Abstract
Background
Thrombotic complications of COVID-19 infection have become increasingly apparent as the disease has infected a growing number of individuals. Although less common than upper respiratory symptoms, thrombotic complications are not infrequent and may result in severe and long-term sequelae. Common thrombotic complications include pulmonary embolism, cerebral infarction, or venous thromboembolism; less commonly seen are acute myocardial injury, renal artery thrombosis, and mesenteric ischemia. Several case reports and case series have described acute myocardial injury in patients with COVID-19 characterized by elevations in serum biomarkers.
Case report
Here, we report the first case to our knowledge of a patient with acute coronary syndrome confirmed on catheter angiography and cardiac MRI. This patient was found to additionally have a left ventricular thrombus and ultimately suffered an acute cerebral infarction. Recognition of thrombotic complications in the setting of COVID-19 infection is essential for initiating appropriate therapy.
Conclusions
In acute myocardial injury, given the different treatment strategies for myocarditis versus acute myocardial infarction secondary to coronary artery thrombus, imaging can play a key role in clinical decision making for patients.
Keywords: COVID-19, Acute coronary syndrome, Cardiac MRI, Thrombosis
1. Background
COVID-19 infection caused by the SARS-CoV-2 virus is widely known for its respiratory and constitutional symptoms, most commonly cough, fever, malaise, and myalgias.1 However, studies have shown that thrombosis can be a serious complication of COVID-19 infection,2 , 3 often manifesting as pulmonary embolism (PE),4 cerebral infarction,5 , 6 or venous thromboembolism (VTE).7 Less common manifestations include renal artery thrombosis,8 acute myocardial injury,9 and mesenteric ischemia.10 , 11 Although seen in fewer patients than upper respiratory symptoms, thrombotic complications often result in severe illness and devastating long term complications.
Despite extensive clinical evidence of thrombosis in COVID-19 infection, the precise cause is still an area of active investigation. Pathology studies of patients with COVID-19 have demonstrated diffuse microthrombi.12 In the lung and skin, these effects occur through complement mediated microvascular injury.13 SARS-CoV-2 is known to infect the ACE2 receptor which is present on endothelial cells and early research on the molecular pathogenesis of the disease described endotheliitis resulting in accumulation of inflammatory cells and microcirculatory dysfunction.14 Recent work suggests that patients with COVID-19 have significantly increased procoagulants which correlate with acute phase reactants, leading authors to postulate that the systemic inflammatory response is a major contributor to thrombogenesis.15 The molecular pathophysiology of thrombosis in patients infected with SARS-CoV-2 is likely a combination of these and other pathways with a final common pathway of clinically significant thrombosis.
An early study from Wuhan, China reported a 12% rate of myocardial injury in patients with COVID-19 infection based on biomarker elevation.16 Several case reports have reported myocarditis resulting from COVID-19 infection,17 , 18 and a case series from the greater New York area described 18 patients with myocardial injury resulting from STEMI.19 Here, we present a case of a right coronary artery thrombus resulting in acute myocardial infarction arising in the setting of COVID-19 infection confirmed on both catheter angiography and cardiac MRI. To our knowledge prior studies demonstrating acute coronary syndrome in the setting of COVID-19 infection have been confirmed with biomarkers and/or EKG, therefore we present the first case confirmed on multimodality imaging.
2. Case report
The patient was a 36-year-old male presenting to the emergency room with dyspnea, chest tightness, and cough. He was in his normal state of health until one day prior to presentation at which time he began to experience progressively worsening symptoms; use of an inhaler temporarily improved dyspnea. He had no wheezing and did report any diarrhea, malaise, or myalgia. His past medical history was significant for mild obesity and intermittent asthma with no exacerbations for two years prior to presentation. He reported no cardiac or neurologic history.
On physical examination, he was found to be febrile to 38.8, tachycardic to 117, and tachypnic to 26. His SpO2 was 95%. He was given DuoNebs (ipratropium bromide and albuterol sulfate) which improved his dyspnea and was discharged home. No COVID-19 test was administered at that time given the strong clinical suspicion for asthma exacerbation.
Approximately one month later, the patient presented to the emergency room complaining of a one-day history of paroxysmal 2–8/10 central chest pain radiating to the jaw accompanied by vomiting. He reported subjective fevers, cough, dyspnea, and pleuritic chest pain for several weeks prior which he attributed to “asthma attacks”. He had presented to the emergency department of an outside hospital and was prescribed an inhaler which he reported temporarily ameliorated his symptoms.
