Abstract
Background
Coronavirus disease 2019 (COVID-19), a highly infectious disease, has been rapidly spreading all over the world and remains a great threat to global public health. Patients diagnosed with severe or critical cases have a poor prognosis. Hence, it is crucial for us to identify potentially severe or critical cases early and give timely treatments for targeted patients. In the clinical practice of treating patients with COVID-19, we have observed that the neutrophil-to-lymphocyte ratio (NLR) of severe patients is higher than that in mild patients. We performed this systematic review and meta-analysis to evaluate the predictive values of NLR on disease severity and mortality in patients with COVID-19.
Methods
We searched PubMed, EMBASE, China National Knowledge Infrastructure (CNKI) and Wanfang databases to identify eligible studies (up to August 11, 2020). Two authors independently screened studies and extracted data. The methodological quality of the included studies was assessed by Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2).
Results
Thirteen studies involving 1579 patients reported the predictive value of NLR on disease severity. The pooled sensitivity (SEN), specificity (SPE) and area under curve (AUC) were 0.78 (95% CI 0.70–0.84), 0.78 (95% CI 0.73–0.83) and 0.85 (95% CI 0.81–0.88), respectively. Ten studies involving 2967 patients reported the predictive value of NLR on mortality. The pooled SEN, SPE and AUC were 0.83 (95% CI 0.75–0.89), 0.83 (95% CI 0.74–0.89) and 0.90 (95% CI 0.87–0.92), respectively.
Conclusions
NLR has good predictive values on disease severity and mortality in patients with COVID-19 infection. Evaluating NLR can help clinicians identify potentially severe cases early, conduct early triage and initiate effective management in time, which may reduce the overall mortality of COVID-19.
Trial registry
This meta-analysis was prospectively registered on PROSPERO database (Registration number: CRD42020203612).
Keywords: Neutrophil-to-lymphocyte ratio, Disease severity, Mortality, Predictive, Systematic review, Meta-analysis
Introduction
Coronavirus disease 2019 (COVID-19), a highly infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has been rapidly spreading all over the world and remains a great threat to global public health [1]. The clinical symptoms of patients with COVID-19 vary widely. A significant proportion of patients with COVID-19 have mild symptoms, such as fever, muscle ache, cough, shortness of breath and fatigue, and about half of patients do not show any obvious symptoms [2, 3]. However, some severe cases with severe pneumonia can develop into acute respiratory distress syndrome (ARDS), pulmonary oedema or multiple organ dysfunction syndrome (MODS), hence leading to a high mortality [4–6]. Although many patients have mild symptoms, they may suddenly progress to ARDS, septic shock or even MODS [7]. Patients diagnosed with severe or critical illness have a poor prognosis. Hence, it is crucial for us to identify potentially severe or critical cases early and give timely treatments for targeted patients. Therefore, we can prevent the progression of COVID-19, save medical resources and reduce mortality.
Similar to patients with Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS), dysregulated inflammation leading to cytokine storms is associated with worsening clinical outcomes in patients with COVID-19 [8–10]. Emerging evidences suggested that peripheral blood neutrophil-to-lymphocyte ratio (NLR) can be used as a marker of systemic inflammation. Furthermore, NLR has shown good predictive values on progression and clinical outcomes in various disease, such as solid tumours, chronic obstructive pulmonary disease (COPD), cardiovascular disease and pancreatitis [11–14]. Recently, several studies have reported that NLR may differentiate between mild/moderate and severe/critical groups and probability of death in patients with COVID-19 infection. In addition, a series of studies have suggested NLR is a reliable predictor of COVID-19 progression and elevated NLR is associated with high mortality [15–20].
NLR is a readily available biomarker that can be calculated from components of the differential white cell count (dividing neutrophil by lymphocyte count). We performed this systematic review and meta-analysis to evaluate the predictive values of NLR on disease severity and mortality in patients with COVID-19 and to provide a reliable marker for early identification of potentially severe or critically ill cases.
Methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA statement) guidelines to perform this meta-analysis [21]. It was prospectively registered on PROSPERO database (Registration number: CRD42020203612).
Selection of studies
We reviewed PubMed, EMBASE, China National Knowledge Infrastructure (CNKI) and Wanfang databases through August 11, 2020. The search terms were as follows: (“Neutrophil to lymphocyte ratio” or “neutrophil lymphocyte ratio” or “neutrophil-to-lymphocyte ratio” or “neutrophil/lymphocyte ratio” or “NLR”) and (“Coronavirus disease 2019” or “2019 Novel Coronavirus” or “SARS-CoV-2” or “2019-nCoV” or “COVID-19”). The detail of search strategy of PubMed is shown in Additional file 1. No language restrictions were imposed. To find additional citations, the reference lists of the included studies and recent review articles were screened when necessary.
Two authors (X.L and C.L) independently screened all identified citations to find studies for the final analysis. Any disagreement was resolved through discussion. In case of persistent disagreement, we consulted the third reviewer (F.Z) for arbitration. Studies were selected if they met the following criteria: (1) The predictive value of NLR on disease severity or mortality in patients with COVID-19 was evaluated; (2) a 2 × 2 table of results could be constructed [sufficient information to calculate true positive (TP), false positive (FP), false negative (FN) and true negative (TN)]. The exclusion criteria were as follows: (1) case report, review, editorial, conference abstract, comment, letter, animal study; (2) unable to extract a 2 × 2 table of results.
Data extraction and quality assessment
Two authors (X.L and C.L) independently extracted relevant information from individual studies, including first author, publication year, country, publication language, number of patients (male/female), mean age, cut-off value, area under curve (AUC), TP, TN, FP, FN, sensitivity (SEN) and specificity (SPE). The extracted information was checked by a third author (Z.M). We used the Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) criteria to evaluate each of the included studies in 4 domains: patient selection; index test; reference standard; and flow and test timing [22].
