Abstract
Purpose
Double and triple femoral neck lengthening osteotomies have been described to correct coxa brevis deformity. Only small studies reported the results. Our aim was to provide an overview of the outcomes of double and triple femoral neck lengthening.
Methods
After an extensive search of different online databases, we included studies reporting the results of double and triple femoral neck osteotomies. Clinical and radiological outcomes, and reported complications were extracted. The review process was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Results
After evaluating 456 articles, we included 11 articles reporting 149 osteotomies in 143 patients (31% male, 64% female, 5% unspecified). Mean age of the patients was 20 years (range 7 years to 52 years). Indications were developmental hip dysplasia (51%), Perthes disease (27%), infection (6%), post-trauma (4%), congenital disorders (2%), slipped capital femoral epiphysis (1%), idiopathic (3%) and unknown (6%). The mean limb length discrepancy reduced by 12 mm (0 mm to 40 mm). In total, 65% of 101 positive Trendelenburg sign hips experienced improvement of abductor muscle strength. An 18% (9% to 36%) increase could be found in functional hip scores. Mean increase in articulo-trochanteric distance was 24 mm (10 mm to 34 mm). Five patients older than 30 years at the time of osteotomy and two younger patients with prior hip incongruency had disappointing results and required arthroplasty. In all, 12 complications occurred in 128 osteotomies, in which complications were reported.
Conclusions
Double and triple femoral neck lengthening osteotomies in coxa brevis show good results with few complications in the literature, especially in young patients with non-arthritic hips.
Level of evidence
III
Keywords: proximal femoral osteotomy, femoral neck lengthening, Morscher osteotomy, Coxa brevis, hip dysplasia
Introduction
Reduced longitudinal growth of the femoral neck or coxa brevis, a result of premature closure of the capital femoral physeal plate, occurs in several conditions such as Legg–Calve–Perthes disease, developmental hip dysplasia, infection, trauma and idiopathic avascular necrosis of the hip, and causes shortening of both the length of lower limb and hip abductor lever arm.1 Furthermore, an enlarged, high-positioned greater trochanter due to relative overgrowth reduces the tension of the abductor muscles and, together with short lever arm, causes abductor insufficiency.2,3 Major clinical manifestations are limping, limited range of motion, pain and early onset of osteoarthritis.4–6 No clear indications for surgical treatment have been described yet, but according to literature, refractive pain, difficulty in walking and functional impairments leading to limitation of daily activities can be considered as general indications for surgery.1
Alongside several recommended interventions for correction of coxa brevis deformity, in 1980 Dr. Erwin W. Morscher described a special femoral neck lengthening osteotomy, which consisted of simultaneous lateralization of the femoral shaft and distal transfer of the greater trochanter by making three parallel osteotomies at the base of the greater trochanter, and at the upper and lower borders of the femoral neck (Fig. 1a).7 The major goals of this method were distalization of the greater trochanter to optimize the abductors’ lever arm and to diminish greater trochanteric–pelvic impingement, lengthening the femoral neck to normalize the articulo-trochanteric distance (ATD), and lengthening of the leg.8 A very similar osteotomy was described later by Lascombes et al, which included two osteotomy lines (Fig. 1b).9 Precursory osteotomies were fixed by angle-blade plates, but some modifications in fixation method were introduced later.10–12
Fig. 1.

Femoral neck lengthening osteotomies: (a) Proximal femoral triple osteotomy,16 (b) proximal femoral double osteotomy.9
Morscher triple osteotomy and the later double proximal femoral osteotomy seem to be unsophisticated and effective methods for lengthening the short femoral neck and improving the related disabilities in patients with coxa brevis. Although primary outcomes were promising and few complications were reported, no consensus exists about the indications for patient selection and appropriate target groups. The aim of this study is to provide a comprehensive overview of the clinical and radiological outcomes, and complications of the double and triple proximal femoral osteotomies in patients with coxa brevis.
Materials and methods
We conducted a comprehensive search in Pubmed, CINAHL and Embase libraries for published articles using the following search strategy: ‘(((proximal femoral deformity) OR hip dysplasia) OR coxa brevis) AND (((femoral neck lengthening) OR double proximal femoral osteotomy) OR triple proximal femoral osteotomy)’. No restrictions were imposed regarding the type of study, language or publication date. References of the selected articles also were checked for possibly missed papers. The search was performed at the end of February 2020. After importing the articles into Covidence systematic review software,13 duplicates were removed and the articles were screened by their title and abstract. Subsequently, authors assessed remaining articles for full-text eligibility. Studies reporting clinical outcomes of double and triple femoral neck lengthening osteotomies in patients with short femoral neck were included for data extraction, while no limitations were placed regarding the patients’ demographic data, underlying cause of deformity and duration of follow-up. Other forms of osteotomies and particularly isolated distal transfer of greater trochanter were excluded.