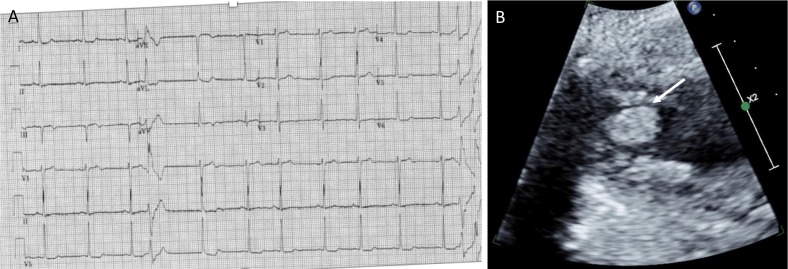
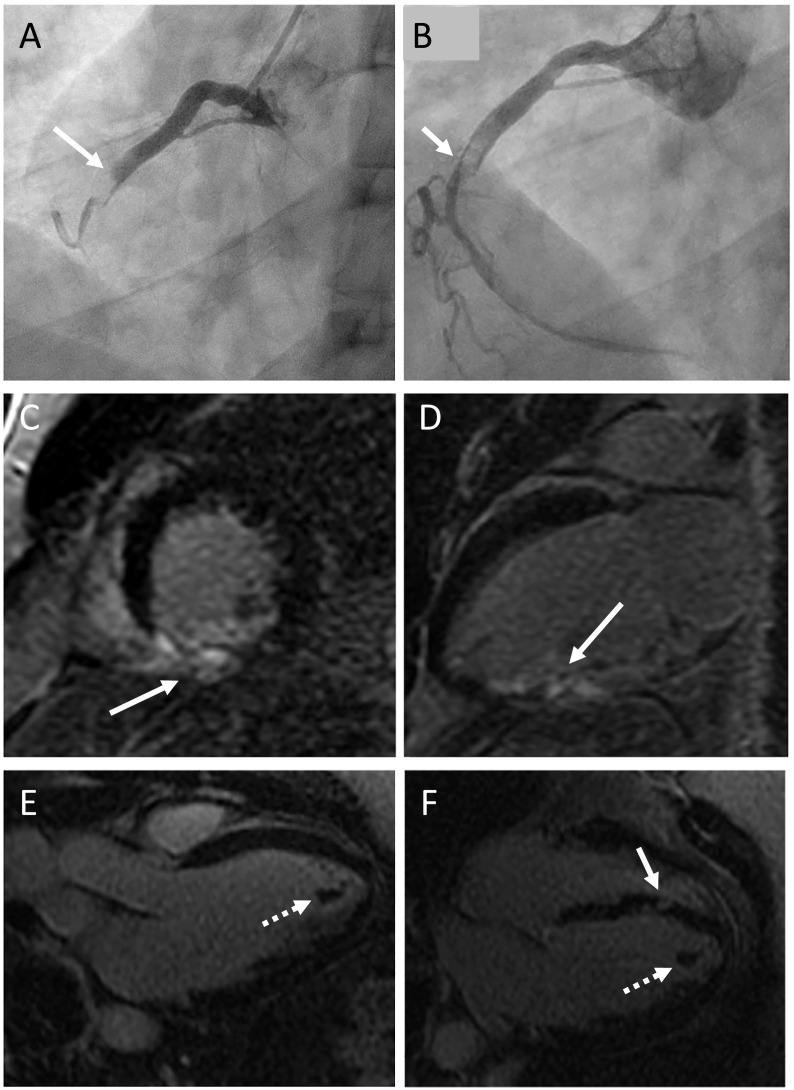
In the ED, vital signs were within normal limits and a COVID-19 test was drawn and ultimately was negative. An EKG demonstrated inferior T-wave inversion and nonspecific ST segment flattening and depressions (Fig. 1A). A bedside echo was performed which demonstrated a severely reduced ejection fraction, global hypokinesis with focal abnormalities, and a left ventricular thrombus (Fig. 1B). No troponin levels were drawn in the ED. The patient received aspirin and nitrates and was taken to the cardiac catheterization lab immediately, where he was found to have an occlusive right coronary artery thrombus (Fig. 2A) for which he underwent manual thrombectomy resulting in reconstitution of right coronary artery flow (Fig. 2B). He was subsequently treated with tirofiban and ticagrelor and was admitted to the CCU. One day after cardiac catheterization, he underwent cardiac MRI which demonstrated delayed hyperenhancement of the inferioseptal wall (Fig. 2C, D) with severe hypokinesis of the inferoseptal and inferior segments from base to apex with associated myocardial edema. Further, there was a left ventricular thrombus consistent the bedside echo (Fig. 2E, F). While in the CCU, the patient received repeat COVID-19 testing which was positive. D-dimer obtained the same day was 0.5 μg/mL FEU, within normal limits. Coagulation parameters were all within normal limits.
