Abstract
Purpose
The objective of this study was to explore the predictors for failed reduction in children with developmental dysplasia of the hip (DDH) managed by arthrogram, closed reduction (CR) and spica cast immobilization.
Methods
We retrospectively reviewed the clinical data of patients with DDH treated by CR and cast immobilization (2015-2020), including age, sex, affected side, presence/absence of an ossific nucleus, International Hip Dysplasia Institute classification, the delineation of labrum and acetabular surface on arthrogram, inverted labrum, acetabular index (AI), hip abduction angle and medial dye pool (MDP) distance. Predictors that potentially predicted failure of CR were evaluated by logistic regression analysis, simple t-test, Fisher’s Exact Test and chi-square test.
Results
In total, 16 out of 187 hips failed to achieve initial CR (8.6%). Gender, age, preoperative AI and poor delineation of arthrogram were candidate predictors for failed CR in children aged six to 24 months with DDH; on the other hand, logistic regression analysis confirmed age and poor delineation of arthrogram significantly predicted failure of CR. Receive operating characteristic curve (ROC) showed MDP less than 6 mm and age higher than 14.5 months significantly increased the failure rate of CR in children aged six to 24 months with DDH.
Conclusion
Age and poor delineation of labrum and acetabular surface during arthrogram predicted failure of CR in children with DDH. In particular, age > 14.5 months and MDP distance ≥ 6 mm significantly increased the risk of CR failure.
Level of evidence
III
Keywords: developmental dysplasia of the hip, closed reduction, arthrogram, poor delineation, predictors
Introduction
Closed reduction (CR) and cast immobilization are common treatments for patients with dysplasia of the hip (DDH) aged six to 24 months.1,2 The goal of the treatments is to achieve a stable and concentric reduction of the hip as early as possible.3
Failure of reduction is a relatively common complication in children with DDH managed by CR with a reported rate ranging from 0% to 25%;1,4-10 moreover, failed CR has been reported to be associated with increased avascular necrosis AVN and poor radiographic outcome.6,9 Despite the fact that several predictors for failed CR in children with DDH have been investigated, including the patient’s age at reduction,11 the severity of the dislocation1 and the presence of an ossific nucleus at the time of reduction,12 controversy still exists. Thus, it is meaningful to investigate which factors can be associated with failed CR.
Arthrogram of the hip joint is a useful tool to evaluate the reduction of the hip during surgery in patients with DDH.6,13,14 Some authors found predictors that significantly predicted failure of CR were the presence of an inverted labrum13 and the widening of the medial dye pool (MDP) distance14 of the hip measured on an arthrogram, although some other authors reported different results.15 Furthermore, in clinical practice, poor delineation of the arthrogram can make the assessment of hip reduction difficult.
The main objective of this study was to evaluate which factors are predictive of early failure of CR in children with DDH.
Patients and methods
Patients
After securing IRB approval (GZWCMC 2015020904), all children aged six to 24 months with DDH managed by CR and spica cast immobilization at our institution were retrospectively reviewed (1st November 2015 to 31st March 2020).
The inclusion criteria were: (1) confirmed diagnosis of DDH; (2) being aged six to 24 months at the time of diagnosis; (3) CR and spica cast immobilization performed under general anaesthesia (GA); (4) complete clinical and radiographic data, including pre- and postoperative anteroposterior (AP) pelvic radiographs, intraoperative arthrogram and postoperative hip Magnetic Resonance Imaging (MRI) scan.
The exclusion criteria were: (1) concomitant diagnosis of developmental, congenital and/or neuromuscular diseases; (2) being aged < 6 months or >24 months at the time of the initial CR; (3) incomplete radiographic data; (4) treatment by open reduction without a prior CR attempt.
Arthrogram, CR and postoperative management
All patients underwent CR and spica cast immobilization under GA. Adductor tenotomy was performed if the adductor was considered to hinder CR (178 hips; 95.2%).
An arthrogram of the affected hip(s) was performed in all patients prior to any attempt of CR in order to (a) visualize the labrum and evaluate whether it was inverted or not; (b) visualize and measure (in mm) the MDP distance of the affected hip (the distance between the femoral head and the roof of the bony acetabulum); (c) assess the quality of the reduction. The arthrogram was considered successful if the following criteria were met: (a) a successful joint puncture and smooth injection of the contrast medium were noted in the surgical record sheet; (b) the diffusion of the contrast medium was limited to the hip joint (femoral head and the acetabulum); (c) the shape of the femoral head could be clearly visualized (Fig. 1).
