Abstract
Background
Reports have indicated an association of large vessel peripheral arterial occlusion in the setting of Coronavirus Disease 2019 (COVID-19). While prior investigations have mostly focused on venous or cerebral arterial occlusions, we examined patients presenting exclusively with peripheral arterial extremity occlusions to investigate for any predisposing factors in this subset of COVID-19 patients.
Materials and methods
This is a retrospective study of COVID-19 patients with peripheral arterial occlusions presenting to a multi-hospital health care system in New York City between February 1st, 2020 and April 30th, 2020. Patient data and computed tomography angiography (CTA) exams in this subset were then collected and analyzed.
Results
For the months of February, March, and April 2020, we identified 9 patients (ages 37–93 yrs) at our health care system who underwent extremity CTA for large vessel upper or lower extremity arterial occlusion and were diagnosed with COVID-19. Patient medical histories and clinical parameters were evaluated to identify common risk factors including obesity, hypertension, hyperlipidemia, and diabetes. Patients presented with increased inflammatory markers including ferritin, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) as well as increased D-dimer.
Conclusion
Our findings suggest patients with COVID-19 and comorbidities presenting with elevated inflammatory markers and D-dimer may be at increased risk of large vessel peripheral arterial occlusion.
Keywords: COVID-19, Peripheral arterial occlusion, Thrombosis, Hypercoagulability, CTA
1. Introduction
The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) which causes COVID-19 has been found to induce a prothrombotic state manifesting in an increased incidence of venous thrombosis, acute coronary syndrome, and large vessel strokes [1,2]. Reports have suggested an increased incidence of acute extremity large vessel arterial occlusions with COVID-19 [3], which could result in limb loss. This led our team to investigate this phenomenon to assess common risk factors that could potentially lead to early screening for high risk patients. We identified 9 patients who presented to our healthcare system emergency rooms between February and April of 2020 with lower or upper extremity large vessel arterial occlusion in the setting of COVID-19.
2. Materials and methods
This was a retrospective institutional review board approved and Health Insurance Portability and Accountability Act (HIPAA) compliant study performed at a multi-hospital healthcare system in New York City. All extremity CTA exams between February 1st 2020 and April 30th 2020 were queried and those patients screened for concurrent SARS-CoV-2 infection. All adult patients (≥18 years old) with large vessel occlusion and confirmed COVID-19 were included in the study.
CTA imaging technique varied slightly between hospitals and scanners but included unenhanced images through the legs to evaluate for below the knee calcifications, thin section arterial phase imaging (0.625 mm to 1.25 mm) usually from the lung bases to the feet utilizing bolus tracking (150 HU threshold of the aorta at L1), immediately followed by repeat imaging from the mid-thigh to the feet to exclude unopacified vessels due to scanner outrunning the bolus. 125 mL iodinated contrast (iohexol 350 mg iodine/mL [Omnipaque 350, GE healthcare]) was administered at a rate of 4 mL/s. In patients with renal dysfunction, no adjustments in contrast amount was made. Complete imaging sets were reviewed including multiplanar reformats and volume rendered imaging by a single radiologist with 17 years' experience in body and vascular imaging (BF). The length of the arterial occlusions were recorded and classified as a short segment occlusion (<10 cm), intermediate length occlusion 10 to 20 cm, or long segment occlusion (>20 cm). The extent of atherosclerotic calcification at the occluded segment was evaluated as absent, mild, moderate, or severe based on a method previously described by Portugaller et al. [4]. If the lungs were partially imaged, the pulmonary findings were categorized as typical, indeterminate, atypical, or negative as per the Radiological Society of North America Consensus statement on Reporting Chest CT Findings Related to COVID-19 [5]. All patients were diagnosed with SARS-CoV-2 infection using rapid polymerase chain reaction tests.
Patient charts were reviewed for medical history, medications, inflammatory and coagulation labs, intervention, and outcomes.
3. Results
A summary of the results is provided in Table 1 . Nine patients [3 male, 6 female, age 37–93 (average age 71)] were admitted with large vessel extremity arterial occlusion in the setting of COVID-19 between the months of February and April 2020. In total, the health care system cared for approximately 6690 inpatients during this time and another 4355 patients through the emergency department who did not need to be admitted. This totals to 11,045 patients diagnosed with COVID-19 during this time period of which 9 individuals were diagnosed with acute extremity arterial occlusion on CTA. The incidence of extremity arterial occlusion by CTA amongst patients with COVID-19 was roughly 0.08%. Hypertension was the most common comorbidity (8/9 patients), followed by obesity (4/9) and insulin dependent diabetes (2/9). Two of the patients were taking anticoagulation medication, one for a history of CVA and the other for a history of atrial fibrillation. None of the patients had a history of an underlying hypercoagulable disorder. The most common patient complaint was extremity pain (6/9). One of the patients sustained multiple embolic cerebral infarcts in addition to the extremity arterial occlusion (Patient 3). None of the other eight patients were found to have an additional site of vascular occlusion other than the extremity arterial occlusions described.
