ABSTRACT
Disease burden and lifestyle patterns have changed rapidly worldwide, especially in some Asian countries over the past 2 decades. However, cross-country comparative research is limited. This study investigated the nutritional status of preschool children and childbearing women in China, India, Nepal, and Pakistan selected based on their socioeconomic status, population size, and urbanization. Nationally representative data were used from the China National Nutrition and Health Surveillance Report, India National Family Health Survey, Nepal Demographic and Health Survey, Pakistan Demographic and Health Survey, the WHO repository, and the World Bank. The prevalence of underweight, overweight, and obesity and some ratios were compared. These rates varied across these 4 countries and were associated with their economic development levels. China's economic status and prevalence of childhood overweight/obesity (11.5%) were highest; India's economic status was higher than that of Nepal and Pakistan, but had higher rates of stunting, wasting, and underweight (38.4%, 21.0%, and 35.7%, respectively) in preschool children. Pakistan had the highest prevalence of overweight/obesity among childbearing women (52.4% in all, 63.0% in urban areas). Nepal had the lowest economic status and overweight/obesity rate in preschool children (1.2%). In general, the prevalence of overweight/obesity was higher in urban than in rural areas, except among childbearing women in China. Nutritional status and health burden are heavily influenced by economic development. The double burden of malnutrition poses prioritization challenges for policymakers and public health efforts. Prevention of obesity is urgently needed, at least in higher-income countries in Asia.
Keywords: Asia, malnutrition, obesity, overweight, socioeconomic status
Overweight/obesity rates are different and have been increasing in China, India, Nepal, and Pakistan; and countries with better social economic development levels and higher family income have higher rates.
Introduction
It is important to address the shifts in disease burden and the burden of malnutrition in developing countries (1–3). The World Health Organization (WHO) defines the double burden of malnutrition as the coexistence of undernutrition and obesity, which has become a major public health concern worldwide (4, 5). Globally, the magnitude of undernutrition is declining along with an escalating prevalence of obesity in many countries (6). Tzioumis et al. examined the prevalence and trends in childhood of the dual burden of malnutrition in low- and middle-income countries (LMICs), and indicated that the prevalence of overweight/obesity in many Asian countries would continue to increase despite the high prevalence of hunger and undernutrition (7).
A recent study comprehensively examined the trends of body mass index (BMI) in countries worldwide, and reported that overweight/obesity rates in rural areas might soon match, if not exceed, those in urban areas. Rural hunger, wasting, and stunting are rapidly being replaced by overweight/obesity in most regions of the world except sub-Saharan Africa, South Asia, and a small number of countries in other areas (8). For example, in Nepal, overweight/obesity are occurring among people living in rural areas, having low income and/or educational levels, although the prevalence is higher among their urban, wealthier, or more educated counterparts (9). However, in some Asian countries with different levels of economic development, the double burden of the malnutrition epidemic has not been extensively examined.
Some Southeast Asian countries are suffering from high levels of the double burden of malnutrition, i.e. obesity coexisting with undernutrition (including energy intake and macro- and micronutrient deficiencies). A recent compilation of indicators across South Asian countries showed that several forms of undernutrition, such as stunting, underweight, wasting, and low birth weight, are commonly observed in the member states of the WHO in its Southeast Asia region. It also showed a declining prevalence of these problems among children and women over the past 2 decades; however, overweight/obesity is emerging as a new concern (10). Although nutrition transition is observed globally, the shifts in dietary and physical activity patterns in some LMICs have been shown to occur more rapidly than in high-income countries (11).
Factors such as changes in lifestyles and food environment, marketing of unhealthy foods and beverages, rapid urbanization, and reduction in physical activity have been shown to be major drivers of the global obesity epidemic (12). Most in-depth studies are mainly conducted in high-income countries, such as the USA and European countries (12, 13), and more research is needed in LMICs (12). To our knowledge, there are no studies that have compared the double burden of malnutrition in Asian countries with great differences in socioeconomic status.
This study aimed to compare the prevalence and shifts of under- and overnutrition levels among preschool children and childbearing women (who are more vulnerable than other groups) in 4 selected developing countries in Asia (China, India, Nepal, and Pakistan). Their total population accounts for 39.3% of the world's population. They have different levels of socioeconomic development, are under social transitions, and have great diversity in population attributes, culture, religions, and food consumption patterns (Figure 1).
FIGURE 1.
