. [DOI] [PubMed] [Google Scholar]
- 89.Fontana F., Alfano G., Mori G., Amurri A., Tei L., Ballestri M. COVID-19 pneumonia in a kidney transplant recipient successfully treated with tocilizumab and hydroxychloroquine. Am J Transplant. 2020;23:23. doi: 10.1111/ajt.15935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fung M., Nambiar A., Pandey S., Aldrich J.M., Teraoka J., Freise C. Treatment of Immunocompromised COVID-19 patients with Convalescent Plasma. Transpl Infect Dis. 2020 doi: 10.1111/tid.13477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.K. Gajurel, Persistently positive severe acute respiratory syndrome coronavirus 2 (SARS-COV2) nasopharyngeal PCR in a kidney transplant recipient, Transpl Infect Dis, (n/a e13408). [DOI] [PMC free article] [PubMed]
- 92.Gao F., Zheng K.I., Gu J.Y., George J., Zheng M.H. COVID-19 and liver transplantation: Lessons learned from three reported cases. Transpl Infect Dis. 2020 doi: 10.1111/tid.13335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gautier-Vargas G., Baldacini C., Benotmane I., Keller N., Perrin P., Moulin B. Rapid resolution of cytokine release syndrome and favorable clinical course of severe COVID-19 in a kidney transplant recipient treated with tocilizumab. Kidney Int. 2020;04:04. doi: 10.1016/j.kint.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.E. Giorgakis, S.P. Zehtaban, A.E. Stevens, S. Bhusal, L. Burdine, COVID-19 in solid organ transplant recipients, Transpl Infect Dis, (n/a e13419). [DOI] [PMC free article] [PubMed]
- 95.Goodlet K.J., Bansal S., Arjuna A., Nailor M.D., Buddhdev B., Abdelrazek H. COVID-19 in a lung transplant recipient: Exploring the diagnostic role of circulating exosomes and the clinical impact of advanced immunosuppression. Transpl Infect Dis. 2020 doi: 10.1111/tid.13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Goss M.B., Galvan N.T.N., Ruan W., Munoz F.M., Brewer E.D., O'Mahony C.A. The Pediatric Solid Organ Transplant Experience with COVID-19: An Initial Multi-Center, Multi-Organ Case Series. Pediatr Transplant. 2020:e13868. doi: 10.1111/petr.13868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Guella A., Elfadil O., Abdulrazaq G., Osman S., Khan M.M., Ahmed A. Favorable Outcome of COVID-19 Pneumonia in a Kidney Transplant Recipient Treated with Tocilizumab. Case Rep Infect Dis. 2020;2020:8830626. doi: 10.1155/2020/8830626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hammami M.B., Garibaldi B., Shah P., Liu G., Jain T., Chen P.H. Clinical course of COVID-19 in a liver transplant recipient on hemodialysis and response to tocilizumab therapy: A case report. Am J Transplant. 2020;02:02. doi: 10.1111/ajt.15985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hann A., Lembach H., McKay S.C., Perrin M., Isaac J., Oo Y.H. Controversies Regarding Shielding and Susceptibility to COVID-19 Disease in Liver transplant Recipients in the United Kingdom. Transpl Infect Dis. 2020 doi: 10.1111/tid.13352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.S. Hartzell, S. Bin, C. Benedetti, M. Haverly, L. Gallon, G. Zaza, L.V. Riella, M.C. Menon, S. Florman, A.H. Rahman, J.M. Leech, P.S. Heeger, P. Cravedi, Evidence of potent humoral immune activity in COVID19-infected kidney transplant recipients, Am J Transplant, (n/a). [DOI] [PMC free article] [PubMed]
- 101.N. Heinz, A. Griesemer, J. Kinney, J. Vittorio, S.M. Lagana, D. Goldner, M. Velasco, T. Kato, S. Lobritto, M. Martinez, A case of an Infant with SARS-CoV-2 hepatitis early after liver transplantation, Pediatr Transplant, (n/a e13778). [DOI] [PMC free article] [PubMed]
- 102.Hoek R.A.S., Manintveld O.C., Betjes M.G.H., Hellemons M.E., Seghers L., van Kampen J.A.A. Covid-19 in solid organ transplant recipients: A single center experience. Transpl Int. 2020;27:27. doi: 10.1111/tri.13662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Holzhauser L., Lourenco L., Sarswat N., Kim G., Chung B., Nguyen A.B. Early Experience of COVID-19 in Two Heart Transplant Recipients: Case Reports and Review of Treatment Options. American journal of transplantation. 2020 doi: 10.1111/ajt.15982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hsu J.J., Gaynor P., Kamath M., Fan A., Al-Saffar F., Cruz D. COVID-19 in a High-Risk Dual Heart and Kidney Transplant Recipient. Am J Transplant. 2020;21:21. doi: 10.1111/ajt.15936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Huang J., Lin H., Wu Y., Fang Y., Kumar R., Chen G. COVID-19 in posttransplant patients-report of 2 cases. Am J Transplant. 2020;03:03. doi: 10.1111/ajt.15896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Huang J.F., Zheng K.I., George J., Gao H.N., Wei R.N., Yan H.D. Fatal outcome in a liver transplant recipient with COVID-19. Am J Transplant. 2020;10:10. doi: 10.1111/ajt.15909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Husain S.A., Dube G., Morris H., Fernandez H., Chang J.H., Paget K. Early Outcomes of Outpatient Management of Kidney Transplant Recipients with Coronavirus Disease 2019. Clin J Am Soc Nephrol. 2020;15:1174–1178. doi: 10.2215/CJN.05170420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Iacovoni A., Boffini M., Pidello S., Simonato E., Barbero C., Sebastiani R. A case series of Novel-Coronavirus infection in heart transplantation from two centers in the pandemic area in the North of Italy. J Heart Lung Transplant. 2020;39:1081–1088. doi: 10.1016/j.healun.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jang K., Khatri A., Majure D.T. COVID-19 Leading to Acute Encephalopathy in a Heart Transplant Patient. J Heart Lung Transplant. 2020;39:853–855. doi: 10.1016/j.healun.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.J. Jiang, Y. Miao, Y. Zhao, X. Lu, P. Zhou, X. Zhou, Z. Chen, D. Du, Convalescent plasma therapy: Helpful treatment of COVID-19 in a kidney transplant recipient presenting with serve clinical manifestation and complex complications, Clin Transplant, (n/a e14025). [DOI] [PMC free article] [PubMed]
