Abstract
Purpose
The purpose of the present study was to investigate the effects of vonoprazan on the pharmacokinetics of venlafaxine in vitro and in vivo.
Methods
The mechanism underlying the inhibitory effect of vonoprazan on venlafaxine was investigated using rat liver microsomes. In vitro, the inhibition was evaluated by determining the production of O-desmethylvenlafaxine. Eighteen male Sprague–Dawley rats were randomly divided into three groups: control group, vonoprazan (5 mg/kg) group, and vonoprazan (20 mg/kg) group. A single dose of 20 mg/kg venlafaxine was administrated to rats orally without or with vonoprazan. Plasma was prepared from blood samples collected via the tail vein at different time points and concentrations of venlafaxine and its metabolite, O-desmethylvenlafaxine, were determined by ultra-performance liquid chromatography-tandem mass spectrometry.
Results
We observed that vonoprazan could significantly decrease the amount of O-desmethylvenlafaxine (IC50 = 5.544 μM). Vonoprazan inhibited the metabolism of venlafaxine by a mixed inhibition, combining competitive and non-competitive inhibitory mechanisms. Compared with that in the control group (without vonoprazan), the pharmacokinetic parameters of venlafaxine and its metabolite, O-desmethylvenlafaxine, were significantly increased in both 5 and 20 mg/kg vonoprazan groups, with an increase in MRO-desmethylvenlafaxine.
Conclusion
Vonoprazan significantly alters the pharmacokinetics of venlafaxine in vitro and in vivo. Further investigations should be conducted to check these effects in humans. Therapeutic drug monitoring of venlafaxine in individuals undergoing venlafaxine maintenance therapy is recommended when vonoprazan is used concomitantly.
Keywords: gastroduodenal ulcer, gastroesophageal reflux disease, proton pump inhibitors, vonoprazan fumarate
Introduction
The high incidence of acid-related diseases, such as gastroduodenal ulcer and gastroesophageal reflux disease, is an important public health issue. The introduction of proton pump inhibitors (PPIs) revolutionized the management of these diseases in clinical practice.1–3 Pharmacological acid suppression has shown success in the treatment of patients and has become the mainstay of treatment for these diseases. Vonoprazan fumarate was the first orally active potassium-competitive acid blocker (P-CAB) to be approved for the treatment of gastroesophageal reflux disease, peptic ulcer, gastric ulcer, erosive esophagitis, and reflux esophagitis, and for use as an adjunct in Helicobacter pylori eradication.4,5 Previous research has shown that vonoprazan is metabolized mainly by CYP3A4/5 and to some extent by CYP2B6, CYP2C19, CYP2D6, and SULT2A1;6 it can also inhibit these enzymes to varying degrees while being metabolized and, therefore, some drugs that are metabolized by these enzymes might be affected by its intake.7
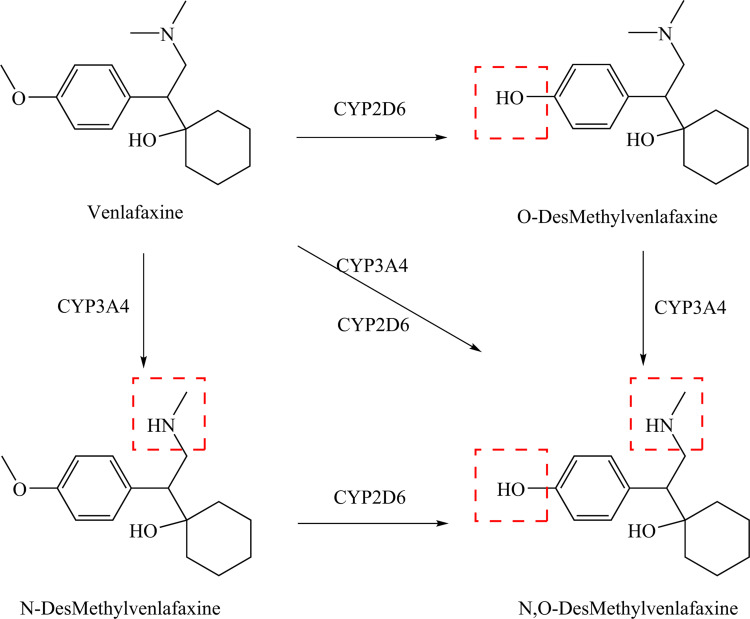
Many antidepressants are substrates of CYPA2D6 or CYP3A4/5, or are inhibitors of both the enzyme systems.8,9 Co-administration of drugs with vonoprazan might affect their curative effect. Venlafaxine (VEN) was the first serotonin–norepinephrine reuptake inhibitor introduced to the market and is one of the most popularly prescribed antidepressants in many countries.10 It has high oral bioavailability and is used in the treatment of a number of psychiatric disorders, including major depressive and anxiety disorders.11 Although VEN is more effective than several other antidepressants in treating major depression disorders, some patients fail to respond to the drug or discontinue the treatment because of a variety of serious side effects. Drug–drug interactions (DDI) may cause adverse drug reactions, which depend on the dose of the drug and its specific metabolism. Previous studies have shown that the biotransformation of VEN to O-desmethylvenlafaxine (ODV) is mediated by CYP2D6, and to N-desmethylvenlafaxine by CYP3A4 (Figure 1). After the administration of a single oral dose, more than half of the dose was metabolized to ODV, mainly through CYP2D6.12 Both VEN and ODV are bioactive in vivo. When CYP2D6 is inhibited by other drugs, such as vonoprazan, the biotransformation of VEN might be affected, thereby, increasing the chance of the treatment being compromised by adverse reactions.
Figure 1.
Venlafaxine metabolism to O-desmethylvenlafaxine, N-desmethylvenlafaxine, and N, O-didesmethylvenlafaxine.