Table 1.
Clinical characteristics of nine patients presenting with peripheral large vessel arterial occlusion.
| Variable | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Patient 7 | Patient 8 | Patient 9 |
|---|---|---|---|---|---|---|---|---|---|
| Age - yr | 38 | 37 | 80 | 84 | 68 | 77 | 69 | 93 | 89 |
| Sex | Male | Female | Female | Male | Female | Male | Female | Female | Female |
| Medical history and risk factors | Hypertension, obese | Obese, hypertension, diabetes, cerebral vascular accident | Atrial fibrillation, hyperlipidemia | Atrial fibrillation, hypertension, hyperlipidemia | Obese, diabetes, hypertension | Obese, hypertension, hyperlipidemia, rheumatoid arthritis | Hypertension, hyperlipidemia, rheumatoid arthritis | No past medical history | Hypertension |
| Home medications | Losartan | Chlorthalidone, clopidogrel | Apixiban | Metformin, pravastatin, amlodipine-olmesartan | Ibuprofen, insulin, levofloxan, simvastatin | Hydrochlorothiazide, tamsulosin, methotrexate | Amlodipine, insulin | None reported | None reported |
| Atherosclerosis | None | None | None | Mild | Moderate | Mild | Moderate | Severe | Moderate |
| COVID symptoms | Cough × 1 week | Dry cough and fever × 1 week | Diagnosed with COVID 1 week prior | Fever and SOB × 2 weeks. | Cough and SOB several days | Congestion and rhinorrhea × 2 weeks | Lack of appetite × 2 days | Altered mental status | Altered mental status |
| Time of COVID diagnosis to presentation? | Time of presentation | Time of presentation | 1 week prior | 1 week prior | Time of presentation | 1 week prior | Time of presentation | Time of presentation | Time of presentation |
| Imaging of Lung Bases for COVID-19 | Typical | Typical | Typical | Not included | Typical | Typical | Not included | Atypical. Pleural effusions and atelectasis. | No evidence for pneumonia. |
| Extremity symptoms | Right leg pain and right foot swelling × 9 days. | Acute onset right foot pain × 1 day. | Left upper extremity numbness & weakness × 1 h | Sudden onset cold left lower extremity. | Transferred from rehab facility with worsening foot pain and discoloration. | Sudden onset left leg pain and numbness 1 week after admission. | Worsening left leg pain and weakness × 2 days. | Transferred from nursing home and found to have lower extremity erythema, left greater than right, and cold to touch. | Pain when ambulating on right leg. |
| Imaging of extremities | 18 cm (intermediate length) occlusion from the right popliteal artery to the posterior tibial artery. | 77 cm (long segment) occlusion from the right proximal femoral artery to the feet. | 6 cm and 3.4 cm (two short segment) occlusions in the left proximal brachial artery and distal brachial artery respectively. | 3 cm and 52 cm (short segment and long segment) occlusions in the left common iliac artery and from the left popliteal artery to the feet respectively. | 25 cm (long segment) occlusion of the left distal femoral artery and popliteal artery stents. | 83 cm (long segment) occlusion of the entire left lower extremity from the common femoral artery to the feet. | 85 cm (long segment) occlusion of the