Abstract
Purpose
To evaluate eye-related quality of life (ER-QOL) and functional vision in children wearing glasses using the Pediatric Eye Questionnaire (PedEyeQ).
Methods
Children 5–17 years of age with normal visual acuity who wore glasses for correction of refractive error and with no other eye condition or treatment and control subjects who did not wear glasses, along with 1 parent for each child, were prospectively enrolled. Children completed the Child 5–11 or 12–17 PedEyeQ (four domains); parents completed the Proxy 5–11 or 12–17 questionnaires (perceived effect on child; five domains) and also the Parent questionnaire (effect on parent themselves; four domains). Each domain was Rasch-scored (converted to 0–100), and scores between groups were compared.
Results
A total of 40 subjects and 99 non-glasses-wearing controls, along with 1 parent for each child, were included. Children 5–11 and 12–17 years of age who wore glasses had lower PedEyeQ scores across all domains compared with controls (mean differences, −6 to −15; P ≤0.04 for each domain). Proxy scores were also lower for glasses wearers across age groups and domains (mean differences, −4 to −18; P ≤ 0.02), and Parent scores were lower for parents of children wearing glasses (mean differences, −6 to −18; P < 0.001 for each domain).
Conclusions
In this study, glasses wearers had reduced ER-QOL and functional vision compared with control subjects. Parents of children wearing glasses also experience reduced quality of life.
The Pediatric Eye Questionnaire (PedEyeQ) was developed to assess functional vision and eye-related quality of life (ER-QOL) in children with any eye condition and in their parents.1,2 In a previous validation study, we reported reduced functional vision and ER-QOL using the PedEyeQ in children with bilateral visual impairment.3 The present study evaluated a less severe but more common eye care scenario: glasses correction for refractive error. According to a national health survey conducted in 2016 by the Centers for Disease Control and Prevention,4 approximately 30% of boys and 36% of girls aged 6–17 years were wearing refractive correction. Nevertheless, although glasses wear in children is encountered relatively frequently, the effects of glasses in child’s functional vision and ER-QOL has not been rigorously studied. In addition, because glasses wear for refractive error is frequently a part of the treatment plan for many different pediatric eye conditions, it would be helpful to understand the effects of glasses wear for refractive error vis-à-vis those for other treatments. The aim of the present study was to characterize and quantify the combined effects of glasses-wear and refractive error on functional vision and ER-QOL in children and their families using the PedEyeQ.1, 2
Subjects and Methods
Institutional Review Board approval was obtained from institutional review boards at the Mayo Clinic, Rochester, Minnesota, and the University of Texas Southwestern Medical Center, Dallas, Texas. All procedures and data collection were conducted in a manner compliant with the US Health Insurance Portability and Accountability Act of 1996, and all research procedures adhered to the tenets of the Declaration of Helsinki. Subjects were prospectively enrolled at Mayo Clinic, Rochester, Minnesota, and at the Retina Foundation of the Southwest, Dallas, Texas.
We included developmentally normal 5- to 17-year-olds with normal visual acuity in each eye as assessed by using age-appropriate clinical tests (the testing method was not standardized but was typically HOTV5 or E-ETDRS6). Because normal visual acuity in young children differs by age, we defined normal thresholds for each year of age based on previously published normal values.7,8 Children wearing glasses for refractive error were identified in outpatient clinics or were referred by friends or colleagues or recruited through a flyer. Glasses were prescribed for full-time wear, and there were no exclusions based on the degree or type of refractive error. Children with no glasses or other refractive correction and normal visual acuity for age were enrolled as a control group. Thirty-six of these control subjects were reported in a previous validation study in children with visual impairment.3 Control subjects were recruited in the same manner as study subjects. We chose a control population with normal visual acuity and no glasses or other refractive correction rather than alternative controls, such as children wearing contact lenses, because we wanted to identify the effects of glasses wear and refractive error compared with no refractive correction rather the effects of two different types of refractive correction. In both groups, all children had no other current or previous eye condition/treatment.