Fig. 1.
A is the EKG performed in the emergency room which demonstrated inferior T-wave inversion and nonspecific ST segment flattening and depressions. B is a representative image from cardiac echo which demonstrates a large hyperechoic focus compatible with left ventricular thrombus (white arrow).
Fig. 2.
A is a representative coronary angiography image demonstrating right coronary artery occlusion pre-thrombectomy (solid white arrow) with no flow distal to occlusive thrombus; B is a post-thrombectomy image of the right coronary artery demonstrating no thrombus and reconstitution of flow (solid white arrow). C and D are representative post-contrast cardiac MR images in the short axis and long axis planes, respectively; these images show delayed hyperenhancement of the inferioseptal wall compatible with infarct. E is a precontrast three chamber image demonstrating left ventricular thrombus (dotted white arrow); F is a post contrast four chamber view demonstrating thrombus (dotted white arrow); septal delayed hyperenhancement is also partially imaged (solid white arrow).
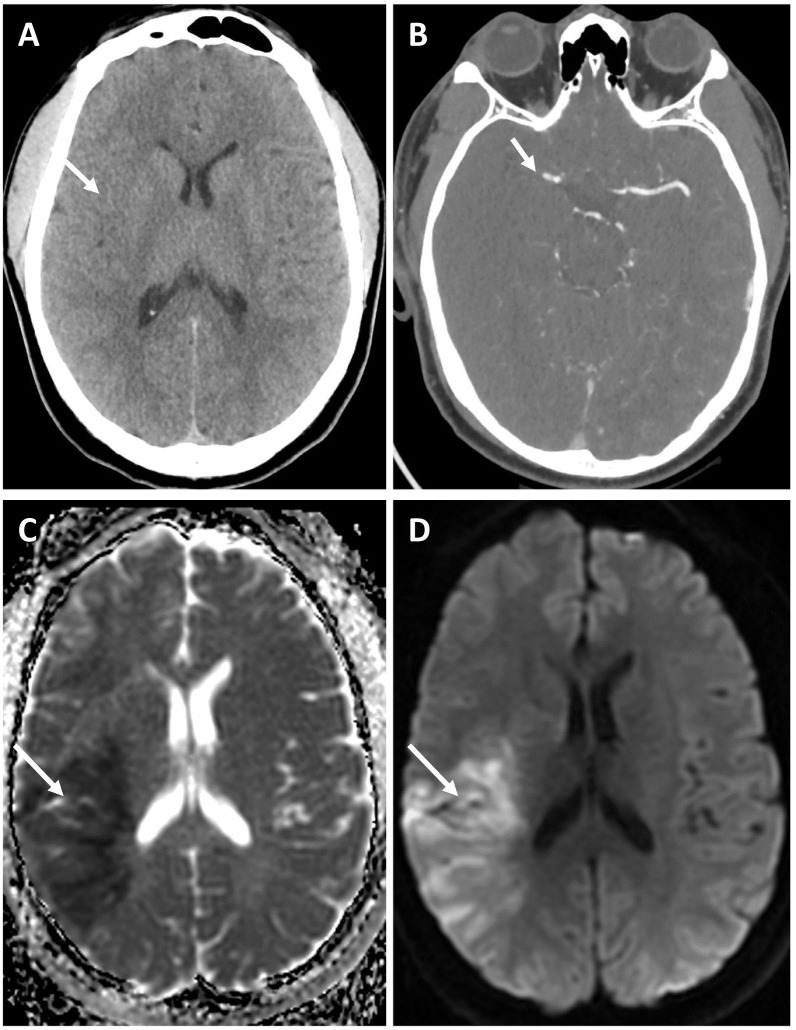
Five days post admission to the CCU, the patient was found down beside his hospital bed with left sided weakness on physical exam. A stroke code was initiated and head CT demonstrated subtle blurring of the gray-white differentiation within the right temporal lobe extending to the right insula (Fig. 3A). CTA performed immediately after showed a focal abrupt cutoff of the proximal right M1 segment just distal to its origin (Fig. 3B) with a paucity of distal inferior right MCA branch vessels. No additional occlusion or vascular abnormality was identified. The patient immediately underwent mechanical thrombectomy and was transferred to the neuro ICU.
