Abstract
Although the cytologic criteria of atypia of undetermined significance (AUS) are defined in The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC), there is heterogeneity in its prevalence, utilization, interpretation, and management. To determine the current practices of physicians of various specialties in the management of thyroid lesions reported as AUS in fine-needle aspirates in the Philippines, a survey consisting of eighteen questions was sent to physicians of varied specialties. Survey questions included geographical location of practice, type of practice (whether in a private or government setting or with academic affiliation), annual patient load, primary operator of fine-needle aspiration (FNA), number of procedures performed, method used, whether by palpation or with ultrasound-guidance, pre-procedure requirements, request for rapid on-site evaluation (ROSE), awareness and utilization of thyroid image reporting and data system (TI-RADS), knowledge of cytologic preparation of aspirates, utilization of TBSRTC nomenclature in the workplace, number of AUS that turned out benign, number of AUS that turned out malignant, management of AUS cases in the setting of patient and physician, utilization of frozen section, implication of surgery over repeat FNA. There were seventy four respondents composed of 20 (27%) otorhinolaryngologists, 15 (20%) pathologists, 14 (19%) endocrinologists, 13 (18%) radiologists, and 12 (16%) general surgeons, practicing in different institutions, with majority (58%) of the respondents based in the National Capital Region. AUS report was encountered by 58 respondents (78%) in up to 10% of their cases, eight respondents (11%) had AUS report in up to 20% of their cases and only one respondent (1%) had AUS report in more than 30% of the cases. Seven (10%), who were mainly radiologists, did not answer the question. Thirty nine physicians (53%) conservatized management with medical follow up and repeat FNA within the time frame prescribed in the Bethesda system, 11 (15%) referred patients with AUS for surgery, 16 (22%) had varied comments. Eight (11%) respondents, who were mainly radiologists, did not answer the question. The data shows that the approach to management of AUS is heterogenous amongst physician-specialists, although, majority of clinicians adhere to the practice guidelines of the American Thyroid Association. Deviation to the guidelines occur since approach to management of patients is individualized.
Keywords: Atypia of undetermined significance, fine-needle aspiration biopsy, thyroid nodules with atypia
Introduction
Although the cytologic criteria of atypia of undetermined significance (AUS) are defined in The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC), there is heterogeneity in its prevalence, utilization, interpretation, and management. With the new development in thyroid pathology, the estimated risk of malignancy of AUS was revised to 15–30% in TBSRTC 2017 (1) which was initially in the range of 5–15% in TBSRTC 2007 (2). A wide range of malignancy rates has been reported all over the world, in as much as wide variation in the approach to management of AUS is available in the literature, despite recommendation of the Bethesda system of a repeat fine-needle aspiration (FNA) (3-5). Studies on thyroid cytology in the Philippines are minimal, composed mainly of cytohistologic correlation reports. Risk of malignancy (ROM) of AUS in five reports in the country ranged from 22.2% to 50% (average: 37.3%) (6-11) and nearer in range from 14.3–75% (average: 44%) as those from other Asian countries (12) but were higher than the Bethesda system implied ROM range from 10% to 30% (1).
Objective
The study aims to determine the current practices of physicians of various specialties in the management of thyroid lesions reported as AUS in fine-needle aspirates in the Philippines.
Methodology
A survey consisting of eighteen questions was sent to physicians of varied specialties (endocrinology, otorhinolaryngology, surgery, radiology, and pathology). Survey questions included geographical location of practice, type of practice (whether in a private or government setting or with academic affiliation), annual patient load, primary operator of FNA, number of procedures performed, method used, whether by palpation or with ultrasound-guidance, pre-procedure requirements, request for rapid on-site evaluation (ROSE), awareness and utilization of thyroid image reporting and data system (TI-RADS), knowledge of cytologic preparation of aspirates, utilization of TBSRTC nomenclature in the workplace, number of AUS that turned out benign, number of AUS that turned out malignant, management of AUS cases in the setting of patient and physician, utilization of frozen section, and implication of surgery over repeat FNA. The answers of the respondents were tabulated, and percentages were computed. Comments and additional notes were analyzed in the context of their answers.