Statistical analysis
The statistical analyses were conducted by STATA (version 14.0) using MIDAS module [23]. A bivariate random-effects regression model was performed to calculate SEN, SPE, positive likelihood ratio, negative likelihood ratio, diagnostic odds ratio (DOR) and corresponding 95% credible interval (CI). A summary receiver operating characteristic (SROC) curve was drawn to assess the overall diagnostic accuracy. The higher the AUC value, the better the diagnostic power [24]. We used Deek funnel plot to detect publication bias. If the P value is less than 0.1, publication bias may exist. I2 index was calculated to assess heterogeneity between studies, and I2 values above 50% were regarded as the indicative of substantial heterogeneity [25]. We conducted Fagan nomograph to explore the relationship between the pre-test probability, likelihood ratio and the post-test probability. To investigate potential sources of heterogeneity among included studies, sensitivity and subgroup analyses were conducted. In sensitivity analyses, we only included studies published in English. We did subgroup analyses based on cut-off value.
Results
Selection and characteristics of studies
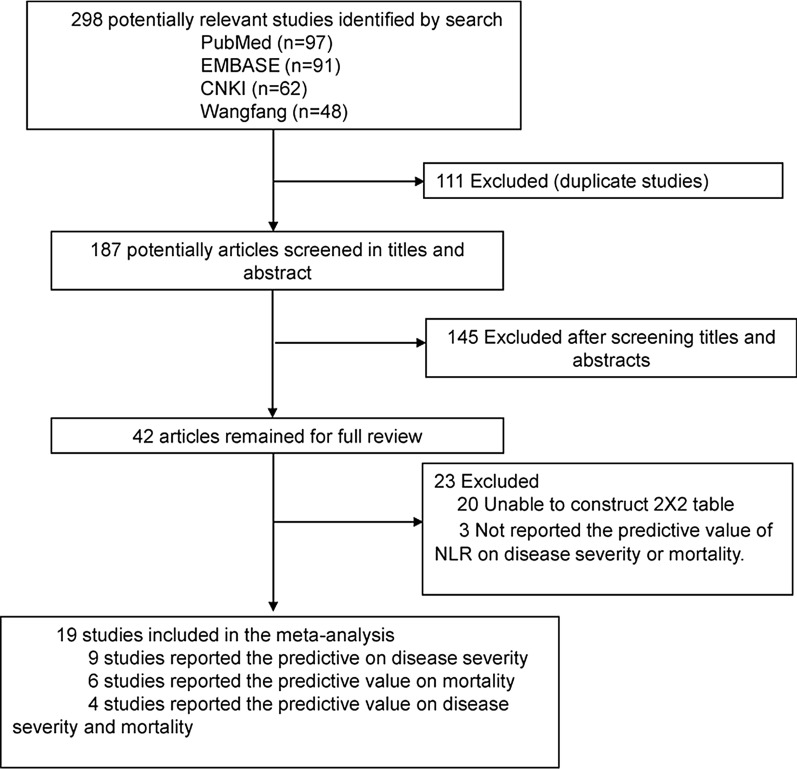
As a result of the literature search, a total of 298 studies were identified, including 97 from PubMed, 91 from EMBASE, 62 from CNKI and 48 from Wanfang debase. Figure 1 shows the study selection process. In total, 111 duplicate publications were excluded. According to the inclusion and exclusion criteria, we excluded 145 studies by evaluating the titles and abstracts. The remaining 42 studies were further scrutinized by reading the full text. Finally, only 19 studies were included in this meta-analysis, of which 9 reported the predictive value on disease severity [26–34], 6 reported the predictive value on mortality [35–40], and 4 reported the predictive value on both disease severity and mortality [41–44].
Fig. 1.
Flow diagram for the identification of eligible studies
The characteristics of the included studies and the predictive value of NLR on disease severity or mortality in each study are presented in Table 1. Most studies were conducted in China. Twelve studies were published in English, six in Chinese and one in Spanish. Except one prospective study [27], all others were retrospective studies. The number of participants across studies ranged from 45 to 1004. Notably, the SEN, SPE, AUC and cut-off value of NLR predicting mortality and disease severity ranged greatly among the included studies. Except two studies [41, 42], all other studies defined severe patients as meeting at least one of the following criterions: shortness of breath, respiratory rate (RR) ≥ 30 times/min or oxygen saturation (resting state) ≤ 93%, or PaO2/FiO2 ≤ 300 mmHg.
Table 1.
Characteristics of the included studies and diagnostic test performance of NLR for disease severity and mortality
| Study | Country | Publication language | No. of patients |
