Abstract
Background
Pain can be considered an early sign of COVID-19 infection. There are no studies that specifically investigate the frequency, characteristics, and presentation patterns of pain in COVID-19 infection.
Aims
Our aim is to evaluate the frequency, localization, and severity of pain among the presenting signs and symptoms in patients with COVID-19.
Methods
Patients with the diagnosis of COVID-19 who were admitted to our hospital between March and June 2020 were retrospectively analyzed. Patients’ general symptoms at the first admission to the hospital, presence of pain at admission, localization, severity, and persistence of pain were queried by phone call.
Results
A total of 210 inpatients diagnosed with COVID-19 were recruited from the hospitals database. Complaints of the patients were 76.6% fatigue, 69.3% pain, 62% fever, 45.3% cough, 43.5% loss of taste and/or smell, 25% diarrhea, and 0.5% skin lesions respectively. Pain was the chief complaint in of 46.61% of the patients. Pain complaints had started on average 2.2 (± 2.8) days before admission. Among 133 patients reporting pain, the distribution of site was 92 (69.2%) myalgia/arthralgia; 67 (50.4%) headache; 58 (43.6%) back pain; 44 (33.1%) low back pain; 33 (25.0%) chest pain; 28 (21.1%) sore throat; and 18 (13.6%) abdominal pain.
Conclusions
The most common pain symptoms were myalgia/arthralgia and headache (69.17% and 50.37%) and found to be much higher than previously reported. Pain is one of the most common complaints of admission to the hospital in patients with COVID-19. Patients who apply to health institutions with pain complaints should be evaluated and questioned in suspicion of COVID-19 infection.
Keywords: Arthralgia, COVID-19, Headache, Myalgia, Pain
Introduction
Pain is one of the most important and most common reasons for admission to emergency department [1]. Pain is also one of the commonest initial symptoms of COVID-19 infection pandemia worldwide since 2019 and having a broad clinical spectrum from asymptomatic or mild forms to clinical conditions that may lead to multi-organ failures. While myalgia and headache are the most common pain symptoms in COVID-19, less frequent presentations include sore throat, abdominal pain, and chest pain [2]. Studies have shown that among COVID-19 patients, myalgia is the most common musculoskeletal symptom observed with a prevalence ranging from 30 to 36% [3–6]. The number of COVID-19 positive patients presenting with pain, while without any initial respiratory tract symptoms, was remarkable. Therefore, pain can be considered an early sign of COVID-19 infection [7]. The aim of this study was to evaluate the frequency, localization, and severity of pain among the presenting signs and symptoms in patients with COVID-19.
Materials and methods
We retrospectively analyzed consecutive selected patients with the diagnosis of COVID-19 who were admitted to our hospital and whose treatment was completed in outpatient or inpatient clinic between March 2020 and June 2020. All patients were diagnosed with COVID-19 according to the polymerase chain reaction (PCR) testing. Inclusion criteria were being COVID-19 positive patient and discharged from hospital. Exclusion criteria were being under 18 years old, pregnancy, and those who died in the time of questionary. Age, gender, height, weight, additional diseases, medication, presence of chronic pain, and smoking of the patients were recorded. Patients’ general symptoms at the first admission to the hospital, presence of pain at admission, localization, severity, and persistence of pain were queried by phone call with the consent of the patient. Pain intensity was evaluated by using the visual analog scale (VAS). The study protocol was approved by the Ethics Committee of Istanbul Medeniyet University (2020/00399).
Statistical analysis
IBM SPSS v22.0 program was used for statistical data analysis. Descriptive statistics are presented with mean ± standard deviation (minimum-maximum) values for continuous variables. The frequency values (number of cases) for categorical variables are shown together with their percentages. Kolmogorov-Smirnov and Shapiro-Wilk tests were used to examine the normal distribution. The level of correlation between variables was determined using Spearman rho correlation coefficients since the data were not normally distributed. The effect size of the relationship is the correlation coefficient according to Cohen’s classification: between 0.10 and 0.29 is defined as small; between 0.30 and 0.49 as medium; and 0.50 to 1.0 as large correlation [8]. The results were evaluated bilaterally at 95% confidence interval, significance level at p < 0.05 and p < 0.01.
