Abstract
BACKGROUND
Programmed death ligand 1 (PD-L1) immunotherapy remains poorly efficacious in colorectal cancer (CRC). The recepteur d’origine nantais (RON) receptor tyrosine kinase plays an important role in regulating tumor immunity.
AIM
To identify the patterns of RON and PD-L1 expression and explore their clinical significance in CRC.
METHODS
Gene expression data from the Gene Expression Omnibus database (GEO; n = 290) and patients at the First Affiliated Hospital, Zhejiang University School of Medicine (FAHZUSM; n = 381) were analyzed to determine the prognostic value of RON and PD-L1 expression within the tumor microenvironment of CRC. HT29 cell line was treated with BMS-777607 to explore the relationship between RON activity and PD-L1 expression. Signaling pathways and protein expression perturbed by RON inhibition were evaluated by cellular immunofluorescence and Western blot.
RESULTS
In the GEO patient cohort, cut-off values for RON and PD-L1 expression were determined to be 7.70 and 4.3, respectively. Stratification of patients based on these cutoffs demonstrated that high expression of RON and PD-L1 was associated with a poor prognosis. In the FAHZUSM cohort, rates of high expression of RON in tumor cells, high PD-L1 expression in tumor cells and tumor infiltrating monocytes, and both high RON and high PD-L1 expression in the tumor microenvironment were 121 (32%), 43 (11%), 91 (24%), and 51 (13.4%), respectively. High expression of RON was significantly correlated with high expression of PD-L1 in the tumor cell compartment (P < 0.001). High expression of RON and that of PD-L1 were independent prognostic factors for poorer overall survival. Concurrent high expression of both RON and PD-L1 in the tumor microenvironment was significantly associated with a poor prognosis. In vitro, BMS-777607 inhibited the phosphorylation of RON, inhibited PD-L1 expression, and attenuated activation of the ERK1/2 and AKT signaling pathways in CRC cells.
CONCLUSION
RON, PD-L1, and their crosstalk are significant in predicting the prognostic value of CRC. Moreover, phosphorylation of RON upregulates PD-L1 expression, which provides a novel approach to immunotherapy in CRC.
Keywords: Colorectal cancer, Programmed death ligand 1, Prognosis, Recepteur d’origine nantais, Tumor infiltrating mononuclear cells, Tumor microenvironment
Core Tip: Recepteur d’origine nantais (RON) expression plays an important role in regulating tumor immunity, and the efficacy of programmed death ligand 1 (PD-L1) immunotherapy in colorectal cancer (CRC) is still not satisfactory. This inspired us to study the clinical significance and correlation of RON and PD-L1 in CRC. The major discoveries and findings in this study are: (1) The abnormal expression of RON and PD-L1 was not only correlated, but was also significant biomarkers for poor prognosis of CRC. This finding was identified in 389 primary CRC clinical samples via multiplex immunofluorescence staining and immunohistochemistry staining; and (2) In in vitro experiments, activation of RON phosphorylation up-regulated the expression of PD-L1 in CRC cells.
INTRODUCTION
Colorectal cancer (CRC) is the fourth most common malignancy worldwide in 2018[1]. Despite advances in CRC treatment methods, it still has a poor prognosis, and many patients will have local recurrence and/or distant metastasis within 5 years after treatment[2].
Immunotherapy has become a promising strategy for treating a wide variety of malignancies[3]. Therapeutic antibodies that block the activity of programmed death ligand 1 (PD-L1, also known as CD274) protein are effective against many cancer types[4]. PD-L1 is a transmembrane immune checkpoint protein that can be expressed on both immune cells and cancer cells, including CRC cells[5-7]. When expressed on immune cells, PD-L1 can be regulated by a variety of inflammatory mediators and cytokines. When expressed on the surface of tumor cells (TCs), PD-L1 enables TCs to evade the immune system[8,9]. Cancer cells can induce the expression of PD-L1 through activation of oncogenic pathways, such as the RAS-ERK or PI3K-AKT pathways, to facilitate immune escape[10-12].
However, the efficacy of PD-L1 immunosuppressive agents in CRC is poor[13,14]. The overall poor response of CRC to PD-L1 blockade may be due to the activity of multiple oncogenes[15,16]. For example, KRAS mutations can up-regulate the expression of PD-L1 in CRC cells, thereby reducing the efficacy of PD-L1 immunosuppressive agents[17]. RON (macrophage-stimulating 1 receptor, MST1R), a member of the MET proto-oncogene family and a receptor for MSP, is an effector of KRAS signaling, and exhibits “KRAS addiction”, a phenomenon that plays an important role in the initiation and development of tumors[18-20]. RON is overexpressed pathologically in various types of cancer, including CRC, and many small-molecule inhibitors are being developed to target RON and its associated compounds[20-22]. BMS-777607 is a highly selective small molecule inhibitor of RON (IC50 1.8nM for RON)[23]. Activation of RON leads to RON phosphorylation, which then activates different signaling pathways in cancer cells, including the RAS-ERK and PI3K-AKT pathways[24-26]. Interactions between RON and other membrane receptors further promote pathway activation, enhancing the migration and invasion of CRC cells[20,22]. In addition, overexpression of RON can damage immune cells and inhibit anti-tumor immunity[27,28]. Thus, abnormal expression of RON may affect the efficacy of PD-L1 immunotherapy in CRC.
In this study, we investigated the clinical significance of expression patterns of RON and PD-L1 in primary CRC samples, and evaluated the potential for RON and PD-L1 as prognostic biomarkers in CRC. We treated CRC cells with BMS777607 in vitro to explore if RON inhibition affects the expression of PD-L1 and results in changes in related signaling pathways in CRC cells. Our data suggested that RON inhibition may be a novel approach to augment immunotherapy in CRC.
MATERIALS AND METHODS
Patient demographics
This study involved a GEO (Gene Expression Omnibus) cohort and a FAHZUSM (The First Affiliated Hospital, Zhejiang University School of Medicine) cohort. In the GEO cohort, the median age of all 287 CRC patients was 70 years (range: 24-97 years). There were 158 (55.1%) male patients and 129 (44.9%) female patients. The median survival time was 58 months, and 94 patients died during follow-up. In the FAHZUSM cohort, the median age of the CRC patients undergoing tumor resection was 61 years (range: 29-94 years). In this cohort, 215 (56.4%) patients were male and 166 (43.6%) were female. The median survival time was 100 months, and 91 patients died during follow-up. The primary site of a tumor, pathological grade, TNM stage, disease stage, histological type, and treatment status of CRC patients are shown in Table 1.
Table 1.
Comparison of RON and PD-L1 expression and clinicopathological characteristics of patients with colorectal cancer in the FAHZUSM and Gene Expression Omnibus cohorts, n (%)
|
FAHZUSM cohort (n = 381)
|
GEO cohort (n = 287)
|
||||||||||||||||
| Characteristic | Cases |
RON expression
|
PD-L1 expression
|
Cases No (%) |
RON expression
|
PD-L1 expression
|
|||||||||||
|
Low
|
High
|
1
P
value
|
Low
|
High (TIMC)
|
2
P
value
|
Low
|
High (TC)
|
3
P
value
|
Low
|
High
|
1
P
value
|
Low
|
High (TC)
|
3
P
value
|
|||
| No. of cases number | 381 | 260 | 121 | 247 | 91 | 247 | 43 | 287 | 193 | 94 | 48 | 239 | |||||
| Age (mean ± SD) | 61.16 ± 12.419 | 60.40 ± 12.560 | 62.81 ± 11.997 | 0.859 | 60.94 ± 12.37 | 62.04 ± 13.080 | 0.771 | 60.94 ± 12.37 | 61.16 ± 12.419 | 0.938 | 68.44 ± 14.00 | 66.87 ± 13.18 | 71.65 ± 15.12 | 0.006 | 66.94 ± 14.33 | 68.74 ± 13.95 | 0.417 |
| Sex | |||||||||||||||||
| Man | 215 (56.4) | 157 (60.4) | 58 (47.9) | 0.023 | 143 (57.9) | 54 (59.3) | 0.811 | 143 (57.9) | 18 (41.9) | 0.051 | 158 (55.1) | 111 (57.5) | 47 (50) | 0.230 | 30 (62.5) | 128 (53.6) | 0.256 |
| Women | 166 (43.6) | 103 (39.6) | 63 (52.1) | 104 (42.1) | 37 (40.7) | 104 (42.1) | 25 (58.1) | 129 (44.9) | 82 (42.5) | 47 (50) | 18 (37.5) | 111 (46.4) | |||||
| Principal diagnosis | |||||||||||||||||
| Rectum | 229 (60.1) | 158 (61.1) | 71 (58.7) | 0.698 | 153 (61.9) | 47 (51.6) | 0.088 | 153 (61.9) | 29 (67.4) | 0.491 | 165 (57.5) | 111 (57.5) | 54 (57.4) | 0.920 | 34 (70.8) | 131 (54.8) | 0.040 |
| Colon | 152 (39.9) | 102 (38.9) | 50 (41.3) | 94 (38.1) | 44 (48.4) | 94 (38.1) | 14 (32.6) | 122 (42.5) | 82 (42.5) | 40 (42.6) | 14 (29.2) | 108 (45.2) | |||||
| Pathological grade | |||||||||||||||||
| Well/moderate | 9 (2.4) | 6 (2.3) | 3 (2.5) | 0.177 | 5 (2) | 3 (3.3) | 0.778 | 5 (2) | 1 (2.3) | 0.898 | NA | ||||||
| Poor | 346 (90.8) | 232 (89.2) | 114 (94.2) | 224 (90.7) | 82 (90.1) | 224 (90.7) | 40 (93) | ||||||||||
| Unknown | 26 (6.8) | 22 (8.5) | 4 (3.3) | 18 (7.1) | 6 (6.3) | 18 (7.3) | 2 (4.7) | ||||||||||
| T stage | |||||||||||||||||