Male/ female |
Mean age | Cut-off | AUC | TP | FP | FN | TN | SEN (%) | SPE (%) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Severity | Yang2020 [33] | China | English | 93 | 56/37 | 46.4 ± 17.6 | 3.3 | 0.84 | 21 | 25 | 3 | 44 | 88.0 | 63.6 |
| Wang2020 [31] | China | English | 45 | 23/22 | 39.0 ± 11.5 | 13.4 | 0.89 | 8 | 6 | 2 | 29 | 83.3 | 82.4 | |
| Fesih2020 [44] | Turkey | English | 139 | 62/77 | 55.5 ± 18.5 | 3.3 | 0.87 | 43 | 25 | 11 | 60 | 79.0 | 71.0 | |
| Jingyuan Liu2020 [27] | China | English | 115 | 64/51 | NA | 3.1 | NA | 28 | 13 | 9 | 65 | 75.7 | 83.3 | |
| Asghar2020 | Pakistan | English | 100 | 69/31 | 52.6 ± 15.7 | 3.7 | 0.80 | 29 | 25 | 4 | 42 | 87.9 | 62.1 | |
| Sun2020 [30] | China | English | 116 | 60/56 | 50.0 ± 4.0 | 4.5 | 0.89 | 20 | 9 | 7 | 80 | 74.1 | 89.9 | |
| Shang2020 [29] | China | English | 443 | 220/223 | 56.0 ± 17.4 | 4.3 | 0.74 | 78 | 50 | 61 | 254 | 56.3 | 83.7 | |
| Yueping Liu2020 [28] | China | English | 84 | 47/37 | 53.0 ± 17.8 | 4.9 | 0.76 | 13 | 8 | 10 | 53 | 56.5 | 86.9 | |
| Basbus2020 [42] | Spain | Spanish | 131 | 71/60 | 52.0 ± 30.4 | 3.0 | NA | 17 | 36 | 4 | 74 | 80.9 | 67.3 | |
| Li2020 [43] | China | Chinese | 93 | 55/38 | 62.1 ± 16.8 | 11.3 | NA | 34 | 4 | 9 | 46 | 79.1 | 92.0 | |
| Zha2020 [34] | China | Chinese | 85 | 57/28 | 54.2 ± 16.0 | 5.6 | 0.77 | 25 | 10 | 12 | 38 | 68.8 | 78.4 | |
| Fei2020 [26] | China | Chinese | 72 | 32/40 | 58.0 ± 13.8 | 3.0 | 0.89 | 20 | 14 | 0 | 38 | 100 | 73.1 | |
| Xia2020 [32] | China | Chinese | 63 | 33/30 | 63.4 ± 14.9 | 4.8 | 0.83 | 26 | 8 | 5 | 24 | 83.9 | 75.0 | |
| Mortality | ||||||||||||||
| Cheng2020 [36] | China | English | 456 | 211/245 | 55.0 ± 18.6 | 3.2 | 0.81 | 26 | 107 | 10 | 303 | 78.3 | 73.9 | |
| Tatum2020 [38] | America | English | 125 | 57/68 | 58.7 ± 14.8 | 10.0 | 0.71 | 12 | 4 | 11 | 98 | 52.4 | 96.7 | |
| Chen2020 [35] | China | English | 681 | 362/219 | 65.0 ± 13.3 | 6.7 | 0.86 | 87 | 130 | 17 | 447 | 83.7 | 77.5 | |
| Fesih2020 [44] | Turkey | English | 139 | 62/77 | 55.5 ± 18.5 | 5.7 | 0.85 | 11 | 13 | 2 | 113 | 83.0 | 90.0 | |
| Asghar2020 [41] | Pakistan | English | 100 | 69/31 | 52.6 ± 15.7 | 4.2 | 0.81 | 20 | 29 | 2 | 49 | 90.9 | 62.6 | |
| Yan2020 [39] | China | English | 1004 | 493/511 | NA | 11.8 | 0.95 | 39 | 211 | 1 | 753 | 97.5 | 78.1 | |
| Basbus2020 [42] | Spain | Spanish | 131 | 71/60 | 52.0 ± 30.4 | 3 | NA | 7 | 46 | 2 | 76 | 77.8 | 62.3 | |
| Li2020 [43] | China | Chinese | 93 | 55/38 | 62.1 ± 16.8 | 11.3 | 0.92 | 28 | 10 | 3 | 52 | 90.3 | 83.9 | |
| Song2020 [37] | China | Chinese | 84 | 56/28 | 66.5 ± 12.2 | 6.1 | 0.87 | 32 | 5 | 10 | 37 | 76.2 | 88.1 | |
| Zhang2020 [40] | China | Chinese | 154 | 81/73 | 69.2 ± 7.5 | 9.4 | 0.86 | 21 | 10 | 6 | 117 | 76.2 | 92.0 |
AUC area under curve, TP true positive, FP false positive, FN false negative, TN true negative, SEN sensitivity, SPE specificity, NLR neutrophil-to-lymphocyte ratio, NA not available
Study quality and publication bias