Results
Physicians’ profile
Of the seventy-four respondents, 20 (27%) were otorhinolaryngologists, 15 (20%) were pathologists, 14 (19%) were endocrinologists, 13 (18%) were radiologists, and 12 (16%) were general surgeons. Physicians’ engagement was not limited to one hospital and was usually affiliated with one other hospital. Sixty-three were practicing in private hospitals, 29 in academic centers and/or university hospitals, 25 in government hospitals, and, 16 in independent private clinics. Fourty three physicians (58%) were based in the National Capital Region while the rest (42%) practiced in various regions (1 to 12) of the country.
Twenty-eight (38%) physicians managed less than 100 patients with thyroid lesions annually, 14 (19%) examined 101 to 200 cases, 11 (14%) examined 201 to 400 cases, and 19 (26%) treated more than 400 patients. Two respondents did not give an answer as to the number of patients that he/she examined annually. FNA was performed by otorhinolaryngologists (25%), pathologists (22%), endocrinologists (18%), surgeons (18%), and radiologists (17%). Thirty physicians (40%) had 20 to 50 FNA procedures, 12 (16%) performed 51 up to 100 FNA, 16 (22%) did more than 100 FNA and the same number did not perform the procedure and referred them to other specialists. Answers to the physicians’ profile are summarized in Table 1.
Table 1. Physicians profile.
| Survey questions | Number | Percentage (%) |
|---|---|---|
| Specialties | ||
| Otorhinolaryngologists | 20 | 27 |
| Pathologists | 15 | 20 |
| Endocrinologists | 14 | 19 |
| Radiologists | 13 | 18 |
| General surgeons | 12 | 16 |
| Number of patients with thyroid lesions examined annually | ||
| <100 | 28 | 38 |
| 101–200 | 14 | 19 |
| 201–400 | 11 | 14 |
| >400 | 19 | 26 |
| No answer | 2 | 3 |
| Number of thyroid FNAs† done annually | ||
| 20–50 | 30 | 40 |
| 51–100 | 12 | 16 |
| >100 | 16 | 22 |
| Did not perform/referred to others | 16 | 22 |
†, fine-needle aspiration.
Clinical practices
In the initial evaluation of thyroid lesions, requests for sonogram, thyroid function tests, FNA and thyroid scan consisted of 44%, 33%, 19%, and 4%, respectively. FNA was performed by 26% of physicians using palpation only, 19% of doctors utilized ultrasound-guidance, and in 55% of them, both palpation and ultrasound-guidance were used regardless of their place of practice whether in an academic setting, private or government hospitals, or independent private clinics.
Rapid on-site evaluation (ROSE) of thyroid aspirates was requested by 22 (30%) physicians in their workplace. Thirty (40%) did not find the request necessary. Twenty-two (30%) commented variably that ROSE would be done when pathologists or radiologists performed the procedure, the latter on ultrasound-guidance for specimen adequacy, and, upon special requests of self-paying patients.
Of the 64 (87%) respondents who were aware of thyroid image reporting and data system (TI-RADS), 20 (31%) required this system in their reports. Ten (14%) did not bother to know TI-RADS and accepted the usual manner of ultrasound reporting. Forty-nine (66%) utilized TBSRTC in their practice, 7 (10%) did not and 18 (24%) claimed that the system of reporting was modified and dependent on the pathologists and their hospital affiliations. Forty-four (60%) physicians were aware of the various types of cytologic preparations of thyroid aspirates in the laboratory while 30 (40%) were not. Frozen section was requested by 20% of physicians while 24% did not; 41% requested for intraoperative consultation in certain situations like poor correlation of clinical assessment and FNA findings, in confirmation of suspicious cases on FNA, and patient’s preferential request. Eleven (15%) respondents, mostly pathologists and radiologists, either did not answer or indicated that they felt that the question was not applicable to them as they did not participate in the active management of the patients. Answers to the clinical practices are summarized in Table 2.