| Tis-T2 | 107 (28.1) | 85 (32.7) | 22 (18.2) | 0.001 | 73 (29.6) | 23 (25.3) | 0.105 | 73 (29.6) | 11 (25.6) | 0.864 | 28 (9.7) | 18 (9.3) | 10 (10.6) | 0.459 | 3 (6.3) | 25 (10.5) | 0.437 |
| T3 | 177 (46.5) | 121 (46.5) | 56 (46.3) | 118 (47.8) (46.8%) | 37 (40.7) | 118 (47.8) | 22 (51.2) | 208 (72.5) | 144 (74.6) | 64 (68.1)20 | 39 (81.3) | 169 (70.7) | |||||
| T4 | 97 (25.5) | 54 (20.8) | 43 (35.5) | 56 (22.7) | 31 (34.1) | 56 (22.7) | 10 (23.3) | 51 (17.8) | 31 (16.1) | 20 (21.3) | 6 (12.5) | 45 (18.8) | |||||
| N stage | |||||||||||||||||
| N0 | 251 (65.9) | 184 (70.8) | 67 (55.4) | 0.003 | 164 (66.4) | 62 (68.1) | 0.764 | 164 (66.4) | 25 (58.1) | 0.294 | 141 (49.1) | 97 (50.3) | 44 (46.8) | 0.583 | 27 (56.3) | 114 (44.7) | 0.279 |
| N (1-2) | 91 (23.9) | 76 (29.2) | 54 (44.6) | 83 (33.6) | 29 (31.9) | 83 (33.6) | 12 (27.9) | 146 (50.9) | 96 (49.7) | 50 (53.2) | 21 (43.7) | 125 (52.3) | |||||
| M stage | |||||||||||||||||
| M0 | 368 (96.6) | 252 (96.9) | 116 (95.9) (96.3%) | 0.822 | 241 (97.6) | 85 (93.4) | 0.133 | 241 (97.6) | 42 (97.7) | 1.000 | 268 (93.4) | 183 (94.8) | 85 (90.4) | 0.160 | 47 (97.9) | 221 (92.5) | 0.216 |
| M1 | 13 (3.4) | 8 (3.1) | 5 (4.1) | 6 (2.4) | 6 (6.6) | 6 (2.4) | 1 (2.3) | 19 (6.6) | 10 (5.2) | 9 (9.6) | 1 (2.1) | 18 (7.5) | |||||
| Disease stage | |||||||||||||||||
| 0-II | 246 (64.6) | 180 (69.2) | 66 (54.5) | 0.016 | 162 (65.6) | 59 (64.8) | 0.897 | 162 (65.6) | 25 (58.1) | 0.346 | 139 (48.4) | 95 (49.2) | 44 (46.8) | 0.701 | 27 (56.3) | 112 (46.9) | 0.235 |
| III-IV | 135 (35.4) | 80 (30.8) | 55 (45.5) | 85 (34.4) | 32 (35.2) | 85 (34.4) | 18 (41.9) | 148 (51.6) | 98 (50.8) | 50 (53.2) | 21 (43.8) | 127 (53.1) | |||||
| Histological type | |||||||||||||||||
| Adenocarcinoma | 335 (87.9) | 227 (87.3) | 108 (89.3) | 0.706 | 214 (86.6) | 84 (92.3) | 0.130 | 214 (86.6) | 37 (86) | 0.488 | 287 (100) | 193 (100) | 94 (100) | 48 (100) | 239 (100) | ||
| Mucinous/SRCC | 36 (9.4) | 25 (9.6) | 11 (9.1) | 28 (11.3) | 4 (4.4) | 28 (11.3) | 4 (9.3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||||
| Other | 10 (2.6) | 8 (3.1) | 2 (1.7) | 5 (2.0) | 3 (3.3) | 5 (2.0) | 2 (4.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||||
| Treatment | |||||||||||||||||
| Yes | 173 (45.4) | 110 (42.3) | 63 (52.1) | 0.043 | 112 (45.3) | 38 (41.8) | 0.694 | 112 (45.3) | 23 (32.6) | 0.472 | 115 (40.1) | 89 (46.1) | 26 (27.7) | 0.003 | 22 (45.8) | 93 (38.9) | 0.372 |
| No | 158 (41.5) | 119 (45.8) | 39 (32.2) | 105 (42.5) | 39 (42.9) | 105 (42.5) | 14 (53.5) | 172 (59.9) | 104 (53.9) | 68 (72.3) | 26 (54.2) | 146 (61.1) | |||||
| Unknown | 50 (13.1) | 31 (11.9) | 19 (15.7) | 30 (12.1) | 14 (15.4) | 30 (12.1) | 6 (14) | 0 (0) | 0 (0) | ||||||||
| PD-L1 (protein) | |||||||||||||||||
| Low | 247 (64.8) | 177 (73.1) | 70 (26.9) | 0.9764 | NA | ||||||||||||
| High (TIMCs) | 91 (23.9) | 65 (26.9) | 26 (27.1) | ||||||||||||||
| High (TCs) | 43 (11.3) | 18 (9.2) | 25 (26.3) | < 0.001 5 | |||||||||||||
| PD-L1 (mRNA) | |||||||||||||||||
| Low | NA | 48 (16.7) | 31 (16.1) | 17 (18.1) | 0.666 | ||||||||||||
| High | 239 (83.3) | 162 (83.9) | 77 (81.9) | ||||||||||||||
Comparing RON high expression and RON low expression.
Comparing PD-L1 low expression and PD-L1 expression in TIMCs.
Comparing PD-L1 low expression and PD-L1 expression in TCs.
PD-L1 low (both TCs and TIMCs) vs PD-L1 high (TIMCs).
PD-L1 low (both TCs and TIMCs) vs PD-L1 high TCs. Bold entries indicate statistical significance (P < 0.05). GEO: The Gene Expression Omnibus; RON: Recepteur d’origine nantais; PD-L1: Programmed death ligand 1; TCs: Tumor cells; TIMCs: Tumor-infiltrating mononuclear cells; FAHZUSM: The First Affiliated Hospital, Zhejiang University School of Medicine.
Cell lines and reagents
The CRC cell line HT29 was obtained from the American Type Cell Culture (ATCC, Manassas, VA, United States). Flow cytometric analysis revealed that RON and PD-L1 were strongly expressed in HT29 cells (Supplementary Figure 1). Cells were cultured in growth medium supplemented with 10% fetal bovine serum and incubated under standard cell culture conditions at 37 °C and 5% CO2. Rabbit anti-RON antibody (5029) and mouse anti-RON monoclonal antibodies (Zt/f2 and Zt/g4) were used as previously described[28]. Macrophage-stimulating protein (MSP) is an activation factor for RON receptor tyrosine kinase phosphorylation and catalytic activity of a number of signal transduction proteins[29]. Human mature MSP was obtained from R&D Systems (Minneapolis, MN, United States). Antibodies against phospho-tyrosine (P-Tyr-100, Cat # 9411), AKT (Cat # 4685), phospho-AKT (Cat # 4060), extracellular signaling regulated kinase (ERK) 1/2 (Cat # 4695), and phospho-ERK1/2 (p44/42) (Cat # 4376) were obtained from Cell Signaling Technology (Beverly, MA, United States). CK antibody was from ZSGB-BIO (Cat # ZM-0069, Beijing, China). The BMS-777607 RON inhibitor was from Medchem Express (Monmouth Junction, NJ, United States). BMS-777607 was dissolved in dimethyl sulfoxide (DMSO) to a final concentration of 10 mmol/L and stored at -20 °C. The PD-L1 antibody (Cat # 13864) for immunohistochemistry and multiplex immunofluorescence was obtained from Cell Signaling Technology (Beverly, MA, United States). The PD-L1 antibody (Cat # 205921) used for cell experiments was from Abcam (Burlingame, CA, United States). Opal tyramine signal amplification (TSA) staining kit was from PerkinElmer (Hopkinton, MA, United States).
The Gene Expression Omnibus database
Gene expression data for RON and PD-L1 and clinical data for CRC patients are available from the GEO database and accessed through the browser web site (https://geonames.org/)[30]. A total of 290 primary CRC tumors from patients with detailed RON and PD-L1 expression data were selected from the GEO database, based on the completeness of patient clinical data. Only patients with complete tumor characteristics, overall survival (OS), and RNA-seq information, and patients whose tumor samples were obtained prior to treatment were included. The clinicopathologic features of the patients included age, sex, tumor location, histological type, tumor-lymph node-metastasis (TNM) stage, treatment regimen, and OS.
Patients and tissue samples
The CRC specimens used for this study were obtained from 381 CRC patients who were pathologically diagnosed and treated between January 2006 and November 2009 at the FAHZUSM. Clinical data for patients included age, sex, tumor location, histological type, TNM stage, tumor differentiation, treatment pattern, and OS rate (Table 1). CRC tissues were fixed in 10% buffered formalin, embedded in paraffin, and were available for immunohistochemical (IHC) evaluation. Detailed demographic data and clinical features of the FAHZUSM cohort are provided in Table 1. This study was approved by the Ethics Committee of the First Affiliated Hospital, Zhejiang University School of Medicine (reference number: 2017427-1).
Multiplex immunofluorescence
Multiplex immunofluorescence staining of paraffin-embedded sections was performed using Zt/f2 (5 μg/mL) as the primary antibody for RON, rabbit anti-PD-L1 antibody (1:150, 13864, CST) for PD-L1, and mouse anti-CK mAb (1:200, ZM-0069, ZSGB-BIO) for CK, and visualized using the Opal tyramine signal amplification (TSA) staining kit. First, the concentration and sequence of the RON, PD-L1, and CK antibodies were optimized. The primary antibodies/fluorescent dyes for PD-L1/Opal 530, RON/Opal 690, and CK /Opal 520 were applied to the CRC tissues in sequence. Finally, sections were stained with DAPI and mounted with an anti-fading mounting agent. PerkinElmer software version 2.1 was used to analyze multispectral images.
Immunohistochemistry
IHC staining was performed according to standard protocols. Primary antibodies were incubated overnight using a dilution of 1:150 for PD-L1 (13684, CST, United States) and 1:800 for RON. Mouse anti-RON mAb (Zt/f2) was used as previously described[31]. The primary antibody was visualized with diaminobenzidine until a brown precipitate appeared at the antigenic site using EnVision + System-HRP (Dako, Carpentaria, CA, United States). Then, sections were counterstained with hematoxylin.
Evaluation of RON and PD-L1 expression in CRC samples
The IHC-stained sections were independently scored by two pathologists who were blinded to the clinicopathological data. RON expression was determined using a semi-quantitative system. According to the percentage of positive staining area in the whole cancer area, the scoring was as follows: 0 (< 5%), 1 (5%-25%), 2 (26%-50%), 3 (51%-75%), and 4 (> 75%). The staining intensity was scored as 0 (negative), 1 (weak), 2 (medium), or 3 (strong). The total score was obtained by adding the positive proportion score and the staining level score. Samples were categorized as follows: Samples with a final staining score ≤ 4 were considered to be low and those with a score of > 4 were considered to be high for RON expression.