PPIs are extensively metabolized by CYP isozymes and show a great potential for DDI. In previous studies, the possible pharmacokinetic interaction between VEN and two PPIs (omeprazole and pantoprazole) has been evaluated; it was suggested that these two PPIs can affect the metabolism of VEN by inhibiting the activity of CYP2C19.13 Vonoprazan has been on the market for a short time, and its metabolic pathways are different from those of omeprazole and pantoprazole, but it is still a substrate for CYP450 isozymes and has potential for interaction with VEN. In the absence of data on the pharmacokinetic interactions between VEN and vonoprazan, a novel PPI, the aim of this study was to investigate the possible pharmacokinetic interactions between vonoprazan and VEN. In this study, the effect of vonoprazan on VEN in rat liver microsomes (RLMs) and the underlying mechanism were studied by ultra-performance liquid chromatography–tandem mass spectrometry (UPLC-MS/MS). The effects of vonoprazan on the pharmacokinetics of VEN and its metabolite ODV in rats were also studied. Because our results showed that vonoprazan has significant inhibitory effect on VEN in RLMs, we conducted in vivo drug interaction experiments, in the presence or absence of vonoprazan, and evaluated the pharmacokinetic parameters of VEN and its metabolite ODV to assess the inhibition of VEN by vonoprazan.
Materials and Methods
Chemicals and Reagent
VEN was purchased from Sigma (St. Louis, MO, USA). ODV was purchased from Shanghai Macklin Biochemical (Shanghai, P.R. China). Vonoprazan was purchased from Send Pharm (Beijing, China). Diazepam (used as an internal standard, IS) and formic acid (gradient grade for liquid chromatography) were purchased from Sigma. Dimethylsulfoxide (DMSO) was purchased from Shanghai Aladdin Biochemical Technology Co. Ltd (Shanghai, P.R. China). Methanol (MeOH) and acetonitrile (ACN) (gradient grade for liquid chromatography) were purchased from Merck (Billerica, MA, USA). Purified water was obtained from the Milli-Q plus filtration system (Millipore, Billerica, MA, USA). All chemicals and solvents were of analytical grade.
Preparation of Rat Liver Microsomes
Rats were killed by cervical dislocation after they were starved for 12 h. The liver of the rat was exposed by opening the abdominal cavity and was perfused with 0.15 mol/L KCL buffer (pH = 7.4) through the superior vena cava till the blood was flushed off. Precisely 3 g liver tissue was removed and transferred to a petri dish and kept at 0–4°C. The tissue was homogenized in 0.15 mol/L KCL-PBS buffer (stored at 4°C). The homogenate was centrifuged (Optima XPN, Beckman Coulter, USA) at 9000 × g for 30 min at 4°C, and the supernatant, thus obtained, was precipitated by centrifugation at 105,000 × g for 60 min at 4°C. The precipitate containing liver microsomes was removed, and resuspended in 0.15 mol/L KCL-PBS buffer. The centrifugation (105,000 × g for 60 min at 4°C) and resuspension (0.15 mol/L KCL-PBS buffer containing 0.25 mol/L sucrose) steps were repeated for the preparation of liver microsome homogenate, which was then stored at −80°C until use. The concentration of liver microsomes was 8.838 mg/mL, as determined using the BCA protein quantitation kit.
Instruments and Conditions
The formation of ODV was measured using the UPLC-MS/MS method established in our laboratory. Waters Acquity UPLC (Waters Corp., Milford, MA, USA) was used for the separation of metabolites. The effective separation of metabolites was achieved on Acquity UPLC BEH C18 column (50 × 2.1 mm, 1.7 μm) (Waters Corporation, Milford, MA, USA) used at a column temperature of 40°C. The mobile phase consisted of a mixture of solvent A (acetonitrile) and solvent B (formic acid/ultrapure water, 1:1000, v/v). The linear gradient program for the mobile phase was set as follows: 0 min 10% A; 0.5 min 30% A; 1 min 95% A; 2 min 95% A; 2.6 min 10% A. The flow rate of the mobile phase was 0.4 mL/min and the injection volume was 2 μL.
The XEVO TQD triple quadrupole mass spectrometer was equipped with an electrospray ionization (ESI) source; multiple reaction monitoring (MRM) mode was selected for quantitation. The Mass Lynx 4.1 software (Waters Corp.) was used for data acquisition. Mass spectral data were obtained in positive electrospray mode (ESI+) in MRM mode. The quantitative ion pairs and related parameters of VEN, and of its metabolite, ODV, and diazepam (IS) are listed in Table 1. Other mass spectrometry parameters were as follows: a capillary voltage of 2000 V, a spray gas temperature of 500°C, and a gas flow rate of 50 L/min.
Table 1.
The Quantitative Ion Pairs and Related Parameters of Venlafaxine (VEN), Its Metabolite, O-Desmethylvenlafaxine (ODV), and Diazepam (Internal Standard)
| Compound | Parent (m/z) | Daughter (m/z) | Cone (V) | Collision (eV) |
|---|---|---|---|---|
| ODV | 264.15 | 57.96 | 30 | 20 |
| ODV | 264.15 | 106.95 | 30 | 30 |
| VEN | 278.19 | 58.00 | 30 | 20 |
| VEN | 278.19 | 120.97 | 30 | 30 |
| Diazepam | 285.10 | 193.10 | 35 | 30 |
Effect of Vonoprazan on the Metabolism of VEN in Rat Liver Microsomes
According to published article,14 range of 2–16 μM VEN was dissolved in methanol to meet concentrations at a series of the Km value. Vonoprazan was dissolved in DMSO and diluted at 0–10 μM concentrations with methanol to meet concentrations at about a series multiple of the IC50 value. The incubation was done in a total volume of 200 μL, which consisted of RLMs (1 mg/mL), 100 mM potassium phosphate buffer (pH = 7.4), 10 mM NADPH, 2–16 μM VEN, with or without vonoprazan at 0–10 μM concentration. After pre-incubation at 37°C for 5 min, the reaction was initiated by adding 10 μL NADPH. The reaction mixtures were incubated for 30 min, and the reaction was stopped by adding 200 μL ice-cold acetonitrile. All the reaction mixtures were centrifuged at 14,000 × g (10 min at 4°C) after mixing with 20 μL IS (500 ng/mL diazepam), and the supernatant obtained was analyzed. A 150 μL aliquot of the supernatant was placed on a UPLC vial and 2 μL was loaded in the UPLC-MS/MS system.