The methodological quality of the included studies is presented in Additional file 2. One study only included patients classified as moderate [36], one included only severe patients [35], and another included only elderly patients [40]. Therefore, these three studies were considered to have a high risk of patient selection bias. One study included 32 moderate cases, and another 31 severe cases were included as a control group [32]. One study included 48 moderate cases, and another 37 severe cases were included as a control group [34]. One study included 50 moderate cases, and another 43 severe cases were included as a control group [43]. One study included 42 dead patients, and another 42 discharged patients were included as a control group [37]. These four studies were also assessed to show high risk of patient selection bias, because they did not avoid a case–control design. One study did not provide sufficient information about patients enrolled and leaded to a high risk of patient selection in our opinion [33]. Most studies were considered to have unclear risk of bias regarding index tests, because they did not report the blindness between index and reference tests. Deek funnel plot is shown in Additional file 3, and publication bias may exist among studies reporting the predictive value of NLR on disease severity (P = 0.04).
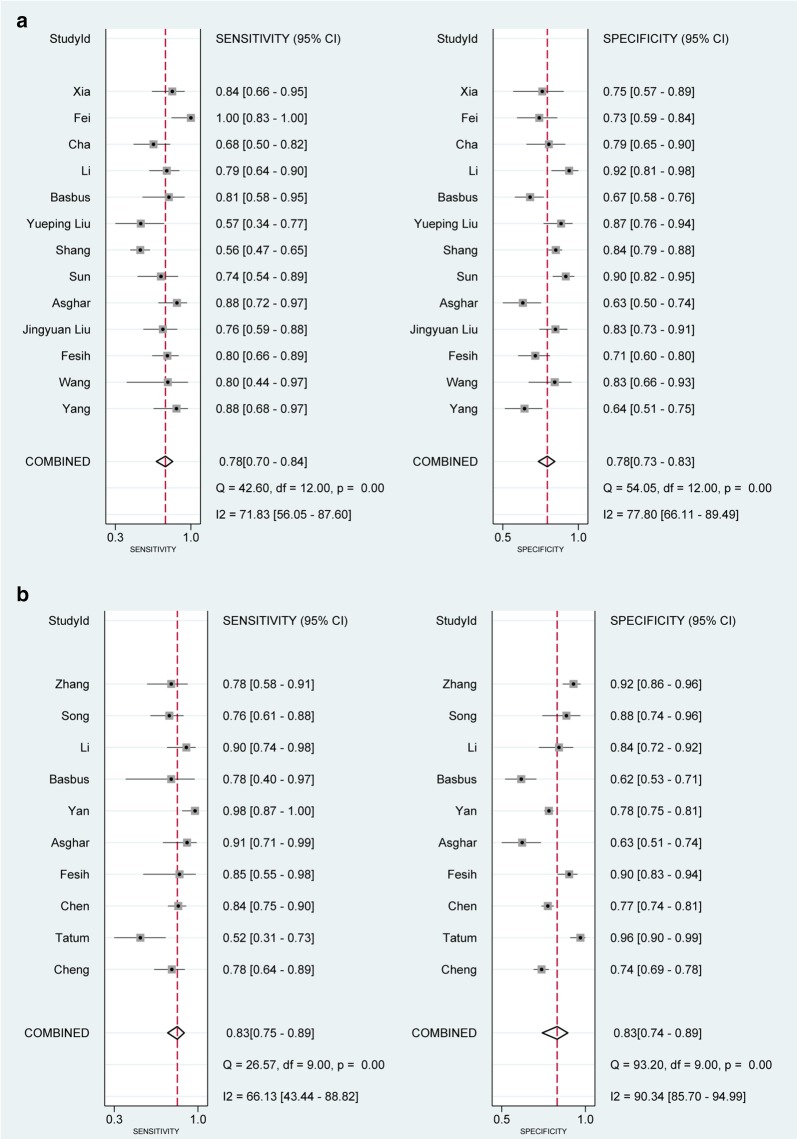
Predictive value of NLR on disease severity
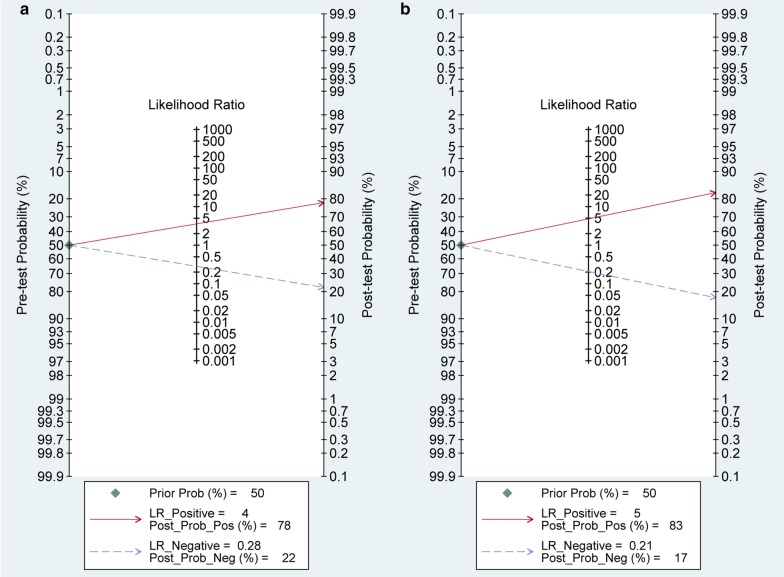
Thirteen studies involving 1579 patients reported the predictive value of NLR on disease severity. The pooled SEN and SPE were 0.78 (95% CI 0.70–0.84, I2 = 71.83) and 0.78 (95% CI 0.73–0.83, I2 = 77.80), respectively (Fig. 2a). The positive likelihood ratio was 3.6 (95% CI 2.9–4.4), and the negative likelihood ratio was 0.28 (95% CI 0.21–0.38). The DOR was 13 (95% CI 9–18). The SROC curve is shown in Fig. 3a. The AUC of NLR for predicting disease severity was 0.85 (95% CI 0.81–0.88), indicating high diagnostic value. We can learn from Fagan nomogram (Fig. 4a) that if the pre-test probability was set to 50%, the post-test probability of NLR for the detection of severe cases was 78% when the NLR was above the cut-off value. On the contrary, when the NLR was below the cut-off value, the post-test probability was 26%.
Fig. 2.
a. Forest plot of the sensitivity and specificity of NLR for predicting disease severity in patients with COVID-19. The pooled sensitivity and specificity were 0.78 (95% CI 0.70–0.84) and 0.78 (95% CI 0.73–0.83), respectively. b. Forest plot of the sensitivity and specificity of NLR for predicting mortality in patients with COVID-19. The pooled sensitivity and specificity were 0.83 (95% CI 0.75–0.89) and 0.83 (95% CI 0.74–0.89), respectively
Fig. 3.
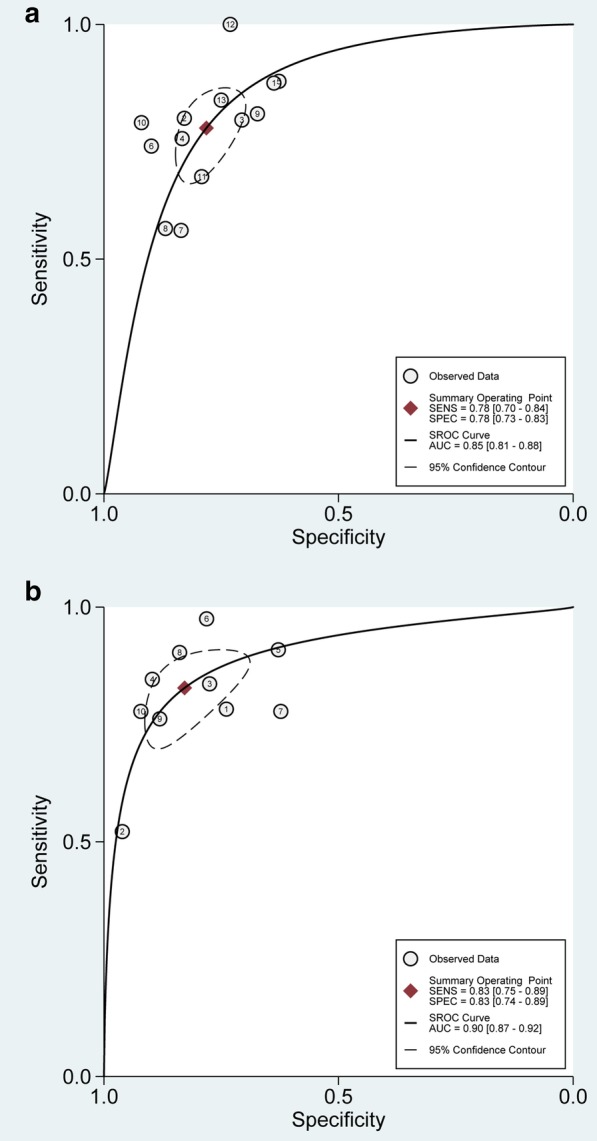
Summary receiver operating characteristic graph for the included studies. a. The AUC of NLR for predicting disease severity was 0.85 (95% CI 0.81–0.88). b. The AUC of NLR for predicting mortality was 0.90 (95% CI 0.87–0.92)
Fig. 4.