Fig. 3.
A demonstrates subtle blurring of the gray-white differentiation within the right temporal lobe extending to the right insula; B shows CTA of the head demonstrating focal abrupt cutoff of the proximal right M1 and a paucity of distal inferior right MCA branch vessels. C and D are representative images from the brain MRI obtained the following day demonstrating restricted diffusion in the area of infarct on DWI and ADC sequences, respectively.
The following day, a brain MRI was performed to assess the extent of infarct. In keeping with the head CT, there was an extensive region of restricted diffusion within the right insula and inferior parietal lobe (Fig. 3C, D). Of note, repeat bedside echo demonstrated no left ventricular clot and improved left ventricular ejection fraction of 30–35%. The patient was started on anticoagulation four days after the procedure and several subsequent head CT scans showed expected evolution of the infarct with no hemorrhagic conversion or other abnormality. Ultimately the patient was transitioned to coumadin and discharged to acute rehab where he progressively improved with physical therapy.
3. Discussion
Thrombotic complications of COVID-19 infection are well established. Although there have been several reports of myocardial injury secondary to SARS-CoV-2 infection, this is the first report of coronary artery occlusion confirmed by catheter angiography and cardiac imaging. Hospital admissions for acute coronary syndromes were decreased by approximately 40% in one study during the COVID-19 pandemic, likely reflecting patient preferences to remain home when experiencing symptoms given the risk of transmission of virus in the healthcare setting.20 Other studies have confirmed this decline in ACS admissions,21 , 22 raising the concern that large numbers of patients may emerge from the pandemic with the sequelae of untreated acute coronary syndrome, such as heart failure.23
A relationship between COVID-19 infection and cardiovascular disease is well established. Studies have shown that patients infected with SARS-CoV-2 in the setting of preexisting cardiovascular disease have increased risk of severe disease and death.24 One study demonstrated an 8% risk of acute cardiac injury in patients with COVID-19, with a 13-fold higher incidence in critically ill patients.25 Notably, nearly all of these studies used biomarkers and/or EKG to diagnose acute myocardial injury. Radiology can play a key role in differentiating between these entities, as evidenced by the cardiac MR findings of this patient. Given the different treatment strategies for myocarditis versus coronary thrombosis, results of catheter angiography and cardiac imaging may serve as a critical branch point in the treatment of patients presenting with cardiac symptoms in the setting of COVID-19 infection.
The RCA infarct in our patient led to a cascade of events, starting with wall motion abnormalities which were visualized on both bedside echocardiogram and cardiac MR that predisposed to left ventricular clot formation. Absence of this clot on follow-up echo after ischemic infarct suggests that it may have embolized to the cerebral vasculature. Given the COVID-19-induced hypercoagulable state and immobilization in the CCU, an alternate possibility is that the cerebral infarct represented a separate thrombus. Indeed, many critically ill COVID-19 patients ultimately die of multi-organ failure which is thought to be at least in part attributable to multiple thrombotic complications.26
Long term complications of COVID-19 have become increasingly apparent.27 Persistent interstitial abnormalities and scarring of the lung parenchyma resulting in pulmonary fibrosis have emerged as an important and worrisome complication occurring in many patients.28 , 29 Reports of long-term neurological sequelae have also surfaced raising questions as to the extent of brain involvement in acute infection and whether complete resolution of symptoms can be expected.30 In addition to direct injury by the virus, thrombosis arising in the setting of acute COVID-19 may also result in long term effects. Our patient had no cardiovascular history prior to this episode. While his EF improved from approximately 15% to 35% by the end of his hospital admission, the infarction resulted in long-term suboptimal cardiac function. Similarly, this patient's large right MCA infarct resulted in long-term disability. Neurologic damage from COVID-19 is not uncommon, and may be the result of the virus itself or cerebral infarction.[31], [32], [33] Numerous long-lasting complications of prolonged critical care have been described,34 likely directly applicable to critically ill COVID-19 patients given prolonged length of stay in the ICU.35 , 36
Given the risk of thrombotic complication in patients with COVID-19, clinical guidelines have been issued recommending the use of anticoagulation in hospitalized COVID-19 patients with continuation for those with high risk.37 Clinically, a high level of suspicion should be raised for thrombosis in patients with SARS-CoV-2 infection and appropriate imaging ordered for confirmation so therapeutic anticoagulation can be initiated to prevent long term complications of thrombosis.