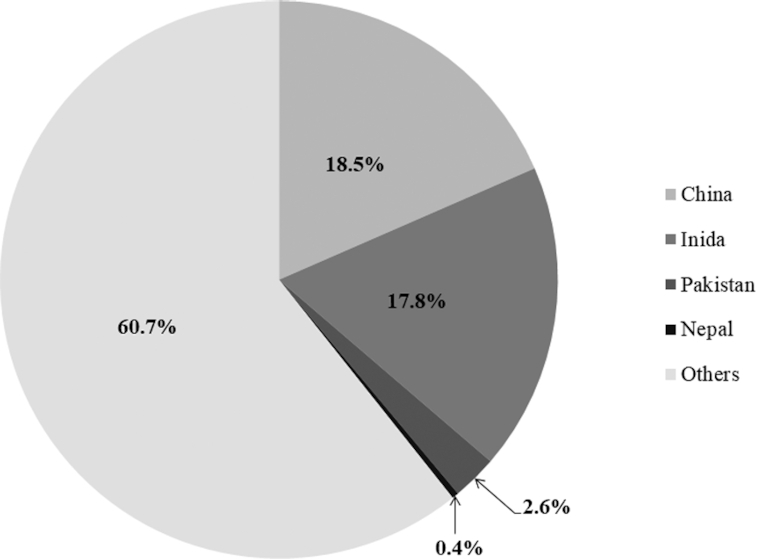
China, India, Pakistan, and Nepal accounted for 39.3% of the global population of 7.5 billion in 2017. (Values are percentage.)
Methods
Literature search strategies
We reviewed and analyzed existing national survey reports and published data from the 4 selected countries covering the past 15 y. We searched various websites of nationally representative surveys for the 4 selected countries, e.g. the China Nutrition and Health Surveillance and Demographic and Health Survey. In addition, in order to obtain information on risk factors for obesity, we searched the websites of the FAO of the UN, the WHO, and the World Bank for related data. Titles and abstracts of relevant reports or studies were examined and the full text was obtained for those fulfilling the inclusion criteria.
Inclusion criteria
Survey reports and original studies in English that provided data on the prevalence of over- or undernutrition in these 4 countries were examined. The inclusion criteria were: 1) data were collected from nationally representative surveys; 2) anthropometric variables such as weight, height, and BMI were measured, and the prevalence of overnutrition (overweight/obesity) and undernutrition (underweight, stunting, and wasting) were reported; 3) established cut-points of BMI were used to classify weight status; 4) data were collected over the past 15 y; and 5) the participants were preschool children or childbearing women. Finally, 5 recently available nutrition-related nationally representative survey reports from the 4 selected countries met the inclusion criteria and were used for analysis, i.e. the China National Nutrition and Health Surveillance Report (2010–2013) (14), the Report on Nutrition and Chronic Disease Status of Chinese Residents (2015) (15), the Indian National Family Health Survey (2015–16) (16), the Nepal Demographic and Health Survey (2016) (17), and the Pakistan Demographic and Health Survey (2017–2018) (18). Please see table 2 and 3's footnote 1.
Classification of over-and undernutrition status
In the published articles and reports, different definitions of overweight/obesity have been used in the 4 countries for preschool children and childbearing women, and there were changes in the practice over time.
For preschool children, in recent years, the 4 countries adopted a weight-for-height Z-score > +2 SD to define overweight for children aged under 5 y, whereas a BMI Z-score > +1 SD was used for Chinese children aged 5 y (19). There were consistent definitions of undernutrition in the 4 countries: stunting (height-for-age, Z score < −2SD), wasting (weight-for-height, Z score < −2 SD), and underweight (weight-for-age, Z score < −2 SD) for children aged ≤5 y (19, 20). Please see table 2's footnote 2 and 3.
For women aged 15–49 y in India, Nepal, and Pakistan, overweight/obesity were defined as BMI 25.0–29.9 and BMI ≥30.0 kg/m2, respectively. For Chinese women aged 15–17 y, the standard recommended by the Working Group on Obesity in China was used (22) and BMI cut-points of ≥24 and ≥28 were used for women aged 18–49 y (23) Please see table 3's footnote 2 and 3.
Measures of risk factors
Information on economics, demographics, and food production of the 4 countries was collected from multiple sources including the World Bank, World Development Indicators, the FAO of the UN, Food Balance Sheets, and the WHO. In addition, information on household socioeconomic status and individual demographic characteristics was extracted from the survey reports.
Statistical analysis
To examine the shifts from under- to overnutrition and to facilitate comparisons across the 4 countries, we calculated the overweight- and obesity-to-underweight ratios, which used the combined overweight/obesity prevalence against the prevalence of underweight in each country. We also calculated the ratios by rural/urban residence and by gender.
Results
Characteristics of the 4 countries
China had the highest per capita income, which was 10 times that of Nepal, 6 times that of Pakistan, and 4.5 times that of India. In addition, China's life expectancy was the highest (76.5 y), followed by Nepal (70.2 y), India (68.2 y), and Pakistan (66.9 y). Under 5-y mortality had a similar pattern, but in the reverse order, i.e. China had the lowest rate, followed by Nepal, India, and Pakistan. China also had the largest proportion of urban population. The availability of domestically produced food was highest in India (Table 1).
TABLE 1.
