Abstract
Objective
To evaluate the effects of health insurance status on long-term cancer-specific survival of non-small cell lung cancer (NSCLC) in Beijing, China, using a population-based cancer registry data.
Methods
Information on NSCLC patients diagnosed in 2008 was derived from the Beijing Cancer Registry. The medical records of 1,134 cases were sampled and re-surveyed to obtain information on potential risk factors. Poorly-insured status was defined as Uninsured and New Rural Cooperative Medical Insurance Scheme (NRCMS), while well-insured included Urban Employees Basic Medical Insurance (UEBMI) and Free Medical Care (FMC). To estimate survival outcomes, individuals were followed-up until December 31, 2018. Cancer-specific survival probabilities at 5 and 10 years after diagnosis were estimated using the Kaplan-Meier method. Log-rank test was used to compare long-term survival with different characteristics. Multivariable Cox proportional hazard regression model was used to examine the relative effect of insurance status on cancer-specific mortality.
Results
Well-insured NSCLC patients have longer cancer-specific survival than poorly-insured individuals [hazard ratio (HR)=0.81; 95% confidence interval (95% CI): 0.67−0.97), even after adjusting for age, gender, cancer stage, smoking status, family history and residential area. Older age and rural residence were associated with a higher risk of cancer-specific mortality (HR=1.03; 95% CI: 1.02−1.03 and HR=1.25; 95% CI: 1.07−1.46, respectively). Smoking individuals had a 41% higher long-term cancer-specific mortality risk than non-smoking ones (HR=1.41; 95% CI: 1.20−1.66).
Conclusions
NSCLC patients with good insurance status had better survival rates than those with poor insurance. An association was significant even after 10 years. Large population-based studies are needed to validate that high reimbursement insurance status can lead to the improvement of long-term cancer prognosis in China.
Keywords: Non-small cell lung cancer, health insurance status, long-term survival
Introduction
Lung cancer is the leading cause of cancer-related death not only in China but also worldwide (1). Recently, there has been an increasing recognition of the financial toxicity of cancer-related treatment (2). Lung cancer is a disease with high cost and ominous prognosis. It brings a high socioeconomic burden and leads to financial loss. The total medical care expenditure of lung cancer in 2015 was 24.31 billion Chinese Yuan, accounting for approximately 0.6% of the total health expenditure in China (3). Despite the fact that the availability of screening and the administration of targeted therapy and immunotherapy are improving, the long-term survival and prognosis of non-small cell lung cancer (NSCLC) patients during the past decade remain unsatisfactory (4). Previous studies have indicated that patients may alter the care they received to help offset the out-of-pocket expenses associated with their oncologic treatment when faced with its financial burden (5). Health insurance status is an important factor in determining the receipt of cancer prevention and screening services as well as access to timely diagnostic care and cancer treatment. Even in individuals with a higher income, an absence of health insurance is associated with a decreased use of cancer screening test.
The potential effects of health insurance status on lung cancer survival have become of interest. A previous study showed that patients without insurance were more likely to present with advanced tumors and to have worse survival outcomes. Even among patients diagnosed with early-stage NSCLC, uninsured patients or patients with low reimbursement medical insurance had significantly lower survival than those with high reimbursement insurance. Moreover, Walker et al. found that among patients with the top 10 most deadly cancers, lung cancer had the highest proportion of uninsured patients in the US (6).
The status of health-care insurance in China has significantly improved in recent years. Near-universal medical insurance coverage has been achieved, with 97% coverage (1.33 billion) of the Chinese population in 2015 compared with only 85% (1.13 billion) in 2008 (7). However, large gaps in health-care utilization among individuals covered by different medical insurance schemes still exist, especially when faced with catastrophic diseases, such as lung cancer. The effects of health insurance status on long-term survival among NSCLC patients are not well studied in China. Thus, the aim of this study was to explore the potential association between health insurance status and 5- and 10-year survival among NSCLC patients using population-based retrospective survey data derived from the Beijing Cancer Registry (BCR).