PD-L1 expression was evaluated using an anti-PD-L1 rabbit antibody (13684, CST, United States). A cutoff of 5% for the total proportion of cells that were positive for PD-L1 was used, such that samples with < 5% PD-L1 positive cells were considered to be low and samples with ≥ 5% PD-L1 positive cells were considered to be high for PD-L1 expression. This standard has been established in various types of cancer[32-34].
Phosphorylation and Western blot analysis
The result of Cell Counting Kit 8 illustrated that the half-maximal inhibitory concentration (IC50) of BMS-777607 in HT29 cells at 72 h was 2 μmol/L (Supplementary Figure 2). HT29 cells were treated with 2 nmol/L MSP, 2 μmol/L BMS-777607, or 2 nmol/L MSP + 2 μmol/L BMS-777607 for 24 h. The culture medium was removed and the cells were washed with ice-cold phosphate buffered saline (PBS). Cells were digested with trypsin, collected, and washed with PBS to remove residual trypsin. Cells were lysed in radioimmunoprecipitation (RIPA) buffer, and 25 μg of total protein per sample was separated by 8% SDS-PAGE. Western blot was performed using antibodies against RON, phospho-RON, PD-L1, ERK1/2, phospho-ERK1/2, AKT, and phospho-AKT; GAPDH protein was evaluated as an internal control to ensure equal sample loading. Immunoreactive protein bands were visually detected using enhanced chemiluminescence reagents.
Immunofluorescence analysis
HT29 cells were cultured overnight in a 6-well plate on a cover slide. After treatment with 2 nmol/L MSP, 2 μmol/L BMS-777607, or 2 nmol/L MSP + 2 μmol/L BMS-777607 for 24 h, cells were fixed with 4% paraformaldehyde at 37 °C for 20 min, then washed with PBS five times for 3 min. Cover slides were then blocked with 5% BSA in PBS at room temperature for 30 min. After that, the cells were incubated with primary antibody against PD-L1 (205921, Abcam, United States) and mouse anti-RON mAb (Zt/f2) overnight at 4 °C. Primary antibodies were then removed by washing with PBS five times for 3 min. The cells were then incubated with a fluorescently labeled secondary antibody in the dark at room temperature for 1 h. Excess secondary antibody was removed and the cells were counterstained with DAPI. Slides were mounted with an anti-quenching agent and sealed. The fluorescently labeled cells were observed using a LEICA DMi8 microscope (Leica). Representative images were selected and photographed.
Statistical analysis
Clinical quantitative data are expressed as the mean ± standard deviation (SD) and count data are expressed as constituent ratio (%) or ratio (%). Statistical evaluation was conducted with SPSS 25.0 (IBM Corp., Armonk, NY, United States) and GraphPad Prism v.8 (La Jolla, CA, United States). X-tile 3.6.1 software (Yale University, New Haven, CT, United States) was used to determine the optimal cut-off values for RON and PD-L1 expression in the GEO cohort[35]. χ2 tests were used to analyze relationships between clinicopathological parameters and RON and PD-L1 expression. Differences between quantitative data with a normal distribution were compared using two independent samples t-tests between two groups and one-way analysis of variance among three groups and SNK-q test between groups. Kaplan-Meier method and log-rank test were used for OS analysis. Univariate and multivariate Cox regression analyses were used for identifying the risk factors for OS. A P value < 0.05 was considered statistically significant. All confidence intervals (CIs) are stated at the 95% confidence level.
RESULTS
Expression patterns of RON and PD-L1 in the GEO cohort
In the GEO cohort, X-tile was used to find the optimal cutoff values to divide the data of RON (the upper panel) and PD-L1 (the lower panel) mRNA expression into either low or high expression by selecting the highest χ2 value and the smallest P value of a standard log-rank test. The cut-off values for RON and PD-L1 mRNA in TCs were determined as 7.70 and 4.30, respectively (Figure 1A and B), and the log-rank χ2 values for RON and PD-L1 were 4.544 and 4.078, respectively. Patients in the GEO cohort were stratified according to RON and PD-L1 status: RON ≤ 7.70 and RON > 7.70, and PD-L1 ≤ 4.30 and PD-L1 > 4.30 (Figure 1A and B). We found that the high expression of RON and PD-L1 was associated with a poor prognosis.
Figure 1.
X-tile analysis to determine the optimal cut-off values for RON and PD-L1 expression and survival analysis in the GEO dataset. The optimal cut-off values are highlighted by black circles (left panels) and shown in histograms for the entire cohort (middle panels). Kaplan-Meier survival plots are shown in right panels. A: The optimal cut-off value for RON was 7.50 (χ2 = 4.544, P = 0.033); B: The optimal cut-off value for PD-L1 was 4.30 (χ2 = 4.078, P = 0.043); C: Effect of different RON and PD-L1 expression states on patient survival. aP < 0.05.
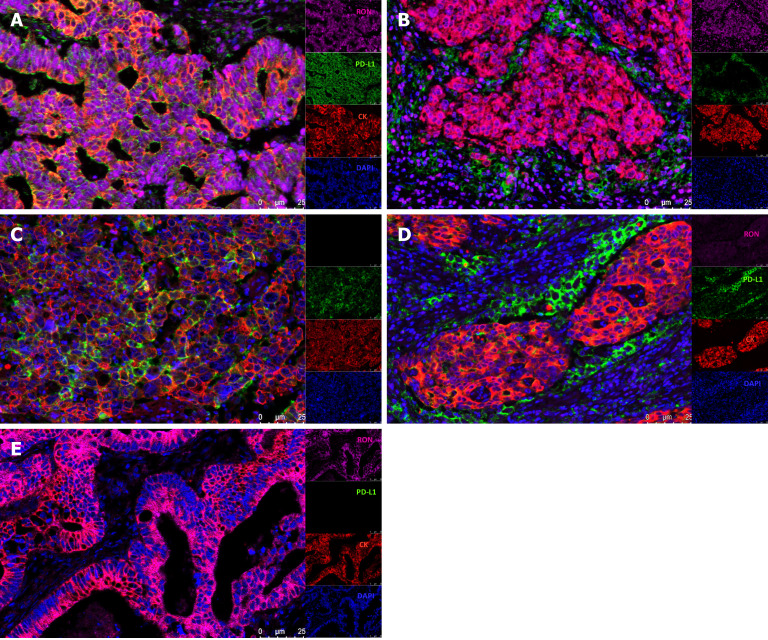
Expression of RON and PD-L1 in CRC tumor tissue
In CRC tissue samples, multiple immunofluorescence staining was used to show the expression patterns of RON in TCs and PD-L1 in the tumor microenvironment. We found that both RON and PD-L1 exhibited membrane-enhanced expression in TCs (Figure 2A); elevated RON expression on the tumor cell membrane was accompanied by enhanced PD-L1 expression in tumor-infiltrating mononuclear cells (TIMCs) (Figure 2B). We also observed cases where PD-L1 expression was enhanced on the tumor cell membrane (Figure 2C) or in TIMCs (Figure 2D), but RON expression was low. Additionally, there were cases where RON expression was enhanced on the TC membrane, but PD-L1 was not expressed in the tumor microenvironment (Figure 2E). In addition, RON and PD-L1 were often accompanied by a cytoplasmic expression of cancer cells. In general, when RON and PD-L1 were enhanced in the tumor cell membrane and cytoplasm, PD-L1 was also expressed in TIMCs. The results of multiplex immunofluorescence are consistent with the evaluation of RON and PD-L1 by immunohistochemical staining (Figure 3A-C).
Figure 2.
Four-color multiplex immunofluorescence staining of paraffin-embedded colorectal cancer tissues. A: High expression of RON and PD-L1 in tumor cells (TCs); B: High expression of RON in TCs and high expression of PD-L1 in tumor-infiltrating mononuclear cells (TIMCs); C: Lack of RON expression and high PD-L1 expression in TCs; D: Low expression of RON in TC and high PD-L1 expression in TIMCs; E: High RON expression in TCs and no PD-L1 expression in either TCs or TIMCs. Blue (DAPI) shows nuclei, green shows PD-L1, pink indicates RON, and red displays CK.
Figure 3.
Immunohistochemical expression of RON and PD-L1 in colorectal cancer tissues. A: High (right) and negative (left) expression of RON in tumor cells (TCs); B: High (right) and negative (left) expression of PD-L1 in tumor-infiltrating mononuclear cells; C: High and negative expression of PD-L1 in TCs (original magnification, × 100 and × 200).
Association of RON and PD-L1 expression with clinicopathological features in the FAHZUSM cohort
In the FAHZUSM cohort, CRC patients were divided into two groups based on high or low expression of RON and PD-L1 detected by IHC staining. In 381 CRC patients, high and low RON expression in TCs was observed in 121 (31.8%) and 260 (68.2%), respectively. High and low expression of PD-L1 in TCs and TIMCs was noted in 43 (11.3%) and 91 (23.9%) patients, respectively, and PD-L1 was lowly expressed in TIMCs in 247 (64.8%) cases. None of the patients had high PD-L1 expression in both TCs and TIMCs. Among all samples expressing RON and PD-L1 in TCs, the proportion with both high RON and high PD-L1 expression was 8.6% (25/290), while the proportion of samples expressing high PD-L1 in TIMCs and high RON in TCs was 7.7% (26/338). Chi-square tests were used to determine the correlation between the expression of RON and PD-L1 in tumor tissues. Compared to samples with low expression of RON, samples with high RON expression levels were more likely to have high levels of PD-L1 in TCs, demonstrating a significant correlation between high RON expression and high PD-L1 expression in TCs (P < 0.001, Table 1). The expression of PD-L1 in TIMCs was not significantly correlated with RON expression in TCs (Table 1).
We compared the clinical characteristics of patient groups categorized based on the expression of RON and PD-L1. High expression of RON was associated with gender, T stage, N stage, disease stage, and treatment. High RON and high PD-L1 expression in TCs was related to T stage (Table 2). High expression of RON and PD-L1 (TIMCs) was associated with T stage, principal diagnosis, histological type, and treatment (P < 0.05; Table 3).