- 111.Johnson K.M., Belfer J.J., Peterson G.R., Boelkins M.R., Dumkow L.E. Managing COVID-19 in Renal Transplant Recipients: A Review of Recent Literature and Case Supporting Corticosteroid-sparing Immunosuppression. Pharmacotherapy. 2020;40:517–524. doi: 10.1002/phar.2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kadosh B.S., Pavone J., Wu M., Reyentovich A., Gidea C. Collapsing Glomerulopathy Associated with COVID-19 Infection in a Heart Transplant Recipient. J Heart Lung Transplant. 2020;39:855–857. doi: 10.1016/j.healun.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kates O.S., Fisher C.E., Stankiewicz-Karita H.C., Shepherd A.K., Church E.C., Kapnadak S.G. Earliest cases of coronavirus disease 2019 (COVID-19) identified in solid organ transplant recipients in the United States. Am J Transplant. 2020;24:24. doi: 10.1111/ajt.15944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Katz-Greenberg G., Yadav A., Gupta M., Martinez-Cantarin M.P., Gulati R., Ackerman L. Outcomes of COVID-19-positive kidney transplant recipients: A single-center experience. Clin Nephrol. 2020;94 doi: 10.5414/CN110311. [DOI] [PubMed] [Google Scholar]
- 115.Keller B.C., Le A., Sobhanie M., Colburn N., Burcham P., Rosenheck J. Early COVID-19 infection after lung transplantation. Am J Transplant. 2020;29:29. doi: 10.1111/ajt.16097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kemmner S., Guba M.O., Schonermarck U., Stangl M., Fischereder M. Cyclosporine as a preferred calcineurin inhibitor in renal allograft recipients with COVID-19 infection. Kidney Int. 2020;98 doi: 10.1016/j.kint.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ketcham S.W., Adie S.K., Malliett A., Abdul-Aziz A.A., Bitar A., Grafton G. Coronavirus Disease-2019 in Heart Transplant Recipients in Southeastern Michigan: A Case Series. J Card Fail. 2020;14:14. doi: 10.1016/j.cardfail.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kim Y., Kwon O., Paek J.H., Park W.Y., Jin K., Hyun M. Two distinct cases with COVID-19 in kidney transplant recipients. Am J Transplant. 2020;26:26. doi: 10.1111/ajt.15947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kocak B., Arpali E., Akyollu B., Yelken B., Tekin S., Kanbay M. A Case Report of Oligosymptomatic Kidney Transplant Patients with COVID-19: Do They Pose a Risk to Other Recipients? Transplant Proc. 2020;15:15. doi: 10.1016/j.transproceed.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Koczulla R.A., Sczepanski B., Koteczki A., Kuhnert S., Hecker M., Askevold I. SARS-CoV-2 infection in two patients following recent lung transplantation. Am J Transplant. 2020;12:12. doi: 10.1111/ajt.15998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.A. Kolonko, S. Dudzicz, A. Wiecek, R. Król, COVID-19 infection in solid organ transplant recipients: A single-center experience with patients immediately after transplantation, Transpl Infect Dis, (n/a e13381). [DOI] [PMC free article] [PubMed]
- 122.Kumar R.N., Tanna S.D., Shetty A.A., Stosor V. COVID-19 in an HIV-positive Kidney Transplant Recipient. Transpl Infect Dis. 2020 doi: 10.1111/tid.13338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lagana S.M., De Michele S., Lee M.J., Emond J.C., Griesemer A.D., Tulin-Silver S.A. COVID-19 Associated Hepatitis Complicating Recent Living Donor Liver Transplantation. Arch Pathol Lab Med. 2020;17:17. doi: 10.5858/arpa.2020-0186-SA. [DOI] [PubMed] [Google Scholar]
- 124.Latif F., Farr M.A., Clerkin K.J., Habal M.V., Takeda K., Naka Y. Characteristics and Outcomes of Recipients of Heart Transplant With Coronavirus Disease 2019. JAMA Cardiol. 2020;13:13. doi: 10.1001/jamacardio.2020.2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lauterio A., Valsecchi M., Santambrogio S., De Carlis R., Merli M., Calini A. Successful recovery from severe COVID-19 pneumonia after kidney transplantation: The interplay between immunosuppression and novel therapy including tocilizumab. Transpl Infect Dis. 2020 doi: 10.1111/tid.13334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.H. Lazareth, H. Péré, Y. Binois, M. Chabannes, J. Schurder, T. Bruneau, A. Karras, E. Thervet, M. Rabant, D. Veyer, N. Pallet, COVID-19–Related Collapsing Glomerulopathy in a Kidney Transplant Recipient, Am J Kidney Dis [DOI] [PMC free article] [PubMed]
- 127.Le M.P., Le Hingrat Q., Jaquet P., Wicky P.H., Bunel V., Massias L. Removal of Remdesivir's Metabolite GS-441524 by Hemodialysis in a Double Lung Transplant Recipient with COVID-19. Antimicrob Agents Chemother. 2020;64 doi: 10.1128/AAC.01521-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lee B.T., Perumalswami P.V., Im G.Y., Florman S., Schiano T.D. COVID-19 in Liver Transplant Recipients: An Initial Experience from the U.S. Epicenter. Gastroenterology. 2020;19:19. doi: 10.1053/j.gastro.2020.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.H. Lee, B.S. Mantell, M.E. Richmond, S.P. Law, W.A. Zuckerman, L.J. Addonizio, T.M. Lee, I.D. Lytrivi, Varying Presentations of COVID-19 in Young Heart Transplant Recipients: A Case Series, Pediatr Transplant, (n/a e13780). [DOI] [PMC free article] [PubMed]