Fagan nomogram of NLR for predicting disease severity and mortality in patients with COVID-19. The pre-test probability was set to 50%. a. The post-test probability of NLR for the detection of severe cases was 78% when the NLR was above the cut-off value. The post-test probability was 22% when the NLR was below the cut-off value. b. The post-test probability of NLR for the detection of mortality was 83% when the NLR was above the cut-off value. The post-test probability was 17% when the NLR was below the cut-off value
Predictive value of NLR on mortality
Ten studies involving 2967 patients reported the predictive value of NLR on mortality. The pooled SEN and SPE were 0.83 (95% CI 0.75–0.89, I2 = 66.13) and 0.83 (95% CI 0.74–0.89, I2 = 90.34), respectively (Fig. 2b). The positive likelihood ratio was 4.8 (95% CI 3.3–7.0), and the negative likelihood ratio was 0.21 (95% CI 0.15–0.30). The DOR was 23 (95% CI 15–36). The SROC with pooled diagnostic accuracy was 0.90 (95% CI 0.87–0.92), presented in Fig. 3b. The Fagan nomogram showed that the post-test probability of NLR for the detection of mortality was 83% when the NLR was above the cut-off value and the post-test probability was 17% when the NLR was below the cut-off value (Fig. 4b).
Subgroup analyses and sensitivity analyses
We conducted the subgroup analyses based on the cut-off value. In terms of predicting disease severity, the cut-off value in six studies was higher than 4.5 and was termed the “high cut-off value” subgroup. Seven others used a lower cut-off value, which were included in the “low cut-off value” subgroup. The AUC was 0.86 (95% CI 0.83–0.89) and 0.82 (95% CI 0.78–0.85), respectively. Similarly, ten studies reporting the predictive value of NLR on mortality were divided into “high cut-off value” (cut-off ≥ 6.5) and “low cut-off value” (< 6.5) subgroups, and the AUC was 0.92 (95% CI 0.89–0.94) and 0.84 (95% CI 0.80–0.87), respectively. In the sensitivity analyses, we only included studies published in English. The pooled AUC for predicting disease severity and mortality was 0.83 (95% CI 0.80–0.86) and 0.90 (95% CI 0.87–0.92), respectively. Detailed results about subgroup analyses and sensitivity analyses are presented in Table 2.
Table 2.
Results of sensitivity analysis and subgroup analysis
| Categories | No. of studies |
Sensitivity (95% CI)/I2 |
Specificity (95% CI) /I2 |
AUC (95% CI) |
DOR (95% CI) |
PLR/NLR |
|---|---|---|---|---|---|---|
| Disease severity | ||||||
| Cut-off ≥ 4.5 | 6 | 0.74(0.66,0.80)/25.56 | 0.86(0.81,0.89)/36.40 | 0.86(0.83,0.89) | 17(10,28) | 5.1/0.31 |
| Cut-off < 4.5 | 7 | 0.82(0.71,0.89)/82.74 | 0.72(0.66,0.78)/79.70 | 0.82(0.78,0.85) | 12(7,19) | 3.0/0.25 |
| Published in English | 8 | 0.74(0.63,0.83)/73.82 | 0.78(0.71,0.84)/81.99 | 0.83(0.80,0.86) | 10(7,16) | 3.4/0.33 |
| Mortality | ||||||
| Cut-off ≥ 6.5 | 5 | 0.83(0.66,0.92)/84.97 | 0.87(0.77,0.93)/92.60 | 0.92(0.89,0.94) | 32(17,61) | 6.3/0.20 |
| Cut-off < 6.5 | 5 | 0.81(0.72,0.87)/0 | 0.77(0.64,0.86)/89.07 | 0.84(0.80,0.87) | 14(7,27) | 3.5/0.25 |
| Published in English | 6 | 0.83(0.69,0.91)/79.98 | 0.82(0.71,0.90)/89.87 | 0.90(0.87,0.92) | 23(12,41) | 4.7/0.21 |
AUC area under curve, PLR positive likelihood ratio, NLR negative likelihood ratio, DOR diagnostic odds ratio, CI credible interval
Discussion
Although in the clinical practice of treating patients with COVID-19, we have observed that the NLR of severe patients is higher than that in mild patients, there is no systematic review and meta-analysis to evaluate the predictive values of NLR on disease severity and mortality in patients with COVID-19. Studies have reported various thresholds to NLR. Clinicians are therefore unclear regarding the thresholds of NLR that should be applied in order to categorize severity of disease and predict prognosis. Our study suggested that NLR can not only be a good biomarker predicting disease severity in patients with COVID-19 (AUC = 0.85, SEN = 0.78 and SPE = 0.78), but also have value in predicting mortality (AUC = 0.90, SEN = 0.83 and SPE = 0.83).
COVID-19 spread rapidly and is an ongoing global pandemic. Medical workers from different countries make efforts to explore the best diagnostic method and the most effective treatment for COVID-19. More and more studies have focused on COVID-19 and published in different languages. To find enough studies that reported the predictive values of NLR on disease severity and mortality in patients with COVID-19, we did not impose any language restrictions. In our final analyses, twelve studies were published in English, six in Chinese and one in Spanish. To our knowledge, English is the most widely used language in the world. Studies published in English may have a wider readership and receive peer review from different countries, while studies published in other languages may be available only to native speakers. Therefore, we performed sensitivity analyses by omitting studies not published in English. The results of the sensitivity analyses were in accordance with the main analyses, indicating that the publish language was not a confounding factor.
To our knowledge, the treatments for mild cases and severe cases are greatly different. For mild cases, there is no need to intervene too much. Some patients can even recover without any treatments. However, for severe cases, even we take many kinds of measures, such as mechanical ventilation, extracorporeal membrane oxygenation (ECMO) and continuous renal replacement therapy (CRRT), the mortality is still high [45, 46]. Therefore, if the potentially severe cases were identified early and effective treatments were taken to prevent the progression of those patients, more patients’ lives may be saved.