Results
A total of 210 inpatients diagnosed with COVID-19 and discharged after treatment were recruited from the hospitals database. Of these 17 (8.1%) had died after the first discharge from the hospital. The remaining 193 patients diagnosed with COVID-19, according to the PCR test results between March and June 2020, were questionaried by phone call included into the analysis. Of the patients, 48.7% were male and 51.3% were female. The mean age was 48.5 (19.0) years, the mean weight was 78.3 (16.0) kilogram, and the mean time since the disease onset to questionary time was 81.4 (20.4) day. Of the patients, 5.7% were smokers, 36.5% had comorbidity, and 48.7% had pulmonary involvement of COVID-19.
Complaints of the patients were 76.6% fatigue, 69.3% pain, 62% fever, 45.3% cough, 43.5% loss of taste and smell, 25% diarrhea, and 0.5% skin lesions respectively (Table 1).
Table 1.
Clinical characteristics of patients with COVID-19 infection
| Symptom | Fatigue | Pain | Fever | Cough | Loss of taste-smell | Diarrhea | Skin lesion |
| n | 147 | 133 | 119 | 87 | 83 | 48 | 1 |
| (%) | (76.6) | (69.3) | (62.0) | (45.3) | (43.5) | (25.0) | (0.5) |
Pain was the chief complaint in 46.61% of the patients, while 92.58% of patients with pain had no previous pain complaints. The 46.61% of the patients with pain were men, and 53.39% were women, 5.6% were smoking, 36.09% had comorbidities, and 49.61% had COVID-19-related pulmonary involvement.
Pain complaints had started on average 2.2 (2.8) days before admission to the hospital. 63.2% of the patients with pain had widespread pain, and 36.8% had local pain. Also, 58.3% of the patients with widespread pain were female, but majority of patients with local pain were male (55.0%).
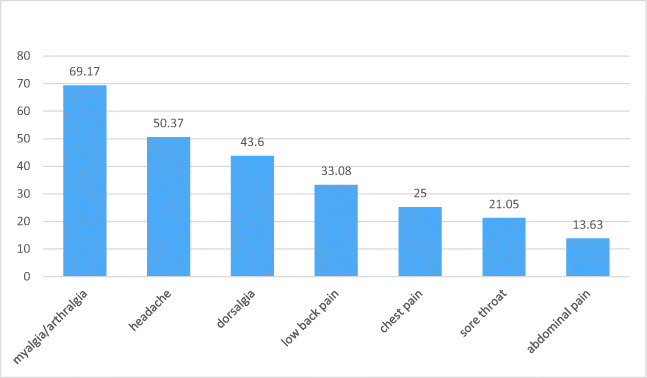
Among 133 patients reporting pain in presentation or during the illness, the distribution of site was 92 (69.2%) myalgia/arthralgia; 67 (50.4%) headache; 58 (43.6%) back pain; 44 (33.1%) low back pain; 33 (25.0%) chest pain; 28 (21.1%) sore throat; and 18 (13.6%) abdominal pain (Fig. 1).
Fig. 1.
Distribution of pain localization (%)
Among patients with pain complaints, the mean value of VAS score was 4.8 (3.7). Of the patients, 96.2% with pain symptom during acute period did not report any pain at the time of the questionnaire.
According to the correlation analysis, a statistically significant relationship was found between presence of pain at presentation and female gender, fatigue, loss of taste and smell, pain intensity, and generalized pain. A statistically significant correlation was found between back pain with abdominal pain and female gender, and between headache and age. A statistically significant relationship was found between the number of days between the onset of pain and the admission and the severity of pain, widespread pain, ongoing pain, and pulmonary involvement. There was also a significant relationship between ongoing pain and pain intensity. Statistically significant correlation analysis results are shown in Table 2 and Table 3.
Table 2.
Results of Spearman correlation analysis among pain-related variables
| Pain (+) | Pain as primary symptom | Time onset of pain | Ongoing pain | Widespread pain | VAS | ||
|---|---|---|---|---|---|---|---|
| Pain (+) | rho | 1 | .460** | .801** | .110 | .587** | .816** |
| P | .000 | .000 | .131 | .000 | .000 | ||
| Pain as primary symptom | rho | .460** | 1 | .528** | .166* | .356** | .556** |
| P | .000 | .000 | .021 | .000 | .000 | ||
| Time onset of pain | rho | .801** | .528** | 1 | .163* | .488** | .741* |
| P | .000 | .000 | .029 | .000 | .000 | ||
| Ongoing pain | rho | .110 | .166* | .163* | 1 | .055 | .190** |
| P | .131 | .021 | .029 | .452 | .009 | ||
| Widespread pain | rho | .587** | .356** | .488** | .055 | 1 | .531** |
| P | .000 | .000 | .000 | .452 | .000 | ||
| VAS | rho | .816** | .556** | .741* | .190** | .531** | 1 |
| P | .000 | .000 | .000 | .009 | .000 | ||
*Significant at the 0.05 level. **Significant at the 0.01 level
Table 3.