- 130.Li F., Cai J., Dong N. First cases of COVID-19 in heart transplantation from China. J Heart Lung Transplant. 2020;39:496–497. doi: 10.1016/j.healun.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Li H., Liu L., Zhang D., Xu J., Dai H., Tang N. SARS-CoV-2 and viral sepsis: observations and hypotheses. Lancet. 2020;395:1517–1520. doi: 10.1016/S0140-6736(20)30920-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Li Q.Y., Cheng Q., Zhao Z.L., Dai N.N., Zeng L., Zhu L. Severe acute respiratory syndrome coronavirus 2 infection in renal transplant recipients: A case report. Health sciences. 2020;52:780–784. doi: 10.19723/j.issn.1671-167X.2020.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.B. Lima, G.T. Gibson, S. Vullaganti, K. Malhame, S. Maybaum, S.T. Hussain, S. Shah, D.T. Majure, F. Wallach, K. Jang, V. Bijol, M.J. Esposito, A.K. Williamson, R.M. Thomas, T.A. Bhuiya, H.A. Fernandez, G.R. Stevens, COVID-19 in recent heart transplant recipients: Clinicopathologic features and early outcomes, Transpl Infect Dis, (n/a e13382). [DOI] [PMC free article] [PubMed]
- 134.Liu B., Wang Y., Zhao Y., Shi H., Zeng F., Chen Z. Successful treatment of severe COVID-19 pneumonia in a liver transplant recipient. Am J Transplant. 2020;03:03. doi: 10.1111/ajt.15901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.C. Loinaz, A. Marcacuzco, M. Fernández-Ruiz, O. Caso, F. Cambra, R. San Juan, I. Justo, J. Calvo, A. García-Sesma, A. Manrique, M.A. Pérez-Jacoiste Asín, M.D. Folgueira, J.M. Aguado, C. Lumbreras, Varied clinical presentation and outcome of SARS-CoV-2 infection in liver transplant recipients: Initial experience at a single center in Madrid, Spain, Transpl Infect Dis, (n/a e13372). [DOI] [PMC free article] [PubMed]
- 136.Lubetzky M., Aull M.J., Craig-Schapiro R., Lee J.R., Marku-Podvorica J., Salinas T. Kidney allograft recipients, immunosuppression, and coronavirus disease-2019: a report of consecutive cases from a New York City transplant center. Nephrol Dial Transplant. 2020;35:1250–1261. doi: 10.1093/ndt/gfaa154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Ma B.M., Hung I.F.N., Chan G.C.W., Tam A.R., Chan S.S.K., Wong B.C.K. Case of "relapsing" COVID-19 in a kidney transplant recipient. Nephrology (Carlton) 2020 doi: 10.1111/nep.13786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Machado D.J.B., Ianhez L.E. COVID-19 pneumonia in kidney transplant recipients-Where we are? Transpl Infect Dis. 2020 doi: 10.1111/tid.13306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Malekhosseini S.A., Nikoupour H., Gholami S., Shamsaeefar A., Arasteh P., Kazemi K. A Report of 85 Cases of COVID-19 and Abdominal Transplantation From a Single Center: What Are the Associated Factors With Death Among Organ Transplantation Patients. Transplantation. 2020 doi: 10.1097/TP.0000000000003470. [DOI] [PubMed] [Google Scholar]
- 140.Man Z., Jing Z., Huibo S., Bin L., Fanjun Z. Viral shedding prolongation in a kidney transplant patient with COVID-19 pneumonia. Am J Transplant. 2020;13:13. doi: 10.1111/ajt.15996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Mansoor E., Perez A., Abou-Saleh M., Sclair S.N., Cohen S., Cooper G.S. Clinical Characteristics, Hospitalization and Mortality Rates of COVID-19 Among Liver Transplant Patients in the United States: A Multi-Center Research Network Study. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Marcault C., Fodil S., Dupont T., Darmon M., Azoulay E. In response to the letter of Montagud-Marrahi et al. Am J Transplant. 2020;08:08. doi: 10.1111/ajt.16126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.F. Maritati, E. Cerutti, L. Zuccatosta, A. Fiorentini, C. Finale, M. Ficosecco, F. Cristiano, A. Capestro, E. Balestra, D. Taruscia, M. Vivarelli, A. Donati, G.P. Perna, A. Giacometti, M. Tavio, M. Onesta, L. Di Sante, A. Ranghino, SARS-CoV-2 infection in kidney transplant recipients: experience of the italian marche region, Transpl Infect Dis, (n/a e13377). [DOI] [PMC free article] [PubMed]
- 144.Marx D., Moulin B., Fafi-Kremer S., Benotmane I., Gautier G., Perrin P. First case of COVID-19 in a kidney transplant recipient treated with belatacept. Am J Transplant. 2020;13:13. doi: 10.1111/ajt.15919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Masset C., Ville S., Halary F., Gaborit B., Bressolette-Bodin C., Deltombe C. Resurgence of BK virus following Covid-19 in kidney transplant recipients. Transpl Infect Dis. 2020 doi: 10.1111/tid.13465. [DOI] [PubMed] [Google Scholar]
- 146.Massoumi H., Rocca J., Frager S., Kinkhabwala M. COVID-19 Infection in Early Post-Operative Period after Liver Transplantation. Liver Transpl. 2020;05:05. [Google Scholar]
- 147.Mathies D., Rauschning D., Wagner U., Mueller F., Maibaum M., Binnemann C. A Case of SARS-CoV-2-pneumonia with successful antiviral therapy in a 77-year-old male with heart transplant. Am J Transplant. 2020;21:21. doi: 10.1111/ajt.15932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.M. Mattioli, E. Fustini, S. Gennarini, Heart transplant recipient patient with COVID-19 treated with tocilizumab, Transpl Infect Dis, (n/a e13380). [DOI] [PubMed]