Materials and methods
Population data
Using the International Classification of Diseases for Oncology (3rd edition, ICD-O-3), NSCLC patients were identified and included in the analysis. In 2010, we conducted a retrospective survey to investigate the potential risk factors, cancer stage and health insurance status of lung cancer patients diagnosed between January 1 and December 31, 2008 in Beijing, China (8). A total of 7,061 lung cancer patients with base-line demographic information (ICD10: C33−34) were extracted from the BCR, which was founded in 1976 and is one of the largest population-based cancer registries in China (9). Lung cancer cases diagnosed with the morphological types of small cell, lymphoma, sarcoma and malignant melanoma (n=531) and those with a death certificate from the Beijing Centre for Disease Control and Prevention (n=2,009) were excluded. Thus, a total of 4,521 patients were diagnosed with NSCLC in 2008. Facilities reporting inpatient information to the BCR included 3 tertiary cancer hospitals, 26 general tertiary hospitals, and 49 secondary hospitals in Beijing, covering 18 administrative districts of Beijing. To facilitate the study procedure, we randomly selected 1,276 cases (accounting for 28.2% of the total number of NSCLC patients) and included them into the retrospective survey (Supplementary Figure S1). This method has been described in detail elsewhere (8). Briefly, the information of the patients was extracted from the inpatient medical records of the hospital by trained registrars using a well-designed questionnaire. The questionnaire was approved by a panel of lung cancer experts, including epidemiologists and surgeons.
S1.
Flowchart of lung cancer cases included into analysis. NSCLC, non-small cell lung cancer.
Death certificate information from the vital statistic department of the Center for Disease Control and Prevention of Beijing was linked annually as a supplementary vital status source (10). For the analysis of cancer-specific mortality, the follow-up time was censored at the date of death for those who died from an underlying cause other than lung cancer. All cases included into analysis were followed up annually for vital status until December 31, 2018 using the passive follow-up method.
Patient-level health insurance status was categorized as no insurance, the Urban Employees Basic Medical Insurance (UEBMI), the New Rural Cooperative Medical Insurance Scheme (NRCMS), or Free Medical Care (FMC). Specifically, UEBMI, which was initiated for urban employees and retired employees in 1998, is a mandatory medical insurance scheme. NRCMS, launched in 2003, is a voluntary medical insurance scheme targeting rural populations. UEBMI is mainly financed by the payroll taxes from beneficiaries, whereas NRCMS is financed by the government. In general, the list of medical services eligible for reimbursement in the NRCMS is shorter than that in the UEBMI and the reimbursement rate is even low (7). FMC, originally introduced in February 1952, provides a lifetime of free outpatient and inpatient health services for government employees, retirees, disabled veterans, university teachers and students. In general, only primary members are covered by the FMC scheme, which is financed exclusively by the state budget, with no individual prepayment by its beneficiaries (11). Cancer stage was initially established on the basis of available information on the pathological stage. If data on the pathological stage were missing, clinical stage data were used instead. The American Join Committee on Cancer staging manual (7th edition; stages I−IV) was used for lung cancer staging in this study (12).
Statistical analysis
Cancer-specific survival probabilities at 5 and 10 years since diagnosis were estimated for each health insurance category using the Kaplan-Meier method. Log-rank test was used to compare the 5- and 10-year survival between Uninsured + NRCMS individuals and individuals with UEBMI+FMC insurance. Multivariable Cox proportional hazard regression model was used to examine the relative effect of insurance status on cancer-specific mortality. The model was adjusted for possible prognostic factors including gender, age, family history of cancer, smoking status, urban/rural residential areas, and cancer stage. Considering the sample size, we divided patients into two groups with different cancer stages: stage I+II and stage III+IV. All analyses were performed in Stata software (Version 15.0; StataCorp LLC, College Station, Texas, USA). Statistical significance was for two-sided tests and was set at P<0.05.
Results
General information
After excluding patients with missing data on covariates or survival time, a total of 1,134 patients who met the inclusion criteria were included. Among them, health insurance status of UEBMI, NRCMS, FMC and Uninsured were 62.96% (714 cases), 18.52% (210 cases), 7.50% (85 cases), and 11.02% (125 cases), respectively. Patients’ characteristics according to insurance status are shown in Table 1. Compared with UEBMI+FMC-insured individuals, a higher percentage of younger individuals (<60 years) were observed in the Uninsured + NRCMS category. UEBMI- and FMC-insured individuals were more likely to be males (65.58%) compared with Uninsured and NRCMS individuals (57.62%). Meanwhile, there was no significant difference in smoking status between the two insurance categories (59.09%vs. 54.76%, P=0.251). The proportion of NSCLC patients with stage I−IV in Beijing was 17.55%, 9.08%, 32.54%, and 40.83%, respectively. However, the distribution of cancer stage between the two insured categories was not significant (P=0.156). Compared with Uninsured + NRCMS patients (19.05%), most patients on UEBMI or FMC insurance (76.84%) resided in urban areas (Table 1).