The current criteria for classifying mild cases and severe cases are mainly based on RR, oxygen saturation and PaO2/FiO2. These indicators are important but lack specificity for COVID-19. In laboratory examination of patients with COVID-19, the absolute value of peripheral white blood cells is usually normal or low, and lymphopenia is common [47]. However, in severe or non-survival patients with COVID-19, the lymphocytes count decreases progressively, while the neutrophils count gradually increases. This may be due to excessive inflammation and immune suppression caused by SARS-CoV-2 infection. On the one hand, neutrophils are generally regarded as pro-inflammatory cells with a range of antimicrobial activities, which can be triggered by virus-related inflammatory factors, such as interleukin-6 and interleukin-8 [9]. On the other hand, systematic inflammation triggered by SARS-CoV-2 significantly depresses cellular immunity, leading to a decrease in CD3 + T cells, CD4 + T cells and CD8 + T cells. In addition, SARS-CoV-2-infected T cells may also cause cytopathic effects on T cells [10, 48–50]. Therefore, NLR, a cost-effective marker, can be easily calculated from peripheral blood routine tests and may be associated with the progression and prognosis of COVID-19. To date, four meta-analyses have reported that patients with severe COVID-19 infection had a higher NLR than those with non-severe COVID-19 infection [51–54]. However, none of them evaluated the predictive values of NLR on disease severity and mortality.
There are several limitations in this meta-analysis. First, all but one of the studies were retrospective, meaning the data were prone to confounding factors. Second, the progression and prognosis of disease were influenced by many factors, such as age, sex and comorbidities, while we did not evaluate other factors. Finally, there was considerable heterogeneity among the included studies. Although we conducted sensitivity and subgroup analyses, the heterogeneity was not significantly decreased. That may be caused by different cut-off values, different conditions of patients or different comorbidities among the included studies. Additional high-quality studies are required to shed light on the role of NLR in the progression and prognosis of COVID-19 and find the optimal cut-off value.
Conclusions
NLR has good predictive values on disease severity and mortality in patients with COVID-19 infection. Evaluating NLR can help clinicians identify potentially severe cases early, conduct early triage and initiate effective management in time, which may reduce the overall mortality of COVID-19.
Supplementary information
Additional file 1. Search strategy terms and results of PubMed.
Additional file 2. Summary of the methodological quality of the studies according to the QUADAS-2 (Quality Assessment of Diagnostic Accuracy Studies-2) criteria.
Additional file 3. Deek funnel plot asymmetry test for publication bias, with P < 0.1 indicating publication bias.
Acknowledgements
We thank all researchers and clinicians involved in the individual trials.
Abbreviations
- COVID-19
Coronavirus disease 2019
- NLR
Neutrophil-to-lymphocyte ratio
- CNKI
China National Knowledge Infrastructure
- QUADAS-2
Quality Assessment of Diagnostic Accuracy Studies 2
- SEN
Sensitivity
- SPE
Specificity
- AUC
Area under curve
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- ARDS
Acute respiratory distress syndrome
- MODS
Multiple organ dysfunction syndrome
- MERS
Middle East respiratory syndrome
- SARS
Severe acute respiratory syndrome
- COPD
Chronic obstructive pulmonary disease
- PRISMA statement
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- TP
True positive
- FP
False positive
- FN
False negative
- TN
True negative
- DOR
Diagnostic odds ratio
- CI
Credible interval
- SROC
Summary receiver operating characteristic
- RR
Respiratory rate
- ECMO
Extracorporeal membrane oxygenation
- CRRT
Continuous renal replacement therapy
Authors’ contributions
XML and CL contributed equally to this work. XML and CL conceived the study, participated in the design, collected the data, performed statistical analyses and drafted the manuscript. ZM and LW collected the data and performed statistical analyses. MLX and SQ collected the data and revised the manuscript critically for important intellectual content. FHZ performed statistical analyses and helped to revise the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Funding
This work was funded by WU Jieping Medical Foundation (No. 320.6750.18383).
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiaoming Li and Chao Liu contributed equally to this work
Contributor Information
Xiaoming Li, Email: xiaomingli329@foxmail.com.
Chao Liu, Email: chaoliu301@foxmail.com.
Zhi Mao, Email: maozhi@126.com.
Minglu Xiao, Email: samanthaily@126.com.
Li Wang, Email: w.l_125@hotmail.com.
Shuang Qi, Email: shuangsemantian@163.com.
Feihu Zhou, Email: feihuzhou301@126.com.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13054-020-03374-8.
References
- 1.Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, Singh KP, Chaicumpa W, Bonilla-Aldana DK. Rodriguez-Morales AJ Coronavirus disease 2019-COVID-19. Clin Microbiol Rev. 2020;33:4. doi: 10.1128/CMR.00028-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feng W, Zong W, Wang F, Ju S. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): a review. Mol Cancer. 2020;19(1):100. doi: 10.1186/s12943-020-01218-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tabata S, Imai K, Kawano S, Ikeda M, Kodama T, Miyoshi K, Obinata H, Mimura S, Kodera T, Kitagaki M, et al. Clinical characteristics of COVID-19 in 104 people with SARS-CoV-2 infection on the Diamond Princess cruise ship: a retrospective analysis. Lancet Infect Dis. 2020;20:1043. doi: 10.1016/S1473-3099(20)30482-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qin H, Zhao A. Mesenchymal stem cell therapy for acute respiratory distress syndrome: from basic to clinics. Protein Cell. 2020;11:707. doi: 10.1007/s13238-020-00738-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Zhou X, Du C, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan. JAMA Intern Med: China; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferrando C, Suarez-Sipmann F, Mellado-Artigas R, Hernandez M, Gea A, Arruti E, Aldecoa C, Martinez-Palli G, Martinez-Gonzalez MA, Slutsky AS et al: Clinical features, ventilatory management, and outcome of ARDS caused by COVID-19 are similar to other causes of ARDS. Intensive Care Med 2020. [DOI] [PMC free article] [PubMed]