- 149.S.A. Mehta, J. Leonard, P. Labella, K. Cartiera, I. Soomro, H. Neumann, R.A. Montgomery, N.M. Ali, Outpatient management of kidney transplant recipients with suspected COVID-19—Single-center experience during the New York City surge, Transpl Infect Dis, (n/a e13383). [DOI] [PMC free article] [PubMed]
- 150.Melgosa M., Madrid A., Alvarez O., Lumbreras J., Nieto F., Parada E. A. Spanish Pediatric Nephrology, SARS-CoV-2 infection in Spanish children with chronic kidney pathologies. Pediatr Nephrol. 2020;20:20. doi: 10.1007/s00467-020-04597-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Mella A., Mingozzi S., Gallo E., Lavacca A., Rossetti M.M., Clari R. Case series of six kidney transplanted patients with COVID-19 pneumonia treated with tocilizumab. Transpl Infect Dis. 2020:e13348. doi: 10.1111/tid.13348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.S. Meziyerh, D. van der Helm, A.P.J. de Vries, Vulnerabilities in kidney transplant recipients with COVID-19: a single center experience, Transpl Int, (n/a). [DOI] [PMC free article] [PubMed]
- 153.Meziyerh S., Zwart T.C., van Etten R.W., Janson J.A., van Gelder T., Alwayn I.P.J. Severe COVID-19 in a renal transplant recipient: A focus on pharmacokinetics. Am J Transplant. 2020;26:26. doi: 10.1111/ajt.15943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Miarons M., Larrosa-Garcia M., Garcia-Garcia S., Los-Arcos I., Moreso F., Berastegui C. COVID-19 in Solid Organ Transplantation: A Matched Retrospective Cohort Study and Evaluation of Immunosuppression Management. Transplantation. 2020 doi: 10.1097/TP.0000000000003460. [DOI] [PubMed] [Google Scholar]
- 155.Modi A.R., Koval C.E., Taege A.J., Modaresi Esfeh J., Eghtesad B., Menon K.V.N. Coronavirus Disease 2019 in an Orthotopic Liver Transplant Recipient Living with Human Immunodeficiency Virus. Transpl Infect Dis. 2020 doi: 10.1111/tid.13351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.I.H. Mohamed, P.B. Chowdary, S. Shetty, C. Sammartino, R. Sivaprakasam, B. Lindsey, R. Thuraisingham, M.M. Yaqoob, M.A. Khurram, Outcomes of Renal Transplant Recipients With SARS-CoV-2 Infection in the Eye of the Storm: A Comparative Study With Waitlisted Patients, Transplantation, (Online First (9000)). [DOI] [PubMed]
- 157.Mohamed M.A., Kaur J., Wani F., Kichloo A., Bhanot R. Renal Transplant Recipient with Concurrent COVID-19 and Stenotrophomonas maltophilia Pneumonia Treated with Trimethoprim/Sulfamethoxazole Leading to Acute Kidney Injury: A Therapeutic Dilemma. Am J Case Rep. 2020;21 doi: 10.12659/AJCR.926464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Molaei H., Khedmat L., Nemati E., Rostami Z., Saadat S.H. Iranian kidney transplant recipients with COVID-19 infection: Clinical outcomes and cytomegalovirus coinfection. Transpl Infect Dis. 2020 doi: 10.1111/tid.13455. [DOI] [PubMed] [Google Scholar]
- 159.Molnar M.Z., Bhalla A., Azhar A., Tsujita M., Talwar M., Balaraman V. Outcomes of critically ill solid organ transplant patients with COVID-19 in the United States. Am J Transplant. 2020;20:3061–3071. doi: 10.1111/ajt.16280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.A. Monfared, S. Dashti-Khavidaki, R. Jafari, A. Jafari, E. Ramezanzade, M.-K. Lebadi, Y. Haghdar-Saheli, P. Aghajanzadeh, M. Khosravi, A. Movassaghi, H. Taghvaye-Masoumi, A. Alavi Foumani, Clinical characteristics and outcome of COVID-19 pneumonia in kidney transplant recipients in Razi hospital, Rasht, Iran, Transpl Infect Dis, (n/a e13420). [DOI] [PMC free article] [PubMed]
- 161.Morand A., Roquelaure B., Colson P., Amrane S., Bosdure E., Raoult D. Child with liver transplant recovers from COVID-19 infection. A case report. Arch Pediatr. 2020;06:06. doi: 10.1016/j.arcped.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Morillas J.A., Marco Canosa F., Srinivas P., Asadi T., Calabrese C., Rajendram P. Tocilizumab therapy in five solid and composite tissue transplant recipients with early ARDS due to SARS-CoV-2. Am J Transplant. 2020;31:31. doi: 10.1111/ajt.16080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Morlacchi L.C., Rossetti V., Gigli L., Amati F., Rosso L., Aliberti S. COVID-19 In Lung Transplant Recipients: A Case Series From Milan, Italy. Transpl Infect Dis. 2020:e13356. doi: 10.1111/tid.13356. [DOI] [PubMed] [Google Scholar]
- 164.Muller H., Kniepeiss D., Stauber R., Schrem H., Rauter M., Krause R. Recovery from COVID-19 following Hepatitis C, Human Immunodeficiency Virus Infection and Liver Transplantation. Am J Transplant. 2020;03:03. doi: 10.1111/ajt.16107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.S. Naeem, R. Gohh, G. Bayliss, C. Cosgrove, D. Farmakiotis, B. Merhi, P. Morrissey, A. Osband, J.A. Bailey, J. Sweeney, R. Rogers, Successful recovery from COVID-19 in three kidney transplant recipients who received convalescent plasma therapy, Transpl Infect Dis, (n/a e13451). [DOI] [PMC free article] [PubMed]