Fig. 1.
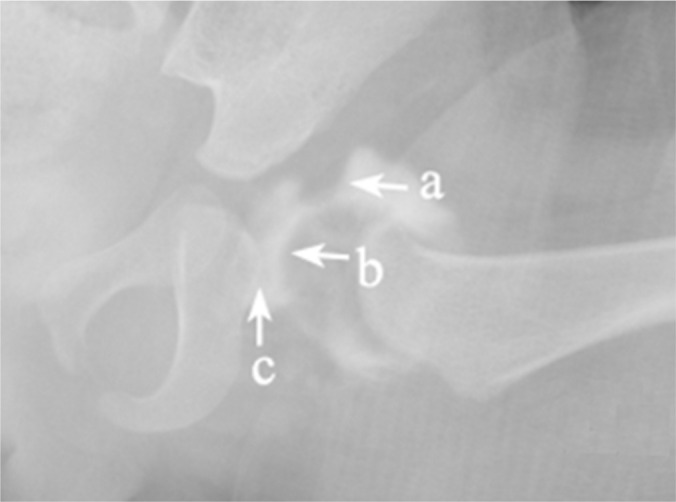
Satisfactory arthrogram with good delineation of labrum (a), femoral head (b) and medial dye pool (c).
Following stable CR, a spica cast in the human position was applied to all patients. AP pelvis radiographs were performed in the operating room to assess the quality of the reduction and an MRI scan was performed within 48 hours following surgery to confirm that the hip was reduced, and to measure the hip abduction angle (HAA). HAA is the angle between the axis of the femoral shaft and a line connecting the posterior edge of the right and left iliac bones, and it was measured on the T1W-SE MRI sequence in the axial plane (Fig. 2).
Fig. 2.
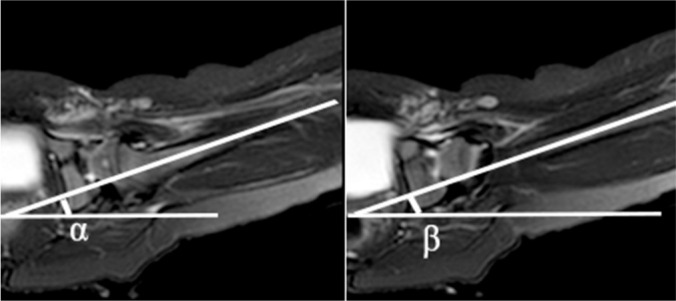
The hip abduction angle (HAA) is the angle between the axis of the femoral shaft and a line connecting the posterior edge of the right and left iliac bones (T1W-SE MRI sequence in the axial plane) (α, β).
Cast immobilization was applied for three months, and a cast change was performed routinely after six weeks to adjust the cast and check the reduction of the hip. Next, the patients were placed into a rigid, custom-made, abduction brace with the hip flexed and abducted at 100° and 60°, respectively, for another six months after cast removal.
Evaluation of the reduction and definition of failure of CR
The presence of the femoral head into the acetabulum was the main criteria to consider the reduction as acceptable.16 In particular, if the postoperative MRI scan showed that the femoral head was located in the acetabulum, the CR was considered acceptable. Failed CR was defined as the following criteria: (1) femoral head cannot be reduced into the acetabulum during the index procedure (open reduction required); (2) postoperative MRI indicated the femoral head was reduced into the acetabulum.17
Measurements on arthrogram
All patients underwent hip arthrogram prior to CR. If the surface of both the femoral head and acetabulum could be clearly identified on arthrogram images, the MDP and labrum were defined as ‘clear’ ( = good delineation) (Fig. 1); on the other hand, if one or both surfaces were not clearly identifiable, and the MDP and or labrum could not be clearly identified, the arthrogram was defined as ‘unclear’ ( = poor delineation) (Fig. 3).
Fig. 3.