Extracted data included characteristics of the patients, in addition to clinical and radiological outcomes and complications. Pain, ability to walk and joint range of motion in the frame of functional hip scores, as well as limb length discrepancy (LLD) and Trendelenburg test were recorded. As radiological measures, we extracted ATD (Fig. 2a), centro-trochanteric distance (CTD)(Fig. 2b), lever-arm ratio (LAR) (Fig. 2c), neck-shaft angle (NSA) (Fig. 2d), femoral neck length and the severity of hip osteoarthritis. We used the method proposed by Black et al to classify the reported complications (Table 1).14 The review process was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (see supplementary information).
Fig. 2.
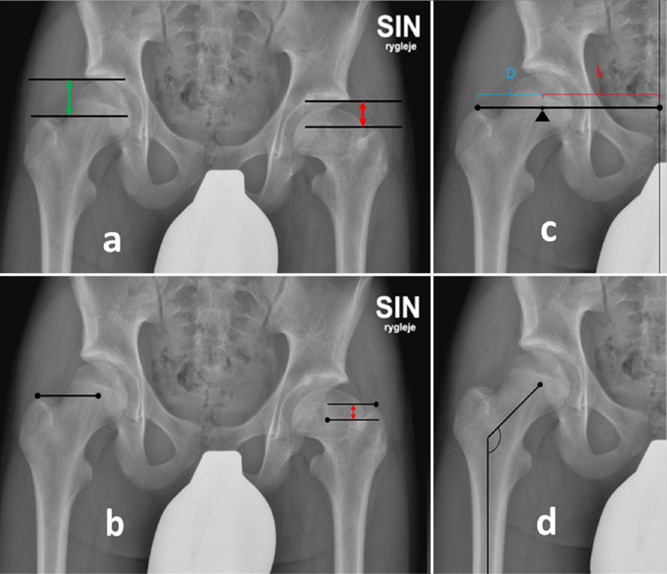
Radiographic criteria in pelvic radiograph from a 14-year-old male with 2 cm limb length discrepancy (LLD) after Perthes disease at the age of six years: (a) Articulo-trochantric distance (ATD) is defined as the vertical distance between the highest part of articular surface of the femoral head and the tip of the greater trochanter. Normal ATD in the right hip (green double arrow), the value is negative when the tip of the greater trochanter is above the most cephalic portion of the femoral head (red double arrow).24 (b) Centro-trochanteric distance (CTD) is the vertical distance between the centre of the femoral head and the tip of the greater trochanter. The value should normally be zero, as the centre of femoral head and tip of greater trochanter lie at the same level (right hip), CTD is abnormal in the left hip (red double arrow).24 (c) Lever arm ratio (LAR) is the ratio of the horizontal distance between the centre of the femoral head and the pubic symphysis (L) to the distance between the centre of the femoral head and the top of the greater trochanter (D) (LAR = L/D).21 (d) Neck-shaft angle (NSA): the angle formed between femoral shaft axis and femoral neck. Normal NSA is 125° to 131°.40
Table 1.
Black classification for complications14
| Category | Definition |
|---|---|
| I | Minimal intervention required; treatment goal still achieved |
| II | Substantial change in treatment plan; treatment goal still achieved |
| IIIA | Failure to achieve treatment goal; no new pathology or permanent sequelae |
| IIIB | Failure to achieve treatment goal and/or new pathology or permanent sequelae developed |
Results
The PRISMA flow diagram for selecting articles is depicted in Fig. 3. All 11 articles finally selected for this review were retrospective studies. Six articles written in other languages were translated into English. The mean duration of follow-up in nine of these studies was 74 months (range 6 months to 192 month), and two articles did not mention the duration of follow-up.11,15 In seven studies, triple osteotomies introduced by Morscher were applied12,15–20 and four studies reported results of double proximal femoral osteotomies.9–11,21 Overall, 143 patients were included, of whom six underwent bilateral osteotomies (149 hips). Demographic data are demonstrated in Table 2.