Table 2.
Comparison of RON (tumor cells) and PD-L1 (tumor cells) expression and clinicopathological characteristics of patients with colorectal cancer in the FAHZUSM cohort, n (%)
| Characteristic | Cases |
RON and PD-L1 (TCs) expression in the tumor microenvironment
|
||||
|
RON low/PD-L1 low
|
RON high/PD-L1 low
|
RON low/PD-L1 high
|
RON high/PD-L1 high
|
P
value
|
||
| Number of cases | 290 | 177 | 70 | 18 | 25 | |
| Age (mean ± SD) | 60.89 ± 12.215 | 60.37 ± 12.299 | 62.40 ± 12.518 | 58.39 ± 12.930 | 62.12 ± 10.179 | 0.495 |
| Sex | ||||||
| Man | 161 (55.5) | 108 (61) | 35 (50.0) | 9 (50.0) | 9 (36.0) | 0.061 |
| Women | 129 (44.5) | 68 (39) | 35 (50.0) | 9 (50.0) | 16 (64.0) | |
| Principal diagnosis | s | |||||
| Rectum | 182 (62.8) | 116 (65.5) | 37 (52.9) | 14 (77.8) | 15 (60.0) | 0.149 |
| Colon | 108 (37.2) | 61 (34.5) | 33 (47.1) | 4 (22.2) | 10 (40.0) | |
| Pathological grade | ||||||
| Well/moderate | 6 (2.1) | 3 (1.7) | 2 (2.9) | 0 (0.0) | 1 (4.0) | 0.264 |
| Poor | 264 (9.1) | 158 (89.3) | 66 (94.3) | 16 (88.9) | 24 (96.0) | |
| Unknown | 20 (6.9) | 16 (9.0) | 2 (2.9) | 2 (11.1) | 0 (0.0) | |
| T stage | ||||||
| Tis-T2 | 84 (29) | 64 (36.2) | 9 (12.9) | 5 (27.8) | 6 (24.0) | 0.003 |
| T3 | 140 (48.3) | 82 (46.3) | 36 (51.4) | 11 (61.1) | 11 (44.0) | |
| T4 | 66 (22.8) | 31 (17.5) | 25 (35.7) | 2 (11.1) | 8 (32.0) | |
| N stage | ||||||
| N0 | 238 (66.9) | 125 (70.6) | 39 (55.7) | 12 (66.7) | 13 (66.4) | 0.072 |
| N (1-2) | 118 (33.1) | 52 (29.4) | 31 (44.3) | 6 (33.3) | 12 (33.6) | |
| M stage | ||||||
| M0 | 283 (97.6) | 173 (97.7) | 68 (97.1) | 18 (100) | 24 (96.0) | 0.735 |
| M1 | 7 (2.4) | 4 (2.3) | 2 (2.9) | 0 (0.0) | 1 (4.0) | |
| Stage | ||||||
| 0-II | 187 (64.5) | 123 (69.5) | 39 (55.7) | 12 (66.7) | 13 (52.0) | 0.110 |
| III-IV | 103 (35.5) | 54 (30.5) | 31 (33.3) | 6 (33.3) | 12 (48.0) | |
| Histological type | ||||||
| Adenocarcinoma | 251 (86.6) | 152 (85.9) | 62 (88.6) | 15 (83.3) | 22 (88.0) | 0.493 |
| Mucinous/SRCC | 32 (11) | 21 (11.9) | 7 (10.0) | 1 (5.6) | 3 (12.0) | |
| Other | 7 (2.4) | 4 (2.3) | 1 (1.4) | 2 (11.1) | 0 (0.0) | |
| Treatment | ||||||
| Yes | 135 (46.6) | 83 (46.9) | 22 (31.4) | 6 (33.3) | 12 (48.0) | 0.158 |
| No | 119 (41.0) | 74 (41.8) | 38 (54.3) | 11 (61.1) | 8 (32.0) | |
| Unknown | 36 (12.4) | 20 (11.3) | 10 (14.3) | 1 (5.6) | 5 (20.0) | |
Bold entries indicate statistical significance (P < 0.05). RON: Recepteur d’origine nantais; PD-L1: Programmed death ligand 1; TCs: Tumor cells; FAHZUSM: The First Affiliated Hospital, Zhejiang University School of Medicine.
Table 3.
Comparison of RON (tumor cells) and PD-L1 (tumor-infiltrating mononuclear cells) expression and clinicopathological characteristics of patients with colorectal cancer in the FAHZUSM cohort, n (%)
| Characteristic | Cases |
RON and PD-L1 (TIMCs) expression in the tumor microenvironment
|
||||
|
RON low/PD-L1 low
|
RON high/PD-L1 low
|
RON low/PD-L1 high
|
RON high/PD-L1 high
|
P
value
|
||
| Number of cases | 338 | 177 | 70 | 65 | 26 | |
| Age (mean ± SD) | 61.24 ± 12.555 | 60.37 ± 12.299 | 62.40 ± 12.518 | 61.03 ± 13.286 | 64.58 ± 12.436 | 0.348 |
| Sex | ||||||
| Man | 197 (58.3) | 108 (61) | 35 (50.0) | 40 (61.5) | 14 (52.8) | 0.368 |
| Women | 141 (41.7) | 68 (39) | 35 (50.0) | 25 (38.5) | 12 (46.2) | |
| Principal diagnosis | ||||||
| Rectum | 200 (59.2) | 116 (65.5) | 37 (52.9) | 28 (43.1) | 19 (73.1) | 0.004 |
| Colon | 138 (40.8) | 61 (34.5) | 33 (47.1) | 37 (56.9) | 7 (26.9) | |
| Pathological grade | ||||||
| Well/moderate | 8 (2.4) | 3 (1.7) | 2 (2.9) | 3 (4.6) | 0 (0) | 0.492 |
| Poor | 306 (90.5) | 158 (89.3) | 66 (94.3) | 58 (89.2) | 24 (92.3) | |
| Unknown | 24 (7.1) | 16 (9.0) | 2 (2.9) | 4 (6.2) | 2 (7.7) | |
| T stage | ||||||
| Tis-T2 | 96 (28.4) | 64 (36.2) | 9 (12.9) | 16 (2.6) | 7 (26.9) | 0.002 |
| T3 | 155 (45.9) | 82 (46.3) | 36 (51.4) | 28 (43.1) | 9 (34.6) | |
| T4 | 87 (25.7) | 31 (17.5) | 25 (35.7) | 21 (32.3) | 10 (38.5) | |
| N stage | ||||||
| N0 | 226 (66.9) | 125 (70.6) | 39 (55.7) | 47 (72.3) | 15 (57.7) | 0.075 |
| N (1-2) | 112 (33.1) | 52 (29.4) | 31 (44.3) | 18 (27.7) | 11 (42.3) | |
| M stage | ||||||
| M0 | 326 (96.4) | 173 (97.7) | 68 (97.1) | 61 (93.8) | 24 (92.3) | 0.235 |
| M1 | 12 (3.6) | 4 (2.3) | 2 (2.9) | 4 (2.3) | 2 (7.7) | |
| Stage | ||||||
| 0-II | 221 (65.4) | 123 (69.5) | 39 (55.7) | 45 (69.2) | 14 (53.8) | 0.104 |
| III-IV | 117 (34.6) | 54 (30.5) | 31 (33.3) | 20 (30.8) | 12 (46.2) | |
| Histological type | ||||||
| Adenocarcinoma | 287 (84.9) | 152 (85.9) | 62 (88.6) | 60 (92.3) | 13 (50) | < 0.001 |
| Mucinous/SRCC | 40 (11.8) | 21 (11.9) | 7 (10.0) | 3 (4.6) | 9 (34.6) | |
| Other | 11 (3.3) | 4 (2.3) | 1 (1.4) | 2 (3.1) | 4 (15.4) | |
| Treatment | ||||||
| Yes | 298 (88.2) | 83 (46.9) | 22 (31.4) | 30 (46.2) | 24 (92.3) | < 0.001 |
| No | 32 (9.5) | 74 (41.8) | 38 (54.3) | 25 (38.5) | 1 (3.8) | |
| Unknown | 8 (2.4) | 20 (11.3) | 10 (14.3) | 10 (15.4) | 1 (3.8) | |
Bold entries indicate statistical significance (P < 0.05). RON: Recepteur d’origine nantais; PD-L1: Programmed death ligand 1; TCs: Tumor cells; TIMCs: Tumor-infiltrating mononuclear cells; FAHZUSM: The First Affiliated Hospital, Zhejiang University School of Medicine.
Prognostic significance of RON and PD-L1 expression in CRC
In the GEO cohort, univariate Cox regression analysis showed that age, T stage, M stage, disease stage, RON, and PD-L1 (TCs) expression were significantly correlated with a poor prognosis in CRC patients (P < 0.05). Multivariate analysis after adjustment showed that only age, T stage, and M stage were independent prognostic factors for OS in CRC patients (P < 0.05); disease stage, RON expression, and PD-L1 expression were not significant factors in the multivariate analysis (P > 0.05; Table 4). Kaplan-Meier analysis showed that high expression of RON or PD-L1 (TCs), and both high RON and PD-L1 expression were all associated with a poor OS (P < 0.05; Figure 1A-C). High expression of RON was associated with patient age and treatment type, and high expression of PD-L1 (TCs) was associated with the primary site of the tumor (P < 0.05; Table 1).
Table 4.