Table 2. Answers to questions pertaining to clinical practices.
| Survey questions | Number | Percentage (%) |
|---|---|---|
| FNA method | ||
| Palpation-guided | 19 | 26 |
| Ultrasound-guided | 14 | 19 |
| Both | 41 | 55 |
| Performance of ROSE† | ||
| Yes | 22 | 30 |
| No | 30 | 40 |
| Only in certain situations | 22 | 30 |
| Awareness of TIRADS‡ | ||
| Yes | 64 | 87 |
| No | 9 | 12 |
| No answer | 1 | 1 |
| Use of TBSRTC§ | ||
| Yes | 49 | 66 |
| No | 7 | 10 |
| Other | 18 | 24 |
| Awareness of cytologic preparations | ||
| Yes | 44 | 60 |
| No | 30 | 40 |
†, rapid on-site evaluation; ‡, thyroid imaging Reporting and Data Systems; §, the Bethesda System for Reporting Thyroid Cytopathology.
Pertaining to AUS
AUS report was encountered by 58 respondents (78%) in up to 10% of their cases, eight respondents (11%) had AUS report in up to 20% of their cases and only one respondent (1%) had AUS report in more than 30% of the cases. Seven (10%), who were mainly radiologists, did not answer the question. Thirty nine physicians (52%) conservatized management with medical follow up and repeat FNA within the time frame prescribed in the Bethesda system, 11 (15%) referred patients with AUS for surgery, 16 (22%) had varied comments ranging from repeat ultrasound, repeat FNA under ultrasound-guidance within variable time frame ranging from 1 to 6 months, and direct surgery referral in cases with nodules bigger than 3.0 cm. and suspicious ultrasound findings. Eight (11%) respondents, who were mainly radiologists, did not answer the question.
Out of 74 respondents, 60 physicians gave an answer when asked “what is the approximate percentage of AUS cases that turned out to be benign upon surgery in your practice?”. Of the 60, 35 (58%) said that these AUS cases turn out to be benign after surgery at most 50% of the time and 25 (42%) of these AUS cases turn out to be benign after surgery more than 50% of the time. Fourteen respondents did not answer the question. Out of the 74 respondents, 50 respondents gave an answer when asked “what is the approximate percentage of AUS cases that turned out to be malignant upon surgery in your practice?”. Eight of them (16%) said that the AUS cases turn out to be malignant less than 5% of the time, 29 (58%) said that the AUS cases turn out to be malignant 5% to 20% of the time, and 13 physicians (26%) said that the AUS cases turn out to be malignant 21% up to 50% of the time. None of the fifty reported that the AUS cases turn out to be malignant more than 50% of the time. Twenty-four respondents did not answer the question.
In both questions, the respondents who did not answer said that they were either unsure of their answer, or, thought that question was not applicable to them.
Responses in favor of conservative management included the following: (I) endocrinologists opting for medical management with regular follow-up; (II) while surgical pathology is the reference standard, FNA is accurate especially in the hands of experienced operator and cytopathologist, and could readily be performed as an out-patient procedure; (III) clinical follow-up rather than surgery being advocated for more than one thyroid nodule or multiple lesions smaller than 2.0 cm. in diameter as these are oftentimes multinodular goiters responding to medical management; (IV) surgery referral only in cases with a strong index of suspicion for malignancy such as increasing size of nodule, change in sonographic pattern, and unfavorable cytology on repeat FNA.
Positive responses to surgery included the following: (I) surgery with histopathologic examination is the gold standard allaying fear of patient in a growing mass lesion; (II) poor patient compliance with loss to follow-up showing more beneficial effect to patients’ well-being with lifetime thyroid hormone supplementation; (III) patient’s choice with reassurance of final diagnosis after surgery. Answers to the questions pertaining to AUS are summarized in Table 3.
