Abstract
Introduction
Endoscopy education in the US traditionally follows the apprenticeship model, in which educators often have little formal training in education, and the acquisition of procedural skills by trainees relies heavily on procedure volume and learning by doing. A growing appreciation of the need to formally educate endoscopy trainers has led to the development of mandatory training curricula in other countries, but the implementation of such courses in the US has been limited. This 1-hour workshop aimed to provide educators the rationale and skills to offer a more standardized approach to procedural training.
Methods
We implemented a 1-hour interactive workshop designed for both gastroenterology faculty and trainees. The four sections of the workshop focused on: (1) rationale for standardized approach, (2) verbal and physical preparation for training, (3) training using standardized language and avoidance of cognitive overload, and (4) providing feedback. Four interactive video cases followed by large-group discussion were included.
Results
A total of 13 gastroenterology faculty and trainees attended the workshop. Eight additional members of the gastroenterology faculty watched an online video of the workshop. Survey data revealed that the workshop was effective in helping faculty set goals with trainees (Mpre = 2.4, Mpost = 3.6), identify standardized language to use during endoscopy (Mpre = 3.1, Mpost = 3.8), and give feedback after sessions (Mpre = 3.4, Mpost = 4.1).
Discussion
A 1-hour lecture-based interactive workshop with video cases was an engaging and effective introduction to formal endoscopy education techniques. The format was easy to incorporate into faculty conferences and can help bridge the current gap in formal endoscopy faculty training.
Keywords: Physician, Gastroenterology, Clinical/Procedural Skills Training, Endoscopy, Procedural Training
Educational Objectives
By the end of this activity, faculty will be able to:
-
1.
Describe task deconstruction during endoscopy.
-
2.
Identify ways to optimize ergonomics during endoscopy.
-
3.
Facilitate goal setting with trainees before an endoscopy session.
-
4.
Utilize standardized language for verbal instruction during an endoscopy session.
-
5.
Identify sources of cognitive load during endoscopy training.
-
6.
Give specific and timely feedback to trainees after an endoscopy session.
Introduction
The traditional approach to teaching procedures such as colonoscopy and other endoscopic procedures is based on the apprenticeship model of “see one, do one” or learning by doing. This training model relies on sheer volume of exposure to procedural caseload, as opposed to any formally structured curricula or standardized approach to training grounded in educational theory. This model had been supported by the ACGME where gastroenterology fellows (trainees) were required to complete at least 140 colonoscopies at the end of fellowship as a marker of completion of training, a target volume now recognized to be insufficient for achieving competency in colonoscopy.1 In the current competency-based assessment era of medical training, we no longer deem a trainee competent to perform colonoscopy based solely on a threshold number of procedures performed. Similarly, we cannot assume an endoscopist is competent or properly equipped to teach colonoscopy based solely on endoscopy experience or number of procedures he or she has supervised.
While the apprenticeship model has stood the test of time, today's trainees face additional challenges. Trainees now often learn under multiple educators, and the absence of a standardized approach to procedural training can lead to inconsistencies that can prove confusing to novice trainees. Moreover, today's endoscopy units, including those in academic medical centers, are under significant pressure to maximize procedure volume and efficiency, which may compromise teaching endeavors. Advances in our understanding of factors such as cognitive load and its impact on learning provide opportunities for more effective teaching.2,3 Endoscopy educators need to be able to teach effectively and purposefully in order to optimize the trainee's learning experience, but the apprenticeship model lacks standardized teaching methods that educators could employ to address these challenges.
The Dreyfus model of skill acquisition describes the progression of learners through multiple stages of skill and proficiency, from novice to expertise.4,5 The beginning stages are characterized by analytical decision making based on strict rules and context. With experience, trainees develop more intuitive understanding of the task, which is the hallmark of the expert level. This educational theory has been applied to several realms of medical education including surgical training6 and the learning of clinical skills for doctors7 and nurses.8,9 We believe it is similarly applicable to endoscopy education. However, it is important to distinguish expertise in performing a skill from expertise in teaching someone else to perform that skill. For example, expert endoscopists—who have had an intuitive understanding of endoscopy for many years—may have difficulty translating this intuitive understanding to more explicit and analytical terms for trainees.