1. Characteristics of NSCLC patients with different insurance status.
| Characteristics | n (%) | P | ||
| All patients | Uninsured+NRCMS | UEBMI+FMC | ||
| NSCLC, non-small cell lung cancer; NRCMS, New Rural Cooperative Medical Insurance Scheme; UEBMI, Urban Employees Basic Medical Insurance; FMC, Free Medical Care. | ||||
| Age [median (range)] (year) | 67 (24−92) | 68 (27−92) | 64 (24−87) | |
| Age groups (year) | 0.023 | |||
| <44 | 48 (4.23) | 15 (7.14) | 33 (3.57) | |
| 45−59 | 288 (25.40) | 62 (29.52) | 226 (24.46) | |
| 60−74 | 567 (50.00) | 99 (47.14) | 468 (50.65) | |
| 75− | 231 (20.37) | 34 (16.19) | 197 (21.32) | |
| Sex | 0.030 | |||
| Male | 727 (64.11) | 121 (57.62) | 606 (65.58) | |
| Female | 407 (35.89) | 89 (42.38) | 318 (34.42) | |
| Smoking | 0.251 | |||
| Yes | 661 (58.29) | 115 (54.76) | 546 (59.09) | |
| No | 473 (41.71) | 95 (45.24) | 378 (40.91) | |
| Cancer stage | 0.156 | |||
| I | 199 (17.55) | 31 (14.76) | 168 (18.18) | |
| II | 103 (9.08) | 18 (8.57) | 85 (9.20) | |
| III | 369 (32.54) | 82 (39.05) | 287 (31.06) | |
| IV | 463 (40.83) | 79 (37.62) | 384 (41.56) | |
| Family history | 0.016 | |||
| Yes | 96 (8.47) | 9 (4.29) | 87 (9.42) | |
| No | 1,038 (91.53) | 201 (95.71) | 837 (90.58) | |
| Residence | <0.001 | |||
| Urban | 750 (66.14) | 40 (19.05) | 710 (76.84) | |
| Rural | 384 (33.86) | 170 (80.95) | 214 (23.16) | |
Long-term survival of NSCLC patients with different health insurance status
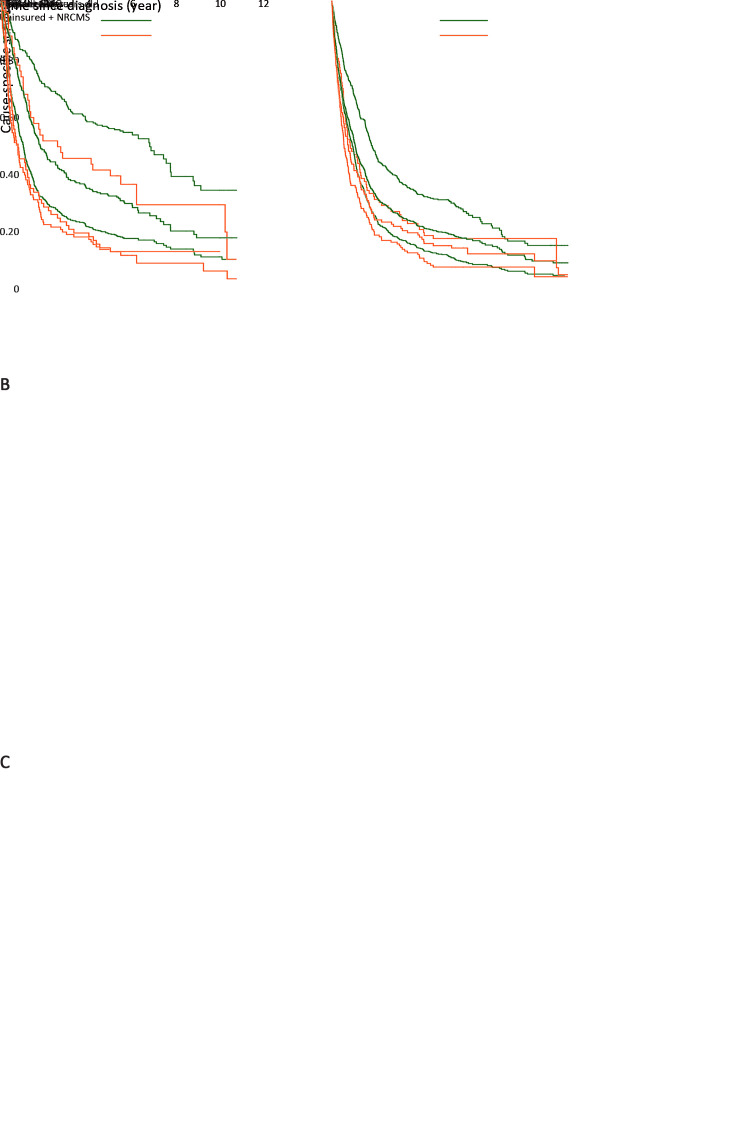
Five-year cancer-specific survival