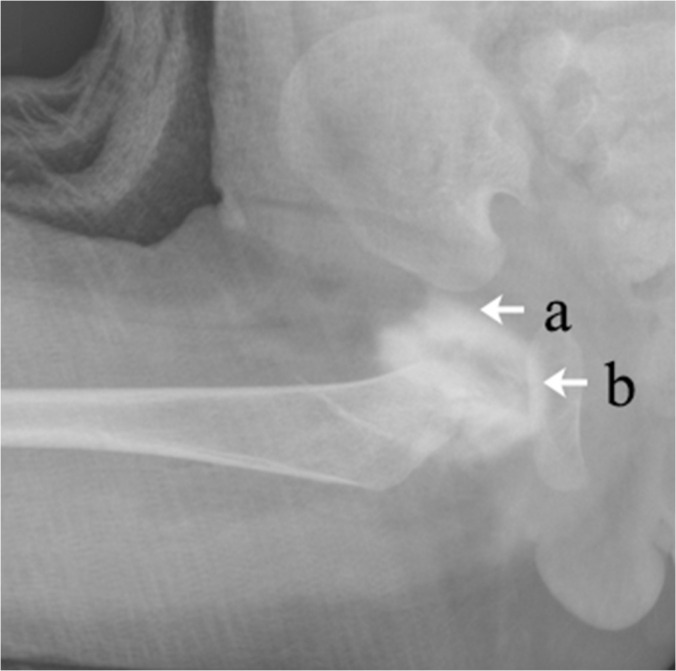
Arthrogram showing poor delineation of both labrum (a) and medial dye pool (b).
Anteroposterior (AP) pelvic radiographs of the hip were obtained after an attempt at a CR and cast immobilization. All the measurements were made on radiographs with hips flexed at 100 degrees and abducted at 60 degrees. The measurement of the MDP was performed on a Picture Archiving and Communication Systems (PACS). The MDP distance was measured in patients with good delineation of the arthrogram; a line parallel to Hilgenreiner’s line through the centre of the femoral head was drawn, and the distance, in mm, between the surface of the femoral head and the surface of acetabulum was measured18 (Fig. 4).
Fig. 4.

Measurement of medial dye pool on arthrogram: the distance (d) between the surface of the femoral head and the surface of the acetabulum is measured.
Statistical analysis
SPSS 19.0 statistical software (SPSS Chicago, Ilinois, USA) was used for data analysis. Data are expressed as frequencies and percentages, with means and standard deviations as appropriate. Chi-square tests, simple t-tests and Fisher exact tests were used to preliminarily screen predictors (p < 0.1), and then all the candidate factors were further confirmed by multivariate logistic regression analysis (p < 0.05). Independent simple t-tests, chi-square tests and Fisher exact tests were used to verify these predictors (p < 0.05). For quantitative data, we analysed the receiver operating characteristic (ROC) curve to determine the cut-off value of the factor. Statistical significance was established at p < 0.05.
Results
A total of 173 patients (21/12.1% males, 152/87.9% females) and 187 hips (88/47% left, 71/38% right, 28/15% bilateral) were enrolled in this study. The mean age at the time of CR and spica cast immobilization was 15.4 ± 4.4 months. According to the International Hip Dysplasia Institute (IHDI) classification,19 31 hips (16.6%) were grade II, 94 hips (50.3%) were grade III, and 62 hips (33.2%) were grade IV (Table 1).
Table 1.
The candidate predicting factors of failure of closed reduction (CR) in children with DDH
| Predictors | Successful CR (n) | Failure of CR (n) | t/χ2 | p* |
|---|---|---|---|---|
| Gender (male/female) | 19/152 | 4/12 | 0.152 | |
| Age (months) | 15.3 ± 4.5 | 17.6 ± 2.6 | 3.266 | 0.003 |
| IHDI grading: | ||||
| Grade II | 31 | 0 | ||
| Grade III | 84 | 10 | ||
| Grade IV | 56 | 6 | 3.521 | 0.172 |
| Severity of hip dislocation | ||||
| Mild (Grade II) | 31 | 0 | ||
| Severe (Grade III, IV) | 140 | 16 | 0.078 | |
| Laterality (left/right/bilateral) | 82/63/26 | 6/8/2 | 1.078 | 0.583 |
| Presence of ossific nucleus (yes/no) | 139/32 | 12/4 | 0.516 | |
| Preoperative Acetabular Index | 36.6 ± 4.5 | 34.4 ± 3.7 | 1.929 | 0.055 |
| Abduction angle | 67.8 ± 9.1 | 64.5 ± 20.1 | 1.096 | 0.274 |
| Delineation of arthrogram (good/poor) | 158/13 | 8/8 | 0.000 | |
| Inverted labrum (yes/no) | 138/20 | 8/0 | 0.598 |
IHDI, International Hip Dysplasia Institute
Simple t-test or Chi-square test or Fisher exact test
CR failed in 16/187 hips (8.6%). Of these 16 hips, four hips (25%) underwent immediate open reduction, five hips (31.3%) received open reduction due to failure of CR as confirmed by MRI scans, and seven hips (43.8%) obtained stable reduction through a second closed attempt within one week after initial CR. All patients were followed for one to three years post index procedure.