Univariate and multivariate Cox proportional hazard analyses of overall survival in patients with colorectal cancer in the FAHZUSM and Gene Expression Omnibus cohorts
| Variable |
FAHZUSM cohort
|
GEO cohort
|
||||||
| Univariate analysis, HR (95%CI) | P value | Multivariate analysis, HR (95%CI) | P value | Univariate analysis, HR (95%CI) | P value | Multivariate analysis, HR (95%CI) | P value | |
| Age (mean ± SD) | 1.029 (1.011-1.048) | 0.002 | 1.031 (1.011-1.050) | 0.002 | 1.025 (1.009-1.041) | 0.002 | 1.028 (1.012-1.045) | 0.001 |
| Gender | ||||||||
| Male | 1.000 | 0.011 | 1.000 | 0.008 | 1.000 | 0.293 | 1.000 | 0.076 |
| Female | 0.562 (0.362-0.874) | 0.527 (0.328-0.847) | 0.814 (0.555-1.194) | 0.698 (0.469-1.039) | ||||
| Principal diagnosis | ||||||||
| Rectum | 1.000 | 0.298 | 1.000 | 0.318 | 1.000 | 0.688 | 1.000 | 0.544 |
| Colon | 0.796 (0.518-1.224) | 0.790 (0.497-1.255) | 1.081 (0.738-1.585) | 0.882 (0.589-1.322) | ||||
| Histological type | ||||||||
| Adenocarcinoma | 1.000 | 0.408 | 1.000 | 0.387 | NA | |||
| Mucinous/SRCC | 2.464 (0.343-17.710) | 2.720 (0.263-28.122) | ||||||
| Unknown | 3.355 (0.433-25.986) | 1.232 (0.129-11.795) | ||||||
| T stage | ||||||||
| Tis-T2 | 1.000 | < 0.001 | 1.000 | 0.003 | 1.000 | 0.001 | 1.000 | 0.007 |
| T3 | 0.211 (0.108-0.413) | 0.298 (0.141-0.632) | 0.333 (0.145-0.766) | 0.381 (0.159-0.914) | ||||
| T4 | 0.503 (0.325-0.781) | 0.596 (0.361-0.897) | 0.455 (0.292-0.709) | 0.476 (0.295-0.769) | ||||
| N stage | ||||||||
| N0 | 1.000 | < 0.001 | 1.000 | 0.111 | 1.000 | 0.062 | 1.000 | 0.141 |
| N (1-2) | 3.156 (2.083-4.783) | 5.376 (0.678-42.660) | 1.435 (0.982-2.097) | 0.306 (0.063-1.479) | ||||
| M stage | ||||||||
| M0 | 1.000 | < 0.001 | 1.000 | 0.039 | 1.000 | < 0.001 | 1.000 | 0.008 |
| M1 | 4.338 (2.094-8.985) | 2.445 (1.048-5.701) | 3.546 (2.013-6.247) | 2.481 (1.269-4.852) | ||||
| Stage | ||||||||
| 0-II | 1.000 | < 0.001 | 1.000 | 0.406 | 1.000 | 0.029 | 1.000 | 0.099 |
| III-IV | 3.102 (2.044-4.708) | 0.409 (0.050-3.366) | 1.530 (1.045-2.242) | 3.924 (0.774-19.888) | ||||
| Pathological grade | ||||||||
| Well/moderate | 1.000 | < 0.001 | 1.000 | 0.003 | NA | |||
| Poor | 7.689 (2.434-24.290) | 4.044 (1.103-14.830) | ||||||
| Unknown | 1.266 (0.513-3.126) | 0.375 (0.104-1.357) | ||||||
| RON (protein) | ||||||||
| Low | 1.000 | 0.001 | 1.000 | 0.012 | 1.000 | 0.035 | 1.000 | 0.466 |
| High | 2.060 (1.364-3.112) | 1.788 (1.138-2.808) | 1.515 (1.030-2.228) | 1.170 (0.767-1.785) | ||||
| RON (mRNA) | ||||||||
| Low | NA | 1.000 | 0.035 | 1.000 | 0.466 | |||
| High | 1.515 (1.030-2.228) | 1.170 (0.767-1.785) | ||||||
| PD-L1 (protein) | ||||||||
| Low | 1.000 | < 0.001 | 1.000 | 0.001 | NA | |||
| High (TIMCs) | 0.544 (0.293-1.011) | 0.676 (0.350-1.304) | ||||||
| High (TCs) | 1.325 (0.669-2.511) | 1.654 (0.819-3.338) | ||||||
| PD-L1 (mRNA) | ||||||||
| Low | NA | 1.000 | 0.047 | 1.000 | 0.083 | |||
| High | 1.835 (1.007-3.345) | 1.719 (0.931-3.173) | ||||||
All variables are adjusted by the Cox proportional hazard model. Bold entries indicate statistical significance (P < 0.05). GEO: The Gene Expression Omnibus; RON: Recepteur d’origine nantais; PD-L1: Programmed death ligand 1; TCs: Tumor cells; TIMCs: Tumor-infiltrating mononuclear cells; FAHZUSM: The First Affiliated Hospital, Zhejiang University School of Medicine.
In the FAHZUSM cohort, Kaplan-Meier analysis showed that high expression of RON in TCs, high PD-L1 expression in TCs, or high PD-L1 expression in TIMCs in CRC tissue samples was correlated with a lower OS (P < 0.05) (Figure 4A-C). Univariate Cox regression analysis showed that age, gender, TNM stage, disease stage, pathological grade, RON expression, and PD-L1 expression were associated with a poor OS in patients with CRC (P < 0.05). Multivariate analysis after adjustment showed that age, gender, T stage, M stage, pathological grade, RON expression, and PD-L1 expression remained independent prognostic factors for OS in CRC patients (P < 0.05), while N and disease stage were not significant (P > 0.05; Table 4). We further analyzed the relationship between OS and RON and PD-L1 expression in the tumor microenvironment. High expression of both RON and PD-L1 in TCs predicted a significantly worse OS, and high RON expression in TCs and high PD-L1 expression in TIMCs were associated with a significantly worse prognosis (P < 0.001; Figure 4D and E).
Figure 4.
Kaplan-Meier analysis of overall survival of patients with colorectal cancer stratified by RON and/or PD-L1 expression. A: Overall survival (OS) according to RON expression in tumor cells (TCs); B: OS according to PD-L1 expression in TCs; C: OS according to PD-L1 expression in tumor-infiltrating mononuclear cells (TIMCs); D: OS according to RON and PD-L1 expression in TCs; E: OS according to RON expression in TCs and PD-L1 expression in TIMCs. aP < 0.05, bP < 0.01, cP < 0.001.
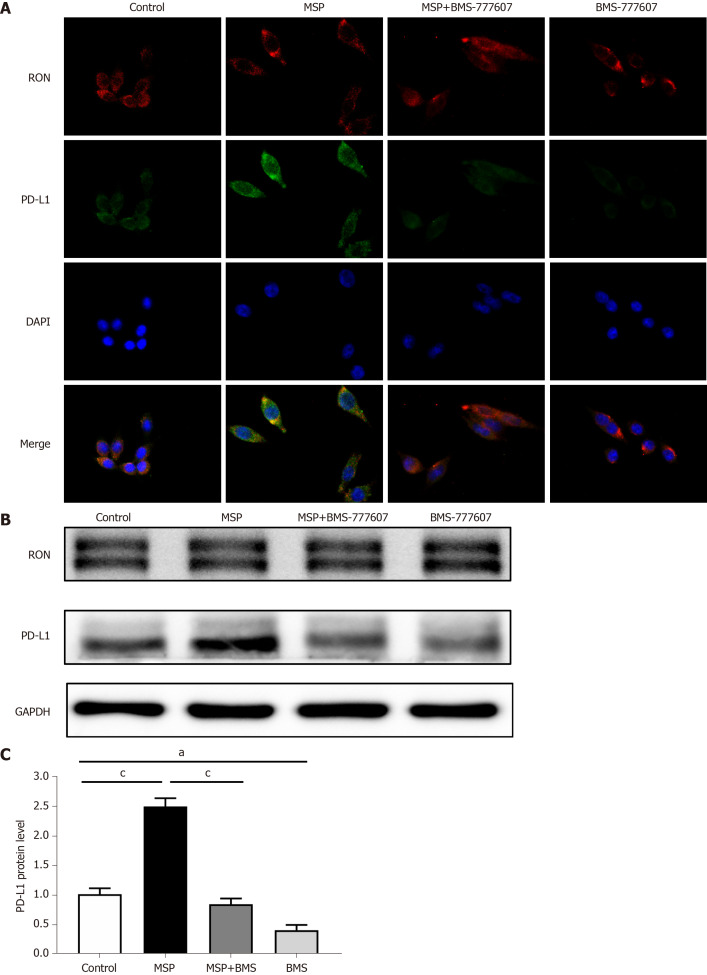
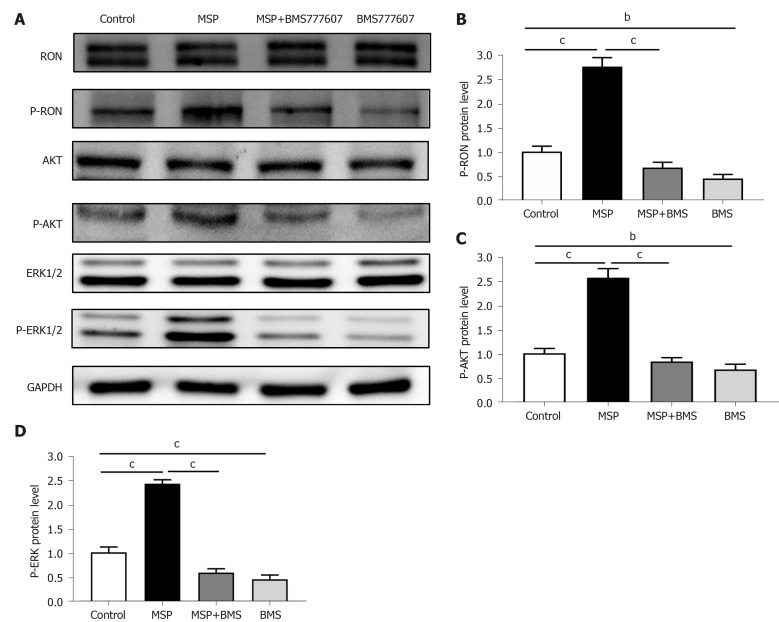
Effects of regulating RON phosphorylation on PD-L1 expression
In order to study the relationship between RON and PD-L1 in CRC cells, HT29 cells (following serum starvation) were treated with MSP, BMS-777607, or MSP + BMS-777607 for 24 h. The effects of treatment on RON and PD-L1 expression were analyzed by cellular immunofluorescence. Activating RON phosphorylation promoted PD-L1 expression, while inhibiting RON phosphorylation down-regulated PD-L1 expression (Figure 5A). This result was confirmed by analysis of protein expression by Western blot (P < 0.05; Figure 5B and C). In addition, we found that RON inhibition significantly reduced the phosphorylation of AKT and ERK1/2, which signal downstream of RON (Figure 6A-D).
Figure 5.