The Pediatric Eye Questionnaire (PedEyeQ)
The PedEyeQ consists of Child, Proxy, and Parent components1 (full questionnaires with Rasch scoring freely available at www.pedig.net) and uses a three-point frequency scale for the responses: “never,” “sometimes,” and “all of the time.” The PedEyeQ was created from specific concerns identified in patient and parent interviews across a large, diverse clinical population, which yielded a large number of candidate questionnaire items.2 Subsequent administration and Rasch analysis of a subset of items in a second large clinical cohort resulted in the development of final of Child, Proxy, and Parent questionnaires, each with distinct domains.1 Children completed the Child PedEyeQ, and a parent or legal guardian for each child completed the Proxy and Parent PedEyeQ. The majority of children/parents completed questionnaires electronically on an iPad, others completing on paper.
The Child PedEyeQ consists of 5–11 years and 12–17 years versions, each with four distinct, separately-scored domains: “Functional vision,” “Bothered by eyes / vision,” “Social,” and “Frustration / worry.”1 The Proxy PedEyeQ consists of 0- to 4-, 5- to 11-, and 12- to 17-year-old versions. The Proxy 5–11 and 12–17 PedEyeQs used in the present study consist of five distinct domains, with “Eye care” added to the previous four.1 In both the Child and Proxy components, there were differences in questions between age-specific versions.1 The Parent PedEyeQ has four distinct domains: “Impact on parent / family,” “Worry regarding child’s eye condition,” “Worry regarding child’s self-perception and interactions,” and “Worry regarding child’s visual function.”1
Analysis
For each subject, on each PedEyeQ domain, Rasch scores were calculated using previously published look-up tables (www.pedig.net) and then converted to 0 (worst) to 100 (best) for interpretation. Domain scores for 5–11 and 12–17 years were analyzed separately. Median scores were compared between glasses wearers and controls by age group using Wilcoxon rank-sum tests, because data were not normally distributed. For ease of interpretation of results, mean differences with a 95% confidence interval around the mean difference were also calculated (because there can be a statistically significant difference in median values, despite identical median values). Effect sizes were calculated based on the mean difference between groups divided by the standard deviation of controls. Effect sizes of 0.20 to 0.49 are considered small; 0.50–0.79, medium; and >0.80, large.9 SAS software version 9.4 (SAS Institute, Cary, NC) was used for all statistical analyses.
Results
A total of 26 children 5–11 years of age (median, 8) and 14 children 12–17 years of age (median, 13.5) were included (Table 1). Demographics are shown in Table 1. In 5- to 11-year-olds, median refractive error (spherical equivalent) was +1.00 D (range, −3.75 to +6.125) and median cylinder was 1.25 D (range, 0.00–4.25 D). In 12- to 17-year-olds, median refractive error by spherical equivalent was −1.94 D (range, −6.75 to −0.50 D), and median cylinder was 0.50 D (range, 0.00–2.00 D). We also included 74 children 5–11 years of age (median, 7) and 25 children 12–17 years old (median, 13) as controlss. Demographics are shown in Table 1.
Table 1.
Demographics of 40 children wearing glasses for correction of refractive error, 99 children enrolled as normal controls, and their parents
| Study parameter | Refractive error | Normal controls | ||
|---|---|---|---|---|
| 5–11 years (n = 26), no. (%) | 12–17 years (n = 14), no. (%) | 5–11 years (n = 74), no. (%) | 12–17 years (n = 25), no. (%) | |
| Sex of child | ||||
| Female | 14 (54) | 7 (50) | 37 (50) | 10 (40) |
| Race | ||||
| White (including Hispanic / Latino) | 19 (73) | 12 (86) | 54 (73) | 16 (64) |