- 166.Nair V., Jandovitz N., Hirsch J.S., Nair G., Abate M., Bhaskaran M. COVID-19 in kidney transplant recipients. Am J Transplant. 2020;29:29. doi: 10.1111/ajt.15967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Namazee N., Mahmoudi H., Afzal P., Ghaffari S. Novel Corona Virus 2019 pneumonia in a kidney transplant recipient. Am J Transplant. 2020;13:13. doi: 10.1111/ajt.15999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Niknam R., Malek-Hosseini S.A., Hashemieh S.S., Dehghani M. COVID-19 in Liver Transplant Patients: Report of 2 Cases and Review of the Literature. Int Med Case Rep J. 2020;13:317–321. doi: 10.2147/IMCRJ.S265910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Nikoupour H., Arasteh P., Gholami S., Nikeghbalian S. Liver transplantation and COVID-19: a case report and cross comparison between two identical twins with COVID-19. BMC Surg. 2020;20:181. doi: 10.1186/s12893-020-00837-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Ning L., Liu L., Li W., Liu H., Wang J., Yao Z. Novel coronavirus (SARS-CoV-2) infection in a renal transplant recipient: Case report. Am J Transplant. 2020;10:10. doi: 10.1111/ajt.15897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Noble R., Tan M.Y., McCulloch T., Shantier M., Byrne C., Hall M. Collapsing Glomerulopathy Affecting Native and Transplant Kidneys in Individuals with COVID-19. Nephron. 2020:1–6. doi: 10.1159/000509938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Oniszczuk J., Moktefi A., Mausoleo A., Pallet N., Malard-Castagnet S., Fourati S. De Novo Focal and Segmental Glomerulosclerosis After COVID-19 in a Patient With a Transplanted Kidney From a Donor With a High-risk APOL1 Variant. Transplantation. 2020 doi: 10.1097/TP.0000000000003432. [DOI] [PubMed] [Google Scholar]
- 173.Ossami Saidy R.R., Globke B., Pratschke J., Schoening W., Eurich D. Successful implementation of preventive measures leads to low relevance of SARS-CoV-2 in liver transplant patients: Observations from a German outpatient department. Transpl Infect Dis. 2020 doi: 10.1111/tid.13363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.R. Papa-Gobbi, A. Bueno, J. Serradilla, P. Talayero, P. Stringa, B. Pascual-Miguel, A. Alcolea-Sánchez, R. González-Sacristan, A.M. Andrés, M. López-Santamaría, M. Rumbo, E. Ramos-Boluda, F. Hernández-Oliveros, Novel coronavirus (SARS-CoV-2) infection in a patient with multivisceral transplant, Transpl Infect Dis, (n/a e13430). [DOI] [PMC free article] [PubMed]
- 175.J. Pascual, E. Melilli, C. Jiménez-Martín, E. González-Monte, S. Zárraga, A. Gutiérrez-Dalmau, V. López-Jiménez, J. Juega, M. Muñoz-Cepeda, I. Lorenzo, C. Facundo, M.D.C. Ruiz-Fuentes, A. Mazuecos, E. Sánchez-Álvarez, M. Crespo, C.-G. Spanish Society of Nephrology, COVID-19-related Mortality During the First 60 Days After Kidney Transplantation, Eur Urol, (2020) S0302-2838(0320)30465-30466. [DOI] [PMC free article] [PubMed]
- 176.Patrono D., Lupo F., Canta F., Mazza E., Mirabella S., Corcione S. Outcome of COVID-19 in Liver Transplant Recipients: a Preliminary Report from Northwestern Italy. Transpl Infect Dis. 2020 doi: 10.1111/tid.13353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Pereira M.R., Aversa M.M., Farr M.A., Miko B.A., Aaron J.G., Mohan S. Tocilizumab for severe COVID-19 in solid organ transplant recipients: a matched cohort study. Am J Transplant. 2020;2:3198–3205. doi: 10.1111/ajt.16314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.M.J. Pérez-Sáez, M. Blasco, D. Redondo-Pachón, P. Ventura Aguilar, T. Bada-Bosch, I. Pérez-Flores, E. Melilli, L.A. Sánchez-Cámara, M.O. López-Oliva, C. Canal, A. Shabaka, N. Garra Moncau, P.L. Martín-Moreno, V. López, R. Hernández-Gallego, O. Siverio, C. Galeano, J. Espí Reig, C.J. Cabezas, M.T. Rodrigo, L. Llinàs-Mallol, M.J. Fernández-Reyes, L. Cruzado Vega, L. Pérez-Tamajón, R. Santana-Estupiñán, M.C. Ruiz-Fuentes, G. Tabernero, S. Zárraga, J. Carlos Ruiz, A. Gutiérrez-Dalmau, A. Mazuecos, E. Sánchez-Álvarez, M. Crespo, J. Pascual, f.T.S.S.o.N.C.-. Group, I. García-Méndez, L. Pérez-Oller, M. Giorgi, Use of tocilizumab in kidney transplant recipients with COVID-19, Am J Transplant, (n/a). [DOI] [PMC free article] [PubMed]
- 179.Pierrotti L.C., Reusing Junior J.O., Freire M.P., Barros Machado D.J., Megale Moreira R., Ventura C.G. COVID-19 among kidney transplant recipients requiring hospitalization: preliminary data and outcomes from a single-center in Brazil. Transpl Int. 2020 doi: 10.1111/tri.13745. [DOI] [PubMed] [Google Scholar]
- 180.Prieto M., Gastaca M., Ruiz P., Ventoso A., Palomares I., Rodriguez-Alvarez R.J. A case of COVID-19 immediately after liver transplantation: Not only bad news. Ann Hepatobiliary Pancreat Surg. 2020;24:314–318. doi: 10.14701/ahbps.2020.24.3.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.T.C.U.K.T. Program, Early Description of Coronavirus 2019 Disease in Kidney Transplant Recipients in New York, J Am Soc Nephrol, 31 (2020) 1150. [DOI] [PMC free article] [PubMed]
- 182.Qin J., Wang H., Qin X., Zhang P., Zhu L., Cai J. Perioperative Presentation of COVID-19 Disease in a Liver Transplant Recipient. Hepatology. 2020;27:27. doi: 10.1002/hep.31257. [DOI] [PubMed] [Google Scholar]
- 183.Rabiee A., Sadowski B., Adeniji N., Perumalswami P., Nguyen V., Moghe A. Liver Injury in Liver Transplant Recipients with Coronavirus Disease 2019 (COVID-19): US Multicenter Experience. Hepatology. 2020 doi: 10.1002/hep.31574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Raëth J., Tomio A., Eugene A., Mouffak A., Durand M., Hamidfar R. Immunosuppression in a lung transplant recipient with COVID-19? Lessons from an early case. Respiratory Medicine and Research. 2020;78:100782. doi: 10.1016/j.resmer.2020.100782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Rahman F., Liu S.T.H., Taimur S., Jacobs S., Sullivan T., Dunn D. Treatment with convalescent plasma in solid organ transplant recipients with COVID-19: Experience at large transplant center in New York City. Clin Transplant. 2020 doi: 10.1111/ctr.14089. [DOI] [PubMed] [Google Scholar]