Figure 1 and Table 2 show the long-term survival of NSCLC patients with different characteristics according to insurance status. The 5-year cancer-specific survival for NSCLC patients with UEBMI+FMC insurance was 23.38% [95% confidence interval (95% CI): 20.70−26.15], which was significantly higher than that of 14.76% (95% CI: 10.36−19.90) among individuals with the insurance status of Uninsured + NRCMS (P<0.001). For patients aged <60 years old, the 5-year survival among individuals with UEBMI+FMC and Uninsured + NRCMS was 32.43% (95% CI: 26.81−38.16) and 14.29% (95% CI: 7.59−23.02) (P<0.001), respectively. However, there was a marginal significant difference between the two insurance groups among patients ≥60 years old, with a 5-year survival of 19.85% (95% CI: 16.91−22.96) and 15.04% (95% CI: 9.59−21.64) (P=0.074), respectively. For patients with early-stage (I+II) NSCLC, the 5-year survival among individuals with UEBMI+FMC and Uninsured + NRCMS was 55.34% (95% CI: 48.99−61.21) and 40.82% (95% CI: 27.11−54.06) (P=0.015), respectively. Similar results were seen among patients with III+IV stage NSCLC. Among the current smoking patients, the 5-year survival among individuals with UEBMI+FMC was higher than that of Uninsured + NRCMS patients, but with no significantly difference [18.50% (95% CI: 15.37−21.86) and 13.04% (95% CI: 15.37−21.86), respectively; P=0.067]. Among the non-smoking patients, a significant difference was observed between the two insurance categories, with a 5-year survival of 30.42% (95% CI: 25.86−35.10) and 16.84% (95% CI: 10.14−25.00) (P<0.001), respectively.
1.
Kaplan-Meier curves for cause-specific survival of NSCLC patients between insurance category by different age groups (A); cancer stage (B) and smoking status (C). NSCLC, non-small cell lung cancer; UEBMI, Urban Employees Basic Medical Insurance; FMC, Free Medical Care; NRCMS, New Rural Cooperative Medical Insurance Scheme.
2. 5- and 10-year survival of patients with different characteristics in two categories of insurance.