| Asian | 6 (23) | 0 (0) | 10 (14) | 3 (12) |
| More than 1 race | 1 (4) | 1 (7) | 9 (12) | 2 (8) |
| Black/African American | 0 (0) | 1 (7) | 1 (1) | 4 (16) |
| American Indian / Alaskan Native | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Native Hawaiian / Other Pacific Islander | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Other | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Ethnicity | ||||
| Not Hispanic / Latino and not Middle Eastern/North African and not Indian Subcontinent | 18 (69) | 11 (79) | 56 (76) | 19 (76) |
| Hispanic/Latino | 2 (8) | 3 (21) | 7 (9) | 1 (4) |
| Indian Subcontinental | 4 (15) | 0 (0) | 1 (1) | 0 (0) |
| Middle Eastern / North African | 0 (0) | 0 (0) | 2 (3) | 2 (8) |
| More than one | 2 (8) | 0 (0) | 9 (11) | 3 (12) |
| Parent / legal guardian completing questionnaires | ||||
| Mother | 22 (85) | 12 (86) | 65 (88) | 23 (92) |
| Father | 4 (15) | 2 (14) | 9 (12) | 2 (8) |
| Legal guardian | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Parent / legal guardian age | ||||
| 21–30 | 0 (0) | 0 (0) | 6 (8) | 0 (0) |
| 31–40 | 14 (54) | 2 (14) | 40 (54) | 9 (36) |
| 41–50 | 11 (42) | 10 (71) | 28 (38) | 15 (60) |
| 51–60 | 1 (4) | 2 (14) | 0 (0) | 1 (4) |
| Parent / legal guardian highest level of education | ||||
| Attended high school | 0 (0) | 0 (0) | 2 (3) | 1 (4) |
| High school graduate | 3 (12) | 0 (0) | 2 (3) | 1 (4) |
| Attended college | 3 (12) | 1 (7) | 14 (19) | 2 (8) |
| College graduate | 9 (35) | 3 (21) | 37 (50) | 15 (60) |
| Postgraduate / professional degree | 11 (42) | 10 (71) | 18 (24) | 6 (24) |
| Not reported | 0 (0) | 0 (0) | 1 (1) | 0 (0) |
| Housing | ||||
| Own | 23 (88) | 11 (79) | 58 (78) | 20 (80) |
| Rent | 2 (8) | 3 (21) | 15 (20) | 5 (20) |
| Other | 1 (4) | 0 (0) | 1 (1) | 0 (0) |
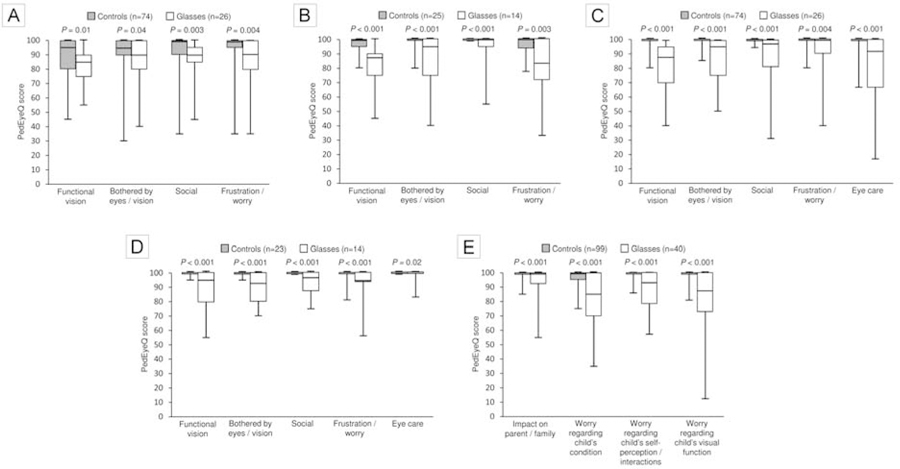
For 5- to 11-year-olds, median Child scores for glasses wearers were lower than those for controls on each domain (P ≤ 0.04 for each; Figure 1A; Table 2). For 12- to 17-year-olds, Child scores were significantly lower for glasses wearers than for controls for each domain (P ≤ 0.003 for each domain, Figure 1B; Table 2). The greatest difference was in the Frustration/Worry domain (median, 83 vs 100; mean difference, −15; 95% CI −26 to −4 [ P = 0.003]; Figure 1B; Table 2). Effect sizes ranged from 0.39 to 0.62 in 5- to 11-year-olds and from 2.18 to 3.31 in 12-to 17-year olds (Table 2).
FIG 1.
A, Child PedEyeQ domain scores in 5- to 11-year olds (“Functional vision,” “Bothered by eyes / vision,” “Social,” and “Frustration /worry”) comparing children wearing glasses for refractive error and controls not wearing glasses; scores lower across all domains (P ≤ 0.04). B, Child PedEyeQ domain scores in 12- to 17-year-olds (same domains) comparing glasses wearers and controls; scores were significantly lower for children wearing glasses for each domain (P < 0.003). C, Proxy PedEyeQ domain scores for 5- to 11-year-olds (same domains, with addition of “Eye care”) comparing glasses wearers and controls. Scores were significantly lower for children wearing glasses across domains (P ≤ 0.004). D, Proxy PedEyeQ domain scores for 12- to 17-year-olds (same domains as for younger children) comparing glasses wearers and controls. Scores were significantly lower for all domains (P ≤ 0.02). E, Parent PedEyeQ domain scores (“Impact on parent/family,” “Worry regarding child’s eye condition,” “Worry regarding child’s self-perception / interactions,” and “Worry regarding child’s visual function”) comparing parents of glasses wearers and parents of controls. Scores were significantly lower for parents of children wearing glasses across all domains (P < 0.001). Boxes represent 1st quartile, median, and 3rd quartile values; whiskers represent extreme values.