entire left lower extremity from the common femoral artery to the feet. | 98 cm (long segment) occlusion of the entire left lower extremity from the common iliac artery to the feet. 28.5 cm (long length) occlusion involving the right femoral artery to the distal popliteal artery. | 18 cm (intermediate length) occlusion involving the left distal femoral artery and popliteal artery. Additional 20 cm (intermediate length) occlusion involving the right distal femoral and popliteal arteries. |
| Intervention | Popliteal artery cutdown, thrombectomy | Heparin infusion, thrombolysis, thrombectomy | Anticoagulation | Thrombectomy, fasciotomies | Left below knee amputation | Cut down, thrombectomy | Balloon angioplasty, cutdown, thrombectomy and above knee amputation | No intervention, palliative | Anticoagulation |
| Outcome | Discharged on anti-coagulation | Discharged on anticoagulation | Discharged on anticoagulation | Prolonged hospitalization | Discharged on anti-coagulation | Discharged on anti-coagulation | Discharged on anti-coagulation | Death | Discharged on anticoagulation |
| White-cell count – per mm3 (4500–11,000 mm3) | 11,900 | 10,700 | 12,000 | 10,000 | 21,100 | 13,800 | 23,000 | 14,800 | 6400 |
| Platelet count – per mm3 (150,000–450,000 mm3) | 370,000 | 429,000 | 563,000 | 325,000 | 613,000 | 323,000 | 427,000 | 313,000 | 228,000 |
| Prothrombin time – sec (12–14.2 s) | 13.3 | 14.6 | 13.9 | 16.9 | 18.6 | 15.2 | 15.8 | 15.7 | 14.8 |
| Fibrinogen – mg/dL (212–516 mg/dL) | – | 389 | 515 | 336 | 531 | – | 897 | 524 | – |
| D-dimer – ng/mL (0.0–500 ng/mL FEU) | 820 | >20,000 | 8210 | >20,000 | 2510 | 6080 | >20,000 | 2610 | – |
| Ferritin – ng/mL (15–150 ng/mL) | 86 | 232 | 395 | 464 | 1024 | 2055 | 2489 | 164 | – |
| Erythrocyte sedimentation rate – mm/h (0–20 mm/h) | – | – | 30 | 59 | 94 | 69 | 75 | 54 | – |
| C-reactive protein – mg/L (0.0–5.0 mg/L) | 15.2 | 62 | 37.6 | 171.3 | 75.1 | 56.5 | 234.2 | 41 | – |
In eight of the patients, CRP, D-dimer, and Ferritin were tested with CRP and D-dimer elevated in all eight patients and Ferritin elevated in seven. ESR was elevated in all six patients tested. White blood cell count was elevated in six of the nine patients.
A majority of the patients (6/9) had long segment lower extremity arterial occlusions (Fig. 1 ) with one having bilateral lower extremity long segment occlusions. One of those six patients had two segments of occlusion in the same lower extremity (one short and another long). One patient had bilateral lower extremity intermediate length arterial occlusions, and another patient had a single side lower extremity intermediate length arterial occlusion. Another patient had two short segments of upper extremity arterial occlusion (Fig. 2 ).
Fig. 1.
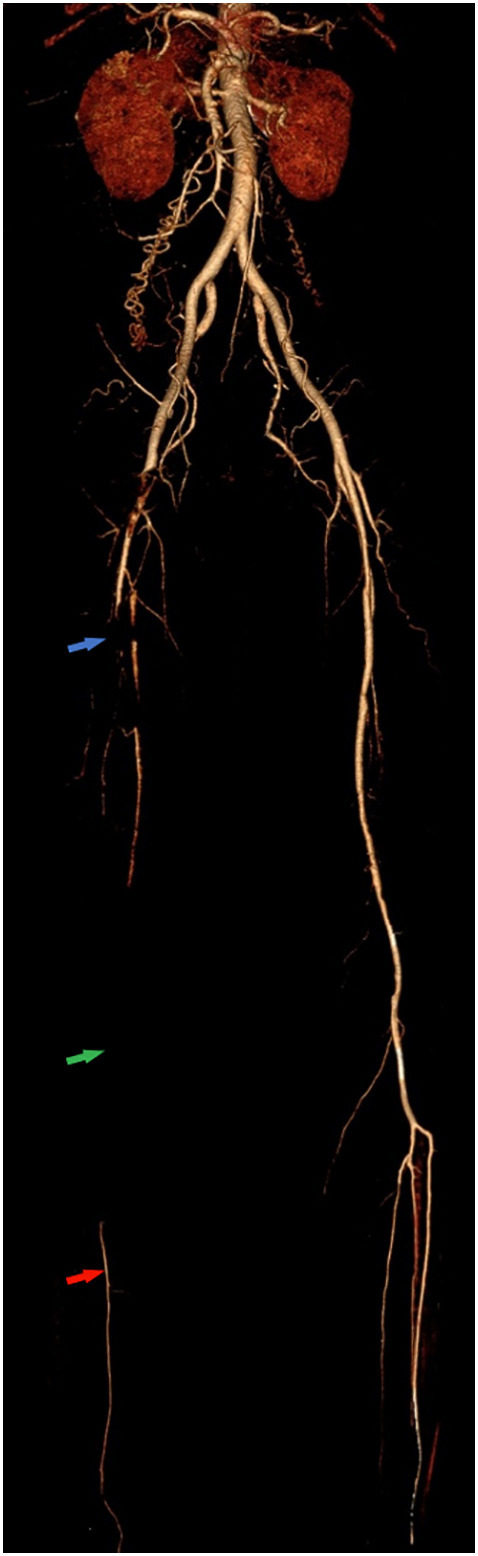
Lower extremity CTA volume rendered 3D reconstruction of a 37 year old female demonstrates long segment occlusion of the right femoral artery (blue arrow), popliteal artery (green arrow), posterior tibial artery and peroneal artery. The right anterior tibial artery remains patent (red arrow). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Fig. 2.