Factors predictive of failed CR
Age, preoperative acetabular index (AI) and poor delineation of arthrogram during surgery were candidate predictive factors of failed CR in children younger than 24 months, and were screened with chi-square tests, simple t-tests and Fisher exact tests (Table 1; p < 0.1).
All factors were further analysed by multivariate logistic regression analysis. Age and poor delineation of arthrogram were confirmed to be predictors that significantly predicted failure of CR in children with DDH (Table 2; p < 0.05).
Table 2.
Logistic analysis of potential predictors of failure closed reduction in children with DDH
| Predictors | Correlation coefficient | Standard error | Wald | p* | RR | 95% CI for RR |
|---|---|---|---|---|---|---|
| Age | 0.14 | 0.07 | 3.951 | 0.047 | 1.150 | 1.002-1.320 |
| Preoperative Acetabular Index | 0.121 | 0.069 | 3.099 | 0.078 | 0.886 | 0.775-1.014 |
| Delineation of arthrogram(good/poor) | 2.397 | 0.609 | 15.501 | 0.000 | 10.995 | 3.333-36.265 |
CI, Confidence Interval; RR, Relative Risk
Multivariate logistic regression analysis
Age
The mean age of children with successful CR (15.3 ± 4.5 months) was significantly lower than that of patients with unsuccessful CR (17.6 ± 2.6 months) (t = 3.266; p = 0.003) (Table 1); the ROC curve analysis showed that an age >14.5 months significantly increased the risk of failed CR (Fig. 5). In particular, the failure rate of CR in patients older than 14.5 months (13%) was significantly higher than that in patients younger than 14.5 months (1.7%) (Table 3; p = 0.023).
Fig. 5.
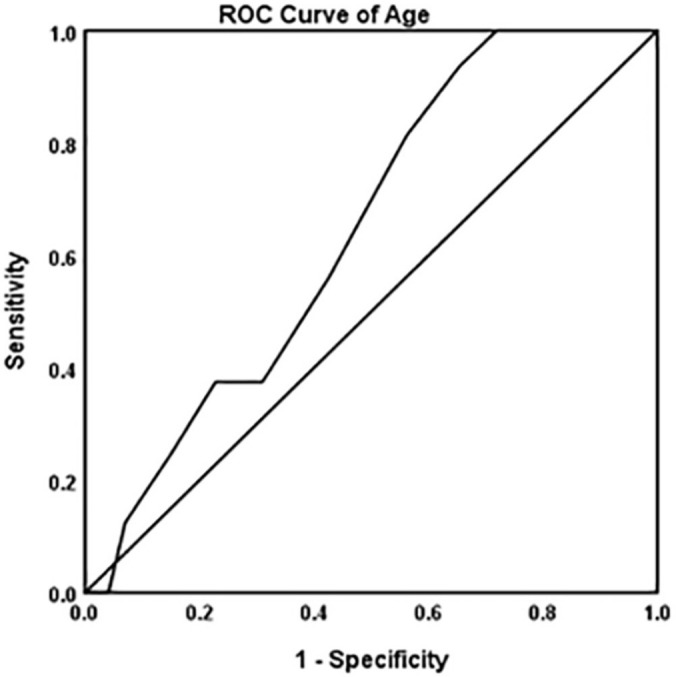
The receiver operating characteristic curve analysis for age; the area under the curve is 0.644, which indicates that age > 14.5 months increases the risk of failure of closed reduction in children with DDH.