Table 2.
PedEyeQ domain scores for children wearing glasses for correction of refractive error, for normal controls, and for their parents
| PedEyeQ domains (by age group for Child and Proxy) | Median (range) PedEyeQ scores | P value for difference, median scores | Mean difference with 95% CI | Effect size | |
|---|---|---|---|---|---|
| Glasses | Controls | ||||
| Child 5–11 years | N = 26 | N = 74 | |||
| Functional vision | 85 (55–100) | 95 (45–100) | 0.01 | −6 (−12 to 0) | 0.48 |
| Bothered by eyes/vision | 90 (40–100) | 95 (30–100) | 0.04 | −8 (−15 to 0) | 0.62 |
| Social | 90 (45–100) | 100 (35–100) | 0.003 | −6 (−11 to 0) | 0.44 |
| Frustration/worry | 90 (35–100) | 100 (35–100) | 0.004 | −6 (−12 to 1) | 0.39 |
| Child 12–17 years | N=14 | N=25 | |||
| Functional vision | 87 (45–100) | 100 (80–100) | <0.001 | −15 (−23 to −6) | 2.63 |
| Bothered by eyes/vision | 95 (40–100) | 100 (80–100) | <0.001 | −15 (−27 to −2) | 3.30 |
| Social | 100 (55–100) | 100 (100–100) | <0.001 | −6 (−14 to 1) | N/Ab |
| Frustration/worry | 83 (33–100) | 100 (78–100) | 0.003 | −15 (−26 to −4) | 2.18 |
| Proxy 5–11 years | N = 26 | N = 74 | |||
| Functional vision | 87 (40–100) | 100 (80–100) | <0.001 | −18 (−25 to −11) | 5.02 |
| Bothered by eyes/vision | 95 (50–100) | 100 (85–100) | <0.001 | −12 (−19 to −5) | 5.25 |
| Social | 97 (31–100) | 100 (94–100) | <0.001 | −13 (−21 to −5) | 9.07 |
| Frustration/worry | 100 (40–100) | 100 (80–100) | 0.004 | −8 (−16 to −1) | 2.63 |
| Eye-care | 92 (17–100) | 100 (67–100) | <0.001 | −16 (−25 to −7) | 3.77 |
| Proxy 12–17 years | N=14 | N = 23a | |||
| Functional vision | 95 (55–100) | 100 (95–100) | <0.001 | −11 (−19 to −3) | 10.40 |
| Bothered by eyes/vision | 93 (70–100) | 100 (95–100) | <0.001 | −10 (−16 to −4) | 7.23 |
| Social | 97 (75–100) | 100 (100–100) | <0.001 | −7 (−12 to −2) | N/Ab |
| Frustration/worry | 94 (56–100) | 100 (81–100) | <0.001 | −9 (−17 to 0) | 2.19 |
| Eye care | 100 (83–100) | 100 (100–100) | 0.02 | −4 (−8 to 1) | N/Ab |
| Parent | N=40 | N=99 | |||
| Impact on parent/family | 100 (55–100) | 100 (85–100) | <0.001 | −6 (−10 to −2) | 3.88 |
| Worry regarding child’s condition | 85 (35–100) | 100 (75–100) | <0.001 | −17 (−23 to −11) | 3.32 |
| Worry regarding child’s self-perception/interactions | 93 (57–100) | 100 (86–100) | <0.001 | −11 (−16 to −7) | 6.63 |
| Worry regarding child’s visual function | 87 (12–100) | 100 (75–100) | <0.001 | −18 (−24 to −11) | 4.12 |
CI, confidence interval; N/A, not available.
Two parents in the normal control group did not complete the proxy questionnaires.
Effect size could not be calculated owing to standard deviation of 0 points in normal controls.