Animal Experiments
Male SPF Sprague-Dawley rats, weighing 180–220 g, were obtained from the Laboratory Animal Center of the Wenzhou Medicine University (Wenzhou, Zhejiang, China). They were fed a standard diet and kept under normal daily light cycle, 40–60% relative humidity at 25°C. The rats were fed once a day in the morning and in the evening and were allowed free access to water. The experimental drug was administered 1 week later. No other drugs were used before the experiment. All experimental produces and protocols were reviewed and approved by the Animal Care and Use Committee of Wenzhou Medical University (approval No. wydw2019-650) and were in accordance with the Guide for the Care and Use of Laboratory Animal.
In vivo Pharmacokinetic Study
Eighteen rats were randomly divided into three groups: control group (n = 6), pretreated with 0.5% Carboxymethylcellulose sodium (CMC-Na) once daily for 7 days before the administration of VEN (20 mg/kg, oral); low-dose group (n = 6), pretreated with vonoprazan (5 mg/kg, oral) in 0.5% CMC-Na once daily for 7 days before the administration of VEN; high-dose group (n = 6), pretreated with vonoprazan (20 mg/kg, oral) in 0.5% CMC-Na once daily for 7 days before the administration of VEN. Animals in both VEN and vonoprazan groups were given VEN at 4 mL/kg, after 30 min of the last treatment with vonoprazan. Rats in all the groups were administered VEN in 0.5% CMC-Na, at different time after the administration (0.083, 0.25, 0.5, 1, 2, 3, 4, 6, 12, 24 h); 300 μL blood samples were collected from the caudal vein and placed in Eppendorf tubes with heparin sodium. The blood samples were centrifuged (Optima XPN) at 4000 rpm for 10 min at 4°C to obtain the plasma, which was stored at −80°C until the analysis.
Preparation of Plasma Samples
The frozen plasma samples were thawed at room temperature and uniformly mixed; 100 μL plasma was taken out and mixed with 20 μL IS (500 ng/mL diazepam), and 200 μL ACN was added to precipitate the proteins, which was followed by vortexing for 30 s and centrifugation at 13,000 rpm for 5 min. A 150 μL aliquot of the supernatant, thus obtained, was transferred to UPLC vials and 2 μL of it was loaded into the UPLC-MS/MS system.
Data Analysis
All the data are averages of duplicate or triplicate determinations. The Km value of VEN, the 50% inhibitory effect of vonoprazan on VEN, and the plot plasma concentration–time curves were determined by nonlinear regression analysis with GraphPad prism (version 7.0; GraphPad Software Inc., San Diego, CA, USA). The pharmacokinetic parameters were calculated by noncompartmental analysis using DAS (version 3.2.8; The People’s Hospital of Lishui, China). Statistical comparisons within groups were conducted with SPSS (version 24.0; SPSS Inc., Chicago, IL, USA), using Student’s t-test. A P-value < 0.05 was considered statistically significant.
Results
Validation of Method
In this study, the regression equation of calibration standard curve is constructed as follows: VEN, y=(0.01565x + 0.00701, r2 = 0.9979); ODV, y=(0.01354x + 0.00034, r2 = 0.9957). The calibration standard curves demonstrated an excellent linearity at a concentration range of 1–500 ng·mL−1 for VEN and that of 0.2–100 ng·mL−1 for ODV. The inter-day and intra-day precision data for VEN in plasma at three quality control (QC) levels (3, 30, 300 ng·mL−1) were less than 8.58% and 9.06%, respectively; the accuracy of which is at a range of 94.70–105.83% and 98.37–103.56%, respectively. The inter-day and intra-day precision data for ODV in plasma at three QC levels (0.6, 6, 60 ng·mL−1) were less than 9.04% and 4.82%, respectively; the accuracy of which is at a range of 106.40–107.33% and 104.97 −109.35%, respectively. All the results are shown in Table 2.
Table 2.
Evaluation of the Inter- and Intra-Day Precision by the Proposed UPLC-MS/MS Method for Determination of VEN and ODV in Rat Plasma (n = 6)
| Analytes | Preparation Concentration (ng·mL−1) | Inter-Day | Intra-Day | ||
|---|---|---|---|---|---|
| Precision | Accuracy | Precision | Accuracy | ||
| RSD (%) | RE (%) | RSD (%) | RE (%) | ||
| VEN | 3 | 7.94 | 94.7 | 6.94 | 98.37 |
| 30 | 6.10 | 105.83 | 9.06 | 103.56 | |
| 300 | 8.58 | 106.22 | 6.38 | 102.15 | |
| ODV | 0.6 | 9.04 | 107.33 | 4.16 | 104.97 |
| 6 | 2.84 | 106.40 | 3.26 | 107.01 | |
| 60 | 5.12 | 106.75 | 4.82 | 109.35 | |
The results of different stability studies in plasma are shown in Table 3. The precision data for VEN and ODV in plasma at three QC levels under three different conditions (placed at 4°C for 24 hours, room temperature for 4 hours, −80°C for 7 days) were less than 11.60% and 5.55%, respectively; the accuracy of which at a range of 99.68–111.18% and 105.72–112.11%, respectively. The results of stability test were within the error range (±15%).
Table 3.