Table 3.
Age >14.5 months and MPD ≥6 mm significantly increased the failure rate of closed reduction (CR) in children with DDH
| Successful CR (n) | Failure of CR (n) | p* | |
|---|---|---|---|
| Age >14.5 months | 112 | 15 | 0.023 |
| Age <14.5 months | 59 | 1 | |
| MPD ≥ 6 mm | 46 | 8 | 0.001 |
| MPD < 6 mm | 112 | 1 |
Fisher exact test
Poor delineation of labrum or MDP
Among the 187 hips, 185 hips (98.9%) had a successful arthrogram during index procedure; arthrogram failed in two hips (1.1%) which were enrolled in the poor delineation (‘unclear’) arthrogram group.
A total of 21 hips (11.2%) had poor delineation of the labrum or MDP: one hip had an unclear labrum (4.8%), 14 hips had an unclear MDP (66.7%), and six hips had both an unclear labrum and MDP (28.5%).
Patients with poor delineation of the labrum or acetabular surface on arthrogram (21 hips) had a significantly higher failure rate of CR (8/21 38.1%) than that (8/166 4.8%) in patients with good delineation of the labrum and acetabular surface (p < 0.001) (Table 1).
MDP ≥ 6 mm
Among the patients with good delineation of arthrogram (166 hips), MDP distance was measured. The MDP distance (4.8 ± 2.3 mm) in patients with successful CR was significantly smaller than that in patients with failed CR (8 ± 2.3 mm; p < 0.001).
ROC curve analysis showed MPD ≥ 6 mm increased the failure rate of CR in children with DDH (Fig. 6). The failure rate of CR in children with an MDP distance ≥ 6 mm (13.2%) was significantly higher than that in patients with an MDP distance < 6 mm (0.9%; p < 0.001) (Table 3).
Fig. 6.
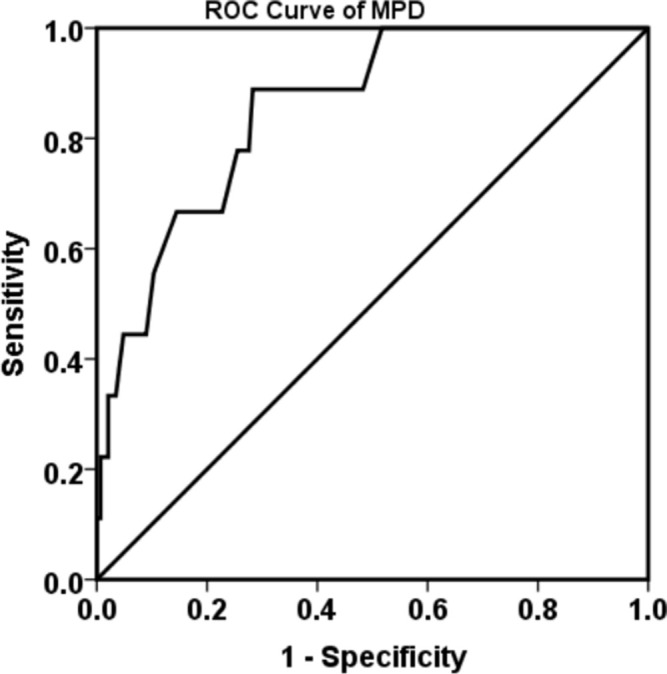
The receiver operating characteristic analysis for medial dye pool (MDP); the area under the curve is 0.795, which indicates that MDP distance ≥ 6 mm increases the risk of failure of closed reduction in children with DDH.
No failed CR was recorded in patients without an inverted labrum, while CR failed in eight out of 146 hips (5.5%) with an inverted labrum; however, the difference between these two groups was not statistically significant (p = 0.598) (Table 1).
Gender, laterality, absence of an ossific nucleus, amount of hip abduction, IHDI grade, severity of hip dislocation and presence of an inverted labrum were not predictors for CR failure in DDH patients (Table 1).
Discussion
Our study highlights that age and poor delineation of labrum and acetabular surface distance on arthrogram significantly predicted failure of CR in children with DDH aged six to 24 months at the time of surgery. In particular, we found age >14.5 months and MDP distance ≥ 6 mm significantly increased the risk of failed CR.