Fig. 3.
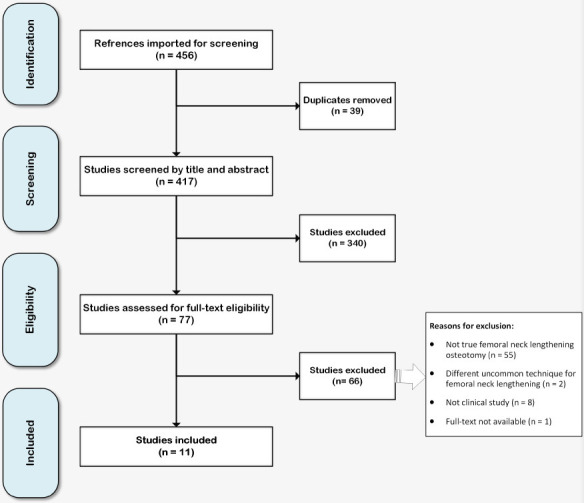
PRISMA flowchart.
Table 2.
Demographic data of the articles reporting double and triple osteotomies
| Type of intervention | Double osteotomy | Triple osteotomy | Total | |
|---|---|---|---|---|
| Age (range, years) | 14(7–36) | 24 (8–52) | 20 (7–52) | |
| Sex | Male | 6 | 39 | 45 |
| Female | 9 | 82 | 91 | |
| Unknown | 7 | 0 | 7 | |
| Etiology | DDH | 9 | 64 | 73 |
| LCPD | 7 | 32 | 39 | |
| Septic | 2 | 6 | 8 | |
| Post-trauma | 1 | 5 | 6 | |
| Idiopatic | 0 | 5 | 5 | |
| Congenital | 3 | 0 | 3 | |
| SCFE | 0 | 1 | 1 | |
| Unknown | 0 | 8 | 8 | |
| Total | 22 | 121 | 143 | |
DDH, developmental dysplasia of the hip; LCPD, Legg–Calve–Perthes disease; SCFE, slipped capital femoral epiphysis
Limb lengthening
Ten papers reported the results of limb lengthening in 144 operated hips of 138 patients with the mean of 12 mm (range 0 mm to 40mm) (n = 144). Eight studies reported reduction in mean LLD, from 23 mm (range 0 mm to 60mm ) preoperatively, to mean11 mm (range 0 mm to 35 mm) post-operatively (Fig. 4).11,12,16–21
Fig. 4.

Column scatter plot, demonstrating the distribution of average limb length discrepancies before and after the operation.
In one study, acute correction of mean LLD from 32 mm (range 20 mm to 45mm) to 0.3 mm (range 0 mm to 10 mm) right after the surgery was reported, but at the end of follow-up, the mean effective limb lengthening was 19 mm (range 0 mm to 40 mm). The authors reported one case with loss of 30 mm of acquired length due to unauthorized early weight bearing.20 In another study, the authors could achieve a mean of 20 mm (range 15 mm to 25 mm) increase in limb length, depending on the width of the graft.15 Decreased mean LLD from 23 mm (range 0 mm to 60 mm) to 13 mm (range 0 mm to 30 mm) in another study, could restore normal gait in 13 of 14 patients with shortening limp.18 In the most recent study, the patients had improvement in mean LLD from 21 mm (range 0 mm to 40 mm) to 8 mm (range 0 mm to 15 mm).17 Inferior results with 6 mm decrease in mean LLD, from 18 mm (range 0 mm to 40 mm) to 12 mm (range 0 mm to 35mm), were found in one study. However, LLD reduced in ten patients, did not change three patients and increased in two patients.12
Trendelenburg test
In seven of these articles a mean 65% (29% to 100%) success rate in converting a Trendelenburg sign to negative was reported in 101 preoperatively positive hips (Fig. 5).10,12,16–19,21
Fig. 5.

Column scatter plot, demonstrating the distribution of positive Trendelenburg test percentage, before and after the osteotomy.
In one case series study of five patients, negative Trendelenburg sign and improvement in abductor insufficiency limp were reported in all patients after six weeks to 12 weeks of follow-up,10 while another study reported that in five of six patients the Trendelenburg sign became negative.21 In the latest study, the Trendelenburg sign remained positive in six of 20 hips, while four of them were sequelae of Perthes disease.17
One study reported an inferior success rate in restoration of abductor strength; five of 17 positive Trendelenburg signs became negative.19
Functional outcomes
Eight studies evaluated functional hip scores in total 102 hips (97 patients). Mean increase in hip function score was 18 % (9% to 36%).