| Characteristics | 5-year survival (95% CI) | P | 10-year survival (95% CI) | P | ||
| Uninsured+NRCMS | UEBMI+FMC | Uninsured+NRCMS | UEBMI+FMC | |||
| 95% CI, 95% confidence interval; NRCMS, New Rural Cooperative Medical Insurance Scheme; UEBMI, Urban Employees Basic Medical Insurance; FMC, Free Medical Care. | ||||||
| Age groups (year) | ||||||
| <60 | 14.29 (7.59−23.02) | 32.43 (26.81−38.16) | <0.001 | 12.38 (6.06−21.09) | 18.04 (12.27−24.71) | <0.001 |
| ≥60 | 15.04 (9.59−21.64) | 19.85 (16.91−22.96) | 0.074 | 10.05 (4.73−17.71) | 9.96 (6.95−13.61) | 0.073 |
| Stage | ||||||
| I+II | 40.82 (27.11−54.06) | 55.34 (48.99−61.21) | 0.015 | 30.47 (16.57−45.58) | 34.91 (25.88−44.08) | 0.008 |
| III+IV | 6.83 (3.62−11.42) | 11.33 (9.07−13.86) | 0.023 | 2.61 (0.52−11.46) | 4.40 (2.71−6.70) | 0.035 |
| Smoking | ||||||
| Yes | 13.04 (15.37−21.86) | 18.50 (15.37−21.86) | 0.067 | 3.11 (1.59−13.94) | 10.42 (7.10−14.46) | 0.044 |
| No | 16.84 (10.14−25.00) | 30.42 (25.86−35.10) | <0.001 | 8.42 (1.16−25.32) | 14.96 (10.38−20.32) | 0.002 |
| Total | 14.76 (10.36−19.90) | 23.38 (20.70−26.15) | <0.001 | 10.25 (5.63−16.48) | 12.27 (9.49−15.44) | <0.001 |
Ten-year cancer-specific survival
The 10-year cancer-specific survival with UEBMI+FMC insurance was 12.27% (95% CI: 9.49−15.44), which was significantly higher than that of 10.25% (95% CI: 5.63−16.48) among NSCLC patients who were Uninsured + NRCMS (P<0.001). However, there was no significance when examining patients aged ≥60 years, for which the 10-year survivals were 10.05% (95% CI: 4.73−17.71) and 9.96% (95% CI: 6.95−13.61) for Uninsured + NRCMS insurance and UEBMI+FMC insurance, respectively (P=0.073).
The 10-year survival rate in different health insurance status was also apparent among patients with stage I or II NSCLC, with 34.91 (95% CI: 25.88−44.08) in UEBMI+FMC group and 30.47% (95% CI: 16.57−45.58) in Uninsured + NRCMS group, respectively (P=0.008). For patients with stage III and IV NSCLC, the 10-year survival rates among patients with UEBMI+FMC insurance was 4.40% (95% CI: 2.71−6.70), while that for the Uninsured + NRCMS group was 2.61% (95% CI: 0.52−11.46) (P=0.035).
Regarding the smoking status, the 10-year survival rate among non-smoking individuals with UEBMI+FMC was higher than that among those with the insurance status of Uninsured + NRCMS, with survivals of 14.96% (95% CI: 10.38−20.32) and 8.42% (95% CI: 1.16−25.32), respectively (P=0.002). Among the smoking patients, survivals were 10.42% (95% CI: 7.10−14.46) and 3.11% (95% CI: 1.59−13.94) for those with UEBMI+FMC and Uninsured + NRCMS (P=0.044), respectively.
Impact factors for long-term survival of NSCLC patients
After controlling for possible confounding factors such as age, gender, cancer stage, smoking status, family history and residential areas in multivariate analysis, individuals with UEBMI+FMC insurance were still independently associated with a higher probability of long-term survival than individuals with Uninsured + NRCMS insurance types [hazard ratio (HR)=0.81; 95% CI: 0.67−0.97]. Further, older age, later stage, smoking status and rural residence were associated with a higher risk of cancer-specific mortality in multivariate analysis (Table 3).
3. Results of multivariable analysis to determine predictors of cancer-specific mortality in Beijing, China.
| Variables | HR | 95% CI | P |
| NRCMS, New Rural Cooperative Medical Insurance Scheme; UEBMI, Urban Employees Basic Medical Insurance; FMC, Free Medical Care; HR, hazard ratio; 95% CI, 95% confidence interval. | |||
| Insurance status | |||
| Uninsured+NRCMS | 1 | ||
| UEBMI+FMC | 0.81 | 0.67−0.97 | 0.021 |
| Age (Continuous) | 1.03 | 1.02−1.03 | <0.001 |
| Gender | |||
| Male | 1 | ||
| Female | 0.94 | 0.80−1.12 | 0.505 |
| Cancer stage | |||
| I | 1 | ||
| II | 1.53 | 1.12−2.10 | 0.007 |
| III | 3.17 | 2.52−3.98 | <0.001 |
| IV | 5.24 | 4.19−6.56 | <0.001 |
| Smoking status | |||
| NO | 1 | ||
| Yes | 1.41 | 1.20−1.66 | <0.001 |
| Family history | |||
| No | 1 | ||
| Yes | 1.18 | 0.94−1.49 | 0.161 |
| Areas | |||
| Urban | 1 | ||
| Rural | 1.25 | 1.07−1.46 | 0.006 |
There was no significant difference in cancer-specific mortality for female patients compared with male patients (HR=0.94, 95% CI: 0.80−1.12, P=0.505). Patients with family history of cancer had no significant elevated risk of death compared with patients with no family history (HR=1.18; 95% CI: 0.94−1.49, P=0.161).
