Abstract
Background/Aims
Multiple meta-analyses and observational studies have reported that alcohol is a risk factor for liver cancer. However, whether there is a safe level of alcohol consumption remains unclear. We performed a systematic review and meta-analysis of the correlation between low-level alcohol consumption and the risk of liver cancer.
Methods
Nested case-control studies and cohort studies involving the general population published prior to July 2019 were searched. In total, 28 publications (31 cohorts) with 4,899 incident cases and 10,859 liver cancer-related deaths were included. The pooled odds ratios (ORs) with 95% confidence intervals (CIs) were calculated.
Results
Compared with those with low levels of alcohol consumption, moderate and heavy drinkers (≥1 drink/day for females and ≥2 drinks/day for males) had pooled ORs of 1.418 (95% CI, 1.192 to 1.687; p<0.001) for liver cancer incidence and 1.167 (95% CI, 1.056 to 1.290; p=0.003) for liver cancer mortality. The pooled OR for liver disease-related mortality for those with more than low levels of alcohol consumption was 3.220 (95% CI, 2.116 to 4.898; p<0.001) and that for all-cause mortality was 1.166 (95% CI, 1.065 to 1.278; p=0.001). The sensitivity analysis showed that none of the studies had a strong effect on the pooled OR. The Egger test, Begg rank correlation test, and the funnel plot showed no overt indication of publication bias.
Conclusions
Continuous consumption of more than a low-level of alcohol (≥1 drink/day for females and ≥2 drinks/day for males) is related to a higher risk of liver cancer.
Keywords: Alcohol, Liver neoplasms, Meta-analysis, Risk factors, Systematic review
INTRODUCTION
According to the World Health Organization, binge drinking is the leading cause of more than 200 diseases and injuries and is associated with premature death and disability; indeed, it is estimated that 3.3 million people worldwide die annually from drinking alcohol. In 1988, the International Agency for Research on Cancer categorized alcohol as a Group 1 human carcinogen.1 Additionally, the International Agency for Research on Cancer regards alcohol consumption as a cause of female breast, colorectal, laryngeal, hepatic, esophageal, oral, and pharyngeal cancers.2,3 Alcohol consumption is estimated to be responsible for 3.5% to 4.4% of cancer deaths annually worldwide.4-6
Animal studies have suggested that consumption of small amounts of alcohol, particularly red wine, can prevent cancer and ameliorate cardiovascular disease.7 However, clinical trials in humans have not provided corroborative evidence regarding the benefits of red wine.8 Few epidemiologic studies have addressed the association between alcohol consumption and cancer risk in humans. A Korean study reported that continuous alcohol consumption, even in small amounts, increases the incidence of esophageal and stomach cancer.9
The causes of chronic liver disease, including liver cancer, vary from region to region, but the most frequent are typically chronic viral hepatitis and alcohol. However, the recent development of effective therapeutics for chronic viral hepatitis has increased the importance of alcohol as a cause of liver disease. Alcohol can initiate the development of liver cancer and is related to tumor progression.10-12 Regular consumption of 40–60 g of alcohol is related to a higher risk of liver cancer; this level has been suggested to be lower for women.12,13 A recent meta-analysis on the incidence of alcohol-related liver cancer found a significant association between the risk of liver cancer and high-level alcohol consumption, with an excess risk of 66% for alcohol consumption of 100 g/day.14 Nevertheless, the effect of low-level alcohol consumption (<40 g/day) on the risk of liver cancer was not evaluated and the safe level of alcohol consumption for women was not proposed.
Therefore, we carried out a meta-analysis to determine whether there is a safe level of alcohol consumption in terms of liver cancer risk in men and women. In expressing the amount of alcohol consumption, existing studies used varying units of measurement (number of drinks, ounces, milliliters, or grams consumed every day, week, month, or year); in this study, grams per day (g/day) was used as the standard measure of alcohol intake using the following equivalences: one drink=0.8 g/mL=28 g/ounce=12.5 g/drink. According to the definitions in the U.S. Government Dietary Guidelines for Americans (2015 to 2020), light alcohol drinking was defined as less than two drinks/day in males and one drink/day in females.15 Using these criteria, we systematically reviewed the existing literature and performed a meta-analysis of the effect of alcohol consumption on the risk of liver cancer.