Results of Spearman correlation analysis among pain-related variables and clinical characteristics
| Pain | Pain as primary symptom | Time onset of pain | Headache | Dorsalgia | Abdominal pain | ||
|---|---|---|---|---|---|---|---|
| Age | rho | − .127 | −.076 | − .061 | − .212** | .052 | − .005 |
| P | .080 | .292 | .415 | .003 | .477 | .943 | |
| Gender | rho | .070 | .186** | .046 | .039 | .213** | .171* |
| P | .332 | .010 | .537 | .587 | .003 | .018 | |
| Fatigue | rho | .378** | .172* | .295** | .328** | .203** | .095 |
| P | .000 | .017 | .000 | .000 | .005 | .193 | |
| Loss of smell/taste | rho | .335** | .182* | .331** | .407** | .271** | .259** |
| P | .000 | .012 | .000 | .000 | .000 | .000 | |
*Significant at the 0.05 level. **Significant at the 0.01 level
Discussion
Recognizing the symptoms of COVID-19 infection is crucial for early detection of the disease, but symptoms of the disease are often not specific. Common symptoms include fever, cough, and myalgia/arthralgia or fatigue. Patients may initially present with diarrhea, nausea, or muscle pain a few days before the fever. Some patients may have headaches or hemoptysis [2, 9] and even be relatively asymptomatic [10].
In a meta-analysis, myalgia is the most common musculoskeletal symptom seen in the prevalence of 30–36% and headache is the most common neurologic symptom in the prevalence of 58.33% among COVID-19 patients [3–6, 11–13]. In patients presenting with widespread body pain, COVID-19 tests were found to be positive without known respiratory symptoms of viral disease. Therefore, pain can be considered an early sign of COVID-19 infection.
The intensity of pain associated with COVID-19 in the literature is reported as mild to moderate, similar to other viral pain models [7]. In our study, the severity of pain was evaluated with VAS and mean VAS found to be moderate, in accordance with the literature.
In the study of Guan et al., while the most common pain presentation in COVID-19 was myalgia/arthralgia (14.9%) and headaches (13.6%), while other complaints were sore throat, abdominal pain and chest pain [2]. There are also studies in the literature with higher rate of myalgia arthralgia up to 59% [14–16].
In our study, the most common pain symptoms were myalgia/arthralgia and headache (69.17% and 50.37%, respectively) and found to be much higher than previously reported.
Studies have shown that the frequency of chest pain varies between 0 and 34%, and this symptom may be a risk factor for critical COVID-19 pneumonia [17–19]. In our study, although the frequency of chest pain was as high as 25%, no relationship was found with lung infection. There was a significant relationship between fever, coughing, smoking, body weight, and pulmonary involvement.
Gastrointestinal symptoms such as anorexia, nausea, vomiting, diarrhea, and abdominal pain can be observed in some patients during infection. The frequency of abdominal pain accompanying the disease has been reported to be 2–8% [9, 17]. Although abdominal pain was the least common pain at presentation, this incidence was 13.63% in our study.
Pain is one of the most common complaints of admission to the hospital in patients with COVID-19, approximately half of the patients, and it starts approximately 2 days before the admission to the hospital. The results of this study show that patients who apply to health institutions with pain complaints should be evaluated and questioned in suspicion of COVID-19 infection.
In correlation analysis, significant relationship was found between time of pain onset and pain intensity. Generalized pain and intensity of pain were also significantly correlated with ongoing pain. Pain may be widespread and in some severe cases it could be the chief complaint. The earlier the pain begins, it can be more severe and widespread and become chronic. In addition, intensity of the pain and widespread pain are related to the presence of pain at presentation. The presence of pain at presentation and how early the pain begins can provide guidance on the character and prognosis of the pain.
Regarding the relationships between pain and other clinical characteristics, while local pain is more common in men, widespread pain is more common in women. Women present with pain more often, and loss of taste-smell and fatigue are more common in patients who present with pain.
Chronic pain and fatigue have been reported after SARS infection in the literature [20]. Whether the pain after COVID-19 infection becomes chronic or not is still unknown. The patients included in our study were patients who had COVID-19 infection, completed their outpatient treatment, or were discharged after completing inpatient treatment. Although the incidence of pain in the course of the disease was found to be very high in our study, the percentage of patients with persistent pain was 3.79%. Based on our results, we conclude that the pain complaint observed in the course of COVID-19 did not become chronic in this patient sample. Still, it is not possible to generalize this conclusion since the patients that died in the intensive care unit were not included in our study.