Our study shows the overall failure rate of CR in children with DDH is 8.6%; previous studies reported a failure rate of CR ranging from 0 to 25%.1,4-10 In particular, the overall rate of failure of reduction in previous studies was 10% (44/441) (Table 4),1,4-10 which is similar to our results.
Table 4.
The reported failure rate of closed treatment in children with DDH
| Study | Journal | No. of hips | Failure rate |
|---|---|---|---|
| Terjesen T1 | Acta Orthop | 78 | 4 (5.1%) |
| Ishii Y4 | Clin Orthop Relat Res | 40 | 0 (0%) |
| Murray T5 | Am J Orthop (Belle Mead NJ) | 35 | 2 (5.7%) |
| Race C6 | J Pediatr Orthop | 59 | 8 (13.6%) |
| Zionts LE7 | J Bone Joint Surg Am | 51 | 13 (25.5%) |
| Yamada N8 | J Bone Joint Surg Br | 62 | 5 (8.1%) |
| Sankar WN9 | J Pediatr Orthop | 87 | 8 (9.2%) |
| Barakat AS10 | Curr Orthop Pract | 29 | 4 (13.8%) |
| Total | 441 | 44 (10%) |
Furthermore, in the present study, seven out of 16 hips (43.8%) with initial failure of CR were successfully reduced through a second closed attempt, and the overall CR failure rate was reduced to 4.8%. The possible reasons for such a finding could be the decreased tension of soft tissue around the hip following initial CR, and the increased abduction angle of the hip that could be achieved during the second closed attempt.
Our study indicates that poor delineation of arthrogram significantly predicts failure of CR. The rate of unsuccessful CR of hips with poor arthrogram (38.1%) was significantly higher compared to hips with good delineation (4.8%) of arthrogram. Although another study showed that evaluation of hip arthrogram during surgery is frequently unreliable,15 most authors believe that intraoperative arthrogram is still an important tool to evaluate the quality of reduction, especially when immediate MRI is not available.6,13,14 In this study, 21 of 187 hips (11.2%) had an ‘unclear’ labrum and/or MDP. Our study found that the main reason for the presence of ‘unclear’ labrum and MDP was not related to technical issues but rather to failure of CR. In patients with failed CR, the dislocated femoral head does not anatomically interact with the acetabulum nor the labrum. Additionally, the femoral head (dislocated posteriorly) and the acetabulum (anterior) are somehow overlapped, thus making the delineation of the intra-articular structures unclear. As a result, intraoperative arthrogram only shows the surface of the femoral head, while the labrum and the MDP appear as ‘unclear’. Thus, if the arthrogram is poorly visualized, failure of CR should be suspected. Under this condition, we recommend removing the cast immediately and repeating the CR procedure as 43.8% of the hips obtained stable reduction through a second closed attempt. However, if the arthrogram still shows poor delineation of the labrum and widening of MDP distance, an open reduction is recommended.
The analysis of our results found that, among patients with good arthrogram, a MDP distance ≥ 6 mm significantly increased the risk of failure of CR. In our study, the failure rate in this subgroup of patients was 13.2%. Race et al. reported that satisfactory reduction could be achieved in patients with an MDP distance < 7 mm.6 Therefore, the quality of reduction should be assessed taking into account objective and measurable MRI findings rather than be based on subjective judgement. In our study, MRI was consistently used to evaluate the quality of the reduction. In particular, we found an MDP distance ≥ 6 mm significantly increased the risk of failure of CR. Hypertrophic ligamentum teres, pulvinar, transverse ligament and compression of the hip capsule by the iliopsoas muscle may explain the increased MDP distance on plain radiographs;6,14,20 moreover, all these factors are mechanical obstacles for the reduction. Thus, if the arthrogram shows good delineation but MDP ≥ 6 mm, careful attention should be paid and an MRI should be performed to make sure whether the reduction has been obtained or not.