Therefore, in recent years there has been a growing appreciation of the need for endoscopy educators to be formally trained how to teach procedures utilizing such evidence-based educational principles. One survey found that 23% of gastroenterology fellowships do not have a formal endoscopy curriculum10 and both endoscopy educators and trainees have expressed desire for a standardized approach to endoscopy education.11
Reflecting this evolution in training approach, several formal train-the-trainer courses have been developed and implemented in the United Kingdom, Canada, Australia, and, to a lesser extent, the US. In fact, formal curricula for endoscopy education have demonstrated better procedural outcomes.12 While these courses are mandatory for adult endoscopy trainers in the United Kingdom, widespread participation in the US is hindered by limited course offerings and course size, as well as time, cost, and travel considerations.
In response, this workshop was developed to provide endoscopy educators the rationale and skills to offer a more standardized approach to endoscopy training using a 1-hour interactive lecture. This format allowed us to combine didactics with brief interactive exercises. Recognizing the challenges of integrating an educational workshop into the busy schedules of our faculty and trainees, this format was chosen in order to optimize the use of available time and space during normal working hours. As with previous MedEdPORTAL workshops regarding procedural training,13,14 our workshop provided structured frameworks for goal-setting and providing feedback. However, it also addressed key challenges specific to teaching endoscopy education, including deconstructing tasks, optimizing endoscopy suite ergonomics, using standardized language, and reducing cognitive load.3,15–17 A literature search demonstrated that there were no other similar learning modules available for reviewing these endoscopy-specific education concepts at time of submission. This workshop was designed to guide endoscopy teachers through basic teaching principles of endoscopy and would be an ideal session to be implemented among educators before new trainees start their gastroenterology fellowships.
Methods
This 1-hour workshop targeted both gastroenterology faculty (endoscopy educators) of various stages of clinical experience who practice endoscopy and were involved in endoscopy education, and gastroenterology fellows (trainees) who were being actively trained in endoscopy. Trainees were included so that they could learn the teaching approach the faculty would be implementing, as well as to provide their perspective. The workshop was especially aimed at those who had previously limited exposure to formal training in endoscopy education, so there was no expected prerequisite exposure to formalized endoscopy education techniques. The recommended audience size for this workshop was 10–20 participants.
This workshop was a collaboration between two gastroenterologists on staff—one fellowship program director and one advanced endoscopist—who functioned as directors of endoscopy education for trainees. This facilitator pairing provided complementary perspectives to allow for learner engagement. Future facilitators should be gastroenterologists with an interest in improving endoscopy education and those respected by the faculty to be expert endoscopy teachers. We split the workshop into didactic components interspersed with interactive components to maximize participant interaction. Before giving the presentation, we divided the parts of the workshop presentation amongst ourselves based on our expertise. We recommend that the facilitator with familiarity with educational goals of trainees focus on teaching the preparation and feedback stage, and the expert endoscopist focus on teaching the training stage of the presentation.
The workshop was broken down into four sections:
-
1.
Establishing the need and rationale for a standardized approach to endoscopy teaching.
-
2.
Preparation stage where goal-setting, ergonomics, and room setup were discussed.
-
3.
Training stage, including review of the standardized language to use during endoscopy, tools for successful deconstruction of tasks during endoscopy training, and discussion of strategies to avoid cognitive overload.
-
4.
Feedback stage with tips for providing effective feedback on the trainee's procedural performance as well as procedure documentation.
The workshop was designed to be completed in 1 hour, and facilitators should feel comfortable allowing for discussion along the way. An approximate timeline to complete the workshop in 1 hour was outlined in Appendix A and follows as such:
-
•
Introductory remarks and ice breaker questions: 5 minutes
-
•
Slides 1–13: 10 minutes
-
•
Slides 14–16 (including exercise 1): 5 minutes
-
•
Slides 17–25: 10 minutes
-
•
Slides 26–37 (including exercise 2): 10 minutes
-
•
Slides 38–44 (including exercise 3): 10 minutes
-
•
Slides 45–54 (including exercise 4): 10 minutes
The presentation included facilitator notes embedded within the slide deck (Appendix A) to help to further facilitate discussion. A facilitators guide (Appendix B) accompanied the slide deck to provide detailed discussion points for the cases presented in the slide deck. The session began with facilitators introducing themselves and presenting workshop objectives, then they took turns presenting the various slides.
Four different cases with supporting videos were embedded in the lecture including: (1) practicing a task deconstruction for polypectomy, (2) using consistent language to help a trainee navigate through the colon, (3) recognizing cognitive overload in the endoscopy suite, and (4) providing feedback for a polypectomy. After each case facilitators asked faculty to report how they would approach a teaching situation presented to them based on the videos. Facilitators encouraged faculty to discuss perceived challenges and next steps to incorporate some of the teaching methods into their daily endoscopy teaching sessions.