MATERIALS AND METHODS
1. Literature search
The search for relevant literature was independently performed by two authors (H.P. and S.K.S.), who searched for articles published prior to July 31, 2019 in Embase and PubMed, by using the following search terms: (alcohol OR ethanol) AND (neoplasm OR carcinoma OR cancer) AND (hepatocellular OR liver) AND (prospective OR cohort OR cohort studies [Medical Subject Headings; MeSH Terms]). The titles and abstracts of all retrieved studies were scanned to exclude all irrelevant studies, and inconsistencies were resolved by review of the full text and discussion. The full texts of the remaining papers were examined to assess their eligibility. We also examined the reference lists of all retrieved articles. This meta-analysis was performed according to the Preferred Reporting Items of the Systematic Reviews and Meta-Analyses statement.16
2. Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) original research articles of nested case-control or cohort studies (letters, reviews, and abstracts were excluded); (2) articles reporting the incidence and mortality of primary liver cancer or hepatocellular carcinoma as odds ratios (ORs), hazard ratios, or relative risks (RRs) (at least two levels of alcohol consumption vs nondrinkers and/or occasional drinkers); and (3) articles using standard errors or confidence intervals (CIs) of the risk estimates or those that provided sufficient data to calculate them. The exclusion criteria were: (1) non-English language articles; (2) non-human studies; and (3) no classification of alcohol consumption. When multiple studies involved the same population, the most recent article was included.
3. Data extraction and quality assessment
Two independent authors (H.P. and S.K.S.) extracted data from the included studies. The following details were retrieved from each study: (1) first author’s name and the year of publication, (2) country, (3) design, (4) follow-up period, (5) subjects’ gender distribution, (6) subjects’ mean age, (7) number of subjects, (8) classification of alcohol consumption, (9) effect size (OR, harzard ratio, or relative risk and 95% CI), and (10) confounders adjusted for. The Newcastle-Ottawa Scale (NOS) was used to estimate the quality of the studies.17 The NOS score ranges from 0 to 9 and is defined as the sum of the scores of the following three subscales: selection of studies, comparability, and outcome. A higher score indicates greater methodological quality. Studies with NOS scores ≥7 were noted as high quality.
4. Statistical analysis
We used the fixed- and random-effects models to estimate the pooled ORs with 95% CIs. Sufficiently homogenous groups of studies were analyzed with the fixed-effects model, and more heterogeneous groups of studies were analyzed with the random-effects model.18 We used Forest plots to identify the heterogeneity among studies, which was quantified using the I2 index, which represents the percentage of the total variability in a set of effect sizes rising from the true heterogeneity among studies.19 To evaluate the stability of the meta-analysis, we carried out a sensitivity analysis. The pooled OR of the remaining studies was computed by excluding one study at a time and compared with that of the fixed-effects model or random-effects model. The funnel plot or Egger regression test was utilized to evaluate the publications.20 When the articles provided ORs by using a different reference category, the ORs were newly calculated by dividing each OR by the OR for non-drinking; CIs were calculated by employing the standard errors of the crude OR estimates that were penalized by a factor of 1.5.21,22
Comprehensive Meta-Analysis version 2.0 (Biostat, Inc., Englewood, NJ, USA) was used for carrying out all statistical analyses. p-values smaller than 0.05 (two-sided) were considered statistically significant.