Expression of RON and PD-L1 in HT29 cells after treatment with 2 nmol/L MSP, 2 nmol/L MSP + 2 μmol/L BMS-777607, or 2 μmol/L BMS-777607. A: Cellular immunofluorescence indicating the expression of RON and PD-L1 after treatment of HT29 cells with 2 nmol/L MSP, 2 nmol/L MSP + 2 μmol/L BMS-777607, or 2 μmol/L BMS-777607 for 24 h, respectively. DAPI indicates nuclei (blue color), FITC indicates PD-L1 (green color), and PE indicates RON (red color). Original magnification × 400 (all photomicrographs). B-C: HT29 cells were treated with 2 nmol/L MSP, 2 nmol/L MSP + 2 μmol/L BMS-777607, or 2 μmol/L BMS-777607 for 24 h, and the expression of RON and PD-L1 was detected by Western blot and quantified according to the immunoblots. aP < 0.05, bP < 0.01, cP < 0.001.
Figure 6.
Expression of RON and PD-L1, and activation of signaling pathways in HT29 cells. A: HT29 cells were treated with 2 nmol/L MSP, 2 nmol/L MSP + 2 μmol/L BMS-777607, or 2 μmol/L BMS-777607 for 1 h. The proteins analyzed include RON, phosphorylated RON, AKT, ERK1/2, phosphorylated AKT, and phosphorylated-ERK1/2. GAPDH was used as a loading control; B-D: The expression of p-RON, p-AKT, and p-ERK1/2 was detected by Western blot and quantified. aP < 0.05, bP < 0.01, cP < 0.001.
DISCUSSION
The application of PD-L1 immunotherapy in cancer treatment is becoming more and more important, but its therapeutic effect has been limited in CRC. This may be due in part to the prevalence of the mismatch repair (MMR) proficient or microsatellite stabilization (MSS) subtypes of CRC[36]. In addition, c-MET plays an important role in regulating PD-L1 expression[37,38]. Therefore, RON may promote the expression of PD-L1 in tumor tissue to affect the efficacy of PD-L1 immunosuppressants.
RON and PD-L1 play important roles in cancer initiation and development and are important targets for tumor therapy. However, few studies have explored the relationship between RON and PD-L1 expression in CRC and the impact that RON and PD-L1 expression patterns may have on pathological characteristics and disease outcomes. It was our hypothesis that activation of the RON receptor tyrosine kinase may promote the expression of PD-L1 in CRC tissue and impair the efficacy of PD-L1 immunotherapy. The purpose of our study was to analyze the expression and clinical significance of RON and PD-L1 in the tumor microenvironment in CRC samples, and to determine whether RON can regulate the expression of PD-L1 in CRC. We discovered that high expression of both RON and PD-L1 in the tumor microenvironment was associated with the poorest OS rate compared to CRC tumors with other RON and PD-L1 expression states. RON and PD-L1 were independent prognostic factors for OS in CRC patients. In addition, we showed that RON phosphorylation led to increased expression of PD-L1 in CRC cells, and that inhibiting RON phosphorylation can reduce PD-L1 expression.
We used publicly available data from the GEO database to investigate the relationship between RON and PD-L1 expression and clinical outcomes in CRC. We used X-tile to determine the optimal cut-off values for RON and PD-L1 levels in the GEO cohort. Kaplan-Meier survival analysis revealed a positive correlation of high RON or PD-L1 expression with worse OS, and high expression of RON and PD-L1 together was associated with the worst OS for CRC patients. However, RON and PD-L1 levels in the GEO dataset were determined by RNA sequencing using RNA extracted from tumor tissue to quantify the expression level in TCs, and it is difficult to determine the interactions between RON and PD-L1 that may arise within the tumor microenvironment from the GEO dataset. Therefore, we used the FAHZUSM cohort, a larger patient cohort with pathological tumor samples, to further study the expression of RON and PD-L1 in CRC tissues and to determine the pathological significance of elevated RON and PD-L1 expression in the tumor microenvironment.
Dysregulation of RON and PD-L1 signal transduction is a key feature of many tumors. Our results and previous studies demonstrated that high expression of RON or PD-L1 in CRC tumor tissues correlated with the extent of primary tumor, lymph node metastasis, and distant metastasis[39,40]. Furthermore, high expression of RON or PD-L1 in the tumor microenvironment was associated with a poor survival in CRC patients[22,39-42].
We demonstrated that high expression of both RON and PD-L1 in TCs was associated with a poor OS in CRC patients. Interestingly, the expression levels of RON were positively correlated with those of PD-L1 in TCs, which has not been previously reported. This may be related to the fact that RON can regulate both the production of and response to IFN-γ[43]. In TCs, long-term continuous activation of IFN-γ can mediate adaptive resistance to PD-L1 tumor immunosuppression; high expression of RON may attenuate resistance, restore the efficacy of PD-L1 targeted therapy, and may even have a promoting effect on the expression of PD-L1 by inhibiting the production of IFN-γ[10,43-45].
MEK/ERK and PI3K/AKT signaling pathways play a central role towards understanding the mechanisms underlying tumorigenesis and tumor development, prevention, and treatment. For example, autophagy caused by the activation of PI3K/AKT pathway plays a significant role in tumors[46,47]. In our study, we demonstrated that RON phosphorylation increased the expression of PD-L1 in CRC cells, proving that RON activation promotes the expression of PD-L1, likely acting through the downstream AKT and ERK1/2 signaling pathways. Previous studies have shown that there is crosstalk between RON phosphorylation and other receptors, which can affect the surface expression of other receptors[22]. Phosphorylation of RON activates downstream oncogenic signaling pathways, such as the RAS-ERK and PI3K-AKT pathways, thereby promoting tumor initiation, growth, invasion, and metastasis[20]. Treatment with BRAF inhibitors or MEK inhibitors, or down-regulation of ERK1/2 can lead to down-regulation of PD-L1 expression in TCs[48]. Thus, RON phosphorylation may promote the expression of PD-L1 in TCs through the RAS-ERK signaling pathway. In addition, PTEN interacts with RTK-dependent signals at multiple levels[48], and has an antagonistic effect on PI3K, which plays an important role in mediating RTK-dependent cell signaling and tumor immune escape[10,48,49]. Therefore, RON phosphorylation may interact with PTEN to activate the PI3K-AKT signaling pathway, thereby promoting PD-L1 expression in TCs.
TIMCs are regarded as an indicator of host immune response to a tumor, and have long been considered an unfavorable prognostic marker in CRC[41,42]. Moreover, RON expression plays an important role in anti-tumor immune responses[27,50]. Previous studies also have shown that RON activation reduced the polarization of inflammatory M1 macrophages and induced the differentiation of immunosuppressive M2 macrophages. M2 macrophages promote PD-L1 expression through autocrine VEGF signaling[51]. In our study, we demonstrated that high expression of both RON and PD-L1 (TIMCs) was associated with a poor OS in patients with CRC. Thus, high expression of RON may impair the anti-tumor immune response by promoting the expression of PD-L1 in TIMCs, leading to tumor growth, invasion, and metastasis.
There were some limitations in this study. First, although we have analyzed a large patient cohort, this was a retrospective analysis and there is the potential for selection bias. Second, we did not evaluate which specific immune cell components in TIMCs expressed PD-L1. Third, although we have preliminarily studied that RON phosphorylation promotes the expression of PD-L1 in CRC cells, the mechanism by which RON promotes PD-L1 expression still needs to be further studied.
CONCLUSION
In summary, high expression of RON and/or PD-L1 in CRC samples is associated with a poor prognosis in CRC patients. The expression status of RON and PD-L1 may be helpful as biomarkers to evaluate the prognosis of patients with CRC. In addition, RON phosphorylation can promote the expression of PD-L1 in CRC cells, possibly through activation of the AKT and ERK1/2 signaling pathways, which provides a new idea for the immunotherapy of CRC.
ARTICLE HIGHLIGHTS
Research background
Programmed death ligand 1 (PD-L1) protein expression on immune cells enables tumor cells to evade the immune system in a wide variety of malignancies. However, the efficacy of PD-L1 immunosuppressive agents in colorectal cancer (CRC) is poor. The recepteur d’origine nantais (RON) receptor tyrosine kinase plays an important role in regulating tumor immunity.
Research motivation
The poor anti-tumor effect of PD-1 inhibitors in CRC promoted the research on the mechanism of PD-1 expression, so as to improve the therapeutic effect of PD-1 inhibitors on CRC.
Research objectives
The present study aimed to identify patterns of RON and PD-L1 expression and explore the clinical significance of these patterns in CRC.
Research methods
The gene expression data from the Gene Expression Omnibus database (GEO; n = 290) and patients at the First Affiliated Hospital, Zhejiang University School of Medicine (FAHZUSM; n = 381) were analyzed to determine the prognostic value of RON and PD-L1 expression in the tumor microenvironment of CRC. HT29 cells were treated with BMS-777607 to explore the relationship between RON activity and PD-L1 expression. Signaling pathways and protein expression perturbed by RON inhibition were evaluated by cellular immunofluorescence and Western blot.
Research results
In the GEO patient cohort, the cut-off values for RON and PD-L1 expression were determined to be 7.70 and 4.30, respectively. Stratification of patients based on these cutoffs demonstrated that high expression of RON and PD-L1 was associated with a poor prognosis. In the FAHZUSM cohort, rates of high expression of RON in tumor cells, high PD-L1 expression in tumor cells and tumor infiltrating monocytes, and both high RON and high PD-L1 expression in the tumor microenvironment were 121 (32%), 43 (11%), 91 (24%), and 51 (13.4%), respectively. High expression of RON was significantly correlated with high expression of PD-L1 in the tumor cell compartment (P < 0.001). High expression of RON and PD-L1 were independent prognostic factors for poorer overall survival. Concurrent high expression of both RON and PD-L1 in the tumor microenvironment was significantly associated with a poor prognosis. In vitro, BMS-777607 inhibited the phosphorylation of RON and PD-L1 expression, and attenuated the activation of the ERK1/2 and AKT signaling pathways in CRC cells.
Research conclusions
RON, PD-L1, and their crosstalk are significant in predicting the prognostic value of CRC. Moreover, phosphorylation of RON upregulates PD-L1 expression, which provides a novel approach to immunotherapy in CRC.
Research perspectives
The study of RON and PD-L1 expression will help improve the efficacy of PD-L1 immunosuppressive agents for CRC.