Economic and demographic characteristics of 4 selected countries in Asia: China, India, Pakistan, and Nepal1
| Country | Income level | GDP per capita (US $) | Life expectancy (y) | Under-5 mortality | Population (thousand) | Urban population (%) | Food Production Index2 |
|---|---|---|---|---|---|---|---|
| China | Upper-middle | 8827.0 | 76.5 | 9.2 | 1386,395.0 | 58.0 | 139.0 |
| India | Lower-middle | 1942.1 | 68.2 | 38.7 | 1339,180.1 | 33.6 | 144.4 |
| Pakistan | Lower-middle | 1547.9 | 66.9 | 71.5 | 197,016.0 | 36.4 | 130.4 |
| Nepal | Low | 849.0 | 70.2 | 33.4 | 29,305.0 | 19.3 | 137.8 |
GDP, gross domestic product; data source: World Development Indicators, World Bank (2017) (21).
The World Bank's Food Production Index is determined on the basis of volumes of animal or plant-based agricultural products, but does not consider seeds, feed, tea, and coffee.
Prevalence of undernutrition, overweight/obesity among preschool children
Undernutrition was least prevalent in China (wasting = 2.0%, underweight = 2.5%), with higher prevalence in Pakistan (wasting = 7.0%, underweight = 23.0%), Nepal (wasting = 9.7%, underweight = 27.0%), and India (wasting = 21.0%, underweight = 35.7%). Stunting was highly prevalent in all countries except China, with slightly over one-third of children being affected. However, the rural/urban difference was higher in China and almost negligible in the other 3 countries.
As opposed to undernutrition, overweight/obesity was more common among preschool children in China (11.5%), followed by Pakistan (2.5%), India (2.1%), and Nepal (1.2%). There was a marked boys-girls difference in prevalence among Chinese children, with boys having a higher prevalence than girls. However, this was not the case in the other 3 countries. For the urban/rural difference in the prevalence of childhood overweight/obesity, it was more common in urban compared with rural areas in all countries except China.
Overall, China had the highest overweight- and obesity-to-underweight ratio (4.60), whereas the ratio in Nepal (0.04) was the lowest (Table 2).
TABLE 2.
Prevalence (%) of under- and overnutrition among children in 4 selected countries in Asia, and the urban/rural and gender differences
| Country | Stunting2 (%) | Wasting2 (%) | Underweight2 (%) | Overweight/obesity2,3 (%) | Overweight/obesity to underweight ratio | |
|---|---|---|---|---|---|---|
| China1 | All | 8.1 | 2.0 | 2.5 | 11.5 | 4.60 |
| (2010–2013) | Rural | 11.3 | 2.4 | 3.2 | 11.7 | 3.65 |
| (14) | Urban | 4.2 | 1.5 | 1.7 | 11.3 | 6.65 |
| Rural/urban ratio | 2.7 | 1.6 | 1.8 | 1.0 | ||
| Boy | 8.7 | 2.0 | 2.6 | 13.0 | 5.00 | |
| Girl | 7.4 | 2.0 | 2.4 | 9.7 | 4.04 | |
| Boy/girl ratio | 1.2 | 1.0 | 1.1 | 1.3 | ||
| India1 | All | 38.4 | 21.0 | 35.7 | 2.1 | 0.06 |
| (2015–2016) | Rural | 41.2 | 21.4 | 38.3 | 1.8 | 0.05 |
| (16) | Urban | 31.0 | 20.0 | 29.1 | 2.8 | 0.10 |
| Rural/urban ratio | 1.3 | 1.1 | 1.3 | 0.6 | ||
| Boy | 38.9 | 21.9 | 36.1 | 2.1 | 0.06 | |
| Girl | 37.9 | 20.1 | 35.3 | 2.1 | 0.06 | |
| Boy/girl ratio | 1.0 | 1.1 | 1.0 | 1.0 | ||
| Nepal1 | All | 35.8 | 9.7 | 27.0 | 1.2 | 0.04 |
| (2016) | Rural | 40.2 | 10.2 | 31.1 | 0.9 | 0.03 |
| (17) | Urban | 32.0 | 9.2 | 23.4 | 1.5 | 0.06 |
| Rural/urban ratio | 1.3 | 1.1 | 1.3 | 0.6 | ||
| Boy | 36.0 | 9.5 | 26.7 | 1.4 | 0.05 | |
| Girl | 35.7 | 9.8 | 27.4 | 1.0 | 0.04 | |
| Boy/girl ratio | 1.0 | 1.0 | 1.0 | 1.4 | ||
| Pakistan1 | All | 37.6 | 7.0 | 23.0 | 2.5 | 0.11 |
| (2017–2018) | Rural | 41.0 | 7.3 | 19.0 | 2.2 | 0.12 |
| (18) | Urban | 31.0 | 6.7 | 25.0 | 3.0 | 0.12 |
| Rural/urban ratio | 1.3 | 1.1 | 0.8 | 0.7 | ||
| Boy | 38.0 | 7.6 | 24.0 | 2.3 | 0.10 | |
| Girl | 37.0 | 6.6 | 22.0 | 2.6 | 0.12 | |
| Boy/girl ratio | 1.0 | 1.2 | 1.1 | 0.9 |
Data sources: China National Nutrition and Health Surveillance Report (2010–2013): data was from the China Nutrition and Health Surveillance 0–5 Years Old Children and Lactating Women project in 2013 (14). Report on Nutrition and Chronic Disease Status of Chinese Residents (2015): data was from the Chinese Center for Disease Control and Prevention, the National Center for Cardiovascular Disease, and the National Cancer Center (15). India National Family Health Survey (NFHS-4) (2015–2016): data was from a large-scale, multiround survey conducted in a representative sample of households throughout India (16). Nepal Demographic and Health Survey (2016): data was from a nationally representative study implemented by New ERA under the aegis of the Ministry of Health of Nepal (17). Pakistan Demographic and Health Survey (2017–2018): data was from a nationally representative study implemented by the National Institute of Population Studies (NIPS) under the aegis of the Ministry of National Health Services, Regulations and Coordination, Islamabad, Pakistan (18). The data in the 2 Chinese reports came from 2010–2015.