At the end of the workshop, facilitators used the summary slide to review the didactic learning points. A handout of these main learning points was also given to all attendees to emphasize the learning objectives (final slide of Appendix A). The facilitators also asked participants what they would incorporate into their own clinical practice.
Room Setup, Equipment, and Environment
The setting for this workshop was a large conference room that could accommodate the number of expected attendees (approximately 10–20 participants). The room was equipped with a traditional projector with projection screen, and a connection to a computer. A large presentation-sized smart TV that displayed the PowerPoint presentation would also work for the presentation.
Workshop Evaluation
To evaluate this workshop, we administered a retrospective pre/postsurvey (Appendix C) upon completion of the workshop. We developed the survey to assess perceived utility and intent to change the methods of endoscopy instruction by setting goals, using standardized language, providing specific feedback, recognizing potential sources of cognitive overload, deconstructing tasks, and reviewing endoscopy reports. We asked participants how often they incorporated and intended to incorporate the teaching techniques learned as part of the endoscopy teaching sessions. We also asked participants if they felt that the session provided them with strategies to improve their ability to teach endoscopy. Responses were provided on 5-point Likert scales (1 = never, 5 = always).
In order to compare responses to our survey questions, we used a series of sign tests, which were appropriate for examining differences between paired observations.
Results
The workshop was implemented at a gastroenterology grand rounds conference to an audience of five trainees and eight faculty. A videotaped version of the lecture was offered to the members of the gastroenterology section who were unable to attend the live presentation. Eight faculty watched the videotaped module. Sixteen out of 21 participants responded to the postworkshop survey. Although this session was intended to be delivered live, we also included in our evaluation the data from participants who watched the video as we did not see any statistically significant differences in method of delivery.
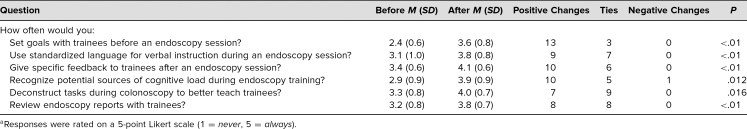
Based on the self-reported averages on a 5-point Likert scale (1 = never, 5 = always; Table), participants reported that after the workshop they would be more likely to apply all six of the formal educational behaviors taught in the workshop. Most notably, survey data revealed that the workshop was effective in helping faculty set goals with trainees (Mpre = 2.4, Mpost = 3.6), identify standardized language to use during endoscopy (Mpre = 3.1, Mpost = 3.8), and give feedback after sessions (Mpre = 3.4, Mpost = 4.1). Participants commented that the workshop was a “great initiative to teach us to be better teachers,” and noted that it was “easy to start with giving feedback on notes as a start.” A trainee who participated wrote, “Glad you included fellows—we should know what to expect.”
Table. Endoscopy Education Workshop Retrospective Pre/PostSurvey Responsesa (N = 16).
Discussion
The need for formal training in endoscopy education has led to the development of curricula for endoscopy educators in other countries. However, there are several barriers of cost, time, and accessibility to these courses that prevent many endoscopy educators in the US from participating. Our short, easily implementable and engaging workshop was effective in introducing important formal endoscopy education techniques to gastroenterology faculty, helping to bridge this gap in training.
Our workshop had several strengths in addressing the needs of endoscopy education. We specifically designed our learning objectives to address education concepts that have been identified as areas needing improvement for endoscopy.3,16–19 The 1-hour duration provided ample time for interactive elements, such as video cases and large-group discussion, while still being brief enough to be easily incorporated into educational conferences. We found that video cases and large-group discussions kept learners engaged. The target audience of 10–20 attendees was ideal for an audience of academic gastroenterologists. The workshop was also effective when delivered as a videotaped version. We also chose to have both trainees and faculty participate in the learning workshop and surveys because we felt that both the trainer and trainee should be aware of the goals of an endoscopy teaching session in order to be most effective. Indeed, the workshop received positive feedback from trainees as they gained an appreciation for the teaching methods they would expect during endoscopy sessions.
Our workshop was implemented for gastroenterology trainees and faculty at our own institution and our survey only assessed our own attendees. Although our workshop was positively received, we encountered challenges that could be relevant when adapting for other audiences. When discussing the topic of endoscopy training, we found a natural tendency to talk only about the actual endoscopy techniques and maneuvers we teach, rather than our teaching techniques. During the planning and implementation of this workshop, we learned the important lesson of keeping the focus of our content and discussion on how to teach, and not what to teach. Another challenge we encountered was overcoming the awkwardness of teaching the more senior and experienced faculty members how to teach. Because many of these senior faculty were themselves trained with the apprenticeship model, we wanted to stress the value of formal education training in endoscopy. However, all of these senior faculty had trained us during our fellowships. We made it clear to our audience at the outset that we did not purport to be experts in the field, and offered examples of our own teaching failures to break the ice.