- 186.Ramos K.J., Kapnadak S.G., Collins B.F., Pottinger P.S., Wall R., Mays J.A. Detection of SARS-CoV-2 by bronchoscopy after negative nasopharyngeal testing: Stay vigilant for COVID-19. Respir Med Case Rep. 2020;30:101120. doi: 10.1016/j.rmcr.2020.101120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Rasekhi A., Hoseinyazdi M., Esmaeilian S., Teimouri A., Safaei A., Rafiee F. COVID-19 pneumonia presenting as a single pulmonary nodule in a kidney transplant recipient: A case report and literature review. Radiology Case Reports. 2020;15:1587–1590. doi: 10.1016/j.radcr.2020.06.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Renaud-Picard B., Gallais F., Ohana M., Zeyons F., Kretz B., Andre J. Bilateral Acute Cardioembolic Limb Ischemia After Coronavirus Disease 2019 Pneumonia in a Lung Transplant Recipient: A Case Report. Transplant Proc. 2020;52:2715–2718. doi: 10.1016/j.transproceed.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.M. Rinaldi, M. Bartoletti, L. Bussini, L. Pancaldi, R. Pascale, G. Comai, M. Morelli, M. Ravaioli, M. Cescon, F. Cristini, P. Viale, M. Giannella, COVID-19 in solid organ transplant recipients: No difference in survival compared to general population, Transpl Infect Dis, (n/a e13421). [DOI] [PMC free article] [PubMed]
- 190.Rivinius R., Kaya Z., Schramm R., Boeken U., Provaznik Z., Heim C. COVID-19 among heart transplant recipients in Germany: a multicenter survey. Clin Res Cardiol. 2020 doi: 10.1007/s00392-020-01722-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.M.B. Roberts, S. Izzy, Z. Tahir, A. Al Jarrah, J.A. Fishman, J. El Khoury, COVID-19 in solid organ transplant recipients: dynamics of disease progression and inflammatory markers in ICU and non-ICU admitted patients, Transpl Infect Dis, (n/a e13407). [DOI] [PMC free article] [PubMed]
- 192.Rodriguez-Cubillo B., Moreno de la Higuera M.A., Lucena R., Valdes Franci E., Hurtado M., Calvo Romero N. Should cyclosporine be useful in renal transplant recipients affected by SARS-CoV-2? Am J Transplant. 2020 doi: 10.1111/ajt.16141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Russell M.R., Halnon N.J., Alejos J.C., Salem M.M., Reardon L.C. COVID-19 in a pediatric heart transplant recipient: Emergence of donor-specific antibodies. J Heart Lung Transplant. 2020;29:29. doi: 10.1016/j.healun.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.P. Sakulkonkij, J. Bruminhent, C. Pankongngam, N. Chalermphunchai, A family cluster of diagnosed coronavirus disease 2019 (COVID-19) kidney transplant recipient in Thailand, Immunity, Inflammation and Disease, (n/a). [DOI] [PMC free article] [PubMed]
- 195.Sánchez Cadena A.D., Negreira Caamaño M., Pérez Serrano R., Porras Leal M.L. Inmunoglobulinas por vía intravenosa: una alternativa terapéutica a tener en cuenta en el paciente trasplantado renal con COVID-19. Nefrología. 2020 doi: 10.1016/j.nefro.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.E. Seminari, M. Colaneri, M. Sambo, I. Gallazzi, A. Di Matteo, S. Roda, R. Bruno, C.I.S.M.P.T.F. the, SARS Cov-2 infection in a renal-transplanted patient: A case report, Am J Transplant, (n/a). [DOI] [PMC free article] [PubMed]
- 197.Serrano O.K., Kutzler H.L., Rochon C., Radojevic J.A., Lawlor M.T., Hammond J.A. Incidental COVID-19 in a Heart-Kidney Transplant Recipient with Malnutrition and Recurrent Infections: Implications for the SARS-CoV-2 Immune Response. Transpl Infect Dis. 2020 doi: 10.1111/tid.13367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Shingare A., Bahadur M.M., Raina S. COVID-19 in recent kidney transplant recipients. Am J Transplant. 2020;08:08. doi: 10.1111/ajt.16120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Singhvi A., Barghash M., Lala A., Mitter S.S., Parikh A., Oliveros E. Challenges in Heart Transplantation during COVID-19: A Single Center Experience. J Heart Lung Transplant. 2020;39:894–903. doi: 10.1016/j.healun.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Song S.H., Chen T.L., Deng L.P., Zhang Y.X., Mo P.Z., Gao S.C. Clinical characteristics of four cancer patients with SARS-CoV-2 infection in Wuhan, China. Infect Dis Poverty. 2020;9:82. doi: 10.1186/s40249-020-00707-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Soquet J., Rousse N., Moussa M., Goeminne C., Deblauwe D., Vuotto F. Heart Retransplantation Following COVID-19 Illness in a Heart Transplant Recipient. J Heart Lung Transplant. 2020;39:983–985. doi: 10.1016/j.healun.2020.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Sperry B.W., Khumri T.M., Kao A.C. Donor-derived cell-free DNA in a heart transplant patient with COVID-19. Clin Transplant. 2020:e14070. doi: 10.1111/ctr.14070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Stachel M.W., Gidea C.G., Reyentovich A., Mehta S.A., Moazami N. COVID-19 pneumonia in a dual heart-kidney recipient. J Heart Lung Transplant. 2020;39:612–614. doi: 10.1016/j.healun.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Suwanwongse K., Shabarek N. Fatal Outcome in a Kidney-Pancreas Transplant Recipient With COVID-19. Cureus. 2020;12 doi: 10.7759/cureus.8691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Taha M., Sharma A., Taha M., Samavati L. Coronavirus Disease 2019 in Immunocompromised Organ Transplant Recipients: A Case Report and Review of the Literature. Transplant Proc. 2020;52:2698–2702. doi: 10.1016/j.transproceed.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.E. Tatar, M. Karatas, I. Bozaci, A. Ari, T. Acar, C. Simsek, A.M. Yildirim, O. Yildirim, A. Uslu, Intravenous Immunoglobulin and Favipiravir treatment for A Kidney Transplant Patient with Severe Covid-19 Pneumonia, Transfus Apher Sci [DOI] [PMC free article] [PubMed]