Discussion
To our knowledge, this is the first study to examine long-term survival disparities of lung cancer according to the type of health insurance in China. Our results indicate that Uninsured or NRCMS-insured NSCLC patients had a significantly higher risk of death within both 5 years and 10 years of diagnosis than UEBMI- or FMC-insured patients, even after adjusting other confoundings such as age, gender, smoking status, family history, residential area and cancer stage. Our data are in line with previous data which show that patients with a good insurance status have better survival than that with poor insurance status, not just among patients with lung cancer, but also for other cancers, such as breast cancer (13), cervical cancer (14), colorectal cancer (15), bladder cancer (16), and soft tissue sarcoma (17).
The importance of insurance status on lung cancer patient’s survival has been highlighted by previous studies. Although many factors such as age, smoking status, residential area, lung cancer stage and histology may affect cancer survival, insurance status is a crucial aspect for the early detection, timely diagnosis and treatment of lung cancer (18).
This is highlighted by the disparities in insurance reimbursement rate. Patients with UEBMI, especially those insured by FMC, have a relatively high socioeconomic status. Individuals in this group are more concerned with health problems, have more cancer screenings, and have full access to medical treatment. Meanwhile, uninsured status is based on patients’ high out-of-pocket medical costs in relation to a lower income. These patients are medically indigent. Researchers have attributed the disparity in insurance to the potential impact that access to health services has on cancer diagnosis and mortality. Compared with well-insured patients, patients with poor or no insurance tend to receive cancer screening less frequently, have less access to hospitals with a higher level of care, are less likely to receive definitive therapy, and have higher mortality rates (19,20). Pezzi et al. showed that being uninsured was associated with a lower likelihood of both chemotherapy and radiation therapy (21). This situation, however, could be improved through the improvement of reimbursement rate of medical insurance, which would facilitate access to care, including prescription drugs.
Our results show that there was also a marked difference in survival among individuals with different insurance status by residential areas. Individuals lived in rural areas of the city were more likely to be Uninsured + NRCMS, while individuals lived in urban areas were more likely to be-insured with UEBMI+FMC. As a result, the long-term survival rates differed significantly according to insurance coverage in patients in different residential areas (rural vs. urban, HR=1.25, P=0.006). Previous studies have also reported that residential areas may influence cancer survival (22).
In this study, compared with poorly-insured patients (including Uninsured and NRCMS), those who were well-insured (including UEBMI and FMC) at diagnosis had a higher percentage of having stage I and stage II disease, although there was no significant difference between the groups. A previous study showed that compared with privately insured patients, uninsured patients had a significantly increased likelihood of stage II or stage III or IV cancer diagnosis versus stage I (18). However, small sample size and possibly selection bias may contribute to insignificant results of cancer stage in this study; thus, future studies with larger cohorts are necessary to validate these findings.
Although our data do not conclude that well-insured patients present with less advanced NSCLC, our study did reveal a trend in which only a minority of poorly-insured patients were among those diagnosed with stage I and II. Meanwhile, the majority of patients diagnosed with stage III lung cancer were poorly-insured or uninsured. This is in line with the results of Slatore et al., which also showed that those without health insurance presented with worse lung cancer stage at diagnosis (23).
In this study, we also assessed the influence of insurance status on cancer-specific mortality based on different age groups (<60 years or ≥60 years), cancer stage and smoking status. Our results are consistent with the research of Slatoreet al., which showed that younger Uninsured + NRCMS patients have worse survival than UEBMI- or FMC-insured patients (23). Similarly, previous research has shown that insurance status may be an independent survival predictor among young cancer patients (24). A prior study also showed that expansion of the insurance coverage may have a greater positive impact on the non-elderly cancer population (18). Our study also shows that even among patients with early stage (I and II) of NSCLC, poorly-insured patients had shorter cancer-specific survival than those with well-insured individuals.