Additionally, our workshop was co-led by the gastroenterology fellowship program director and an advanced endoscopist who functioned as director of endoscopy education for the trainees. Having an expert educator and an expert endoscopist lead the session helped to engage the audience and lent credibility. As the workshop is implemented at other institutions, we recommend that it should be facilitated by faculty with an interest in improving endoscopy education and those respected by fellow faculty to be expert endoscopy teachers. Finally, encouraging faculty who could not attend the live session to watch the session online was a challenge. We ultimately achieved viewership by sending multiple email reminders, and also via positive reviews from faculty who attended the live session. In future adaptations, efforts to encourage attendance at the live session will be important. Alternatively, the workshop could also be conducted through a live virtual conference to optimize attendance and participation. That such media are becoming increasingly common methods to deliver medical education serves as another strength of our workshop's format.
We acknowledge that our workshop/study had several limitations. As mentioned above, our workshop was only implemented at our own institution, which limits its generalizability. However, none of the material was specific to our institution or its practices. The 1-hour length and lecture-based format of the workshop was a strength as discussed above, but it was also a weakness. As would be expected, it was a challenge to try to condense a large amount of material into a short amount of time with a captive audience. The typical teach-the-teacher course offerings for endoscopy educators span 1 to 2 days, allowing for more exercises such as role-playing and practicing teaching techniques under direct observation. We obviously could not replicate that kind of experience, but believe our approach is readily reproducible and can be easily implemented by other programs with similar time and space constraints. If our workshop promotes further interest in formal education training, future iterations could include video cases showcasing examples of good and bad feedback and examples of poor ergonomics. Such additions reinforced our teaching techniques while remaining time efficient. We did not include these in this version of our workshop in favor of keeping the workshop within the 1-hour time constraint.
Our survey intended to assess the attitudes of our faculty towards incorporating these teaching techniques into their endoscopy sessions, but other studies beyond the scope of survey data are needed to answer whether the workshop translated into practical improvements in the educational quality of endoscopy sessions. Our retrospective pre/postsurvey also asked about prior and current behavior in one questionnaire, rather than conducting separate pre- and postworkshop surveys. Although this was done to reduce the burden on the participating attendees, we acknowledge that this is a limitation from a research perspective. Further, we acknowledge that asking participants about their future intended behavior immediately after participating in a session which lays out the importance of this behavior is not ideal. However, we were unable to conduct long-term follow-up or observation with participants. As such, we looked at intent to change behavior as at least a preliminary indicator of actual behavioral change. Future materials developed on this topic should include a long-term follow up to see the extent to which plans to implement behavior corresponds to actual behavior change.
In conclusion, our workshop was effective in introducing important formal education concepts such as standardized language, task deconstruction, and cognitive load, as well as emphasizing the importance of preendoscopy session goal setting and postendoscopy session feedback. We believe that this workshop can be easily implemented at other academic gastroenterology training programs and can serve as a way to develop standards and structure to endoscopy education.
Appendices
- Lecture PowerPoint.pptx
- Facilitators Guide.docx
- Evaluation Forms.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Disclosures
None to report.
Funding/Support
None to report.
Ethical Approval
Reported as not applicable.