RESULTS
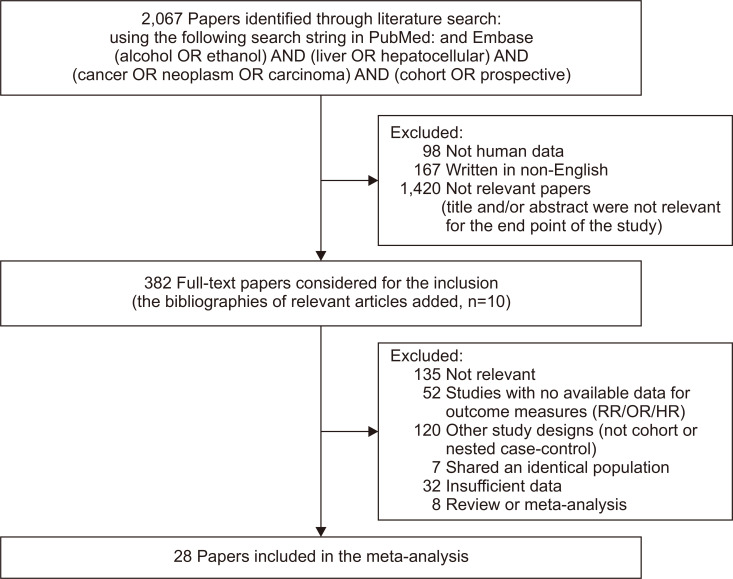
A total of 2,067 articles were initially retrieved from PubMed and Embase. After applying the exclusion criteria, the full texts of 382 potentially relevant studies were reviewed. Of these, 28 were finally included for meta-analysis (Fig. 1):22-49 22 were cohort studies and six nested case-control studies; 18 studies were from Asia, five were from the United States, and the other five were from Europe.
Fig. 1.
Flowchart of the literature search and inclusion criteria of the meta-analysis.
RR/OR/HR, relative risk/odds ratio/hazard ratio.
Table 1 shows the characteristics of the included studies. In total, 28 publications (31 cohorts) were included. A total of 4,899 incident cases and 10,859 deaths from liver cancer were included in the articles as a whole. A total of 1,669 deaths from liver disease and 91,256 all-cause deaths were also included.
Table 1.
Characteristics of the Studies Included in the Meta-Analysis
| First author (year) | Country | Study design | Mean follow-up, yr | Sex | Age, yr* | Participants (total) | Case (HCC incidence) | Case (HCC induced death) | Case (liver disease-related death) | Case (all-cause death) | Classification of alcohol consumption | Adjusted covariates |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Allen (2009)23 | UK | Cohort | 7.2 | F | 55 | 12,980,296 | 337 | ≤2 vs none, 3–6, 7–14, ≥15 drinks/wk | Age, region of residence, socioeconomic status, BMI, smoking, physical activity, use of oral contraceptives, and hormone replacement therapy | |||
| Persson (2013)22 | USA | Cohort | 10.5 | M/F | 50–71 | 404,743 | 435 | 785 | <1 vs none, 1–3, >3 drinks/day | Sex, age, race, education, smoking, BMI, and diabetes | ||
| Kawamura (2016)25 | Japan | Cohort | 5.4 | M/F | 19–96 | 9,959 | 49 | <20 vs 20–39, 40–69, ≥70 g/day | Sex, age, BMI, alcohol intake, albumin, bilirubin, AST, ALT, LDH, G-GTP, PLT, DM, uric acid, total cholesterol, TG, LDL, HDL | |||
| Schwartz (2013)24 | Finland | Cohort | 7 | M | 50–69 | 29,133 | 194 | 213 | <5.33 vs 5.33–20.44, >20.44 g/day | Age, education, smoking, BMI, DM, study arm | ||
| Setiawan (2016)26 | USA | Cohort | 19.6 | M/F | 45–75 | 38,684 | 189 | None vs <2, ≥2 drinks/day | Cohort entry, education, BMI, alcohol intake, smoking status, diabetes, vigorous activity, and sex | |||
| Cohort (USA born) | 19.6 | M/F | 45–75 | 18,485 | 194 | |||||||
| Cohort (foreign born) | 19.6 | M/F | 45–75 | 18,379 | 104 | |||||||
| Michikawa (2012)27 | Japan | Cohort | 7 | M/F | 40–69 | 17,654 | 104 | <150 vs 150–450 ≥450 g/wk | Age, sex, area, alcohol consumption, BMI, diabetes, coffee consumption, HBsAg, and anti-hepatitis C virus antibody | |||
| Chen (1996)28 | Taiwan | Nested case-control | 2 | M/F | 30–65 | 156 | 33 | None vs <20, ≥20 L/yr | Age, sex | |||