Finally, there was no significant difference in 5-year survival between the two insurance categories among smoking patients. Nevertheless, non-smoking patients did have an advantage over current smokers in terms of long-time survival rates according to insurance status. Further, compared with those with poor insurance, non-smoking patients benefit the most in the well-insured group.
The major strength of this study is that we used a high-quality population-based cancer registration data to assess the relationship between insurance status and long-term cancer prognosis. Further, we specifically reported long-term survival results on NSCLC patients in Beijing. We identified insurance status as an impact factor on the survival of NSCLC patients, and showed that having poor health insurance is an important barrier for the fully receipt of medical care. In the context of cancer survival, long-term monitoring is essential to evaluate the effectiveness of treatment and cancer control activities at the population level. Thus, in this study, to determine the relationship between insurance status and NSCLC mortality, we used the 5- and 10-year cancer-specific survival as the primary outcome. Effects of insurance status vary greatly among different cancer types (15) and thus, we focus on NSCLC patients only in taking consideration of the heavy disease burden of lung cancer in Beijing.
This study has some limitations, most of which are from the database used for analysis. The database is sampled from a regional population-based cancer registry, which includes NSCLC patients previously diagnosed and treated in the hospitals in Beijing, and thus it may not represent prognosis of the whole lung cancer patients in Beijing. Small sample size was also an obstacle for detailed subgroups statistics and utilizing statistical models to control potential confoundings. In addition, due to the lack of historical data on other confounders, such as personal or family incomes, socioeconomic status, and careers, which have been also linked to insurance status and prognosis of lung cancer. We were unable to adjust these confounding factors in data analyses, which might lead to overestimation on the effect of health care insurance status, particularly on the attributable cancer-specific mortality risks. This should be the subject of future studies when such data are available. Further, it is important to note that patients who may have enrolled for other private insurance (commercial) may not have been fully captured in our data set. The database may also have some inherent limitations, owing to the lack of some important prognostic factors such as surgery methods, gene mutation status, comorbidities, and treatment methods. Future research should evaluate potential reasons for these disparities, including factors that lead to appropriate gene detection, surgical procedures, and targeted medication.
Conclusions
NSCLC patients with good insurance status had better survival rates than those with poor insurance. An association was significant even after 10 years. Large population-based studies are needed to validate that high reimbursement insurance status can lead to the improvement of long-term cancer prognosis in China.
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (No. 81600070) and Science Foundation of Peking University Cancer Hospital (No. 2020-10).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Contributor Information
Ning Wang, Email: bjwangning@126.com.
Jiafu Ji, Email: jiafuji@jhu.edu.
References
- 1.Bray F, Ferlay J, Soerjomataram I, et al Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Tran G, Zafar SY Financial toxicity and implications for cancer care in the era of molecular and immune therapies. Ann Transl Med. 2018;6:166. doi: 10.21037/atm.2018.03.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cai Y, Yan B, Zhou G Analysis of direct economic burden and average hospitalization cost of lung cancer in China in 2011-2015. Zhongguo Wei Sheng Tong Ji. 2018;35:334–7. [Google Scholar]
- 4.Zeng H, Chen W, Zheng R, et al Changing cancer survival in China during 2003-15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health. 2018;6:e555–e567. doi: 10.1016/S2214-109X(18)30127-X. [DOI] [PubMed] [Google Scholar]
- 5.Ellis L, Canchola AJ, Spiegel D, et al Trends in cancer survival by health insurance status in California from 1997 to 2014. JAMA Oncol. 2018;4:317–23. doi: 10.1001/jamaoncol.2017.3846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Walker GV, Grant SR, Guadagnolo BA, et al Disparities in stage at diagnosis, treatment, and survival in nonelderly adult patients with cancer according to insurance status. J Clin Oncol. 2014;32:3118–25. doi: 10.1200/JCO.2014.55.6258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou Y, Wushouer H, Vuillermin D, et al Medical insurance and healthcare utilization among the middle-aged and elderly in China: evidence from the China health and retirement longitudinal study 2011, 2013 and 2015. BMC Health Serv Res. 2020;20:654. doi: 10.1186/s12913-020-05522-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang N, Yang L, Yuan X, et al Current diagnosis status of the inpatient patients in Beijing, 2008. Zhonghua Yu Fang Yi Xue Za Zhi. 2013;47:278–9. [Google Scholar]
- 9.Yang L, Wang N, Yuan Y Secular trends in incidence of lung cancer by histological type in Beijing, China, 2000 - 2016. Chin J Cancer Res. 2019;31:306–15. doi: 10.21147/j.issn.1000-9604.2019.02.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang L, Yuan Y, Sun T, et al Population-based cancer incidence analysis in Beijing, 2008-2012. Chin J Cancer Res. 2015;27:13–21. doi: 10.3978/j.issn.1000-9604.2015.01.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ma J Reform of government employee and labor health insurance in China. Zhongguo Wei Sheng Jing Ji (in Chinese) 2000;19:60–2. [Google Scholar]
- 12.Sobin L, Gospodarowicz M, Wittekind C. TNM Classification of Malignant Tumors (7th Edition). Hoboken: Wiley-Blackwell, 2010.