- 7.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manjili RH, Zarei M, Habibi M, Manjili MH. COVID-19 as an acute inflammatory disease. J Immunol. 2020;205(1):12–19. doi: 10.4049/jimmunol.2000413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mangalmurti N, Hunter CA. Cytokine storms: understanding COVID-19. Immunity. 2020;53(1):19–25. doi: 10.1016/j.immuni.2020.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Azkur AK, Akdis M, Azkur D, Sokolowska M, van de Veen W, Bruggen MC, O'Mahony L, Gao Y, Nadeau K, Akdis CA. Immune response to SARS-CoV-2 and mechanisms of immunopathological changes in COVID-19. Allergy. 2020;75(7):1564–1581. doi: 10.1111/all.14364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Templeton AJ, McNamara MG, Seruga B, Vera-Badillo FE, Aneja P, Ocana A, Leibowitz-Amit R, Sonpavde G, Knox JJ, Tran B, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):124. doi: 10.1093/jnci/dju124. [DOI] [PubMed] [Google Scholar]
- 12.Kim S, Eliot M, Koestler DC, Wu WC, Kelsey KT. Association of neutrophil-to-lymphocyte ratio with mortality and cardiovascular disease in the Jackson heart study and modification by the duffy antigen variant. JAMA Cardiol. 2018;3(6):455–462. doi: 10.1001/jamacardio.2018.1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paliogiannis P, Fois AG, Sotgia S, Mangoni AA, Zinellu E, Pirina P, Negri S, Carru C, Zinellu A. Neutrophil to lymphocyte ratio and clinical outcomes in COPD: recent evidence and future perspectives. Eur Respir Rev. 2018;27:147. doi: 10.1183/16000617.0113-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kong W, He Y, Bao H, Zhang W, Wang X. Diagnostic value of neutrophil-lymphocyte ratio for predicting the severity of acute pancreatitis: a meta-analysis. Dis Markers. 2020;2020:9731854. doi: 10.1155/2020/9731854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lian J, Jin C, Hao S, Zhang X, Yang M, Jin X, Lu Y, Hu J, Zhang S, Zheng L, et al. High neutrophil-to-lymphocyte ratio associated with progression to critical illness in older patients with COVID-19: a multicenter retrospective study. Aging (Albany NY) 2020;12(14):13849–13859. doi: 10.18632/aging.103582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang JJ, Cao YY, Tan G, Dong X, Wang BC, Lin J, Yan YQ, Liu GH, Akdis M, Akdis CA et al: Clinical, radiological and laboratory characteristics and risk factors for severity and mortality of 289 hospitalized COVID-19 patients. Allergy 2020. [DOI] [PMC free article] [PubMed]
- 17.Fu J, Kong J, Wang W, Wu M, Yao L, Wang Z, Jin J, Wu D, Yu X. The clinical implication of dynamic neutrophil to lymphocyte ratio and D-dimer in COVID-19: A retrospective study in Suzhou China. Thromb Res. 2020;192:3–8. doi: 10.1016/j.thromres.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liao D, Zhou F, Luo L, Xu M, Wang H, Xia J, Gao Y, Cai L, Wang Z, Yin P et al: Haematological characteristics and risk factors in the classification and prognosis evaluation of COVID-19: a retrospective cohort study. Lancet Haematol 2020. [DOI] [PMC free article] [PubMed]
- 19.Nalbant A, Kaya T, Varim C, Yaylaci S, Tamer A. Cinemre H (2020) Can the neutrophil/lymphocyte ratio (NLR) have a role in the diagnosis of coronavirus 2019 disease (COVID-19)? Rev Assoc Med Bras. 1992;66(6):746–751. doi: 10.1590/1806-9282.66.6.746. [DOI] [PubMed] [Google Scholar]
- 20.Ma A, Cheng J, Yang J, Dong M, Liao X, Kang Y. Neutrophil-to-lymphocyte ratio as a predictive biomarker for moderate-severe ARDS in severe COVID-19 patients. Crit Care. 2020;24(1):288. doi: 10.1186/s13054-020-03007-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 22.Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM. Group Q-: QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 23.Dwamena BJSSC: MIDAS: Stata module for meta-analytical integration of diagnostic test accuracy studies. 2007.
- 24.Jones CM, Athanasiou T. Summary receiver operating characteristic curve analysis techniques in the evaluation of diagnostic tests. Ann Thorac Surg. 2005;79(1):16–20. doi: 10.1016/j.athoracsur.2004.09.040. [DOI] [PubMed] [Google Scholar]
- 25.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fei M, Tong F, Tao X, Wang J. Value of neutrophil-to-lymphocyte ratio in the classification diagnosis of coronavirus disease 2019. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2020;32(5):554–558. doi: 10.3760/cma.j.cn121430-20200413-00506. [DOI] [PubMed] [Google Scholar]
- 27.Liu J, Liu Y, Xiang P, Pu L, Xiong H, Li C, Zhang M, Tan J, Xu Y, Song R, et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Transl Med. 2020;18(1):206. doi: 10.1186/s12967-020-02374-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu YP, Li GM, He J, Liu Y, Li M, Zhang R, Li YL, Wu YZ, Diao B. Combined use of the neutrophil-to-lymphocyte ratio and CRP to predict 7-day disease severity in 84 hospitalized patients with COVID-19 pneumonia: a retrospective cohort study. Ann Transl Med. 2020;8(10):635. doi: 10.21037/atm-20-2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shang W, Dong J, Ren Y, Tian M, Li W, Hu J, Li Y: The value of clinical parameters in predicting the severity of COVID-19. J Med Virol 2020. [DOI] [PMC free article] [PubMed]
- 30.Sun S, Cai X, Wang H, He G, Lin Y, Lu B, Chen C, Pan Y, Hu X. Abnormalities of peripheral blood system in patients with COVID-19 in Wenzhou, China. Clin Chim Acta. 2020;507:174–180. doi: 10.1016/j.cca.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang C, Deng R, Gou L, Fu Z, Zhang X, Shao F, Wang G, Fu W, Xiao J, Ding X, et al. Preliminary study to identify severe from moderate cases of COVID-19 using combined hematology parameters. Ann Transl Med. 2020;8(9):593. doi: 10.21037/atm-20-3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xia X, Wen M, Zhan S, He J, Chen W. An increased neutrophil/lymphocyte ratio is an early warning signal of severe COVID-19. Nan Fang Yi Ke Da Xue Xue Bao. 2020;40(3):333–336. doi: 10.12122/j.issn.1673-4254.2020.03.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang AP, Liu JP, Tao WQ, Li HM. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. 2020;84:106504. doi: 10.1016/j.intimp.2020.106504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zha Q, Feng B, Li X, Zhou D, Kang Y, Qin H. Study on early laboratory warning of severe COVID-19. Laboratory Medicine. 2020;35(06):557–560. [Google Scholar]