For both 5- to 11-year-olds (Figure 1C; Table 2) and 12- to 17-year-olds (Figure 1D; Table 2), Proxy scores were significantly lower for glasses wearers on each domain (P ≤ 0.02 for each). Effect sizes ranged from 2.63 to 9.07 for 5- to 11-year-olds and 2.19 to 10.40 for 12- to 17-year olds (Table 2).
Parent scores were also lower for parents of glasses wearers across all four domains (P < 0.001 for each; Figure 1E; Table 2). Effect sizes ranged from 3.32 to 6.63 (Table 2).
Discussion
ER-QOL and functional vision scores in 5- to 11-year-olds and 12- to 17-year-olds wearing glasses for correction of refractive error were lower than those of controls by both child self-report (Child PedEyeQ) and by parent report (Proxy PedEyeQ). In addition, we found lower ER-QOL in parents of glasses wearers. Although spectacle correction of refractive error might be considered a mild treatment, our study highlights a small but significant effect on both children and their parents.
The effects on children of wearing glasses has not been well studied. Some investigators10,11 have reported improved vision-related quality of life in children wearing contact lenses compared with glasses, but we are unaware of any studies comparing children with normal vision who wear glasses to children with normal vision who do not. Other studies have reported increased bullying,12 decreased satisfaction with physical appearance,13 lower attractiveness, and poorer school performance, conduct, and sociability14 associated with glasses wear, which, although not direct measures of ER-QOL, may be expected to affect a child’s ER-QOL. In contrast, Walline and colleagues15 reported that children wearing glasses were perceived by other children to be smarter and more honest than children not wearing glasses. In the present study, we used the recently developed PedEyeQ1 to assess everyday effects and found that on average children wearing glasses had lower ER-QOL and functional vision than controls when measured by Child self-report and Proxy report.
We also found that the parents of glasses wearers were affected by their children’s glasses. These findings are analogous to those of a previous study16 in which the Intermittent Exotropia Questionnaire was administered to nonstrabismic children with visual acuity of at least 20/40 who were either wearing glasses for correction of refractive error (n = 20) or who had no refractive error and no glasses (n = 29). In this previous study,16 scores on the Parent component of the Intermittent Exotropia Questionnaire were significantly lower for parents of children wearing glasses than for parents of children who did not wear glasses. It is possible that some parental worry is out of proportion to the state of a child wearing glasses for refractive error. It is possible that the effect on parents may be ameliorated by educational interventions.
Overall, the magnitude of mean differences between glasses wearers and controls was less (range of mean differences, −6 to −15) than those found in a previous study of children with visual impairment (range of mean differences, −10 to −46).3 This difference in magnitude of effect for children with visual impairment versus children with glasses correction of refractive error serves to confirm known-group validity of the PedEyeQ, with expected lower effect in glasses wearers and greater effect in visual impairment.
Our finding of reduced ER-QOL and functional vision in glasses wearers has implications when evaluating the effect of other pediatric eye conditions. When glasses wear is prescribed as part of a child’s treatment plan, care should be taken to acknowledge that a component of any ER-QOL and/or functional vision effect may in fact be attributable to glasses wear. Nevertheless, the magnitude of effect from glasses wear for a given child and/or a given eye condition remains unknown. We caution against applying the magnitude of effect found in the present study as a threshold for effect in any eye condition. Indeed, we speculate that the relative effect of glasses wear may be lower in a child with severe eye disease and higher in a child with mild disease.
The present study is not without limitations. The effects of underlying refractive error are difficult to distinguish from that of glasses wear to correct the refractive error, but the purpose of the present study was to evaluate the combined effect of refractive error and glasses wear in children. In future studies, it would be helpful to evaluate the effects of uncorrected refractive error followed by a reassessment of the combined effects of refractive error and glasses once they are prescribed. By including only children who had normal visual acuity in glasses, we aimed primarily to identify the effects of glasses wear itself. That said, we did not obtain a measure of adherence with glasses wear, and it is possible that some findings (eg, reduced functional vision) were related to the child’s experience when not wearing their glasses. Knowledge of glasses adherence may help with interpretation of ER-QOL and functional vision effects. In addition, we used a control group with normal visual acuity and no refractive correction, but additional questions remain regarding how glasses wear compares with other types of refractive correction (eg, contact lenses) in children with refractive error. Also, the relative effects of different types of refractive error and uncorrected or suboptimally corrected refractive error on a child’s ER-QOL and functional vision remains unclear. We enrolled only a relatively small number of children and heterogeneity regarding race/ethnicity was limited; our results may not be generalizable to all children wearing glasses.