- 13.Ko NY, Hong S, Winn RA, et al Association of insurance status and racial disparities with the detection of early-stage breast cancer. JAMA Oncol. 2020;6:385–92. doi: 10.1001/jamaoncol.2019.5672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Churilla T, Egleston B, Dong Y, et al Disparities in the management and outcome of cervical cancer in the United States according to health insurance status. Gynecol Oncol. 2016;141:516–23. doi: 10.1016/j.ygyno.2016.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cole AP, Lu C, Krimphove MJ, et al Comparing the association between insurance and mortality in ovarian, pancreatic, lung, colorectal, prostate, and breast cancers. J Natl Compr Canc Netw. 2019;17:1049–58. doi: 10.6004/jnccn.2019.7296. [DOI] [PubMed] [Google Scholar]
- 16.Fletcher SA, Cole AP, Lu C, et al The impact of underinsurance on bladder cancer diagnosis, survival, and care delivery for individuals under the age of 65years. Cancer. 2020;126:496–505. doi: 10.1002/cncr.32562. [DOI] [PubMed] [Google Scholar]
- 17.Jain V, Venigalla S, Sebro RA, et al Association of health insurance status with presentation, treatment and outcomes in soft tissue sarcoma. Cancer Med. 2019;8:6295–304. doi: 10.1002/cam4.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jemal A, Lin CC, Davidoff AJ, et al Changes in insurance coverage and stage at diagnosis among nonelderly patients with cancer after the affordable care act. J Clin Oncol. 2017;35:3906–15. doi: 10.1200/JCO.2017.73.7817. [DOI] [PubMed] [Google Scholar]
- 19.Abdelsattar ZM, Hendren S, Wong SL The impact of health insurance on cancer care in disadvantaged communities. Cancer. 2017;123:1219–27. doi: 10.1002/cncr.30431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stokes SM, Wakeam E, Swords DS, et al Impact of insurance status on receipt of definitive surgical therapy and posttreatment outcomes in early stage lung cancer. Surgery. 2018;164:1287–93. doi: 10.1016/j.surg.2018.07.020. [DOI] [PubMed] [Google Scholar]
- 21.Pezzi TA, Schwartz DL, Mohamed ASR, et al Barriers to combined-modality therapy for limited-stage small cell lung cancer. JAMA Oncol. 2018;4:e174504. doi: 10.1001/jamaoncol.2017.4504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mehta AJ, Stock S, Gray SW, et al Factors contributing to disparities in mortality among patients with non-small-cell lung cancer. Cancer Med. 2018;7:5832–42. doi: 10.1002/cam4.1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Slatore CG, Au DH, Gould MK, on behalf of the American Thoracic Society Disparities in Healthcare Group An official American Thoracic Society systematic review: insurance status and disparities in lung cancer practices and outcomes. Am J Respir Crit Care Med. 2010;182:1195–205. doi: 10.1164/rccm.2009-038ST. [DOI] [PubMed] [Google Scholar]
- 24.Aizer AA, Falit B, Mendu ML, et al Cancer-specific outcomes among young adults without health insurance. J Clin Oncol. 2014;32:2025–30. doi: 10.1200/JCO.2013.54.2555. [DOI] [PMC free article] [PubMed] [Google Scholar]