For children aged under 5 y in 4 countries: stunting: height-for-age < -2 SD; wasting: weight-for-height <-2 SD; underweight: weight-for-age <-2 SD, overweight/obesity: weight-for-height Z-score > +2 SD (19, 20).
For children aged 5 y in China: overweight: BMI Z-score > +1 SD (19).
Prevalence of overweight/obesity among childbearing women
In all countries, the prevalence of overweight/obesity among women was much higher than in children. The prevalence was highest in Pakistan (52.4% for women and 2.5% for children), followed by China (34.6% for women and 11.5% for children). The prevalence was much lower in Nepal (22.2% for women and 1.2% for children) and India (20.6% for women and 2.1% for children). A marked difference in the prevalence of overweight/obesity between rural and urban women was observed in all countries except China. The highest ratio was recorded for Pakistan (0.7), followed by Nepal (0.6) and India (0.5) (Table 3).
TABLE 3.
Prevalence (%) of overweight/obesity among women of childbearing age (15–49 y) in 4 selected countries in Asia
| Country | Overweight2,3 (%) | Obesity2,3 (%) | Overweight/obesity2,3 (%) | |
|---|---|---|---|---|
| China1 | All | 25.4 | 9.2 | 34.6 |
| (2012–2013) | Rural | 25.3 | 9.0 | 34.3 |
| (15) | Urban | 25.5 | 9.4 | 34.9 |
| Rural/urban ratio | 1.0 | 1.0 | 1.0 | |
| India1 | All | 15.5 | 5.1 | 20.6 |
| (2015–2016) | Rural | 12.0 | 3.1 | 15.1 |
| (16) | Urban | 22.2 | 9.1 | 31.3 |
| Rural/urban ratio | 0.5 | 0.3 | 0.5 | |
| Nepal1 | All | 17.1 | 5.1 | 22.2 |
| (2016) | Rural | 13.4 | 2.0 | 15.4 |
| (17) | Urban | 19.2 | 6.8 | 26.0 |
| Rural/urban ratio | 0.7 | 0.3 | 0.6 | |
| Pakistan1 | All | 30.4 | 22.0 | 52.4 |
| (2017–2018) | Rural | 25.7 | 19.5 | 45.2 |
| (18) | Urban | 37.7 | 25.3 | 63.0 |
| Rural/urban ratio | 0.7 | 0.8 | 0.7 |
Data sources: China National Nutrition and Health Surveillance Report (2010–2013): data was from the China Nutrition and Health Surveillance 0–5 Years Old Children and Lactating Women project in 2013 (14). Report on Nutrition and Chronic Disease Status of Chinese Residents (2015): data was from the Chinese Center for Disease Control and Prevention, the National Center for Cardiovascular Disease, and the National Cancer Center (15). India National Family Health Survey (NFHS-4) (2015–2016): data was from a large-scale, multiround survey conducted in a representative sample of households throughout India (16). Nepal Demographic and Health Survey (2016): data was from a nationally representative study implemented by New ERA under the aegis of the Ministry of Health of Nepal (17). Pakistan Demographic and Health Survey (2017–2018): data was from a nationally representative study implemented by the National Institute of Population Studies (NIPS) under the aegis of the Ministry of National Health Services, Regulations and Coordination, Islamabad, Pakistan (18). The data in the 2 Chinese reports came from 2010–2013.
For women aged 15–49 y in India, Nepal, and Pakistan: overweight: BMI 25.0–29.9, obesity: BMI ≥30.0.
Selected obesity-related risk factors
Between 2000 and 2013, the gross availability of food items increased substantially in all 4 countries. Per capita energy supply increased almost uniformly across all countries, with China having the highest value. The availability of grains increased by nearly 50% in China and 20–30% in the other 3 countries. Meat availability increased most in Pakistan, followed by Nepal, China, and India. Domestic production of vegetables and fruits almost doubled in Nepal, India, and China, but there was little change in Pakistan. In 2016, more than one-third of adults did not engage in sufficient physical activity (as per WHO recommendations) in India and Pakistan, whereas in Nepal and China the prevalence of sufficient physical activity was just over one-tenth of that in India and Pakistan (24) (Table 4).