Harris Hip Score was reported in 26 hips of 23 patients in two papers.11,17 Mean scores increased from 73 to 95,17 and from 83 to 94, after the osteotomy.11
Six studies applied Merle d’Aubigné score in 76 hips (74 patients), and reported a mean a three-point increase in the overall score, from 14 (range seven to 16) to 17 (range two to 18).12,16,18–21
The maximum reported increase was from 13 (SD = 2) to 18 (SD = 2).21 Another report on 16 operated hips demonstrated increasing Merle d’Aubigné scores from 14 (7 to 16) to 16 (2 to 18). The scores for ‘pain’, ‘ability to walk’ and ‘range of motion’ increased from 4.2 to 5.0, 4.2 to 5.3 and 5.2 to 5.3, respectively. The authors also reported an unexpected decrease in the score from nine to two in one patient with preoperatively moderate to severe osteoarthritis, who underwent arthroplasty one year after the osteotomy.16 Similar findings could be found in another study.18 ‘Very good’ and ‘good’ results were demonstrated in all eight patients of another study and, regarding pain control, two showed total pain relief and four experienced marked improvements.20 Another study reported improvement of the functional score in six of 15 patients.12
In regard to range of motion, 10° to 20° improvement in hip abduction was reported in one study,9 and another study reported a non-limited range of motion after about three months to six months.10
Radiologic evaluation
Radiological measures were documented in seven of 11 articles, including 99 operated hips of 95 patients.9,11,12,17,18,20,21
Four articles reported ‘severity of osteoarthritis’ in 78 patients (80 hips).12,17,18,20 In one study, authors noted a worsening of osteoarthritis and the necessity for arthroplasty in five of eight patients in the 30 years to 49 years age group with preoperative osteoarthritis.18 In another study, 12 of 15 patients experienced some degree of deterioration of osteoarthritis based on Croft classification22 (seven patients had one grade, four patients had two grades and one patient had three grades worsening of the osteoarthritis).12 Another study reported two cases of progression of osteoarthritis in younger patients; a 16-year-old female and a 20-year-old male (bilateral), both were the sequalae of Perthes disease and finally required total hip arthroplasty.17
Changes in NSA were described in 17 patients (19 operated hips). Two studies reported increasing NSA from 86° to 110° and from 110° to 116°.9,11 while one study demonstrated no significant change.21 Regarding ATD, four studies reported a mean 24 mm (range 10 mm to 34 mm) increase in 34 operated hips of 32 patients, who had negative amounts preoperatively.9,11,12,21 Two studies reported a mean 24 mm decrease in CTD in 20 operated hips, from 33 mm to 7 mm,12 and from 38 mm to 19 mm.9 Femoral neck length was only reported in one study, and a mean 17 mm increase in femoral neck length was recorded in five hips.9 Decrease in LAR from 1.97 (SD = 0.28) to 1.60 (SD = 0.13) was demonstrated in another study.21
Complications
Three studies stated that they did not have any complications,10–12 while there were no reports regarding complications in three articles.9,15,21
Overall, 12 complications were recorded in five articles, reporting the results of 128 osteotomies.16–20 We categorized the complications based on the Black classification:14
Nine category-I complications included: hematoma due to anti-coagulant (n = 3); wire breakage (n = 2); greater trochanter slide up (n = 2); asymptomatic pseudarthrosis of greater trochanter (n = 1); transient peroneal nerve palsy (n = 1).
Two category-II complications included: angle-blade plate migration that required revision (n = 1); non-union of greater trochanter due to inadequate fixation which required revision (n = 1).
No category-IIIA.
One category-IIIB included: loss of reduction due to angle-blade migration due to unauthorized early weight bearing, causing varus deformity and failure of lengthening of the limb (n = 1).20
Overall results regarding limb lengthening, abductor function improvement, functional scores and duration of follow-up are shown in Table 3.
Table 3.