References
- 1.Spier BJ, Benson M, Pfau PR, Nelligan G, Lucey MR, Gaumnitz EA. Colonoscopy training in gastroenterology fellowships: determining competence. Gastrointest Endosc. 2010;71(2):319–324. 10.1016/j.gie.2009.05.012 [DOI] [PubMed] [Google Scholar]
- 2.Sewell JL, Boscardin CK, Young JQ, Ten Cate O, O'Sullivan PS. Learner, patient, and supervisor features are associated with different types of cognitive load during procedural skills training: implications for teaching and instructional design. Acad Med. 2017;92(11):1622–1631. 10.1097/acm.0000000000001690 [DOI] [PubMed] [Google Scholar]
- 3.Sewell JL, Young JQ, Boscardin CK, Ten Cate O, O'Sullivan PS. Trainee perception of cognitive load during observed faculty staff teaching of procedural skills. Med Educ. 2019;53(9):925–940. 10.1111/medu.13914 [DOI] [PubMed] [Google Scholar]
- 4.Dreyfus SE, Dreyfus HL. A five-stage model of the mental activities involved in directed skill acquisition. Distribution. 1980:22. [Google Scholar]
- 5.Dreyfus SE. The five-stage model of adult skill acquisition. Bulletin Sci Tech Society. 2004;24:177–181. 10.1177/0270467604264992 [DOI] [Google Scholar]
- 6.Sadideen H, Plonczak A, Saadeddin M, Kneebone R. How educational theory can inform the training and practice of plastic surgeons. Plast Reconstr Surg Glob Open. 2018;6(12):e2042 10.1097/gox.0000000000002042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carraccio CL, Benson BJ, Nixon LJ, Derstine PL. From the educational bench to the clinical bedside: translating the Dreyfus developmental model to the learning of clinical skills. Acad Med. 2008;83(8):761–767. 10.1097/acm.0b013e31817eb632 [DOI] [PubMed] [Google Scholar]
- 8.Benner P, Tanner C, Chesla C. From beginner to expert: gaining a differentiated clinical world in critical care nursing. ANS Adv Nurs Sci. 1992;14(3):13–28. 10.1097/00012272-199203000-00005 [DOI] [PubMed] [Google Scholar]
- 9.Benner P. Using the Dreyfus model of skill acquisition to describe and interpret skill acquisition and clinical judgment in nursing practice and education. Bulletin Sci Tech Society. 2004;24(3):188–199. 10.1177/0270467604265061 [DOI] [Google Scholar]
- 10.Patel SG, Keswani R, Elta G, et al. Status of competency-based medical education in endoscopy training: a nationwide survey of US ACGME-accredited gastroenterology training programs. Am J Gastroenterol. 2015;110(7):956–962. 10.1038/ajg.2015.24 [DOI] [PubMed] [Google Scholar]
- 11.Zanchetti DJ, Schueler SA, Jacobson BC, Lowe RC. Effective teaching of endoscopy: a qualitative study of the perceptions of gastroenterology fellows and attending gastroenterologists. Gastroenterol Rep (Oxf). 2016;4(2):125–130. 10.1093/gastro/gow003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Waschke KA, Anderson J, Macintosh D, Valori RM. Training the gastrointestinal endoscopy trainer. Best Pract Res Clin Gastroenterol. 2016;30(3):409–419. 10.1016/j.bpg.2016.05.001 [DOI] [PubMed] [Google Scholar]
- 13.Patton K, Morris A, Kross E, Çoruh B, Carlbom D, Thronson LR. Teaching to teach procedures: a simulation-based curriculum for senior residents or fellows. MedEdPORTAL. 2015;11:9997 10.15766/mep_2374-8265.9997 [DOI] [Google Scholar]
- 14.Smyth P, Jeerakathil T, Roberts T. Lumbar puncture teaching skills objective structured clinical examination (OSCE) station. MedEdPORTAL. 2014;10:9800 10.15766/mep_2374-8265.9800 [DOI] [Google Scholar]
- 15.Pourmand K, Sewell JL, Shah BJ. What makes a good endoscopic teacher: a qualitative analysis. J Surg Educ. 2018;75(5):1195–1199. 10.1016/j.jsurg.2018.02.016 [DOI] [PubMed] [Google Scholar]
- 16.Singla M, Kwok RM, Deriban G, Young PE. Training the endo-athlete: an update in ergonomics in endoscopy. Clin Gastroenterol Hepatol. 2018;16(7):1003–1006. 10.1016/j.cgh.2018.04.019 [DOI] [PubMed] [Google Scholar]
- 17.Dilly CK, Sewell JL. How to give feedback during endoscopy training. Gastroenterol. 2017;153(3):632–636. 10.1053/j.gastro.2017.07.023 [DOI] [PubMed] [Google Scholar]
- 18.Coderre S, Anderson J, Rostom A, McLaughlin K. Training the endoscopy trainer: from general principles to specific concepts. Can J Gastroenterol. 2010;24(12):700–704. 10.1155/2010/493578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kumar NL, Smith BN, Lee LS, Sewell JL. Best practices in teaching endoscopy based on a delphi survey of gastroenterology program directors and experts in endoscopy education. Clin Gastroenterol Hepatol. 2020;18(3):574–579.e1. 10.1016/j.cgh.2019.05.023 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- Lecture PowerPoint.pptx
- Facilitators Guide.docx
- Evaluation Forms.docx
All appendices are peer reviewed as integral parts of the Original Publication.