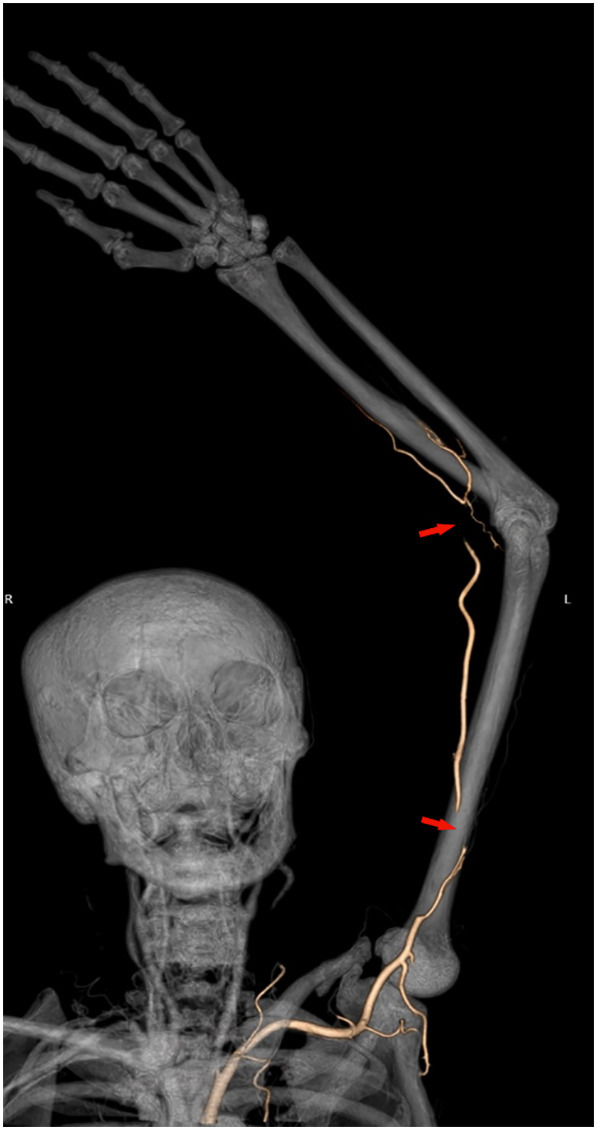
CTA volume rendered 3D reconstruction from an 80 year old female demonstrates two short segment left upper extremity brachial artery occlusions (red arrows). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Calcific atherosclerotic disease was relatively common with 4 of 9 patients with moderate or severe disease and 5 of 9 patients with none or mild disease. Only one patient had a prior lower extremity arterial intervention with stents and presented with a long segment occlusion of the stents extending from the left distal femoral artery to the popliteal artery (Fig. 3 ). Seven patients had a portion of the lungs included in the imaging with five of these patients having typical imaging findings for COVID-19 pneumonia. In patients with typical findings for COVID-19 pneumonia at the lung bases, the lengths of occlusion ranged from 3 cm to 83 cm with a mean of 33.4 cm. In the patient with atypical findings of COVID-19 pneumonia, the length of occlusion was 98 cm, and in the patient with no pulmonary findings for pneumonia, there were two intermediate length occlusions measuring 18 cm and 20 cm.
Fig. 3.