Overall outcomes of reviewed studies
| Author | Year of publication | Number of the patients | Number of the hips | Limb lengthening (mm) | Abductor improvement* (%) | HHS** (Pre-op–Post-op) | Merle d’Aubigné (Pre-op–Post-op) | Follow-up (range, months) |
|---|---|---|---|---|---|---|---|---|
| Eidelman et al17 | 2019 | 18 | 20 | 13 | 70 | (73–95) | N/A | 84 (54–120) |
| Plazcek et al | 2018 | 5 | 5 | N/A | 100 | N/A | N/A | (3–6) |
| Libri et al11 | 2010 | 5 | 6 | 15 | N/A | (83–94) | N/A | N/A |
| Lengsfeld et al12 | 2001 | 15 | 15 | 6 | 75 | N/A | (7–9)*** | 122 (102–147) |
| Hasler et al18 | 1999 | 37 | 37 | 10 | 70 | N/A | (16–17) | 96 (12–192) |
| Takata et al21 | 1999 | 7 | 8 | 9 | 83 | N/A | (13–17) | 71 |
| Weissinger et al20 | 1995 | 8 | 8 | 19 | N/A | N/A | N/A | 45 (13–76) |
| Dostal et al | 1994 | 8 | 8 | 20 | N/A | N/A | N/A | N/A |
| Hefti et al19 | 1989 | 20 | 21 | 10 | 29 | N/A | N/A | 36 (6–72) |
| Buess et al16 | 1988 | 15 | 16 | 12.5 | 67 | N/A | (13–15) | 62 (9–84) |
| Lascombes et al9 | 1985 | 5 | 5 | 15 | N/A | N/A | N/A | (12–36) |
| Sum | 143 | 149 | ||||||
| Average | 12 | 65 | (78–94) | (14–17) | 74 (3–192) |
Success rate in converting a positive Trendelenburg test to negative
Harris Hip Score
Sum of ‘pain’ and ‘ability to walk’ scores
Discussion
To our knowledge, this is the first review of the clinical and radiological outcomes of double and triple femoral neck lengthening osteotomies. Although coxa brevis is a paediatric orthopaedic disease and the underlying problem occurs during the childhood, many patients develop physical limitations and osteoarthritis during early adulthood, and the mean age of the patients at the time of surgery was 20 years (range 7 years to 52 years). The results indicate substantial improvement in LLD and functional score. In addition, hip abductor strength was enhanced in the majority of the patients, while few complications were reported.
Several interventions with different results have been proposed for correction of short femoral neck deformity, such as epiphysiodesis of the greater trochanter,23 lateral transfer of greater trochanter,24 distraction osteogenesis by Ilizarov technique25 and different proximal femoral osteotomies.26–28 In patients with concurrent intra- and extra-articular hip pathologies, relative femoral neck lengthening in combination with head–neck osteochondroplasty via surgical hip dislocation has shown promising early and mid-term results with regard to pain reduction and improving function and radiographic parameters.29–31 However, Morscher proximal femoral osteotomy and its modifications have been described as completely extra-articular procedures with the goal of lengthening the femoral neck and improving the anatomy and biomechanics of the hip in patients with coxa brevis. Theoretically, increasing the length of the femoral neck will reduce limb shortening, relieve pain and improve functional outcomes. However, only a few retrospective studies have reported the outcomes of the operations. Therefore, we systematically searched the literature to answer questions regarding the potential risks, pitfalls and complications.
Functional outcome scores by measuring several criteria provide a practical tool for evaluation of the outcome of an intervention. The Harris Hip Score and Merle d’Aubigné scores were used by these studies. To our knowledge these scores have not been validated for the paediatric population. The main components of the Harris Hip Score are pain, function and range of motion, and was primarily developed for the evaluation of the results of hip arthroplasty in an adult population,32 but has been applied frequently in various hip disabilities.33–35 The Merle d’Aubigné score takes pain, gait and mobility into account to analyse hip function.36 Ability to walk, as one of these criteria, revealed significant improvement in the majority of patients. Limping in patients with coxa brevis is attributable to several factors such as LLD, abductor insufficiency, pain and impingement.1 The results of double and triple proximal femoral osteotomies, in terms of pain relief and improvement in abductor force and functional outcomes, were comparable to reported results on relative femoral neck lengthening and osteochondroplasty.29–31 but unlike relative femoral neck lengthening, favourable increase in the length of the respective leg has been reported in double and triple proximal femoral osteotomies and, consequently, gait improvement is expected in patients with LLD. The results demonstrated that almost full equalization of the length of the lower limbs was possible in some patients, given the fact that the amount of shortening is not generally substantial in isolated hip deformities. The strength of hip abductor muscles as another contributing factor in normal gait increased in about two-thirds of patients. In comparison with other treatment methods, the proportion of hips with normal abductor strength after surgical hip dislocation and relative neck lengthening increased by 74%,29 while after isolated intertrochanteric osteotomy, no hip showed normal abductor strength.37 In our review the lowest percentage in elimination of Trendelenburg sign was reported in one study with the success rate of 30%.19 A possible explanation is that the mean age of the patients in the study was higher compared to the mean age of the patients in all studies (34 years versus 20 years). This finding suggests that satisfactory outcomes are more achievable in younger subjects with a higher capacity to restore abductor muscle strength.