Table 3. Answers to questions pertaining to AUS†.
| Survey questions | Number | Percentage (%) |
|---|---|---|
| Rate of category III (AUS/FLUS‡) | ||
| ≤10% | 58 | 78 |
| 11–20% | 8 | 11 |
| 21–20% | 0 | 0 |
| >30% | 1 | 1 |
| No answer | 7 | 10 |
| Management | ||
| Observe and follow-up | 7 | 9 |
| Follow-up and repeat FNA§ | 32 | 43 |
| Refer for surgery | 11 | 15 |
| Other | 16 | 22 |
| No answer | 8 | 11 |
| Percentage of AUS cases that turn out to be benign (60 respondents) | ||
| Up to 50% | 35 | 58 |
| More than 50% | 25 | 42 |
| Percentage of AUS cases that turn out to be malignant (50 respondents) | ||
| Less than 5% | 8 | 16 |
| 5% to 20% | 29 | 58 |
| 21% to 50% | 13 | 26 |
| More than 50% | 0 | 0 |
†, atypia of undetermined significance; ‡, atypia of undetermined significance/Follicular lesion of undetermined significance; §, fine-needle aspiration. AUS, atypia of undetermined significance.
Discussion
The current diagnostic algorithm as prescribed by the American Thyroid Association in the evaluation of thyroid nodules follows a linear approach in the management that includes utilization of clinical information, sonographic and cytologic features and in certain indeterminate cases, use of molecular markers (13). A triage scheme of repeat FNA, ultrasound findings and BRAFV600E gene mutation in AUS thyroid aspirates can be used to identify patients with low or high risk of cancer (14). The algorithm is generally used by various physician-specialists in the country except for the molecular studies in deciding whether patients will be subjected to active surveillance or surgery. Molecular studies are rarely ordered since the tests are unaffordable with limited availability even in large centers in the national capital region and utilized only for those who are willing to self-pay.
Patients are subjected to FNA after results of ultrasound and thyroid function tests are available as practiced by 77% of attending physicians. Thyroid function abnormalities in the Philippines are prevalent in 8.53% with majority having subclinical thyroid diseases (15). Prevalence of AUS ranges from 5.4% to 8.9% (7,8). In the present review, AUS in thyroid FNA is encountered at its highest by 78% of physicians in only up to one tenth of their thyroid cases.
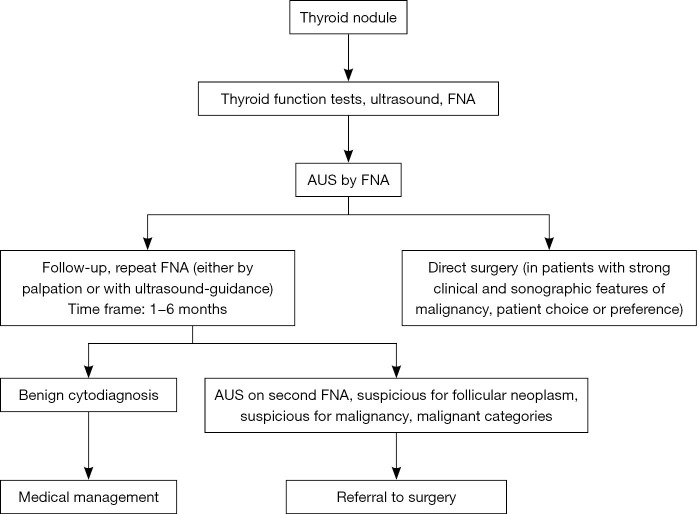
A conservative approach with repeat FNA after an initial diagnosis of AUS is done by 52% of physicians (Figure 1), who are mainly endocrinologists who tend to adhere to the guidelines of American Thyroid Association. The AUS category is a low risk category for malignancy for which a repeat FNA would be the most appropriate management in majority of cases (2,5). The repeat sonogram and FNA, usually under the guidance of ultrasound at least on or after the third month of the procedure following the initial recommendation of TBSRTC (2010) (2) is mostly adhered to, ending with either benign or suspicious or malignant cytodiagnosis in the hands of experienced cytopathologists. The second edition of TBSRTC, however, does not impose the same restriction in terms of timing of the repeat FNA and permit shorter intervals shorter than 3 months. Repeat FNA in an initial AUS cytodiagnosis has shown a higher rate of reclassification (67.6%) to a definitive diagnosis (16). The repeat procedure outside the initial recommended time frame ranging from one to less than three months is considered by endocrinologists in cases with discordant radiographic findings and cytodiagnosis, presence of a growing mass or a recurrent cystic lesion. This is concordant with the findings of various investigators that physicians use their own criteria as to the timing of repeat FNA and they have also shown that clinical variables such as age and gender are more important than the timing of the repeat procedure (17). On the other hand, ultrasound features of hypo- or anechogenicity rather than age and gender were significantly associated with higher malignancy risk (18).