- 207.D.R.B. Terrabuio, L. Haddad, L. Ducatti, L. Nunes Gouveia, V. Rocha-Santos, R.M.T. Ferreira, G.F. Darce, A.J.A. Cardoso, F.J. Carrilho, W. Andraus, E. Abdala, L.A.C. D´Albuquerque, Insights in the approach of long-term liver transplant recipients with COVID-19, Transpl Infect Dis, (n/a e13424). [DOI] [PMC free article] [PubMed]
- 208.T. Thammathiwat, S. Tungsanga, K. Tiankanon, P. Torvorapanit, W. Chumpangern, S. Udomkarnjananun, Y. Avihingsanon, T. Sriprasart, N. Srisawat, K. Jutivorakool, L. Paitoonpong, O. Putcharoen, N. Townamchai, A case of successful treatment of severe COVID-19 pneumonia with favipiravir and tocilizumab in post–kidney transplant recipient, Transpl Infect Dis, (n/a e13388). [DOI] [PMC free article] [PubMed]
- 209.Tian S., Xiong Y., Liu H., Niu L., Guo J., Liao M. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol. 2020;33:1007–1014. doi: 10.1038/s41379-020-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Trujillo H., Caravaca-Fontan F., Sevillano A., Gutierrez E., Caro J., Gutierrez E. SARS-CoV-2 Infection in Hospitalized Patients with Kidney Disease. KI Reports. 2020;01:01. doi: 10.1016/j.ekir.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Trujillo H., Caravaca-Fontan F., Sevillano A., Gutierrez E., Fernandez-Ruiz M., Lopez-Medrano F. Tocilizumab use in Kidney Transplant Patients with COVID-19. Clin Transplant. 2020 doi: 10.1111/ctr.14072. [DOI] [PubMed] [Google Scholar]
- 212.J. Tschopp, A.G. L'Huillier, M. Mombelli, N.J. Mueller, N. Khanna, C. Garzoni, D. Meloni, M. Papadimitriou-Olivgeris, D. Neofytos, H.H. Hirsch, M.M. Schuurmans, T. Müller, T. Berney, J. Steiger, M. Pascual, O. Manuel, C. van Delden, S. Swiss Transplant Cohort, First experience of SARS-CoV-2 infections in solid organ transplant recipients in the Swiss Transplant Cohort Study, Am J Transplant, (n/a). [DOI] [PMC free article] [PubMed]
- 213.Vaidya G., Czer L.S.C., Kobashigawa J., Kittleson M., Patel J., Chang D. Successful Treatment of Severe COVID-19 Pneumonia With Clazakizumab in a Heart Transplant Recipient: A Case Report. Transplant Proc. 2020;52:2711–2714. doi: 10.1016/j.transproceed.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Vechorko V., Gordeev I., Gubareva E., Ryndyaeva E., Averkov O. COVID-19 infection after recent heart transplantation: a case report. Russian Journal of Cardiology. 2020;25:3904. [Google Scholar]
- 215.A. Velioglu, S. Tuglular, Care of Asymptomatic SARS-CoV-2 positive Kidney Transplant Recipients, Transpl Int, (n/a). [DOI] [PMC free article] [PubMed]
- 216.G.M. Verleden, L. Godinas, N. Lorent, P. Van Bleyenbergh, L. Dupont, M. Delcroix, J. Yserbyt, C. Dooms, R. Vos, COVID-19 in lung transplant patients: a case series, Am J Transplant, (n/a). [DOI] [PMC free article] [PubMed]
- 217.Verma A., Khorsandi S.E., Dolcet A., Prachalias A., Suddle A., Heaton N. Low prevalence and disease severity of COVID-19 in post liver transplant recipients - a single centre experience. Liver Int. 2020;29:29. doi: 10.1111/liv.14552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Vilaro J., Al-Ani M., Manjarres D.G., Lascano J.E., Cherabuddi K., Elgendy A.Y. Severe COVID-19 After Recent Heart Transplantation Complicated by Allograft Dysfunction. JACC. 2020;2:1347–1350. doi: 10.1016/j.jaccas.2020.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.D.R. Waisberg, E. Abdala, L.S. Nacif, L.B. Haddad, L. Ducatti, V. Rocha-Santos, L.N. Gouveia, C.S. Lazari, R.B. Martino, R.S. Pinheiro, R.M. Arantes, D.R. Terrabuio, L.M. Malbouisson, F.H. Galvao, W. Andraus, L.A. Carneiro-D´Albuquerque, Liver Transplant Recipients Infected with SARS-CoV-2 in the Early Postoperative Period: Lessons from a Single Center in the Epicenter of the Pandemic, Transpl Infect Dis, (n/a e13418). [DOI] [PMC free article] [PubMed]
- 220.A.X. Wang, O. Quintero Cardona, D.Y. Ho, S. Busque, C.R. Lenihan, Influence of immunosuppression on seroconversion against SARS-CoV-2 in two kidney transplant recipients, Transpl Infect Dis, (n/a e13423). [DOI] [PMC free article] [PubMed]
- 221.Wang J., Li X., Cao G., Wu X., Wang Z., Yan T. COVID-19 in a Kidney Transplant Patient. Eur Urol. 2020;77:769–770. doi: 10.1016/j.eururo.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Webb G.J., Marjot T., Cook J.A., Aloman C., Armstrong M.J., Brenner E.J. Outcomes following SARS-CoV-2 infection in liver transplant recipients: an international registry study. Lancet Gastroenterol Hepatol. 2020;5:1008–1016. doi: 10.1016/S2468-1253(20)30271-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Webb G.J., Moon A.M., Barnes E., Barritt A.S., Marjot T. Determining risk factors for mortality in liver transplant patients with COVID-19. Lancet Gastroenterol Hepatol. 2020;5:643–644. doi: 10.1016/S2468-1253(20)30125-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.T.H. Westhoff, F.S. Seibert, F. Bauer, U. Stervbo, M. Anft, A.A.N. Doevelaar, B.J. Rohn, G. Winnekendonk, U. Dittmer, P. Schenker, E. Vonbrunn, K. Amann, R. Viebahn, N. Babel, Allograft infiltration and meningoencephalitis by SARS-CoV-2 in a pancreas-kidney transplant recipient, Am J Transplant, (n/a). [DOI] [PMC free article] [PubMed]