Several factors, including muscle fatigue, bony impingement and degenerative changes, cause pain in patients with coxa brevis.29 Although it is difficult to interpret ‘pain relief’ as a criterion for outcome due to its subjective nature and also its insufficient report in the studies, good results regarding pain relief have been demonstrated by some of the articles.12,16,18,20 Reasonably, restoration of the normal hip anatomy and biomechanics would contribute to pain relief by enhancing the stamina of muscles and elimination of impingement. Most of the studies reported satisfactory clinical outcomes, although the progression of osteoarthritis after double and triple proximal femoral osteotomies was inevitable.12,20 Even other treatment options for coxa brevis, such as relative femoral neck lengthening and osteochondroplasty by surgical hip dislocation, that address the intra-articular pathologies, could not prevent the process of degeneration.29 This is possibly due to pre-existing articular damage and also the inability to fully restore a normal hip anatomy.38 However, it is not known whether and to what extent the improvements in hip biomechanics and thereby the distribution of the forces around the joint might slow down the process of degeneration. On the other hand, elongation of the femoral neck to restore LLD in patients with coxa brevis will increase the pressure in the hip joint and will have a negative effect on pre-existing articular pathology. However, in patients without prior intra-articular pathology, improvement in hip biomechanics would outweigh this adverse effect.
An important finding is that ‘age at the time of surgery’ seems to be an important determinant factor of the outcomes. We found superior results regarding limb lengthening, abductor strength improvement and functional outcome scores in studies with younger subjects (mean age < 18 years old (range seven years to 20 years)) compared with the studies with mean age of the patients older than 18 years (range eight years to 49 years). In addition, of the five out of seven patients that required arthroplasty, more were more than 30 years old at the time of surgery,18 and two young patients had hip incongruency and osteoarthritis before osteotomy.17
The rate of reported complications in double and triple osteotomies was similar to the relative neck lengthening and osteochondroplasty, and half of the complications were due to fixation of greater trochanter.29 However, in contrast to relative neck lengthening and osteochondroplasty, no intra-articular complications were reported in the articles in our review. Between double and triple osteotomies, making three osteotomy lines would hypothetically increase the risk of developing complications and all reported complications occurred in the triple osteotomy group. Overall, 50% of the 12 recorded complications were related to the fixation of the greater trochanter, and this observation highlights the importance of applying more reliable methods in fixation of greater trochanter in patients with preoperatively short, contracted abductor muscles. Overall, there were three major complications; two resolved with additional interventions, and only one complication could not be corrected finally and resulted in permanent loss of achieved limb length.20
The major limitation of our review results from the fact that our data were obtained exclusively from retrospective case series. We were also required to translate six articles to English to extract the data. Moreover, as a result of low numbers of double and triple osteotomies, we could not perform reasonable statistical comparison between the two groups. Besides, outcomes were not reported adequately. For example, no papers reported how the Trendelenburg test was performed and it is unclear how the outcome was interpreted. This makes comparison between studies difficult. The major weakness in terms of reporting complications was that no articles met the criteria for describing the methods for collecting data, definition, severity grading, risk factors and duration of the complications.39 In addition, the absence of reporting ‘zero’ complications in three articles made it unclear whether data was omitted or complications did not occur.9,15,21
Overall, favourable clinical outcomes can be expected after double and triple osteotomies. However, the patients should be selected meticulously since the results were rather disappointing in older patients with incongruent hips and pre-existing degenerative changes.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with Ethical Standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical Statement
Ethical approval: This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent: Not required for this work.
ICMJE Conflict of Interest Statement
The authors declare that they have no ICMJE conflict of interest
Author Contributions
AG: Searching databases, Screening the articles by title, abstract, and full-text, Quality assessment and data extraction, Analysis and interpretation of the data, Writing the manuscript, Making the figures and tables.
SK: Original idea, Analysis and interpretation of the data, Writing the manuscript, Making the figures and tables.