Figure 1.
Flow diagram on the management approach to AUS thyroid nodules as surveyed from 74 clinician-specialists. AUS, atypia of undetermined significance; FNA, fine-needle aspiration.
AUS nodules that have a benign cytodiagnosis after a repeat FNA are subjected to regular follow-up with thyroid function tests and imaging surveillance, duration of which is dependent on the evaluation of the attending physician. The repeat FNA, preferably with ultrasound guidance if requested may be done at a much later time if the stable nodules increase in size even in the absence of radiologic findings suspicious of malignancy.
Several studies have demonstrated deviation from standard approach to management with surgical intervention without the benefit of repeat FNA (Figure 1) (3). In the local setting, direct referral to either surgeons or otorhinolaryngologists without the benefit of a repeat FNA after an AUS cytodiagnosis is individualized. These are done in cases with a strong suspicion of malignancy. Presence of a solid nodule, sonographic findings of hypoechogenicity, microcalcifications and irregular borders, and a high TI-RADS score are factors that influence our clinicians for surgery referral. Hypo- or anechogenicity as an ultrasound feature is strongly associated with a malignancy risk in AUS. Clinical predictors of malignancy among adult Filipino patients include presence of firm to hard solid nodule, microcalcifications and irregular margins on ultrasound (19). In another local study, size of the nodule, duration of the lesion, and history of childhood irradiation were not useful parameters in distinguishing benign from malignant lesions since most of the cases presented as slowly growing goiter with average duration of 6 years with malignant cases occurring sporadically and with rare cases among family members with similar malignancy (20). Solid nodules, microcalcifications, increased nodule size greater than or equal to 2 cm. and younger patient age (less than 65 years) were associated with triage to surgery (21).
Use of molecular markers in AUS is limited only to self-paying patients as contrasted to other parts of the world wherein NRAS, HRAS, TERT gene, and BRAFV600E gene mutations are utilized in some cases of AUS, and once detected, malignancy risk is strong (22). In contrast, BRAFV600E gene mutation is typically encountered in aspirates of thyroid papillary carcinoma and cases of suspicious for papillary carcinoma and rarely in AUS and suspicious for follicular neoplasm (23). Our local patients prefer to undergo surgery than be subjected to active medical surveillance including molecular studies in the interest of saving money and resolve fears of what the underlying thyroid pathology really is.
Direct surgery after an AUS cytodiagnosis is done by 15% of physicians in our study and this is mainly due to a strong suspicion of malignancy after clinical and sonographic correlation. Thyroidectomy whether subtotal or total is also influenced by patient’s personal choice of treatment prevailing over the standard approach to management due to geographic location and to allay fear of resolving whether there is malignancy or not. Intraoperative consultation during thyroid surgery is utilized by 41% of physicians in certain cases only especially with poor clinical and sonographic correlation and patients’ preference. Majority of patients who opted for total thyroidectomy were made to understand the aftermath of surgery with lifetime exogenous thyroid hormone medication.