Interestingly we found inverted labrum is not a predictor of failed CR. However, controversy still exists as to whether the presence of an inverted labrum can increase the risk for CR failure in children with DDH. Staheli et al. considered that an inverted labrum was one of the factors inhibiting hip reduction,21 while some authors believe that there is no correlation between an inverted labrum and failure of CR in children younger than 24 months of age.12,13 In our study, the vast majority of DDH patients (88%) had an inverted labrum while only 20 hips (12%) did not. Patients with and without inverted labrum had a similar failure of CR rate (p = 0.598). In our clinical practice we found that successful CR can be achieved even though the labrum is inverted; moreover, it has been shown that an inverted labrum can gradually improve after reduction (‘docking effect’).12,22 Additionally, although an inverted labrum might contribute to a wide MDP,20 which was identified as a predictor of failure of reduction, the statistical analysis did not show any correlation between an inverted labrum and failure of reduction. Thus, further study should be performed to investigate the effect of an inverted labrum on the failure of reduction.
Our study did identify age as a significant predictor of failure of CR. Controversy still exists as to whether age at closed treatment influences the outcome in children aged six to 24 months with DDH. In particular, several authors reported that older patients had a greater chance of open reduction than younger patients.23-25 However, some other authors could not find a significant correlation between age and failure of CR.9,13,26 In our study, the mean age of patients with failed CR was significantly higher than that of patients with successful CR; in particular, multivariate logistic regression analysis indicates age was a predictor for failure of CR.
In conclusion, age and poor delineation of labrum and acetabular surface during arthrogram predicted the failure of CR in children with DDH. In particular, age > 14.5 months and MDP distance ≥ 6 mm significantly increased the risk of failure of CR in children with DDH aged six to 24 months.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: Approval from our Institutional Review Board was obtained for this retrospective study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was not required from all individual participants included in the study.
ICMJE Conflict of interest statement
None declared.
Author Contributions
ZY: Study design, Performed measurements, Data analysis, Manuscript preparation.
YQL: Statistical analysis, Performed measurements, Manuscript preparation.
KH: Data collection, Statistical analysis, Manuscript preparation.
JPW: Data collection, Performed measurements.
FC: Study design, Manuscript preparation and modification.
HWX: Study design, Performed measurements, Manuscript preparation.
References
- 1. Terjesen T, Halvorsen V. Long-term results after closed reduction of latedetected hip dislocation: 60 patients followed up to skeletal maturity. Acta Orthop 2007;78:236-246. [DOI] [PubMed] [Google Scholar]
- 2. Cooper AP, Doddabasappa SN, Mulpuri K. Evidence-based management of developmental dysplasia of the hip. Orthop Clin North Am 2014;45:341-354. [DOI] [PubMed] [Google Scholar]
- 3. Dezateux C, Rosendahl K. Developmental dysplasia of the hip. Lancet 2007;369:1541-1552. [DOI] [PubMed] [Google Scholar]
- 4. Ishii Y, Ponseti IV. Long-term results of closed reduction of complete congenital dislocation of the hip in children under one year of age. Clin Orthop Relat Res 1978:167-174. [PubMed] [Google Scholar]
- 5. Murray T, Cooperman DR, Thompson GH, Ballock T. Closed reduction for treatment of development dysplasia of the hip in children. Am J Orthop (Belle Mead NJ) 2007;36:82-84. [PubMed] [Google Scholar]
- 6. Race C, Herring JA. Congenital dislocation of the hip: an evaluation of closed reduction. J Pediatr Orthop 1983;3:166-172. [DOI] [PubMed] [Google Scholar]
- 7. Zionts LE, MacEwen GD. Treatment of congenital dislocation of the hip in children between the ages of one and three years. J Bone Joint Surg [Am] 1986;68:829-846. [PubMed] [Google Scholar]
- 8. Yamada N, Maeda S, Fujii G, Kita A, Funayama K, Kokubun S. Closed reductionof developmental dislocation of the hip by prolonged traction. J Bone Joint Surg [Br] 2003;85:1173-1177. [DOI] [PubMed] [Google Scholar]