- 225.Xia Z., Liu X., Hu X., Zhong Z., Wang Y., Peng G. Failed antibody response in a renal transplant recipient with SARS-CoV-2 infected. Transpl Infect Dis. 2020 doi: 10.1111/tid.13349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.J.J. Xu, D. Samaha, S. Mondhe, D. Massicotte-Azarniouch, G. Knoll, M. Ruzicka, Renal Infarct in a COVID-19 Positive Kidney-Pancreas Transplant Recipient, Am J Transplant, (n/a). [DOI] [PMC free article] [PubMed]
- 227.Yamada M., Rastogi P., Ince D., Thayyil A., Adela Mansilla M., Smith R.J.H. Minimal Change Disease With Nephrotic Syndrome Associated With Coronavirus Disease 2019 After Apolipoprotein L1 Risk Variant Kidney Transplant: A Case Report. Transplant Proc. 2020;52:2693–2697. doi: 10.1016/j.transproceed.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.S.G. Yi, A.W. Rogers, A. Saharia, M. Aoun, R. Faour, M. Abdelrahim, R.J. Knight, K. Grimes, S. Bullock, M. Hobeika, R. McMillan, C. Mobley, M. Moaddab, H.J. Huang, A. Bhimaraj, R.M. Ghobrial, A.O. Gaber, Early Experience With COVID-19 and Solid Organ Transplantation at a US High-volume Transplant Center, Transplantation, Online First (9000). [DOI] [PMC free article] [PubMed]
- 229.Zhang H., Chen Y., Yuan Q., Xia Q.X., Zeng X.P., Peng J.T. Identification of Kidney Transplant Recipients with Coronavirus Disease 2019. Eur Urol. 2020;77:742–747. doi: 10.1016/j.eururo.2020.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Zhong Z., Zhang Q., Xia H., Wang A., Liang W., Zhou W. Clinical characteristics and immunosuppressant management of coronavirus disease 2019 in solid organ transplant recipients. Am J Transplant. 2020;13:13. doi: 10.1111/ajt.15928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Zhu L., Gong N., Liu B., Lu X., Chen D., Chen S. Coronavirus Disease 2019 Pneumonia in Immunosuppressed Renal Transplant Recipients: A Summary of 10 Confirmed Cases in Wuhan, China. Eur Urol. 2020;77:748–754. doi: 10.1016/j.eururo.2020.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.L. Zhu, H. Shu, H. Li, T. Qiu, J. Zhou, G. Chen, Slow Recovery from Critical Coronavirus Disease 2019 Pneumonia in an Immunosuppressed Renal Transplant Recipient with Early Acute Cardiorenal Syndrome, Cardiorenal Med, (2020) 1-6. [DOI] [PMC free article] [PubMed]
- 233.Chen D., Yang B., Zhang Y., Chen L., Wei L., Zhang W. Withdrawing mycophenolate mofetil in treating a young kidney transplant recipient with COVID-19: A case report. Medicine (Baltimore) 2020;99 doi: 10.1097/MD.0000000000020481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.K.T. Mahendraraj, Tsuyoshi; Nissen, Nicholas; Kosari, Kambiz; Brennan, Todd; Voidonikolas, Georgios; Klein, Andrew; Kim, Irene, First report of novel coronavirus infection following abdominal organ transplantation in North America during the COVID-19 pandemic, Transplantation, 104 (2020) S321.
- 235.Li J., Chen G., Zhang M., Tu S., Chen C. Different clinical presentations of two renal transplant recipients with coronavirus disease 2019: a case report. BMC Infect Dis. 2020;20:707. doi: 10.1186/s12879-020-05434-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.M. Ahluwalia, M.M. Givertz, M.R. Mehra, A Proposed Strategy for Management of Immunosuppression in Heart Transplant Patients with COVID-19, Clin Transplant, (n/a e14032). [DOI] [PMC free article] [PubMed]
- 237.Binda B., Picchi G., Carucci A.C., Sinatti G., Di Norcia M., Grimaldi A. Follow-up and Management of Kidney Transplant Recipients During the COVID-19 Lockdown: The Experience of an Italian Transplant Center, Including Two Cases of COVID-19 Pneumonia. Transplant Proc. 2020;52:2614–2619. doi: 10.1016/j.transproceed.2020.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.M. Ghaffari Rahbar, M. Nafar, A. Khoshdel, N. Dalili, A. Abrishami, A. Firouzan, F. Poorrezagholi, F. Samadian, S. Ziaie, S. Fatemizadeh, S. Samavat, Low Rate of COVID-19 pneumonia in Kidney Transplant Recipients - A Battle Between Infection and Immune Response?, Transpl Infect Dis, (n/a e13406). [DOI] [PMC free article] [PubMed]
- 239.F. Silva, A. Cipriano, H. Cruz, J. Tavares, J. Fragoso, J. Malheiro, M. Almeida, L.S. Martins, M. Abreu, S. Pedroso, L. Dias, A.C. Henriques, SARS-CoV-2 infection in kidney transplant recipients: Early report of five cases, Transpl Infect Dis, (n/a e13394). [DOI] [PMC free article] [PubMed]
- 240.Caillard S., Anglicheau D., Matignon M., Durrbach A., Greze C., Frimat L. An initial report from the French SOT COVID Registry suggests high mortality due to Covid-19 in recipients of kidney transplants. Kidney Int. 2020 doi: 10.1016/j.kint.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Ahmad S.H., Smith R., Camilleri B. Belatacept, kidney transplantation and COVID-19: Successful management of the first reported case within the United Kingdom. Clin Transplant. 2020 doi: 10.1111/ctr.14026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. C. China Medical Treatment Expert Group for, Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Desai A., Sachdeva S., Parekh T., Desai R. COVID-19 and Cancer: Lessons From a Pooled Meta-Analysis. JCO Glob Oncol. 2020;6:557–559. doi: 10.1200/GO.20.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Malard F., Genthon A., Brissot E., van de Wyngaert Z., Marjanovic Z., Ikhlef S. COVID-19 outcomes in patients with hematologic disease. Bone Marrow Transplant. 2020;50:2180–2184. doi: 10.1038/s41409-020-0931-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1
Supplementary material 2