Stability Results of VEN and ODV in Rat Plasma Under Different Conditions (n = 6)
| Analytes | Preparation Concentration (ng·mL−1) | Room Temperature, 6h | 4°C, 24h | −80°C, 7 Days | |||
|---|---|---|---|---|---|---|---|
| Precision | Accuracy | Precision | Accuracy | Precision | Accuracy | ||
| RSD (%) | RE (%) | RSD (%) | RE (%) | RSD (%) | RE (%) | ||
| VEN | 3 | 11.60 | 102.90 | 7.55 | 108.99 | 9.35 | 99.68 |
| 30 | 8.42 | 103.09 | 7.83 | 111.18 | 7.36 | 108.61 | |
| 300 | 8.09 | 102.08 | 6.68 | 106.95 | 8.86 | 105.33 | |
| ODV | 0.6 | 3.36 | 107.58 | 4.37 | 112.11 | 3.29 | 105.72 |
| 6 | 3.68 | 109.40 | 2.30 | 107.41 | 4.43 | 103.07 | |
| 60 | 5.55 | 109.57 | 3.39 | 108.96 | 2.39 | 106.85 | |
Effects of Vonoprazan on the Enzyme Kinetics of VEN in vitro
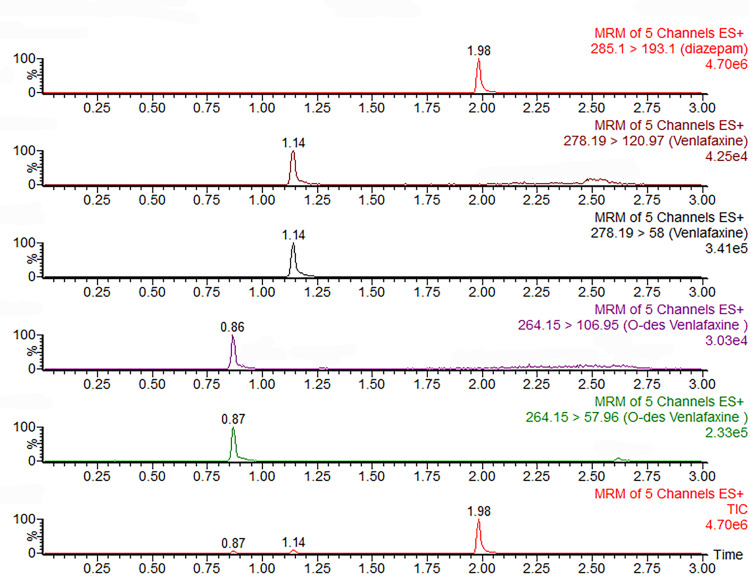
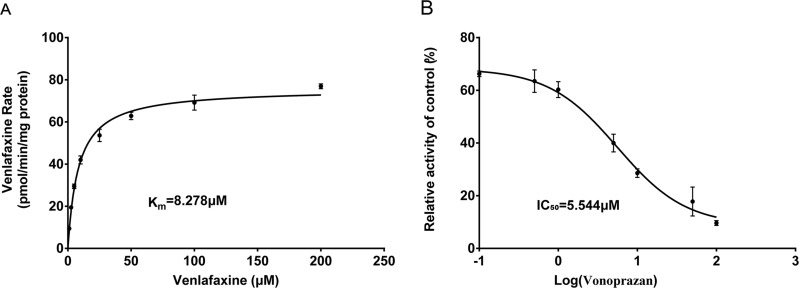
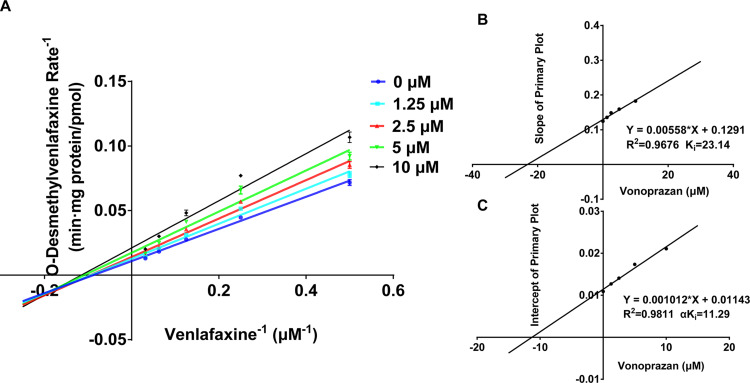
The method of quantification of ODV was established successfully without any interfering peaks as shown in Figure 2. The calibration curves demonstrated linearity over the range from 0.025 to 5 μM for ODV. The Km value for VEN was determined by non-linear regression of the reaction velocity versus substrate concentration (Figure 3). A value of Km = 8.278 μM for VEN was determined as the concentration of ODV. The assessment of inhibition revealed that vonoprazan could significantly decrease the concentration of ODV (IC50 = 5.544 μM). Vonoprazan inhibited the metabolism of VEN, with a Ki of 23.14 μM and a Ki’ of 11.29 μM, by a mixed inhibition mechanism, involving competitive as well as non-competitive inhibition.
Figure 2.
Typical MRM chromatograms of venlafaxine, O-desmethylvenlafaxine and diazepam (IS).
Figure 3.
(A) Substrate saturation plots, from product formation data, for venlafaxine (1–200 µM) in RLMs. (B) Effect of the vonoprazan on venlafaxine metabolism in RLMs (vonoprazan 0.1–100 µM).