Children wearing glasses for refractive error have reduced ER-QOL and functional vision compared with normal controls, as reported by the child themselves and by proxy reporters. Eye care providers should weigh the benefits and possible adverse effects when correcting very low levels of refractive error and when there is questionable benefit to vision.
Acknowledgments
Financial support: National Institutes of Health Grants EY024333 (JMH [PI] and EEB [Co-I]), EY011751 (JMH), and EY022313 (EEB), and Mayo Foundation, Rochester, Minnesota. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented in part at the Annual Meeting of the Association for Research in Vision and Ophthalmology meeting, Vancouver, BC, Canada, Monday April 28-May 2, 2019.
References
- 1.Hatt SR, Leske DA, Castañeda YS, et al. Development of pediatric eye questionnaires for children with eye disease. Am J Ophthalmol 2019;200:201–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hatt SR, Leske DA, Castañeda YS, et al. Patient-derived questionnaire items for patient-reported outcome measures in pediatric eye conditions. J AAPOS 2018;22:445–8.e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leske DA, Hatt SR, Castañeda YS, et al. Validation of the Pediatric Eye Questionnaire (PedEyeQ) in children with visual impairment. Am J Ophthalmol 2019;208:124–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.QuickStats: Percentage of children aged 6–17 years who wear glasses or contact lenses, by sex and age group—national health interview survey, 2016. MMWR Morb Mortal Wkly Rep 2017;66:917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: adaptation of the Amblyopia Treatment Study visual acuity testing protocol. Am J Ophthalmol 2001;132:903–9. [DOI] [PubMed] [Google Scholar]
- 6.Beck RW, Moke PS, Turpin AH, et al. A computerized method of visual acuity testing: adaptation of the Early Treatment of Diabetic Retinopathy Study testing protocol. Am J Ophthalmol 2003;135:194–205. [DOI] [PubMed] [Google Scholar]
- 7.Drover JR, Felius J, Cheng CS, Morale SE, Wyatt L, Birch EE. Normative pediatric visual acuity using single surrounded HOTV optotypes on the Electronic Visual Acuity Tester following the Amblyopia Treatment Study protocol. J AAPOS 2008;12:145–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pan Y, Tarczy-Hornoch K, Cotter SA, et al. ; Multi-Ethnic Pediatric Eye Disease Study Group. Visual acuity norms in pre-school children: the Multi-Ethnic Pediatric Eye Disease Study. Optom Vis Sci 2009;86:607–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cohen J Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc.; 1988:19–74. [Google Scholar]
- 10.Walline JJ, Gaume A, Jones LA, et al. Benefits of contact lens wear for children and teens. Eye Contact Lens 2007;33:317–21. [DOI] [PubMed] [Google Scholar]
- 11.Rah MJ, Walline JJ, Jones-Jordan LA, et al. ; ACHIEVE Study Group. Vision specific quality of life of pediatric contact lens wearers. Optom Vis Sci 2010;87:560–66. [DOI] [PubMed] [Google Scholar]
- 12.Horwood J, Waylen A, Herrick D, Williams C, Wolke D. Common visual defects and peer victimization in children. Invest Ophthalmol Vis Sci 2005;46:1177–81. [DOI] [PubMed] [Google Scholar]
- 13.Dias L, Hyman L, Manny RE, Fern K; COMET Group. Evaluating the self-esteem of myopic children over a three-year period: The COMET Experience. Optom Vis Sci 2005;82:338–47. [DOI] [PubMed] [Google Scholar]
- 14.Terry RL, Stockton LA. Eyeglasses and children’s schemata. J Soc Psychol 1993;133:425–38. [DOI] [PubMed] [Google Scholar]
- 15.Walline JJ, Sinnott L, Johnson ED, Ticak A, Jones SL, Jones LA. What do kids think about kids in eyeglasses? Ophthalmic and Physiological Optics 2008;28:218–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamada T, Hatt SR, Leske DA, Holmes JM. Spectacle wear in children reduces parental health-related quality of life. J AAPOS 2011;15:24–8. [DOI] [PMC free article] [PubMed] [Google Scholar]