Our case demonstrates that in the setting of high community transmission of COVID-19, the specter should be raised that the infection is the cause of non-specific symptoms or symptoms that could be attributed to another etiology. This patient's initial presentation to the emergency room was attributed to his asthma, however likely represented early COVID-19 infection. Prolonged infection without monitoring allowed for the development of acute coronary syndrome ultimately resulting in heart failure, ventricular thrombosis, and cerebral infarction. Further, the patient may have exposed hundreds of people to COVID-19 during the time between emergency room presentations. Clinicians must be vigilant in the recognition of COVID-19 infection as well as its complications.
4. Conclusions
Here we present a rare case of acute coronary artery occlusion secondary to COVID-19 infection which subsequently resulted in left ventricular thrombus formation and acute ischemic cerebral infarct. To our knowledge, this is the first case where these findings are demonstrated on coronary angiography and cardiac MR. Given that COVID-19 causes myocarditis and acute coronary syndrome, imaging to identify the etiology of biochemical markers of myocardial injury may serve as a critical branch point in patient care decisions.
Funding
No funding was received for the completion of this project.
Declaration of competing interest
Mary M. Salvatore - Speaker and consultant: Genentech, Boehringer Ingelheim. Grant funding: Genentech, Boehringer Ingelheim. The remaining authors have no conflicts to disclose.
References
- 1.Chen N., Zhou M., Dong X. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helms J., Tacquard C., Severac F. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46(6):1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dolhnikoff M., Duarte-Neto A.N., de Almeida Monteiro R.A. Pathological evidence of pulmonary thrombotic phenomena in severe COVID-19. J Thromb Haemost. 2020;18(6):1517–1519. doi: 10.1111/jth.14844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reddy S.T., Garg T., Shah C. Cerebrovascular disease in patients with COVID-19: a review of the literature and case series. Case Rep Neurol. 2020;12(2):199–209. doi: 10.1159/000508958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaminetzky M., Moore W., Fansiwala K. Pulmonary embolism on CTPA in COVID-19 patients. Radiol Cardiothorac Imaging. 2020;2(4):e200308. doi: 10.1148/ryct.2020200308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Porfidia A., Valeriani E., Pola R., Porreca E., Rutjes A.W.S., Di Nisio M. Venous thromboembolism in patients with COVID-19: systematic review and meta-analysis. Thromb Res. 2020;196:67–74. doi: 10.1016/j.thromres.2020.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Su H., Yang M., Wan C. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;98(1):219–227. doi: 10.1016/j.kint.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zheng Y.-Y., Ma Y.-T., Zhang J.-Y., Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17(5):259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parry A.H., Wani A.H., Yaseen M. Acute mesenteric ischemia in severe coronavirus-19 (COVID-19): possible mechanisms and diagnostic pathway. Acad Radiol. 2020;27(8):1190. doi: 10.1016/j.acra.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Norsa L., Valle C., Morotti D., Bonaffini P.A., Indriolo A., Sonzogni A. Intestinal ischemia in the COVID-19 era. Dig Liver Dis. 2020;52(10):1090–1091. doi: 10.1016/j.dld.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Michele S., Sun Y., Yilmaz M.M. Forty postmortem examinations in COVID-19 patients. Am J Clin Pathol. 2020;154(6):748–760. doi: 10.1093/ajcp/aqaa156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Magro C., Mulvey J.J., Berlin D. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Varga Z., Flammer A.J., Steiger P. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Masi P., Hékimian G., Lejeune M. Systemic inflammatory response syndrome is a major contributor to COVID-19–associated coagulopathy. Circulation. 2020;142(6):611–614. doi: 10.1161/CIRCULATIONAHA.120.048925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Juusela A., Nazir M., Gimovsky M. Two cases of coronavirus 2019–related cardiomyopathy in pregnancy. Am J Obstet Gynecol MFM. 2020;2(2, Supplement):100113. doi: 10.1016/j.ajogmf.2020.100113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim I.