Effects of Vonoprazan on the Pharmacokinetics of VEN in vivo
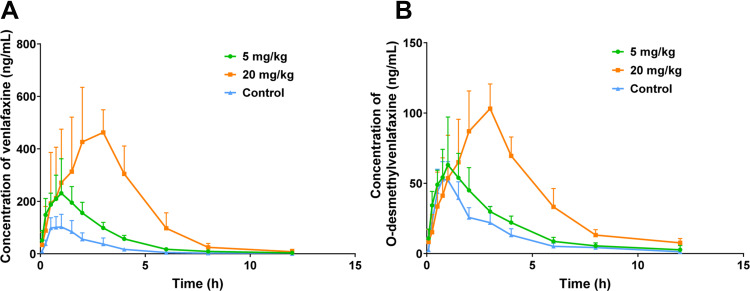
Mean plasma concentration-time profiles of VEN and ODV after oral administration of VEN (20 mg/kg) in the presence and absence of vonoprazan (5 and 20 mg/kg) in rat are shown in Figures 4 and 5; the corresponding pharmacokinetic parameters for VEN and ODV are shown in Tables 4 and 5. Compared with the control group, when co-administrated with 20 mg/kg vonoprazan, the AUC (0-∞) values for VEN and ODV were significantly increased by 6.37- and 2.05-fold, and the MRT (0-∞) values were increased by 0.58- and 0.39-fold, respectively. The Tmax and Cmax of VEN and ODV were elevated by 2.71-, 2.46-fold and 3.12- and 0.88-fold, respectively. Additionally, vonoprazan significantly decreased the CLz/F of VEN and ODV, and the Vz/F of VEN and ODV were decreased by 86.87%, 68.33%, 89.35%, and 62.08%, respectively. When co-administrated with 5 mg/kg vonoprazan, only the AUC(0-t) of VEN and ODV, and Cmax of VEN were increased by 1.66-, 0.39-, and 1.05-fold, respectively. The Clz/F of VEN was significantly decreased by 65.73%; the other parameters of VEN and ODV were not altered by the presence of vonoprazan. However, the metabolite (M. R.) in the rats co-administered with 5 and 20 mg/kg vonoprazan increased by 0.87- and 1.34-fold compared to that in the control group.
Figure 4.
Lineweaver–Burk plots for vonoprazan inhibition of venlafaxine in rat livers microsomes. Data shown are the mean ± standard deviation of triplicate experiment. (A) Lineweaver–Burk plots for vonoprazan (0, 1.25, 2.5, 5, 10 μM) inhibition of venlafaxine (2, 4, 6, 8 μΜ) in rat livers microsomes. (B) Slope of Primary Plot. (C) Intercept of Primary Plot.
Figure 5.
Mean plasma concentration–time profiles of venlafaxine (A) and O-desmethylvenlafaxine (B) after an oral administration of venlafaxine (20 mg/kg) to rats in the presence and absence of vonoprazan (5 and 20 mg/kg) (mean ± S.D., n=6); (1) Low-dose group was pretreat with vonoprazan (5 mg/kg, oral); (2) High-dose group was pretreat with vonoprazan (20 mg/kg, oral); (3) Control group was administered by venlafaxine (20 mg/kg, oral).
Table 4.
Mean Pharmacokinetic Parameters of Venlafaxine (VEN) After Oral Administration (20 mg/kg) to Rats in the Presence and Absence of Vonoprazan (5 and 20 mg/kg)
| Parameters | VEN | VEN + Vonoprazan | |
|---|---|---|---|
| 5 mg/kg | 20 mg/kg | ||
| AUC(0-t) (µg·L−1·h−1) | 260.40 ± 101.62 | 688.80 ± 160.61* | 1,905.03 ± 548.19* |
| AUC (0-∞) (µg·L−1·h−1) | 260.91 ± 101.43 | 693.96 ± 162.74* | 1,922.61 ± 565.66* |
| MRT(0-t) (h) | 2.09 ± 0.18 | 2.44 ± 0.30 | 3.28 ± 0.52* |
| MRT (0-∞) (h) | 2.12 ± 0.17 | 2.52 ± 0.43 | 3.36 ± 0.56* |
| t1/2z (h) | 1.39 ± 0.32 | 1.48 ± 0.46 | 1.28 ± 0.53 |
| Tmax (h) | 0.70 ± 0.21 | 0.95 ± 0.37 | 2.60 ± 0.55* |
| Vz/F (L·kg−1) | 187.22 ± 129.65 | 62.08 ± 15.41 | 19.93 ± 7.19* |
| CLz/F (L·h−1·kg−1) | 87.60 ± 37.78 | 30.02 ± 6.51* | 11.50 ± 4.80* |
| Cmax (µg·L−1) | 127.38 ± 41.53 | 261.43 ± 109.51* | 525.11 ± 114.59* |
Notes: n = 6 per group; data are expressed as mean ± SD. *Significantly different from control, P < 0.05.
Abbreviations: AUC, area under the plasma concentration–time curve; CL, plasma clearance; Cmax, maximum plasma concentration; MRT, mean residence time; t1/2, half-life; Tmax, time taken to reach maximum plasma level.
Table 5.
Mean Pharmacokinetic Parameters of O-Desmethylvenlafaxine (ODV) After Oral Administration of Venlafaxine (VEN; 20mg/kg) to Rats in the Presence and Absence of Vonoprazan (5 and 20 mg/kg)
| Parameters | VEN | VEN + Vonoprazan | |
|---|---|---|---|
| 5 mg/kg | 20 mg/kg | ||
| AUC(0-t) (µg·L−1·h−1) | 155.32 ± 36.65 | 220.80 ± 31.51* | 469.33 ± 68.58* |
| AUC(0-∞) (µg·L−1·h−1) | 160.95 ± 43.45 | 224.59 ± 31.70* | 491.64 ± 79.81* |
| MRT(0-t) (h) | 2.82 ± 0.55 | 3.08 ± 0.48 | 3.92 ± 0.38* |
| MRT(0-∞) (h) | 3.20 ± 1.16 | 3.28 ± 0.49 | 4.44 ± 0.52 |
| t1/2z (h) | 2.05 ± 1.05 | 2.01 ± 0.36 | 2.43 ± 0.75 |
| Tmax (h) | 0.75 ± 0.18 | 0.95 ± 0.37 | 2.60 ± 0.55* |
| Vz/F (L·kg−1) | 373.67 ± 170.49 | 259.92 ± 41.47 | 141.68 ± 30.36* |
| CLz/F (L·h−1·kg−1) | 131.82 ± 35.47 | 90.37 ± 11.76 | 41.74 ± 8.16* |
| Cmax (µg·L−1) | 58.10 ± 14.09 | 69.72 ± 30.05 | 109.35 ± 13.42* |
| MR | 1.64±0.52 | 3.06±0.29* | 3.84±0.69* |
Notes: n = 6 per group; data are expressed as mean ± SD; *Significantly different from control, P < 0.05.*MR ODV =AUC VEN/AUC ODV.15
Abbreviations: AUC, area under the plasma concentration–time curve; CL, plasma clearance; Cmax, maximum plasma concentration; MRT, mean residence time; t1/2, half-life; Tmax, time taken to reach maximum plasma level.