OR: Original idea, Screening the articles by title, abstract, and full text, Quality assessment and data extraction, Analysis and interpretation of the data, Writing the manuscript, Making the figures and tables.
References
- 1. Standard SC. Treatment of coxa brevis. Orthop Clin North Am 2011;42:373-387, vii. [DOI] [PubMed] [Google Scholar]
- 2. Stevens PM, Coleman SS. Coxa breva: its pathogenesis and a rationale for its management. J Pediatr Orthop 1985;5:515-521. [PubMed] [Google Scholar]
- 3. Siffert RS. Patterns of deformity of the developing hip. Clin Orthop Relat Res 1981:14-29. [PubMed]
- 4. Elftman H. Biomechanics of muscle with particular application to studies of gait. J Bone Joint Surg [Am]. 1966;48:363-377. [PubMed] [Google Scholar]
- 5. Iwersen LJ, Kalen V, Eberle C. Relative trochanteric overgrowth after ischemic necrosis in congenital dislocation of the hip. J Pediatr Orthop 1989;9:381-385. [PubMed] [Google Scholar]
- 6. Murphy NJ, Eyles JP, Hunter DJ. Hip osteoarthritis: etiopathogenesis and implications for management. Adv Ther. 2016. November;33:1921-1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Morscher E. Intertrochanteric osteotomy in osteoarthritis of the hip. In: Riley L. ed, Proceedings of the eighth open scientific meeting of the Hip Society. Urbana, IL: Mosby, 1980. [Google Scholar]
- 8. Belzile ÉL. Morscher osteotomy. Pediatric pelvic and proximal femoral osteotomies. A case-based approach. Cham, Switzerland: Springer, 2018. [Google Scholar]
- 9. Lascombes P, Prevot J, Allouche A, Ligier JN, Metaizeau JP. Lengthening osteotomy of the femoral neck with transposition of the greater trochanter in acquired coxa vara. Rev Chir Orthop Repar Appar Mot 1985;71:599-601. [PubMed] [Google Scholar]
- 10. Placzek R, Gathen M, Koob S, Jacobs C, Ploeger MM. Modified neck-lengthening osteotomy after Morscher in children and adolescents. Oper Orthop Traumatol 2018;30:379-386. [DOI] [PubMed] [Google Scholar]
- 11. Libri R, Marchesini Reggiani L. A modified technique for reconstruction of the femoral neck in paediatric patients. Hip Int 2010;20:529-534. [DOI] [PubMed] [Google Scholar]
- 12. Lengsfeld M, Schuler P, Griss P. The long-term (8-12 years) results of valgus and lengthening osteotomy of the femoral neck. Arch Orthop Trauma Surg 2001;121:201-204. [DOI] [PubMed] [Google Scholar]
- 13. Covidence systematic review software[Internet]. Melbourne, Australia: Veritas Health Innovation; 2018. [cited 2020 Apr 24]. Available from: www.covidence.org
- 14. Black SR, Kwon MS, Cherkashin AM, Samchukov ML, Birch JG, Jo CH. Lengthening in congenital femoral deficiency a comparison of circular external fixation and a motorized intramedullary nail. J Bone Joint Surg [Am]. 2015;97:1432-1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dostál M, Ditmar R, Pach M. Initial experience with Morscher’s elongation osteotomy in coxa brevis. Acta Chir Orthop Traumatol Cech 1994;61:171-176. [PubMed] [Google Scholar]
- 16. Buess P, Morscher E. Osteotomy to lengthen the femoral neck with distal transfer of the greater trochanter in coxa vara after hip dislocation. Orthopade 1988;17:485-490. [PubMed] [Google Scholar]
- 17. Eidelman M, Keshet D, Nelson S, Bor N. Intermediate to long-term results of femoral neck lengthening (Morscher osteotomy). J Pediatr Orthop 2019;39:181-186. [DOI] [PubMed] [Google Scholar]
- 18. Hasler CC, Morscher EW. Femoral neck lengthening osteotomy after growth disturbance of the proximal femur. J Pediatr Orthop B 1999;8:271-275. [PubMed] [Google Scholar]
- 19. Hefti F, Morscher E. Die schenkelhalsverlängernde Osteotomie. Oper Orthop Traumatol 1989;1:170-178. [Google Scholar]
- 20. Weissinger M, Helmreich C, Keppel A. Reconstruction osteotomy by Morscher’s method in coxa vara. Acta Chir Orthop Traumatol Cech 1995;62:331-335. [PubMed] [Google Scholar]
- 21. Takata K, Maniwa S, Ochi M. Surgical treatment of high-standing greater trochanter. Arch Orthop Trauma Surg 1999;119:461-463. [DOI] [PubMed] [Google Scholar]