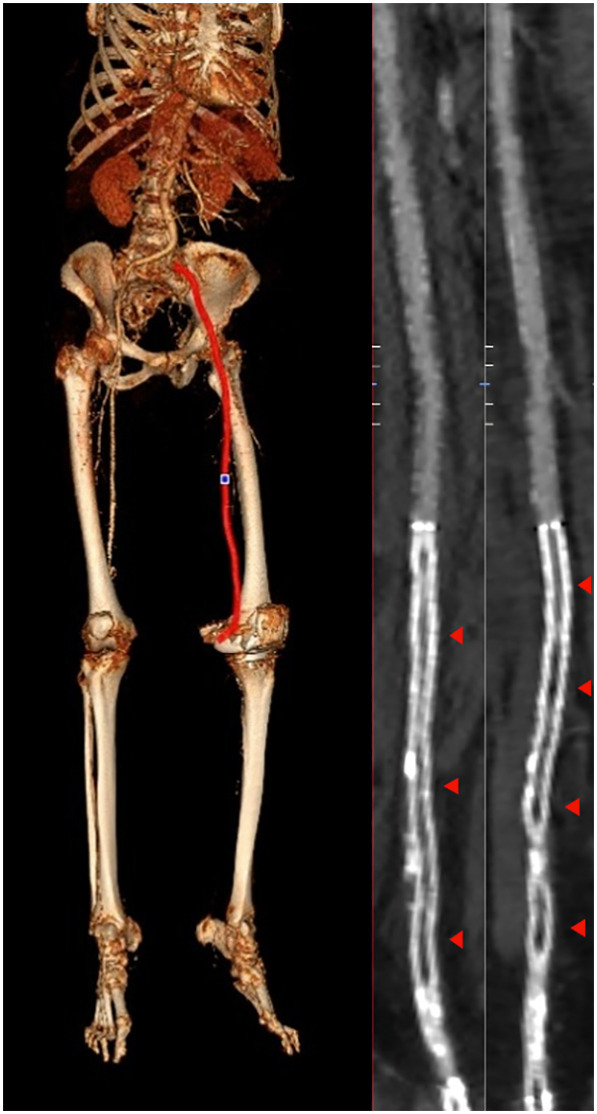
Lower extremity CTA volume rendered 3D reconstruction (image on left) with a red line indicating the vessel course used for two oblique curved reformats perpendicular to each other (two images on right) in a 68 year old female demonstrates long segment in-stent occlusion of the left distal femoral and popliteal artery stents (red arrowheads). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Two patients, both of whom had long segment arterial occlusions, required surgical amputation of the affected limb. Another patient declined intervention for palliative care. Five patients were managed with thrombectomy and two patients were treated with anticoagulation alone.
4. Discussion
To our knowledge this is the first study of large vessel peripheral extremity arterial occlusion in patients with COVID-19. The majority of our patients had associated comorbidities with hypertension and obesity being the most common. Most patients also had typical pulmonary findings of COVID pneumonia in the visualized lung bases. The length of arterial occlusion did not correlate with the severity of pneumonia. All patients with lower extremity arterial occlusions had at least one occlusive segment longer than 10 cm which was readily apparent on all multiplanar reformats as well as volume rendered imaging. We found that pre-existing calcific atherosclerotic disease is not a necessary factor in the development of COVID related arterial occlusion. Though the incidence is low, most of our patients that developed large vessel extremity arterial occlusion required invasive interventions such as open thrombectomy or amputation.
The mechanism of action is theorized to be in part due to systemic inflammatory changes and direct endothelial damage caused by SARS-CoV-2 induced endotheliitis [6,7]. This theory is supported by the presence of increased ESR and CRP in this patient population.
While this is the first study to examine this phenomenon in this novel disease, our study has inherent limitations. In addition to the biases of a retrospective study, this study is also limited by looking only at CTAs. If patients had been taken to the operating room immediately without a CTA for a suspected ischemic limb, this large vessel occlusion would not have been identified. Therefore, the incidence of extremity arterial occlusions in COVID-19 could be higher than what we report. Another limitation is having one unblinded radiologist view the images which creates bias and does not allow for evaluation of interobserver variability. However, we felt the arterial occlusions would be readily apparent to radiologists with vascular imaging experience.
5. Conclusion
Peripheral extremity arterial occlusion can be a presenting feature of COVID-19. Patients with a history of obesity or hypertension, with increased inflammatory markers and elevated D-dimer are potentially at increased risk. This observation suggests consideration for a lower threshold for performing CTAs on these patients, particularly if presenting with extremity symptoms. Additional studies with larger patient numbers are indicated to further study patients at risk for extremity arterial occlusion in COVID-19 and to evaluate which therapy may be most beneficial for this patient population.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Oxley T.J., et al. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020 doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bonow R.O., Fonarow G.C., O’Gara P.T., Yancy C.W. Association of Coronavirus Disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1105. [DOI] [PubMed] [Google Scholar]
- 3.Klok F.A., et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020 doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Portugaller H.R., Schoellnast H., Hausegger K.A., Tiesenhausen K., Amann W., Berghold A. Multislice spiral CT angiography in peripheral arterial occlusive disease: a valuable tool in detecting significant arterial lumen narrowing? Eur Radiol. 2004 doi: 10.1007/s00330-004-2289-1. [DOI] [PubMed] [Google Scholar]
- 5.Simpson S., et al. Radiological Society of North America expert consensus statement on reporting chest CT findings related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiol. Cardiothorac. Imaging. 2020 doi: 10.1148/ryct.2020200152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bikdeli B., et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Magro C., et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020 doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