TABLE 4.
Time trends in recent years in selected obesity-related risk factors of 4 selected countries in Asia
| Per capita total energy supply per day1 | Grains (1000 tons)1 | Meats1 | Vegetables and fruits1 | Prevalence of inadequate physical activity2 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Country | Income level | 2000 | 2013 | 2000 | 2013 | 2000 | 2013 | 2000 | 2013 | 2016 |
| China | Upper-middle | 2814 | 3108 | 344,128 | 486,280 | 57,965 | 85,180 | 426,550 | 737,692 | 14.1 |
| India | Lower-middle | 2380 | 2459 | 192,485 | 240,926 | 4444 | 6215 | 115,284 | 203,647 | 34.0 |
| Nepal | Low | 2257 | 2673 | 5712 | 7080 | 237 | 347 | 2350 | 5139 | 13.4 |
| Pakistan | Lower-middle | 2398 | 2440 | 28,062 | 36,012 | 1701 | 3040 | 10,047 | 11,093 | 33.7 |
Data source: FAO of the UN (42). The figures represent amounts produced domestically.
The values indicate age-standardized estimate for adults aged ≥18 y; inadequate physical activity is defined as a population attaining <150 min of moderate-intensity physical activity per week, or <75 min of vigorous-intensity physical activity per week, or equivalent, according to recommendation of WHO (24).
Discussion
Based on findings from nationally representative surveys in China, India, Nepal, and Pakistan, we compared the prevalence of undernutrition, overweight, and obesity among preschool children and childbearing women in conjunction with selected socioeconomic indicators at the country level. There were large disparities in the nutritional status among the populations of children and women across the 4 countries. Generally, countries with higher economic status had a lower prevalence of undernutrition and a higher prevalence of overweight/obesity in children, most notably in China (with the highest income level among the 4 countries), where the prevalence of overweight/obesity was much higher than that of underweight. The patterns in these health outcomes in childbearing women were mixed. Pakistan had the highest prevalence of overweight/obesity in this group among the 4 countries although it has the second lowest income level. This might have resulted from sociocultural norms that affect obesity risk factors like eating and physical activity behaviors (25, 26). Most of the women, especially those living in urban areas, stay at home and may not have good access to open spaces for exercise. For example, public parks and gymnasiums are not as common in Pakistan as in China.
Some large rural-urban differences in the prevalence of these outcomes were found in both preschool children and childbearing women. Stunting in preschool children was more prevalent in rural areas than in urban areas. Gender differences in the prevalence of overweight/obesity and underweight were not observed in preschool children.
Overall, overweight/obesity in preschool children and childbearing women occurred more frequently in countries with higher income per capita than in those with lower income. This is consistent with existing evidence that obesity is associated with higher income (27). However, overweight/obesity was more prevalent in children in Pakistan than in India, although the country had a lower level of economic development.
The differences between Pakistan and India may be due to differences in their food supply and physical activity. Between 2000 and 2013, the production of grains and meats increased more rapidly in Pakistan than in India. In contrast, the production of vegetables and fruits increased faster in India than in Pakistan. The consumption of carbohydrates and meats are positively associated with obesity (28–30).
Overall, the prevalence of overweight/obesity was higher in urban than in rural populations, except among childbearing women in China (where there was little difference). This is possibly because urban people are more likely to be exposed to obesogenic factors (e.g. foods with higher energy density and a more sedentary lifestyle) than rural dwellers (31–34). Interestingly, in China, the prevalence was similar in childbearing women in urban and rural areas, according to recent national data. Recent research conducted in Kenya similarly showed that after adjusting for wealth there was no significant difference in obesity prevalence between people living in rural areas and those who had migrated to cities (35).
Small gender differences in nutritional outcomes were observed among preschool children in this study. In China, the prevalence of overweight/obesity among school-age boys was higher than that in school-age girls, whereas in Nepal, the prevalence of overweight/obesity in girls was higher than in boys. This might be due to environmental and cultural influences; for instance, Chinese parents and grandparents still have a stereotypical image of ideal children: chubby boys and slim girls (36). We did not compare the prevalence of overweight/obesity between women and men in this study, but findings from another study showed that in 105 countries, overall, the prevalence of overweight/obesity was higher in women than in men (37). Most of these studies point toward culture as a factor, such as when a larger body size in women is considered more desirable in some African communities than a more normal body size (38, 39). Indeed, 1 study in Morocco showed intentional strategies for weight gain in women including consumption of appetite enhancers and excessive food along with a reduction in physical activity (40).
The UN Sustainable Development Goals (SDGs) called on countries to develop policies that deal with issues of poverty, hunger, and health. The first 3 SDGs are: 1) no poverty, 2) zero hunger, and 3) good health and well-being (41). Although these goals are related to managing malnutrition, they are more focused on undernutrition and infectious diseases. Thus, they may not be adequate for preventing obesity and other noncommunicable chronic diseases. Unfortunately, many health-related policies in some Asian countries continue to emphasize reducing undernutrition and infectious diseases but are not adequate in fighting the rapidly increasing chronic diseases and obesity.