- 35.Chen FF, Zhong M, Liu Y, Zhang Y, Zhang K, Su DZ, Meng X, Zhang Y. The characteristics and outcomes of 681 severe cases with COVID-19 in China. J Crit Care. 2020;60:32–37. doi: 10.1016/j.jcrc.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cheng B, Hu J, Zuo X, Chen J, Li X, Chen Y, Yang G, Shi X, Deng A. Predictors of progression from moderate to severe coronavirus disease 2019: a retrospective cohort. Clin Microbiol Infect. 2020;26:1400. doi: 10.1016/j.cmi.2020.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Song H, Bai T, Shi J, Yang J. Predictive value of multiple inflammatory indexes on the prognosis of patients with corona virus disease 2019. Pract J Cardiac Cerebr Pneumal Vasc Dis. 2020;28(06):13–16. [Google Scholar]
- 38.Tatum D, Taghavi S, Houghton A, Stover J, Toraih E, Duchesne J: Neutrophil-to-lymphocyte ratio and outcomes in Louisiana Covid-19 patients. Shock 2020. [DOI] [PMC free article] [PubMed]
- 39.Yan X, Li F, Wang X, Yan J, Zhu F, Tang S, Deng Y, Wang H, Chen R, Yu Z et al: Neutrophil to lymphocyte ratio as prognostic and predictive factor in patients with coronavirus disease 2019: a retrospective cross-sectional study. J Med Virol 2020. [DOI] [PMC free article] [PubMed]
- 40.Zhang W, Li S, Xie X, Wang J, Guo W, Lei Y, Wang X, Xu C, Li Z, Chen Y, et al. Clinical characteristics and risk factors of mortality in elderly patients with novel coronavirus pneumonia. Pract Geriatr. 2020;34(7):745–749. [Google Scholar]
- 41.Asghar MS, Haider Kazmi SJ, Ahmed Khan N, Akram M, Ahmed Khan S, Rasheed U, Hassan M, Memon GM. Clinical profiles, characteristics, and outcomes of the first 100 admitted COVID-19 patients in Pakistan: a single-center retrospective study in a tertiary care Hospital of Karachi. Cureus. 2020;12(6):e8712. doi: 10.7759/cureus.8712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Basbus L, Lapidus MI, Martingano I, Puga MC, Pollan J. Neutrophil to lymphocyte ratio as a prognostic marker in COVID-19. Medicina (B Aires) 2020;80(Suppl 3):31–36. [PubMed] [Google Scholar]
- 43.Li H, Zhao M, Xu Y. Biochemical analysis between common type and critical type of COVID-19 and clinical value of neutrophil/lymphocyte ratio. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2020;40(7):965–971. doi: 10.12122/j.issn.1673-4254.2020.07.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ok F, Erdogan O, Durmus E, Carkci S, Canik A. Predictive values of blood urea nitrogen/creatinine ratio and other routine blood parameters on disease severity and survival of COVID-19 patients. J Med Virol. 2020;22:10. doi: 10.1002/jmv.26300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schmidt M, Hajage D, Lebreton G, Monsel A, Voiriot G, Levy D, Baron E, Beurton A, Chommeloux J, Meng P, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: a retrospective cohort study. Lancet Respir Med. 2020;8:1123. doi: 10.1016/S2213-2600(20)30328-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xie J, Wu W, Li S, Hu Y, Hu M, Li J, Yang Y, Huang T, Zheng K, Wang Y, et al. Clinical characteristics and outcomes of critically ill patients with novel coronavirus infectious disease (COVID-19) in China: a retrospective multicenter study. Intensive Care Med. 2020;20:1. doi: 10.1007/s00134-020-06211-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Singhal T. A review of coronavirus disease-2019 (COVID-19) Indian J Pediatr. 2020;87(4):281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang X, Xu W, Hu G, Xia S, Sun Z, Liu Z, Xie Y, Zhang R, Jiang S, Lu L. RETRACTED ARTICLE: SARS-CoV-2 infects T lymphocytes through its spike protein-mediated membrane fusion. Cell Mol Immunol. 2020;7:1. doi: 10.1038/s41423-020-0424-9. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 49.van der Poll T, van de Veerdonk FL, Scicluna BP, Netea MG. The immunopathology of sepsis and potential therapeutic targets. Nat Rev Immunol. 2017;17(7):407–420. doi: 10.1038/nri.2017.36. [DOI] [PubMed] [Google Scholar]
- 50.Zhang X, Tan Y, Ling Y, Lu G, Liu F, Yi Z, Jia X, Wu M, Shi B, Xu S, et al. Viral and host factors related to the clinical outcome of COVID-19. Nature. 2020;583(7816):437–440. doi: 10.1038/s41586-020-2355-0. [DOI] [PubMed] [Google Scholar]
- 51.Chan AS, Rout A. Use of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in COVID-19. J Clin Med Res. 2020;12(7):448–453. doi: 10.14740/jocmr4240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zeng F, Li L, Zeng J, Deng Y, Huang H, Chen B, Deng G. Can we predict the severity of coronavirus disease 2019 with a routine blood test? Pol Arch Intern Med. 2020;130(5):400–406. doi: 10.20452/pamw.15331. [DOI] [PubMed] [Google Scholar]
- 53.Ghahramani S, Tabrizi R, Lankarani KB, Kashani SMA, Rezaei S, Zeidi N, Akbari M, Heydari ST, Akbari H, Nowrouzi-Sohrabi P, et al. Laboratory features of severe vs. non-severe COVID-19 patients in Asian populations: a systematic review and meta-analysis. Eur J Med Res. 2020;25(1):30. doi: 10.1186/s40001-020-00432-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lagunas-Rangel FA. Neutrophil-to-lymphocyte ratio and lymphocyte-to-C-reactive protein ratio in patients with severe coronavirus disease 2019 (COVID-19): A meta-analysis. J Med Virol. 2020;92:10. doi: 10.1002/jmv.25819. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Search strategy terms and results of PubMed.
Additional file 2. Summary of the methodological quality of the studies according to the QUADAS-2 (Quality Assessment of Diagnostic Accuracy Studies-2) criteria.
Additional file 3. Deek funnel plot asymmetry test for publication bias, with P < 0.1 indicating publication bias.
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its supplementary information files].