- 22. Croft P, Cooper C, Wickham C, Coggon D. Defining osteoarthritis of the hip for epidemiologic studies. Am J Epidemiol 1990;132:514-522. [DOI] [PubMed] [Google Scholar]
- 23. Gage JR, Cary JM. The effects of trochanteric epiphyseodesis on growth of the proximal end of the femur following necrosis of the capital femoral epiphysis. J Bone Joint Surg [Am] 1980. July;62:785-94. [PubMed] [Google Scholar]
- 24. Garcia FL, Picado CHF, Cardinali LP. Does trochanteric transfer eliminate the Trendelenburg sign in adults? Clin Orthop Relat Res 2011;469:1984-1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Teplenky M, Mekki W. Pertrochanteric osteotomy and distraction femoral neck lengthening for treatment of proximal hip ischemic deformities in children. J Child Orthop 2016;10:31-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Papavasiliou VA, Kirkos JM. Reconstruction of residual deformities of the hip. A new surgical option. Clin Orthop Relat Res 1997:123-127. [PubMed]
- 27. Schneidmueller D, Carstens C, Thomsen M. Surgical treatment of overgrowth of the greater trochanter in children and adolescents. J Pediatr Orthop 2006;26:486-490. [DOI] [PubMed] [Google Scholar]
- 28. Garrido IM, Moltó FJ, Lluch DB. Distal transfer of the greater trochanter in acquired coxa vara. Clinical and radiographic results. J Pediatr Orthop B 2003;12:38-43. [DOI] [PubMed] [Google Scholar]
- 29. Albers CE, Steppacher SD, Schwab JM, Tannast M, Siebenrock KA. Relative femoral neck lengthening improves pain and hip function in proximal femoral deformities with a high-riding trochanter. Clin Orthop Relat Res 2015;473:1378-1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Shore BJ, Novais EN, Millis MB, Kim YJ. Low early failure rates using a surgical dislocation approach in healed Legg-Calvé-Perthes disease pediatrics. Clin Orthop Relat Res 2012. September;470:2441-2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Anderson LA, Erickson JA, Severson EP, Peters CL. Sequelae of Perthes disease: treatment with surgical hip dislocation and relative femoral neck lengthening. J Pediatr Orthop 2010;30:758-766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg [Am] 1969;51:737-755. [PubMed] [Google Scholar]
- 33. Söderman P, Malchau H, Herberts P. Outcome of total hip replacement: a comparison of different measurement methods. Clin Orthop Relat Res 2001:163-172. [DOI] [PubMed]
- 34. Frihagen F, Grotle M, Madsen JE, Wyller TB, Mowinckel P, Nordsletten L. Outcome after femoral neck fractures: a comparison of Harris Hip Score, Eq-5d and Barthel Index. Injury 2008;39:1147-1156. [DOI] [PubMed] [Google Scholar]
- 35. Hoeksma HL, Van Den Ende CHM, Ronday HK, Heering A, Breedveld FC. Comparison of the responsiveness of the Harris Hip Score with generic measures for hip function in osteoarthritis of the hip. Ann Rheum Dis 2003;62:935-938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ugino FK, Righetti CM, Alves DPL, Guimarães RP, Honda EK, Ono NK. Evaluation of the reliability of the modified Merle d’Aubigné and Postel Method. Acta Ortop Bras 2012;20:213-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Joo SY, Lee KS, Koh IH, Park HW, Kim HW. Trochanteric advancement in patients with Legg-Calvé-Perthes disease does not improve pain or limp. Clin Orthop Relat Res 2008;466:927-934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Albers CE, Steppacher SD, Ganz R, Siebenrock KA, Tannast M. Joint-preserving surgery improves pain, range of motion, and abductor strength after Legg-Calvé-Perthes disease hip. Clin Orthop Relat Res. 2012;470:2450-2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Martin RCG II, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg 2002;235:803-813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Paley D. Normal Lower Limb Alignment and Joint Orientation. In: Principles of Deformity Correction. Berlin Heidelberg: Springer; 2002:1-18. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