Our data shows that the approach to management of AUS is heterogenous amongst physician-specialists in the country. There is no structured continuity of consultation. Data base of patients, if available, is confined within the physicians’ workplace whether in hospitals or clinics, and not linked all throughout the country. Patients’ mobility gives them the choice to transfer from one physician to another and therefore work up and treatment may be interrupted and become disjointed. In situations where patient needs to transfer to another geographic location, management may be delayed since retrieval of previous pertinent data may take a while to become available.
While endocrinologists usually adopt a conservative type of treatment of their AUS cases with a repeat FNA, referral to surgery is made without hesitation in cases with strong index of suspicion for malignancy. Some general surgeons and otorhinolaryngologists opt for early surgical intervention once an AUS cytodiagnosis is encountered. They are also largely influenced by the patients’ desire to have the mass removed.
Radiologists perform ultrasound-guided FNA and simply confine themselves in the performance of the diagnostic procedure. Pathologists are usually called upon by some radiologists who perform the procedure to render rapid on-site evaluation of the sample aspirates, allowing multiple and repeat punctures until an adequate specimen is obtained. Doing ROSE on collected material would help prevent repeat biopsy at another time (24,25). There are also a handful of endocrinologists and few cytopathologists who perform the procedure and most of them do not find the need to do an on-site cytodiagnosis since they are confident of their FNA biopsy technique. The effect of doing ROSE on adequacy rate is varied and controversial with some studies showing an increased rate of adequacy but depending on the initial adequacy rate (26) and others showing no significant effect (24,27) and so whether to do it or not depends on the person performing the procedure, and the ability of the patient to avail of such services. Performing ROSE could also make the procedure longer (27). Ultrasound-guided biopsies are preferred with better yield especially for smaller lesions, however, in the setting of a middle income country where sonogram is not always available especially in small clinics, FNA guided by palpation, which is performed by 26% of physicians in our survey, still predominates over that of ultrasound-guided procedure.
While 25 (42%) of 60 physicians received a benign histodiagnosis after surgery of more than half of their AUS cases, 37 (74%) of 50 physicians received a malignant histopathologic report in only up to a quarter of their AUS cases. This shows the wide variation in the numbers of both benign and malignant histopathologic outcome of their AUS cases in various proportions.
Conclusions
Management of patients with AUS diagnosis is heterogenous within and across the different specialties. This includes combinations of diagnostic tests, biopsy practices, use of sonographic and pathologic reporting systems, availability and request for frozen section services and ROSE. Although majority of clinicians adhere to the practice guidelines of the American Thyroid Association, deviations from the guidelines occur since approach to management of patients, whether conservative or surgery, is individualized depending on clinical and sonographic features as well as patient preference.
Recommendations
Recommendations for future studies include (I) recruitment of more respondents, particularly those in far-flung areas of the country in order to compare management of different specialties and patient outcomes in both rural and urban settings (II) exploring the role of molecular studies, including NRAS, HRAS TERT gene and BRAFV600E gene mutation, among others, in the management of Filipino patients with AUS, especially when these tests become more widely available, and see how the Philippines fare compared with other countries, (III) following up on patients diagnosed with AUS and comparing the final histopathogic diagnosis, including patients diagnosed with NIFTP.
Acknowledgments
The authors would like to thank the following for their support for this work: Dr. Raquel R. Fortun, Ms. Eustachia Matias and Dr. Mark Angelo Ang.