Footnotes
Institutional review board statement: The study was reviewed and approved by the First Affiliated Hospital, Zhejiang University School of Medicine (reference number: 2017427-1).
Conflict-of-interest statement: The authors confirm that there are no known conflicts of interest associated with this publication. The manuscript has been read and approved by all authors and there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of authors.
ARRIVE guidelines statement: The authors have read the ARRIVE guidelines, and the manuscript was prepared and revised according to the ARRIVE guidelines.
Manuscript source: Invited manuscript
Peer-review started: August 9, 2020
First decision: August 22, 2020
Article in press: September 18, 2020
Specialty type: Pathology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Koustas E, Zhu Y S-Editor: Gong ZM L-Editor: Wang TQ P-Editor: Li JH
Contributor Information
Yi-Zhi Liu, Department of Cancer Biology Research, State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, National Clinical Research Center for Infectious Diseases, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, Zhejiang Province, China.
Da-Ting Han, Department of Cancer Biology Research, State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, National Clinical Research Center for Infectious Diseases, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, Zhejiang Province, China.
Dan-Rong Shi, Department of Cancer Biology Research, State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, National Clinical Research Center for Infectious Diseases, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, Zhejiang Province, China.
Bo Hong, Department of Pathology, The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, Zhejiang Province, China.
Yun Qian, Department of Clinical Laboratory, The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, Zhejiang Province, China.
Zhi-Gang Wu, Department of Cancer Biology Research, State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, National Clinical Research Center for Infectious Diseases, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, Zhejiang Province, China.
Shu-Hao Yao, Department of Stomatology, Wenzhou Medical University Renji College, Wenzhou 325035, Zhejiang Province, China.
Tao-Ming Tang, Department of Cancer Biology Research, State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, National Clinical Research Center for Infectious Diseases, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, Zhejiang Province, China.
Ming-Hai Wang, Cancer Biology Research Center and Department of Pharmaceutical Sciences, School of Pharmacy, Texas Tech University Health Sciences Center, Amarillo, TX 79106, United States.
Xiang-Ming Xu, Department of Cancer Biology Research, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, Zhejiang Province, China.
Hang-Ping Yao, Department of Cancer Biology Research, State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, National Clinical Research Center for Infectious Diseases, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, Zhejiang Province, China. yaohangping@zju.edu.cn.
Data sharing statement
All data generated or analyzed during this study are included in the published paper. More details can be provided on request.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Arshad U, Sutton PA, Ashford MB, Treacher KE, Liptrott NJ, Rannard SP, Goldring CE, Owen A. Critical considerations for targeting colorectal liver metastases with nanotechnology. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2020;12:e1588. doi: 10.1002/wnan.1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell. 2015;27:450–461. doi: 10.1016/j.ccell.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Masugi Y, Nishihara R, Yang J, Mima K, da Silva A, Shi Y, Inamura K, Cao Y, Song M, Nowak JA, Liao X, Nosho K, Chan AT, Giannakis M, Bass AJ, Hodi FS, Freeman GJ, Rodig S, Fuchs CS, Qian ZR, Ogino S. Tumour CD274 (PD-L1) expression and T cells in colorectal cancer. Gut. 2017;66:1463–1473. doi: 10.1136/gutjnl-2016-311421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamanishi J, Mandai M, Matsumura N, Abiko K, Baba T, Konishi I. PD-1/PD-L1 blockade in cancer treatment: perspectives and issues. Int J Clin Oncol. 2016;21:462–473. doi: 10.1007/s10147-016-0959-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong H, Zhu G, Tamada K, Chen L. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med. 1999;5:1365–1369. doi: 10.1038/70932. [DOI] [PubMed] [Google Scholar]
- 7.Baeten JM, Palanee-Phillips T, Brown ER, Schwartz K, Soto-Torres LE, Govender V, Mgodi NM, Matovu Kiweewa F, Nair G, Mhlanga F, Siva S, Bekker LG, Jeenarain N, Gaffoor Z, Martinson F, Makanani B, Pather A, Naidoo L, Husnik M, Richardson BA, Parikh UM, Mellors JW, Marzinke MA, Hendrix CW, van der Straten A, Ramjee G, Chirenje ZM, Nakabiito C, Taha TE, Jones J, Mayo A, Scheckter R, Berthiaume J, Livant E, Jacobson C, Ndase P, White R, Patterson K, Germuga D, Galaska B, Bunge K, Singh D, Szydlo DW, Montgomery ET, Mensch BS, Torjesen K, Grossman CI, Chakhtoura N, Nel A, Rosenberg Z, McGowan I, Hillier S MTN-020–ASPIRE Study Team. Use of a Vaginal Ring Containing Dapivirine for HIV-1 Prevention in Women. N Engl J Med. 2016;375:2121–2132. doi: 10.1056/NEJMoa1506110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prall F, Hühns M. The PD-1 expressing immune phenotype of T cell exhaustion is prominent in the 'immunoreactive' microenvironment of colorectal carcinoma. Histopathology. 2017;71:366–374. doi: 10.1111/his.13231. [DOI] [PubMed] [Google Scholar]
- 9.Ji S, Xu Y, Han D, Peng X, Lu X, Brockmeyer NH, Wu N. Changes in Lipid Indices in HIV+ Cases on HAART. Biomed Res Int. 2019;2019:2870647. doi: 10.1155/2019/2870647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalbasi A, Ribas A. Tumour-intrinsic resistance to immune checkpoint blockade. Nat Rev Immunol. 2020;20:25–39. doi: 10.1038/s41577-019-0218-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feng D, Qin B, Pal K, Sun L, Dutta S, Dong H, Liu X, Mukhopadhyay D, Huang S, Sinicrope FA. BRAFV600E-induced, tumor intrinsic PD-L1 can regulate chemotherapy-induced apoptosis in human colon cancer cells and in tumor xenografts. Oncogene. 2019;38:6752–6766. doi: 10.1038/s41388-019-0919-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peng S, Wang R, Zhang X, Ma Y, Zhong L, Li K, Nishiyama A, Arai S, Yano S, Wang W. EGFR-TKI resistance promotes immune escape in lung cancer via increased PD-L1 expression. Mol Cancer. 2019;18:165. doi: 10.1186/s12943-019-1073-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, Powderly JD, Carvajal RD, Sosman JA, Atkins MB, Leming PD, Spigel DR, Antonia SJ, Horn L, Drake CG, Pardoll DM, Chen L, Sharfman WH, Anders RA, Taube JM, McMiller TL, Xu H, Korman AJ, Jure-Kunkel M, Agrawal S, McDonald D, Kollia GD, Gupta A, Wigginton JM, Sznol M. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, Drake CG, Camacho LH, Kauh J, Odunsi K, Pitot HC, Hamid O, Bhatia S, Martins R, Eaton K, Chen S, Salay TM, Alaparthy S, Grosso JF, Korman AJ, Parker SM, Agrawal S, Goldberg SM, Pardoll DM, Gupta A, Wigginton JM. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366:2455–2465. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ng C, Li H, Wu WKK, Wong SH, Yu J. Genomics and metagenomics of colorectal cancer. J Gastrointest Oncol. 2019;10:1164–1170. doi: 10.21037/jgo.2019.06.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arai H, Battaglin F, Wang J, Lo JH, Soni S, Zhang W, Lenz HJ. Molecular insight of regorafenib treatment for colorectal cancer. Cancer Treat Rev. 2019;81:101912. doi: 10.1016/j.ctrv.2019.101912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ledys F, Klopfenstein Q, Truntzer C, Arnould L, Vincent J, Bengrine L, Remark R, Boidot R, Ladoire S, Ghiringhelli F, Derangere V. RAS status and neoadjuvant chemotherapy impact CD8+ cells and tumor HLA class I expression in liver metastatic colorectal cancer. J Immunother Cancer. 2018;6:123. doi: 10.1186/s40425-018-0438-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh A, Greninger P, Rhodes D, Koopman L, Violette S, Bardeesy N, Settleman J. A gene expression signature associated with "K-Ras addiction" reveals regulators of EMT and tumor cell survival. Cancer Cell. 2009;15:489–500. doi: 10.1016/j.ccr.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ronsin C, Muscatelli F, Mattei MG, Breathnach R. A novel putative receptor protein tyrosine kinase of the met family. Oncogene. 1993;8:1195–1202. [PubMed] [Google Scholar]
- 20.Yao HP, Zhou YQ, Zhang R, Wang MH. MSP-RON signalling in cancer: pathogenesis and therapeutic potential. Nat Rev Cancer. 2013;13:466–481. doi: 10.1038/nrc3545. [DOI] [PubMed] [Google Scholar]
- 21.Graves-Deal R, Bogatcheva G, Rehman S, Lu Y, Higginbotham JN, Singh B. Broad-spectrum receptor tyrosine kinase inhibitors overcome de novo and acquired modes of resistance to EGFR-targeted therapies in colorectal cancer. Oncotarget. 2019;10:1320–1333. doi: 10.18632/oncotarget.26663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee CT, Chow NH, Su PF, Lin SC, Lin PC, Lee JC. The prognostic significance of RON and MET receptor coexpression in patients with colorectal cancer. Dis Colon Rectum. 2008;51:1268–1274. doi: 10.1007/s10350-008-9297-1. [DOI] [PubMed] [Google Scholar]