There are limited policies that have been established to focus on the prevention and control of obesity in these 4 countries, which have yet to be evaluated for their effectiveness. Among these 4 countries overall, China has the worst obesity problem and has more policies and intervention efforts related to this issue. However, they have been inadequate in controlling the rapid increase in overweight/obesity over the past 2 decades. In China, there is a lack of prevention and control efforts for key factors related to obesogenic environments. There is also a need to consider genetic and psychological factors in developing policies and programs to fight the obesity epidemic (43, 44). Approximately 300 studies have reported that nearly 100 candidate genes are associated with obesity-related traits. Among them, FTO and MC4R have the best repeatability in different ethnic groups. Europeans and East Asians share >50% of BMI-related single nucleotide polymorphisms (45, 46). Consciously perceived psychosocial stress was found to be a main factor to disturb health and promote unhealthy cognitive patterns, which may affect eating and physical activity behaviors (47).
A major strength of the study is that the 4 countries are located in 3 WHO regions, namely Western Pacific, Eastern Mediterranean, and Southeast Asia. Together, they represent a large proportion of the world's population and cover a wide diversity in terms of socioeconomic characteristics. This study also has some limitations. First, we compared the prevalence of overweight/obesity across countries and over time, and the data obtained from China were earlier than those from the other 3 countries. Second, it has been recommended that BMI cut-points <25 and 30 should be used to classify overweight and obesity in some Asian populations, respectively. For example, BMI cut-points of 24 and 28 as well as 23 and 25 are used to define overweight and obesity in China and Korea, respectively. Similarly, Japanese adults with BMI ≥25 are considered obese (48–51); however, the reported overweight and obesity rates in India, Nepal, and Pakistan are mainly based on BMI cut-points of 25 and 30, which limits an appropriate comparison across countries. This has caused the prevalence in these countries to be underestimated. Future research needs to use appropriate BMI cut-points to classify overweight and obesity in these countries.
In conclusion, the available national data showed that the prevalence of overweight/obesity has been increasing in these 4 Asian countries, whereas the prevalence of undernutrition has been declining. National economic development, changes in the food supply, urbanization, and lack of adequate physical activity are positively associated with increasing overweight/obesity. These factors must be considered when formulating and implementing national policies and programs to fight obesity. Countries with a high prevalence of overweight/obesity like China, India, and Pakistan need to take timely and effective actions to fight the epidemic, whereas Nepal, where the overweight/obesity prevalence remains low, needs to take action to prevent this epidemic.
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows––YW: designed the research; LG, AB, and PA: performed the literature search; AB, LG, PA, JW, and LW: drafted the manuscript; LG and YW: had primary responsibility for the final content and are the guarantors; all authors provided relevant intellectual input, revised the manuscript, and read and approved the final manuscript.
Notes
This research was funded in part by research grants from the China Medical Board (16-262), the UN International Children's Emergency Fund (2018-Nutrition-2.1.2.3), and the US NIH (U54 HD070725).
Author disclosures: The authors report no conflicts of interest.
LG and AB contributed equally to this work.
Abbreviations used: LMIC, low- and middle-income country; SDG, The UN Sustainable Development Goal.
Contributor Information
Liwang Gao, Global Health Institute, School of Public Health, Xi'an Jiaotong University Health Science Center, Xi'an, Shaanxi, China.
Ashok Bhurtyal, Global Health Institute, School of Public Health, Xi'an Jiaotong University Health Science Center, Xi'an, Shaanxi, China; Nepal Public Health Foundation, Kathmandu, Nepal; Central Department of Public Health, Institute of Medicine, Tribhuvan University, Kathmandu, Nepal.
Junxiang Wei, Global Health Institute, School of Public Health, Xi'an Jiaotong University Health Science Center, Xi'an, Shaanxi, China.
Parveen Akhtar, Global Health Institute, School of Public Health, Xi'an Jiaotong University Health Science Center, Xi'an, Shaanxi, China.
Liang Wang, Department of Biostatistics and Epidemiology, College of Public Health, East Tennessee State University, Johnson City, TN, USA.
Youfa Wang, Global Health Institute, School of Public Health, Xi'an Jiaotong University Health Science Center, Xi'an, Shaanxi, China; Fisher Institute of Health and Well-Being, Department of Nutrition and Health Science, College of Health, Ball State University, Muncie, IN, USA.