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Verbal informed consent was obtained from all subjects before the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Footnotes
Provenance and Peer Review: This article was commissioned by the Guest Editor (Kennichi Kakudo) for the series “Asian and Western Practice in Thyroid Pathology: Similarities and Differences” published in Gland Surgery. The article was sent for external peer review organized by the Guest Editor and the editorial office.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs-20-426). The series “Asian and Western Practice in Thyroid Pathology: Similarities and Differences” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
References
- 1.Ali SZ, Cibas ES. editors. The Bethesda system for reporting thyroid cytopathology: definitions, criteria, and explanatory notes. 2nd ed. Cham, Switzerland: Springer International Publishing, 2018. [Google Scholar]
- 2.Ali SZ, Cibas ES. editors. The Bethesda system for reporting thyroid cytopathology: definitions, criteria, and explanatory notes. New York: Springer, 2010:171. [Google Scholar]
- 3.VanderLaan PA, Marqusee E, Krane JF. Clinical Outcome for Atypia of Undetermined Significance in Thyroid Fine-Needle Aspirations: Should Repeated FNA Be the Preferred Initial Approach? Am J Clin Pathol 2011;135:770-5. 10.1309/AJCP4P2GCCDNHFMY [DOI] [PubMed] [Google Scholar]
- 4.Jo VY, Stelow EB, Dustin SM, et al. Malignancy Risk for Fine-Needle Aspiration of Thyroid Lesions According to The Bethesda System for Reporting Thyroid Cytopathology. Am J Clin Pathol 2010;134:450-6. 10.1309/AJCP5N4MTHPAFXFB [DOI] [PubMed] [Google Scholar]
- 5.Nayar R, Ivanovic M. The indeterminate thyroid fine-needle aspiration: Experience from an academic center using terminology similar to that proposed in the 2007 National Cancer Institute Thyroid Fine Needle Aspiration State of the Science Conference. Cancer 2009;117:195-202. [DOI] [PubMed] [Google Scholar]
- 6.Abelardo AD. Thyroid Fine-Needle Aspiration Practice in the Philippines. J Pathol Transl Med 2017;51:555-9. 10.4132/jptm.2017.07.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carlos AD, Mirasol R, Thomas Aquino E, et al. Management and Malignancy Rate of Thyroid Nodules with a Cytologic Diagnosis of Atypia or Follicular Lesion of Undetermined Significance. J ASEAN Fed Endocr Soc 2014;29:78 10.15605/jafes.029.01.12 [DOI] [Google Scholar]
- 8.Salillas AL, Almocera EG. The implication of atypia of undetermined significance (AUS) category to a pathologist in a third world country. Acta Cytol 2016;60:50-1. [Google Scholar]
- 9.OngRamos C. Ultrasound guidance improves the diagnostic yield and accuracy of fine needle aspiration biopsy of thyroid nodules in detecting malignancy. J Thyroid Disord Ther 2014. Available online: http://www.omicsgroup.org/journals/ultrasound-guidance-improves-the-diagnostic-yield-and-accuracy-of-fine-needle-aspiration-biopsy-of-thyroid-nodules-in-detecting-malignancy-2167-7948-3-148.php?aid=25619
- 10.Salillas AL, Sun FCS, Almocera EG. Review of the Bethesda System for Reporting Thyroid Cytopathology: A Local Study in Bohol Island, Philippines. Acta Cytol 2015;59:77-82. 10.1159/000371752 [DOI] [PubMed] [Google Scholar]
- 11.Abelardo AD, Enriquez AM. Thyroid aspirates using the Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) in the assessment of risk malignancy: a comparison with conventional system of cytodiagnosis. Proc Taiwan Soc Pathol 2011;148. [Google Scholar]
- 12.Kakudo K, Higuchi M, Hirokawa M, et al. Thyroid FNA cytology in Asian practice-Active surveillance for indeterminate thyroid nodules reduces overtreatment of thyroid carcinomas. Cytopathology 2017;28:455-66. 10.1111/cyt.12491 [DOI] [PubMed] [Google Scholar]