- 23.Schroeder GM, An Y, Cai ZW, Chen XT, Clark C, Cornelius LA, Dai J, Gullo-Brown J, Gupta A, Henley B, Hunt JT, Jeyaseelan R, Kamath A, Kim K, Lippy J, Lombardo LJ, Manne V, Oppenheimer S, Sack JS, Schmidt RJ, Shen G, Stefanski K, Tokarski JS, Trainor GL, Wautlet BS, Wei D, Williams DK, Zhang Y, Zhang Y, Fargnoli J, Borzilleri RM. Discovery of N-(4-(2-amino-3-chloropyridin-4-yloxy)-3-fluorophenyl)-4-ethoxy-1-(4-fluorophenyl)-2-oxo-1,2-dihydropyridine-3-carboxamide (BMS-777607), a selective and orally efficacious inhibitor of the Met kinase superfamily. J Med Chem. 2009;52:1251–1254. doi: 10.1021/jm801586s. [DOI] [PubMed] [Google Scholar]
- 24.Wang J, Rajput A, Kan JL, Rose R, Liu XQ, Kuropatwinski K, Hauser J, Beko A, Dominquez I, Sharratt EA, Brattain L, Levea C, Sun FL, Keane DM, Gibson NW, Brattain MG. Knockdown of Ron kinase inhibits mutant phosphatidylinositol 3-kinase and reduces metastasis in human colon carcinoma. J Biol Chem. 2009;284:10912–10922. doi: 10.1074/jbc.M809551200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xu XM, Wang D, Shen Q, Chen YQ, Wang MH. RNA-mediated gene silencing of the RON receptor tyrosine kinase alters oncogenic phenotypes of human colorectal carcinoma cells. Oncogene. 2004;23:8464–8474. doi: 10.1038/sj.onc.1207907. [DOI] [PubMed] [Google Scholar]
- 26.Yao HP, Zhou YQ, Ma Q, Guin S, Padhye SS, Zhang RW, Wang MH. The monoclonal antibody Zt/f2 targeting RON receptor tyrosine kinase as potential therapeutics against tumor growth-mediated by colon cancer cells. Mol Cancer. 2011;10:82. doi: 10.1186/1476-4598-10-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eyob H, Ekiz HA, Welm AL. RON promotes the metastatic spread of breast carcinomas by subverting antitumor immune responses. Oncoimmunology. 2013;2:e25670. doi: 10.4161/onci.25670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eyob H, Ekiz HA, Derose YS, Waltz SE, Williams MA, Welm AL. Inhibition of ron kinase blocks conversion of micrometastases to overt metastases by boosting antitumor immunity. Cancer Discov. 2013;3:751–760. doi: 10.1158/2159-8290.CD-12-0480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Danilkovitch A, Donley S, Skeel A, Leonard EJ. Two independent signaling pathways mediate the antiapoptotic action of macrophage-stimulating protein on epithelial cells. Mol Cell Biol. 2000;20:2218–2227. doi: 10.1128/mcb.20.6.2218-2227.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clough E, Barrett T. The Gene Expression Omnibus Database. Methods Mol Biol. 2016;1418:93–110. doi: 10.1007/978-1-4939-3578-9_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feng L, Yao HP, Wang W, Zhou YQ, Zhou J, Zhang R, Wang MH. Efficacy of anti-RON antibody Zt/g4-drug maytansinoid conjugation (Anti-RON ADC) as a novel therapeutics for targeted colorectal cancer therapy. Clin Cancer Res. 2014;20:6045–6058. doi: 10.1158/1078-0432.CCR-14-0898. [DOI] [PubMed] [Google Scholar]
- 32.Herbst RS, Soria JC, Kowanetz M, Fine GD, Hamid O, Gordon MS, Sosman JA, McDermott DF, Powderly JD, Gettinger SN, Kohrt HE, Horn L, Lawrence DP, Rost S, Leabman M, Xiao Y, Mokatrin A, Koeppen H, Hegde PS, Mellman I, Chen DS, Hodi FS. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature. 2014;515:563–567. doi: 10.1038/nature14011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fehrenbacher L, Spira A, Ballinger M, Kowanetz M, Vansteenkiste J, Mazieres J, Park K, Smith D, Artal-Cortes A, Lewanski C, Braiteh F, Waterkamp D, He P, Zou W, Chen DS, Yi J, Sandler A, Rittmeyer A POPLAR Study Group. Atezolizumab versus docetaxel for patients with previously treated non-small-cell lung cancer (POPLAR): a multicentre, open-label, phase 2 randomised controlled trial. Lancet. 2016;387:1837–1846. doi: 10.1016/S0140-6736(16)00587-0. [DOI] [PubMed] [Google Scholar]
- 34.Rosenberg JE, Hoffman-Censits J, Powles T, van der Heijden MS, Balar AV, Necchi A, Dawson N, O'Donnell PH, Balmanoukian A, Loriot Y, Srinivas S, Retz MM, Grivas P, Joseph RW, Galsky MD, Fleming MT, Petrylak DP, Perez-Gracia JL, Burris HA, Castellano D, Canil C, Bellmunt J, Bajorin D, Nickles D, Bourgon R, Frampton GM, Cui N, Mariathasan S, Abidoye O, Fine GD, Dreicer R. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet. 2016;387:1909–1920. doi: 10.1016/S0140-6736(16)00561-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Camp RL, Dolled-Filhart M, Rimm DL. X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res. 2004;10:7252–7259. doi: 10.1158/1078-0432.CCR-04-0713. [DOI] [PubMed] [Google Scholar]
- 36.Gelsomino F, Barbolini M, Spallanzani A, Pugliese G, Cascinu S. The evolving role of microsatellite instability in colorectal cancer: A review. Cancer Treat Rev. 2016;51:19–26. doi: 10.1016/j.ctrv.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 37.Chun HW, Hong R. Significance of PD-L1 clones and C-MET expression in hepatocellular carcinoma. Oncol Lett. 2019;17:5487–5498. doi: 10.3892/ol.2019.10222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kammerer-Jacquet SF, Medane S, Bensalah K, Bernhard JC, Yacoub M, Dupuis F, Ravaud A, Verhoest G, Mathieu R, Peyronnet B, Brunot A, Laguerre B, Lespagnol A, Mosser J, Dugay F, Belaud-Rotureau MA, Rioux-Leclercq N. Correlation of c-MET Expression with PD-L1 Expression in Metastatic Clear Cell Renal Cell Carcinoma Treated by Sunitinib First-Line Therapy. Target Oncol. 2017;12:487–494. doi: 10.1007/s11523-017-0498-1. [DOI] [PubMed] [Google Scholar]
- 39.Park YL, Lee GH, Kim KY, Myung E, Kim JS, Myung DS, Park KJ, Cho SB, Lee WS, Jung YD, Kim HS, Joo YE. Expression of RON in colorectal cancer and its relationships with tumor cell behavior and prognosis. Tumori. 2012;98:652–662. doi: 10.1177/030089161209800517. [DOI] [PubMed] [Google Scholar]
- 40.Koganemaru S, Inoshita N, Miura Y, Miyama Y, Fukui Y, Ozaki Y, Tomizawa K, Hanaoka Y, Toda S, Suyama K, Tanabe Y, Moriyama J, Fujii T, Matoba S, Kuroyanagi H, Takano T. Prognostic value of programmed death-ligand 1 expression in patients with stage III colorectal cancer. Cancer Sci. 2017;108:853–858. doi: 10.1111/cas.13229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang L, Ren F, Wang Q, Baldridge LA, Monn MF, Fisher KW, Sheng W, Zhou X, Du X, Cheng L. Significance of Programmed Death Ligand 1 (PD-L1) Immunohistochemical Expression in Colorectal Cancer. Mol Diagn Ther. 2016;20:175–181. doi: 10.1007/s40291-016-0188-1. [DOI] [PubMed] [Google Scholar]
- 42.Lee LH, Cavalcanti MS, Segal NH, Hechtman JF, Weiser MR, Smith JJ, Garcia-Aguilar J, Sadot E, Ntiamoah P, Markowitz AJ, Shike M, Stadler ZK, Vakiani E, Klimstra DS, Shia J. Patterns and prognostic relevance of PD-1 and PD-L1 expression in colorectal carcinoma. Mod Pathol. 2016;29:1433–1442. doi: 10.1038/modpathol.2016.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilson CB, Ray M, Lutz M, Sharda D, Xu J, Hankey PA. The RON receptor tyrosine kinase regulates IFN-gamma production and responses in innate immunity. J Immunol. 2008;181:2303–2310. doi: 10.4049/jimmunol.181.4.2303. [DOI] [PubMed] [Google Scholar]
- 44.Wilson EB, Yamada DH, Elsaesser H, Herskovitz J, Deng J, Cheng G, Aronow BJ, Karp CL, Brooks DG. Blockade of chronic type I interferon signaling to control persistent LCMV infection. Science. 2013;340:202–207. doi: 10.1126/science.1235208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Teijaro JR, Ng C, Lee AM, Sullivan BM, Sheehan KC, Welch M, Schreiber RD, de la Torre JC, Oldstone MB. Persistent LCMV infection is controlled by blockade of type I interferon signaling. Science. 2013;340:207–211. doi: 10.1126/science.1235214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Koustas E, Papavassiliou AG, Karamouzis MV. The role of autophagy in the treatment of BRAF mutant colorectal carcinomas differs based on microsatellite instability status. PLoS One. 2018;13:e0207227. doi: 10.1371/journal.pone.0207227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Koustas E, Sarantis P, Kyriakopoulou G, Papavassiliou AG, Karamouzis MV. The Interplay of Autophagy and Tumor Microenvironment in Colorectal Cancer-Ways of Enhancing Immunotherapy Action. Cancers (Basel) 2019;11:533. doi: 10.3390/cancers11040533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jiang X, Zhou J, Giobbie-Hurder A, Wargo J, Hodi FS. The activation of MAPK in melanoma cells resistant to BRAF inhibition promotes PD-L1 expression that is reversible by MEK and PI3K inhibition. Clin Cancer Res. 2013;19:598–609. doi: 10.1158/1078-0432.CCR-12-2731. [DOI] [PubMed] [Google Scholar]
- 49.Atefi M, Avramis E, Lassen A, Wong DJ, Robert L, Foulad D, Cerniglia M, Titz B, Chodon T, Graeber TG, Comin-Anduix B, Ribas A. Effects of MAPK and PI3K pathways on PD-L1 expression in melanoma. Clin Cancer Res. 2014;20:3446–3457. doi: 10.1158/1078-0432.CCR-13-2797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Babicky ML, Harper MM, Chakedis J, Cazes A, Mose ES, Jaquish DV, French RP, Childers B, Alakus H, Schmid MC, Foubert P, Miyamoto J, Holman PJ, Walterscheid ZJ, Tang CM, Varki N, Sicklick JK, Messer K, Varner JA, Waltz SE, Lowy AM. MST1R kinase accelerates pancreatic cancer progression via effects on both epithelial cells and macrophages. Oncogene. 2019;38:5599–5611. doi: 10.1038/s41388-019-0811-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lai YS, Wahyuningtyas R, Aui SP, Chang KT. Autocrine VEGF signalling on M2 macrophages regulates PD-L1 expression for immunomodulation of T cells. J Cell Mol Med. 2019;23:1257–1267. doi: 10.1111/jcmm.14027. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in the published paper. More details can be provided on request.