Discussion
PPI affects drug absorption and metabolism by interacting with the CYP450 enzyme system. With the increasing clinical use of PPIs, the risk of unnecessary DDI increases inevitably. Vonoprazan was marketed in Japan as the first orally active P-CAB. Vonoprazan is metabolized mainly by CYP3A4/5 and to some extent by CYP2B6, CYP2C19, CYP2D6, and SULT2A1, it can also inhibit these enzymes to varying degrees.5,7 Many antidepressants are substrates of CYPA2D6 or CYP3A4/5, or inhibitors of both the enzyme systems, such as VEN, the first serotonin-norepinephrine and norepinephrine reuptake inhibitors introduced to the market, which was used in the treatment of a number of psychiatric disorders, including major depressive disorders and anxiety disorders.11 The biotransformation of VEN to its active metabolite, ODV, is mediated by CYP2D6, and to N-desmethylvenlafaxine via CYP3A4. More than half of the dose is converted to ODV after a single oral administration, mainly by metabolism through CYP2D6.
Drug–drug interactions may cause adverse drug reactions, which depend on the dose of the drug and its specific metabolism. In this study, we first investigated the inhibitory mechanism of vonoprazan on VEN in rat liver microsomes by calculating the generation of ODV. The results suggested that vonoprazan significantly inhibited the formation of ODV and exhibited moderate inhibition of the VEN metabolism (IC50 = 8.278 μM). The inhibition of vonoprazan by VEN, with a Ki of 23.14 μM and a Ki’ of 11.29 μM, occurred through a mixed inhibition mechanism, combining both competitive and non-competitive inhibition. The mechanism of inhibition suggests that vonoprazan may display mixed inhibition through multiple pathways, such as CYP3A4 or 2D6.
In our previous studies, results of in vitro and in vivo experiments showed that vonoprazan inhibited CYP3A4, CYP2C9, CYP2D6, and CYP2B6 in vitro and in vivo.16 It has been previously established that metabolism of VEN is dominated by CYP2D6 and it is transformed into the active metabolite ODV in the liver,17–19 In addition, CYP3A4/5 also participate partially in the metabolism of VEN.20 Therefore, VEN is susceptible to CYP450-mediated DDI, especially through the CYP2D6 metabolic pathway.21 In this study, the plasma concentrations of VEN and ODV were significantly elevated, suggesting that vonoprazan causes clinically relevant inhibition of VEN metabolism via CYP3A4 or 2D6. In the presence of vonoprazan, the AUC(0-t) and Cmax values for VEN and ODV were significantly increased. Vonoprazan (20 mg/kg) had a more significant effect on enhancing the oral exposure of venlafaxine. VEN undergoes first-pass metabolism; under the influence of vonoprazan, the first-pass metabolism was reduced, thereby, increasing the drug absorption, which might be the reason for the increased AUC(0-t) and Cmax for VEN. The metabolite–parent ratio (MR) in rats administrated vonoprazan (5 and 20 mg/kg) increased significantly (P < 0.05) compared with that in the control, implying that vonoprazan had obvious inhibitory effect on the transformation of VEN to ODV, and displayed dose-dependent effect on VEN metabolism. The results of in vitro and in vivo studies indicate that vonoprazan can significantly inhibit the activity of CYP3A4 or 2D6. In the present study, the significant alteration in MRODV in the presence of 5 and 20 mg/kg vonoprazan suggested that vonoprazan is capable of altering the formation of ODV, which is mainly metabolized by CYP2D6.15,20 As shown in Figure 5, while the slope of the concentration–time curve was similar in all the rats after oral administration, the coadministration of vonoprazan increased the AUC(0-t), Cmax and MRODV of VEN with a decrease in the total plasma clearance. These results indicate that vonoprazan can reduce the metabolism in the GI tract during the intestinal absorption. A dose of 5 mg/kg vonoprazan may provide the inhibitory concentration in vivo.