References
- 1. Wang YF, Mi J, Shan XY, Wang QJ, Ge KY. Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. Int J Obes. 2007;31(1):177–88. [DOI] [PubMed] [Google Scholar]
- 2. Wang YF, Chen HJ, Shaikh S, Mathur P. Is obesity becoming a public health problem in India? Examine the shift from under- to overnutrition problems over time. Obes Rev. 2009;10(4):456–74. [DOI] [PubMed] [Google Scholar]
- 3. Wang YF, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1(1):11–25. [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization. Double burden of malnutrition. [Internet]. Available from: http://www.who.int/nutrition/double-burden-malnutrition/en/. Accessed 2018 Sep 8. [Google Scholar]
- 5. Min J, Zhao Y, Slivka L, Wang YF. Double burden of diseases worldwide: coexistence of undernutrition and overnutrition-related non-communicable chronic diseases. Obes Rev. 2018;19(1):49–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416, population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tzioumis E, Kay MC, Bentley ME, Adair LS. Prevalence and trends in the childhood dual burden of malnutrition in low- and middle-income countries, 1990–2012. Public Health Nutr. 2016;19(8):1375–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Popkin BM. Rural areas drive increases in global obesity. Nature. 2019;569(7755):200–1. [DOI] [PubMed] [Google Scholar]
- 9. Wei JX, Bhurtyal A, Dhungana RR, Bhattarai B, Zheng JG, Wang L, Sun X, Maskey M, Wang Y. Changes in patterns of the double burden of under- and over-nutrition in Nepal over time. Obes Rev. 2019;20(9):1321–34. [DOI] [PubMed] [Google Scholar]
- 10. World Health Organization, Regional Office for South-East Asia. Strategic action plan to reduce the double burden of malnutirtion in the south-east Asia region 2016–2025. [Internet]. Available from: https://apps.who.int/iris/handle/10665/253377 Accessed 2018 Apr 7. [Google Scholar]
- 11. Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Romieu I, Dossus L, Barquera S, Blottière HM, Franks PW, Gunter M, Hwalla N, Hursting SD, Leitzmann M, Margetts B et al. Energy balance and obesity: what are the main drivers?. Cancer Causes Control. 2017;28(3):247–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Due P, Damsgaard MT, Rasmussen M, Holstein BE, Wardle J, Merlo J, Currie C, Ahluwalia N, Sørensen TI, Lynch J et al. Socioeconomic position, macroeconomic environment and overweight among adolescents in 35 countries. Int J Obes. 2009;33(10):1084–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. National Health Commission of the People's Republic of China China National Nutrition and Health Surveillance report 2010-2013. Beijing: People's Medical Publishing House; 2014. [Google Scholar]
- 15. National Health Commission of the People's Republic of China Report on Chinese Residents' Choronic Diseases and Nutrition 2015. Beijing: People's Medical Publishing House; 2016. [Google Scholar]
- 16. International Institute of Population Sciences, ICF National Family Health Survey (NFHS-4) 2015-16. Mumbai: International Institute of Population Sciences; 2017. [Google Scholar]
- 17. Ministry of Health, Nepal Nepal Demographic and Health Survey 2016. Kathmandu: Ministry of Health; 2017. [Google Scholar]
- 18. National Institute of Population Studies, Pakistan Pakistan Demographic and Health Survey 2017-18. Islamabad; 2019. [Google Scholar]
- 19. World Health Organization [Internet]. Available from: https://www.who.int/childgrowth/standards/ Accessed 2018 Apr 7. [Google Scholar]
- 20. World Health Organization [Internet]. Available from: https://www.who.int/topics/obesity/en/ Accessed 2018 Apr 7. [Google Scholar]
- 21. World Bank [Internet]. Available from: https://data.worldbank.org. Accessed 2018 Apr 7. [Google Scholar]
- 22. Ji CY, Working Group on Obesity in China . Report on childhood obesity in China – body mass index reference for screening overweight and obesity in Chinese school-age children. Biomed Environ Sci. 2005;18:390–400. [PubMed] [Google Scholar]
- 23. Zhou B, Coorperative Meta-analysis Group of China Obesity Task Force . Predictive values of body mass index and waist circumference to risk factors of related diseases in Chinese adult population. Chin J Epidemiol. 2002;23(1):5–10. [PubMed] [Google Scholar]
- 24. World Health Organization [Internet]. Available from: http://apps.who.int/gho/data/view.main.2463?lang=en. Accessed 2018 Apr 7. [Google Scholar]
- 25. Cannon G. Why the Bush administration and the global sugar industry are determined to demolish the 2004 WHO global strategy on diet, physical activity and health. Public Health Nutr. 2004;7(3):369–80. [DOI] [PubMed] [Google Scholar]
- 26. Raza L, Ali TM, Hasnain A. Comparison of dietary practices and body mass index among educated housewives and working women in Karachi. J Ayub Med Coll Abbottabad. 2017;29(2):293–7. [PubMed] [Google Scholar]