The main caveat of this study was omitting the fatal cases as inpatient and deaths after discharge. Also since the data was collected with questionary in a retrospective manner, the patients’ memory may lapse and mix due to different intellectual levels. Even though the severity of pain was assessed by VAS, the features of pain as continuity or intermittence were not sought.
COVID-19 infection should not be ignored in patients who apply with only pain complaint, and physicians should be careful in this regard.
More research is needed to evaluate how pain patterns change over time, particularly in various COVID-19 treatments, and the impact of disease severity and disease characteristics on pain patterns.
Compliance with ethical standards
The study protocol was approved by the Ethics Committee of Istanbul Medeniyet University Goztepe Training and Research Hospital (2020/00399). All participants provided informed consent.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sadiye Murat, Email: samurftr@gmail.com.
Bilinc Dogruoz Karatekin, Email: bilincdogruoz@hotmail.com.
Afitap Icagasioglu, Email: afitapi@gmail.com.
Celal Ulasoglu, Email: ulasoglu@gmail.com.
Sacit İçten, Email: sctctn@gmail.com.
Onur Incealtin, Email: onurincealtin@hotmail.com.
References
- 1.Kamberi F, Sinaj E, Ndreu V (2017) Pain the most common symptom in the emergency department: an observational study
- 2.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang X, Wei F, Hu L, et al. Epidemiology and clinical characteristics of COVID-19. Arch Iran Med. 2020;23(4):268–271. doi: 10.34172/aim.2020.09. [DOI] [PubMed] [Google Scholar]
- 4.Feng Y, Ling Y, Bai T, et al. COVID-19 with different severities: a multicenter study of clinical features. Am J Respir Crit Care Med. 2020;201(11):1380–1388. doi: 10.1164/rccm.202002-0445OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lian J, Jin X, Hao S, et al. Analysis of epidemiological and clinical features in older patients with coronavirus disease 2019 (COVID-19) outside Wuhan. Clin Infect Dis. 2020;71(15):740–747. doi: 10.1093/cid/ciaa242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goyal P, Choi JJ, Pinheiro LC, et al. Clinical characteristics of Covid-19 in New York City. N Engl J Med. 2020;382(24):2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Song XJ, Xiong DL, Wang ZY, et al. Pain management during the COVID-19 pandemic in China: lessons learned. Pain Med. 2020;21(7):1319–1323. doi: 10.1093/pm/pnaa143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen J Statistical power analysis for the behavioral sciences. Second edition edn,
- 9.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qian GQ, Yang NB, Ding F, et al. Epidemiologic and clinical characteristics of 91 hospitalized patients with COVID-19 in Zhejiang, China: a retrospective, multi-centre case series. QJM. 2020;113(7):474–481. doi: 10.1093/qjmed/hcaa089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang X, Fang J, Zhu Y, et al. Clinical characteristics of non-critically ill patients with novel coronavirus infection (COVID-19) in a Fangcang hospital. Clin Microbiol Infect. 2020;26(8):1063–1068. doi: 10.1016/j.cmi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abdullahi A, Candan SA, Abba MA, et al. Neurological and musculoskeletal features of COVID-19: a systematic review and meta-analysis. Front Neurol. 2020;11:687. doi: 10.3389/fneur.2020.00687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vetter P, Vu DL, L'Huillier AG, et al. Clinical features of covid-19. BMJ. 2020;369:m1470. doi: 10.1136/bmj.m1470. [DOI] [PubMed] [Google Scholar]
- 15.Escalera-Antezana JP, Lizon-Ferrufino NF, Maldonado-Alanoca A, et al. Clinical features of the first cases and a cluster of coronavirus disease 2019 (COVID-19) in Bolivia imported from Italy and Spain. Travel Med Infect Dis. 2020;35:101653. doi: 10.1016/j.tmaid.2020.101653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cipollaro L, Giordano L, Padulo J, et al. Musculoskeletal symptoms in SARS-CoV-2 (COVID-19) patients. J Orthop Surg Res. 2020;15(1):178. doi: 10.1186/s13018-020-01702-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li K, Wu J, Wu F, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Investig Radiol. 2020;55(6):327–331. doi: 10.1097/RLI.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu XW, Wu XX, Jiang XG, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606. doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moldofsky H, Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol. 2011;11:37. doi: 10.1186/1471-2377-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]