- 13.Haugen BR. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: What is new and what has changed?: ATA 2015 Thyroid Nodule/DTC Guidelines. Cancer 2017;123:372-81. 10.1002/cncr.30360 [DOI] [PubMed] [Google Scholar]
- 14.Kim TH, Jeong DJ, Hahn SY, et al. Triage of patients with AUS/FLUS on thyroid cytopathology: effectiveness of the multimodal diagnostic techniques. Cancer Med 2016;5:769-77. 10.1002/cam4.636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carlos-Raboca J, Jimeno CA, Kho SA, et al. The Philippine Thyroid Diseases Study (PhilTiDeS 1): prevalence of thyroid disorders among adults in the Philippines. J ASEAN Fed Endocr Soc 2014;27:27. [Google Scholar]
- 16.Brandler TC, Aziz MS, Coutsouvelis C, et al. Young investigator challenge: Atypia of undetermined significance in thyroid FNA: Standardized terminology without standardized management-a closer look at repeat FNA and quality measures: AUS: Repeat FNA and Quality Monitoring. Cancer Cytopathol 2016;124:37-43. 10.1002/cncy.21648 [DOI] [PubMed] [Google Scholar]
- 17.Nagarkatti SS, Faquin WC, Lubitz CC, et al. Management of thyroid nodules with atypical cytology on fine-needle aspiration biopsy. Ann Surg Oncol 2013;20:60-5. 10.1245/s10434-012-2601-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hong SH, Lee H, Cho MS, et al. Malignancy risk and related factors of atypia of undetermined significance/follicular lesion of undetermined significance in thyroid fine needle aspiration. Int J Endocrinol 2018;2018:4521984. 10.1155/2018/4521984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cañete EJ, Sison-Peña CM, Jimeno CA. Clinicopathological, biochemical, and sonographic features of thyroid nodule predictive of malignancy among adult Filipino patients in a tertiary hospital in the Philippines. Endocrinol Metab (Seoul) 2014;29:489. 10.3803/EnM.2014.29.4.489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lo TEN, Uy AT, Maningat PDD. Well-Differentiated Thyroid Cancer: The Philippine General Hospital Experience. Endocrinol Metab (Seoul) 2016;31:72. 10.3803/EnM.2016.31.1.72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kuru B, Atmaca A, Tarim IA, et al. Risk factors associated with malignancy and with triage to surgery in thyroid nodules classified as Bethesda category III (AUS/FLUS). Eur J Surg Oncol 2016;42:87-93. 10.1016/j.ejso.2015.09.026 [DOI] [PubMed] [Google Scholar]
- 22.Choi HR, Choi BY, Cho JH, et al. BRAFV600E Mutation is a Strong Preoperative Indicator for Predicting Malignancy in Thyroid Nodule Patients with Atypia of Undetermined Significance Identified by Fine Needle Aspiration. Korean J Otorhinolaryngol-Head Neck Surg 2018;61:600-4. 10.3342/kjorl-hns.2018.00199 [DOI] [Google Scholar]
- 23.Valderrabano P, McIver B. Evaluation and Management of Indeterminate Thyroid Nodules: The Revolution of Risk Stratification Beyond Cytological Diagnosis. Cancer Control 2017;24:1073274817729231. 10.1177/1073274817729231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jiang D, Zang Y, Jiang D, et al. Value of rapid on-site evaluation for ultrasound-guided thyroid fine needle aspiration. J Int Med Res 2019;47:626-34. 10.1177/0300060518807060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim MJ, Kim EK, Park SI, et al. US-guided Fine-Needle Aspiration of Thyroid Nodules: Indications, Techniques, Results. RadioGraphics 2008;28:1869-86. 10.1148/rg.287085033 [DOI] [PubMed] [Google Scholar]
- 26.Witt BL, Schmidt RL. Rapid Onsite Evaluation Improves the Adequacy of Fine-Needle Aspiration for Thyroid Lesions: A Systematic Review and Meta-Analysis. Thyroid 2013;23:428-35. 10.1089/thy.2012.0211 [DOI] [PubMed] [Google Scholar]
- 27.O’Malley ME, Weir MM, Hahn PF, et al. US-guided fine-needle aspiration biopsy of thyroid nodules: adequacy of cytologic material and procedure time with and without immediate cytologic analysis. Radiology 2002;222:383-7. 10.1148/radiol.2222010201 [DOI] [PubMed] [Google Scholar]