ODV is considered to have an antidepressant effect similar to that of VEN.22,23 CYP2D6 is an enzyme with high affinity and low volume, which dominates the VEN metabolism;17 its activity is considered to be a major intrinsic factor in the pharmacokinetics of VEN,11 but it is speculated that the clinical significance of altering the activity of CYP2D6 is limited.24 Both vonoprazan and VEN are substrates of CYP2D6. The inhibitory mechanism of vonoprazan may be due to the competition between these two drugs for the CYP2D6 binding sites, leading to decreased VEN metabolism while increasing the plasma concentration of VEN and ODV.25 In addition, a portion of VEN metabolized by CYP3A4 was reported to be inactive N-desmethylvenlafaxine.26 Vonoprazan is mainly metabolized by CYP3A4 and exhibits a certain degree of activity.27 We suspected that the inhibition of CYP3A4 activity by vonoprazan may block the formation of N-desmethylvenlafaxine, and support the formation to ODV via CYP2D6.13 Inhibition of VEN formatted into N-demethylation via CYP3A4 results only in minor changes in its pharmacokinetics, because CYP3A4 has a small effect on VEN metabolism, in general.24 Moreover, VEN and ODV are both P-glycoprotein (P-gp) substrates. Hence, alterations in the activity of P-gp may essentially affect the absorption and metabolism of VEN,13 which may be the reason that vonoprazan reduced the metabolism of the VEN in the gastrointestinal tract during intestinal absorption and increased the AUC(0-t) and Cmax of VEN and its active metabolic ODV.28
Vonoprazan is a new PPI that was launched in December 2014. It has the advantages of new mechanism of action, faster onset time, longer acid inhibition time, and less drug and food influence. Vonoprazan has been on the market for a very short time, there are many clinical trials to support its clinical application, but still lack of medical experience and comprehensive clinical data, especially the part related to drug–drug interactions. This study explored the effects of vonoprazan on venlafaxine in vitro and in vivo and found that vonoprazan can significantly affect the absorption and metabolism of venlafaxine, which is an important reference for the verification of real DDI in the clinical environment in the future.
Owing to limited conditions, we have not been able to conduct experiments in a real clinical environment. On the basis of the current rat experiment results, further research would be under consideration in the future. In addition, specific inhibitory mechanism can also be explored in depth. Therefore, more rigorous clinical trials are needed to further confirm these findings.
In summary, our study investigated the effects of vonoprazan on venlafaxine in vitro and in vivo. The results showed that vonoprazan inhibited the absorption and metabolism of venlafaxine, suggesting that attention should be paid to the effects of vonoprazan on venlafaxine in clinical applications. The clinical significance of these findings needs to be further evaluated in clinical studies.
Conclusion
The results of our study indicate that vonoprazan significantly inhibits VEN metabolism in vivo and in vitro in a dose-dependent manner, and that this inhibition occurs through a mixed inhibition mechanism, involving competitive and non-competitive inhibition. Vonoprazan (5 and 20 mg/kg) could significantly change the pharmacokinetic parameters of VEN and ODV, when co-administered with VEN. Therefore, concomitant use of vonoprazan and VEN will require close monitoring of potential drug–drug interactions.
Acknowledgments
The authors gratefully thank Prof. Longyou Zhao for their helpful writing-review and editing of the manuscript.
Funding Statement
This work was supported by grants funded by Public Welfare Technology Research Funding Project of Zhejiang (LGD19H090001 and LGD20H060001), High-level talent training project of Lishui (2018RC18), Medical and Health Research Project of Zhejiang province (2017KY731 and 2019ZYY10), City level key research and development Project of Lishui (2017ZDYF15 and 2020ZDYF12) and CAMS Innovation Fund for Medical Sciences (2018-I2M-1-002).
Data Sharing Statement
The data used to support the findings of this study are included within the article.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Scarpignato C, Gatta L, Zullo A, et al. Effective and safe proton pump inhibitor therapy in acid-related diseases - A position paper addressing benefits and potential harms of acid suppression. BMC Med. 2016;14(1):179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Malfertheiner P, Kandulski A, Venerito M. Proton-pump inhibitors: understanding the complications and risks. Nat Rev Gastroenterol Hepatol. 2017;14(12):697–710. doi: 10.1038/nrgastro.2017.117 [DOI] [PubMed] [Google Scholar]
- 3.Murakami K, Sakurai Y, Shiino M, Funao N, Nishimura A, Asaka M. Vonoprazan, a novel potassium-competitive acid blocker, as a component of first-line and second-line triple therapy for Helicobacter pylori eradication: a Phase III, randomised, double-blind study. Gut. 2016;65(9):1439–1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kinoshita Y, Sakurai Y, Takabayashi N, et al. Efficacy and safety of vonoprazan in patients with nonerosive gastroesophageal reflux disease. Clin Transl Gastroenterol. 2019;10(11). doi: 10.14309/ctg.0000000000000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nishihara M, Yamasaki H, Czerniak R, Jenkins H. In vitro assessment of potential for Cyp-inhibition-based drug-drug interaction between vonoprazan and clopidogrel. Eur J Drug Metab Pharmacokinet. 2019;44(2):217–227. doi: 10.1007/s13318-018-0521-7 [DOI] [PubMed] [Google Scholar]