-C., Kim J.Y., Kim H.A., Han S. COVID-19-related myocarditis in a 21-year-old female patient. Eur Heart J. 2020;41(19):1859. doi: 10.1093/eurheartj/ehaa288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bangalore S., Sharma A., Slotwiner A. ST-segment elevation in patients with Covid-19 - a case series. N Engl J Med. 2020;382(25):2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mafham M.M., Spata E., Goldacre R. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396(10248):381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Braiteh N., Rehman W.U., Alom M. Decrease in acute coronary syndrome presentations during the COVID-19 pandemic in upstate New York. Am Heart J. 2020;226:147–151. doi: 10.1016/j.ahj.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Papafaklis M.I., Katsouras C.S., Tsigkas G. “Missing” acute coronary syndrome hospitalizations during the COVID-19 era in Greece: medical care avoidance combined with a true reduction in incidence? Clin Cardiol. 2020;43:1142–1149. doi: 10.1002/clc.23424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kapoor A., Yadav R. Will the hidden specter of acute coronary syndrome (ACS) and ST-segment elevation myocardial infarction (STEMI) emerge from the avalanche of COVID-19? Indian Heart J. 2020;72(3):192–193. doi: 10.1016/j.ihj.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Driggin E., Madhavan M.V., Bikdeli B. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75(18):2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li B., Yang J., Zhao F. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–538. doi: 10.1007/s00392-020-01626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang T., Du Z., Zhu F. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet. 2020;395(10228):e52. doi: 10.1016/S0140-6736(20)30558-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carda S., Invernizzi M., Bavikatte G. COVID-19 pandemic. What should PRM specialists do? A clinician’s perspective. Eur J Phys Rehabil Med. 2020;56(4):515–524. doi: 10.23736/S1973-9087.20.06317-0. [DOI] [PubMed] [Google Scholar]
- 28.Bernheim A., Mei X., Huang M. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295(3) doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ding X., Xu J., Zhou J., Long Q. Chest CT findings of COVID-19 pneumonia by duration of symptoms. Eur J Radiol. 2020;127 doi: 10.1016/j.ejrad.2020.109009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Troyer E.A., Kohn J.N., Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020;87:34–39. doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Belani P., Schefflein J., Kihira S. COVID-19 is an independent risk factor for acute ischemic stroke. Am J Neuroradiol. 2020;41(8):1361–1364. doi: 10.3174/ajnr.A6650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gulko E., Oleksk M.L., Gomes W. MRI brain findings in 126 patients with COVID-19: initial observations from a descriptive literature review. Am J Neuroradiol. 2020 doi: 10.3174/ajnr.A6805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li Z., Liu T., Yang N. Neurological manifestations of patients with COVID-19: potential routes of SARS-CoV-2 neuroinvasion from the periphery to the brain. Front Med. 2020:1–9. doi: 10.1007/s11684-020-0786-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Desai S.V., Law T.J., Needham D.M. Long-term complications of critical care. Crit Care Med. 2011;39(2):371–379. doi: 10.1097/CCM.0b013e3181fd66e5. [DOI] [PubMed] [Google Scholar]
- 35.Rees E.M., Nightingale E.S., Jafari Y. COVID-19 length of hospital stay: a systematic review and data synthesis. BMC Med. 2020;18(1):270. doi: 10.1186/s12916-020-01726-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thai P.Q., Toan D.T.T., Son D.T. Factors associated with the duration of hospitalisation among COVID-19 patients in Vietnam: a survival analysis. Epidemiol Infect. 2020;e114:148. doi: 10.1017/S0950268820001259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barnes G.D., Burnett A., Allen A. Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: interim clinical guidance from the anticoagulation forum. J Thromb Thrombolysis. 2020;50(1):72–81. doi: 10.1007/s11239-020-02138-z. [DOI] [PMC free article] [PubMed] [Google Scholar]