- 27. Neuman M, Kawachi I, Gortmaker S, Subramanian S. National economic development and disparities in body mass index: a cross-sectional study of data from 38 countries. PLoS One. 2014;9(6):e99327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. van Dam RM, Seidell JC. Carbohydrate intake and obesity. Eur J Clin Nutr. 2007;61(Suppl 1):S75–99. [DOI] [PubMed] [Google Scholar]
- 29. Wang YF, Beydoun MA. Meat consumption is associated with obesity and central obesity among US adults. Int J Obes. 2009;33(6):621–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. You WP, Henneberg M. Meat consumption providing a surplus energy in modern diet contributes to obesity prevalence: an ecological analysis. BMC Nutr. 2016;2:22. [Google Scholar]
- 31. Gong P, Liang S, Carlton EJ, Jiang Q, Wu J, Wang L, Remais JV. Urbanisation and health in China. Lancet. 2012;379(9818):843–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pirgon O, Aslan N. The role of urbanization in childhood obesity. J Clin Res Pediatr Endocrinol. 2015;7(3):163–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fox A, Feng W, Asal V. What is driving global obesity trends? Globalization or “modernization”?. Global Health. 2019;15(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Assah FK, Ekelund U, Brage S, Mbanya JC, Wareham NJ. Urbanization, physical activity, and metabolic health in sub-Saharan Africa. Diabetes Care. 2011;34(2):491–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Peters R, Amugsi DA, Mberu B, Ensor T, Hill AJ, Newell JN, Elsey H. Nutrition transition, overweight and obesity among rural-to-urban migrant women in Kenya. Public Health Nutr. 2019;; 22(17):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jiang J, Rosenqvist U, Wang H, Greiner T, Lian G, Sarkadi A. Influence of grandparents on eating behaviors of young children in Chinese three-generation families. Appetite. 2007;48:377–83. [DOI] [PubMed] [Google Scholar]
- 37. Kanter R, Caballero B. Global gender disparities in obesity: a review. Adv Nutr. 2012;3(4):491–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Holdsworth M, Gartner A, Landais E, Maire B, Delpeuch F. Perceptions of healthy and desirable body size in urban Senegalese women. Int J Obes. 2004;28(12):1561–8. [DOI] [PubMed] [Google Scholar]
- 39. Tateyama Y, Techasrivichien T, Musumari PM, Suguimoto SP, Zulu R, Macwan'gi M, Dube C, Ono-Kihara M, Kihara M. Obesity matters but is not perceived: a cross-sectional study on cardiovascular disease risk factors among a population-based probability sample in rural Zambia. PLoS One. 2018;13(11):e0208176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rguibi M, Belahsen R. Fattening practices among Moroccan Saharawi women. East Mediterr Health J. 2006;12(5):619–24. [PubMed] [Google Scholar]
- 41. United Nations. Sustainable development goals [Internet]. Available from: https://www.un.org/sustainabledevelopment/sustainable-development-goals/. Accessed 2018 Apr 7. [Google Scholar]
- 42. Food and Agricultural Organization of The United Nations [Internet]. Available from: http://www.fao.org/faostat/en/#data/FBS/report. Accessed 2019 Sep 24. [Google Scholar]
- 43. Wang YF, Sun MX, Yang YX. China Blue Paper on obesity prevention and control. Peking University Medical Press; 2019. [DOI] [PubMed] [Google Scholar]
- 44. Wang YF, Xue H, Sun MX, Zhu XY, Zhao L, Yang YX. Prevention and control of obesity in China. Lancet Glob Health. 2019;7(9):e1166–7. [DOI] [PubMed] [Google Scholar]
- 45. Pérusse L, Rankinen T, Zuberi A, Chagnon YC, Weisnagel SJ, Argyropoulos G, Walts B, Snyder EE, Bouchard C. The human obesity gene map: the 2004 update. Obes Res. 2005;13(3):381–490. [DOI] [PubMed] [Google Scholar]
- 46. Lu Y, Loos RJ. Obesity genomics: assessing the transferability of susceptibility loci across diverse populations. Genome Med. 2013;5(6):55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mathieu L, Bitterlich N, Meissner F, von Wolff M, Poethig D, Stute P. Illness perception in overweight and obesity and impact on bio-functional age. Arch Gynecol Obstet. 2018;298(2):415–26. [DOI] [PubMed] [Google Scholar]
- 48. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63. [DOI] [PubMed] [Google Scholar]
- 49. Kanazawa M, Yoshiike N, Osaka T, Numba Y, Zimmet P, Inoue S. Criteria and classification of obesity in Japan and Asia-Oceania. World Rev Nutr Diet. 2005;94:1–12. [DOI] [PubMed] [Google Scholar]
- 50. Seo MH, Lee WY, Kim SS, Kang JH, Kang JH, Kim KK, Kim BY, Kim YH, Kim WJ, Kim EM et al. 2018 Korean society for the study of obesity guideline for the management of obesity in Korea. J Obes Metab Syndr. 2019;28(1):40–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. National Health Commission of the People's Republic of China. Weight for adults (WS/T 428–2013) [18-04-2013] [Internet]. Available from: http://www.nhc.gov.cn/wjw/yingyang/201308/a233d450fdbc47c5ad4f08b7e394d1e8.shtml. Accessed 2018 Apr 7. [Google Scholar]