- 6.Shen J, Wang B, Wang S, et al. Effects of voriconazole on the pharmacokinetics of vonoprazan in rats. Drug Des Devel Ther. 2020;14:2199–2206. doi: 10.2147/DDDT.S255427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Echizen H. The first-in-class potassium-competitive acid blocker, vonoprazan fumarate: pharmacokinetic and pharmacodynamic considerations. Clin Pharmacokinet. 2016;55(4):409–418. doi: 10.1007/s40262-015-0326-7 [DOI] [PubMed] [Google Scholar]
- 8.Wang SH, Wang ZY, Chen DX, et al. Effect of acute paraquat poisoning on CYP450 isoforms activity in rats by cocktail method. Int J Clin Exp Med. 2015;8(10):19100–19106. [PMC free article] [PubMed] [Google Scholar]
- 9.Wang SH, Dong YW, Su K, et al. Effect of codeine on CYP450 isoform activity of rats. Pharm Biol. 2017;55(1):1223–1227. doi: 10.1080/13880209.2017.1297466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Furukawa TA, Cipriani A, Cowen PJ, Leucht S, Egger M, Salanti G. Optimal dose of selective serotonin reuptake inhibitors, venlafaxine, and mirtazapine in major depression: a systematic review and dose-response meta-analysis. Lancet Psychiatry. 2019;6(7):601–609. doi: 10.1016/S2215-0366(19)30217-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jiang F, Kim HD, Na HS, et al. The influences of CYP2D6 genotypes and drug interactions on the pharmacokinetics of venlafaxine: exploring predictive biomarkers for treatment outcomes. Psychopharmacology (Berl). 2015;232(11):1899–1909. doi: 10.1007/s00213-014-3825-6 [DOI] [PubMed] [Google Scholar]
- 12.Pan PP, Wang SH, Wang J, et al. Simultaneous determination of methadone, fluoxetine, venlafaxine and their metabolites in rat plasma by UPLC–MS/MS for drug interaction study. Chromatographia. 2016;79(9–10):1–8. [Google Scholar]
- 13.Kuzin M, Schoretsanitis G, Haen E, et al. Effects of the proton pump inhibitors omeprazole and pantoprazole on the cytochrome P450-mediated metabolism of venlafaxine. Clin Pharmacokinet. 2018;57(6):729–737. doi: 10.1007/s40262-017-0591-8 [DOI] [PubMed] [Google Scholar]
- 14.Zhou Y, Tu Y, Zhou Q, et al. Evaluation of acacetin inhibition potential against cytochrome P450 in vitro and in vivo. Chem Biol Interact. 2020;329:109147. doi: 10.1016/j.cbi.2020.109147 [DOI] [PubMed] [Google Scholar]
- 15.Pan PP, Wang J, Luo J, et al. Silibinin affects the pharmacokinetics of methadone in rats. Drug Test Anal. 2018;10(3):557–561. doi: 10.1002/dta.2235 [DOI] [PubMed] [Google Scholar]
- 16.Wang Y, Wang C, Wang S, et al. Cytochrome P450-based drug-drug interactions of vonoprazan in vitro and in vivo. Front Pharmacol. 2020;11:53. doi: 10.3389/fphar.2020.00053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fogelman SMSJ, Venkatakrishnan K, Moltke LL, Harmatz JS, Shader RI, Greenblatt DJ. O- and N-demethylation of venlafaxine in vitro by human liver microsomes and by microsomes from cDNA-transfected cells: effect of metabolic inhibitors and SSRI antidepressants. Neuropsychopharmacology. 1999;20(50):480–490. doi: 10.1016/S0893-133X(98)00113-4 [DOI] [PubMed] [Google Scholar]
- 18.Dai DP, Wang SH, Geng PW, Hu GX, Cai JP. In vitro assessment of 36 CYP2C9 allelic isoforms found in the chinese population on the metabolism of glimepiride. Basic Clin Pharmacol Toxicol. 2014;114(4):305–310. [DOI] [PubMed] [Google Scholar]
- 19.Dai DP, Wang SH, Li CB, et al. Identification and functional assessment of a new CYP2C9 allelic variant CYP2C9(star)59. Drug Metab. Dispos. 2015;43(8):1246–1249. doi: 10.1124/dmd.115.063412 [DOI] [PubMed] [Google Scholar]
- 20.Godoy AL, Rocha A, da Silva Souza C, Lanchote VL. Pharmacokinetics of venlafaxine enantiomers and their metabolites in psoriasis patients. J Clin Pharmacol. 2016;56(5):567–575. doi: 10.1002/jcph.630 [DOI] [PubMed] [Google Scholar]
- 21.Augustin M, Schoretsanitis G, Grunder G, Haen E, Paulzen M. How to treat hypertension in venlafaxine-medicated patients-pharmacokinetic considerations in prescribing amlodipine and ramipril. J Clin Psychopharmacol. 2018;38(5):498–501. doi: 10.1097/JCP.0000000000000929 [DOI] [PubMed] [Google Scholar]
- 22.Schoretsanitis G, Haen E, Hiemke C, et al. Pharmacokinetic correlates of venlafaxine: associated adverse reactions. Eur Arch Psychiatry Clin Neurosci. 2019;269(7):851–857. doi: 10.1007/s00406-019-01005-0 [DOI] [PubMed] [Google Scholar]
- 23.Lin XQ, Wang P, Cai WK, et al. The associations between CYP2D6 metabolizer status and pharmacokinetics and clinical outcomes of venlafaxine: a systematic review and meta-analysis. Pharmacopsychiatry. 2019;52(5):222–231. doi: 10.1055/a-0792-1340 [DOI] [PubMed] [Google Scholar]
- 24.Hynninen VVOKT, Bertilsson L, Kurkinen K, Neuvonen PJ, Laine K Effect of terbinafine and voriconazole on the pharmacokinetics of the antidepressant venlafaxine. Clin Pharmacol Ther. 2008;83(2):342–348. doi: 10.1038/sj.clpt.6100311 [DOI] [PubMed] [Google Scholar]
- 25.Kowalewski C, Haen E, Hiemke C, et al. Cytochrome P450-mediated inhibition of venlafaxine metabolism by trimipramine. Int Clin Psychopharmacol. 2019;34(5):241–246. doi: 10.1097/YIC.0000000000000268 [DOI] [PubMed] [Google Scholar]
- 26.Paulzen M, Schoretsanitis G, Hiemke C, Grunder G, Haen E, Augustin M. Reduced clearance of venlafaxine in a combined treatment with quetiapine. Prog Neuropsychopharmacol Biol Psychiatry. 2018;85:116–121. doi: 10.1016/j.pnpbp.2018.04.014 [DOI] [PubMed] [Google Scholar]
- 27.Martinucci I, Blandizzi C, Bodini G, et al. Vonoprazan fumarate for the management of acid-related diseases. Expert Opin Pharmacother. 2017;18(11):1145–1152. doi: 10.1080/14656566.2017.1346087 [DOI] [PubMed] [Google Scholar]
- 28.Choi JS, Han HK. Pharmacokinetic interaction between diltiazem and morin, a flavonoid, in rats. Pharmacol. Res. 2005;52(5):386–391. doi: 10.1016/j.phrs.2005.05.011 [DOI] [PubMed] [Google Scholar]