- 9. Sankar WN Gornitzky AL, Clarke NMP, et al. , ; International Hip Dysplasia Institute Closed reduction for developmental dysplasia of the hip: early-term results from a prospective, multicenter cohort. J Pediatr Orthop 2019;39:111-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Barakat AS, Zein AB, Arafa AS, et al. Closed reduction with or without adductor tenotomy for developmental dysplasia of the hip presenting at walking age. Curr Orthop Pract 2017;28:195-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Alassaf N. Prediction of the requirement of open reduction for developmental dysplasia of the hip. J Int Med Res 2018;46:54-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hattori T, Ono Y, Kitakoji T, Takashi S, Iwata H. Soft-tissue interposition after closed reduction in developmental dysplasia of the hip. The long-term effect on acetabular development and avascular necrosis. J Bone Joint Surg [Br] 1999;81:385-391. [DOI] [PubMed] [Google Scholar]
- 13. Forlin E, Choi IH, Guille JT, Bowen JR, Glutting J. Prognostic factors in congenital dislocation of the hip treated with closed reduction. The importance of arthrographic evaluation. J Bone Joint Surg [Am] 1992;74:1140-1152. [PubMed] [Google Scholar]
- 14. Liu JS, Kuo KN, Lubicky JP. Arthrographic evaluation of developmental dysplasia of the hip. Outcome prediction. Clin Orthop Relat Res 1996:229-237. [DOI] [PubMed] [Google Scholar]
- 15. Yong B, Li Y, Li J, et al. Post-operative radiograph assessment of children undergoing closed reduction and spica cast immobilization for developmental dysplasia of the hip: does experience matter? Int Orthop 2018;42:2725-2731. [DOI] [PubMed] [Google Scholar]
- 16. Li YQ Li M, Guo YM, et al. , Chinese Pediatric Orthopedics Multicenter Clinical Study Group Traction does not decrease failure of reduction and femoral head avascular necrosis in patients aged 6-24 months with developmental dysplasia of the hip treated by closed reduction: a review of 385 patients and meta-analysis. J Pediatr Orthop B 2019;28:436-441. [DOI] [PubMed] [Google Scholar]
- 17. Druschel C, Placzek R, Selka L, Seidl T, Funk J. MRI evaluation of hip containment and congruency after closed reduction in congenital hip dislocation. Hip Int 2013;23:552-559. [DOI] [PubMed] [Google Scholar]
- 18. Gans I, Sankar WN. The medial dye pool revisited: correlation between arthrography and MRI In closed reductions for DDH. J Pediatr Orthop 2014;34:787-790. [DOI] [PubMed] [Google Scholar]
- 19. Narayanan U Mulpuri K, Sankar WN, Clarke NM, Hosalkar H, Price CT; International Hip Dysplasia Institute , . Reliability of a new radiographic classification for developmental dysplasia of the hip. J Pediatr Orthop 2015;35:478-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Studer K, Williams N, Studer P, et al. Obstacles to reduction in infantile developmental dysplasia of the hip. J Child Orthop 2017;11:358-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Staheli LT, Dion M, Tuell JI. The effect of the inverted limbus on closed management of congenital hip dislocation. Clin Orthop Relat Res 1978:163-166. [PubMed] [Google Scholar]
- 22. Talathi NS, Chauvin NA, Sankar WN. Docking of the femoral head following closed reduction for DDH: does it really occur? J Pediatr Orthop 2018;38:e440-e445. [DOI] [PubMed] [Google Scholar]
- 23. Roposch A, Stöhr KK, Dobson M. The effect of the femoral head ossific nucleus in the treatment of developmental dysplasia of the hip. A meta-analysis. J Bone Joint Surg [Am] 2009;91:911-918. [DOI] [PubMed] [Google Scholar]
- 24. Luhmann SJ, Bassett GS, Gordon JE, Schootman M, Schoenecker PL. Reduction of a dislocation of the hip due to developmental dysplasia. Implications for the need for future surgery. J Bone Joint Surg [Am] 2003;85:239-243. [DOI] [PubMed] [Google Scholar]
- 25. Bolland BJ, Wahed A, Al-Hallao S, Culliford DJ, Clarke NM. Late reduction in congenital dislocation of the hip and the need for secondary surgery: radiologic predictors and confounding variables. J Pediatr Orthop 2010;30:676-682. [DOI] [PubMed] [Google Scholar]
- 26. Schur MD, Lee C, Arkader A, Catalano A, Choi PD. Risk factors for avascular necrosis after closed reduction for developmental dysplasia of the hip. J Child Orthop 2016;10:185-192. [DOI] [PMC free article] [PubMed] [Google Scholar]