| Ohishi (2008)29 | Japan | Nested case-control | 32 | M/F | 67.6 | 868 | 224 | None vs 0–20, 20–40, ≥40 g/day | Hepatitis virus infection, continuous alcohol consumption, smoking habit, coffee drinking, BMI, DM, and radiation dose to the liver | |||
| Koh (2011)30 | Singapore | Nested case-control | 11.5 | M/F | 45–74 | 366 | 92 | None vs less than daily <2, ≥2 drinks/day | Gender, age at recruitment (yr), year of recruitment, dialect group (Hokkien, Cantonese), and the level of education, BMI (<20, 20–24, >24 kg/m2), DM (yes, no), and cups of coffee per day | |||
| Trichopoulos (2011)31 | Europe | Nested case-control | 8.9 | M/F | 25–70 | 344 | 115 | M <10, F <5 vs M 10–40, F 5–20, M ≥40, F ≥20 g/day | All indicated possible risk factors | |||
| Yuan (2004)32 | USA | Nested case-control | 15 | M | 18–74 | 465 | 245 | None vs 0–2, 2–4, >4 drinks/day | Age, gender, race, and level of education, smoking status, number of alcoholic drinks per day, and history of diabetes | |||
| Loftfield (2016)33 | Finland | Nested case-control | 22 | M | 50–69 | 391 | 138 | ≤11.3 vs >11.3 g/day | Age-adjusted | |||
| Yi (2018)34 | Korea | Cohort | 10.5 | M/F | 53.0 | 504,646 | 2,744 | None vs <10, 10–39, ≥40 g/day | Age, sex, smoking status, alcohol use, physical activity, income status, BMI, diabetes status, cirrhosis and hepatitis B virus and C virus infection | |||
| Kim (2010)35 | Korea | Cohort | 5 | M | 48.3 | 919,199 | 1,506 | 16,108 | None vs 1–14.9, 15–29.9, 30–89.9, ≥90 g/day | Age, residential (urban, rural), smoking status (current, former, never), ≥3 times/wk regular exercise (yes, no), BMI (kg/m2, continuous), systolic and diastolic blood pressure (mm Hg, continuous), and fasting blood sugar (mg/dL, continuous) | ||
| Kim (2010)35 | Korea | Cohort | 5 | F | 49 | 422,194 | 174 | 3,267 | None vs 1–14.9, ≥15 g/day | Age, residential (urban, rural), smoking status (current, former, never), ≥3 times/wk regular exercise (yes, no), BMI (kg/m2, continuous), systolic and diastolic blood pressure (mm Hg, continuous), and fasting blood sugar (mg/dL, continuous) | ||
| Yi (2010)36 | Korea | Cohort | 20.8 | M | 66.3 | 2,696 | 36 | None vs <138, <540, ≥540 g/wk | Age (year of recruitment), history of chronic disease, smoking habit, ginseng intake, pesticide use, BMI, and education status | |||
| Korea | Cohort | 20.8 | F | 66.9 | 3,595 | 52 | None vs <12, ≥12 g/wk | Age (year of recruitment), history of chronic disease, smoking habit, ginseng intake, pesticide use, BMI, and education status | ||||
| Yang (2012)37 | China | Cohort | 15 | M | 40–79 | 220,000 | 1,115 | 20,977 | None vs <140, 140–279, 280–419, 420–699, ≥700 g/wk | Age, area, smoking and education | ||
| Jee (2004)38 | Korea | Cohort | 10 | M/F | 30–95 | 1,329,525 | 3,341 | None vs 1–24.9, 25–49.9, 50–99.9, ≥100 g/day | Age, age squared, smoking, alcohol use, and diabetes | |||
| Joshi (2008)39 | Korea | Cohort | 6 | M | 30–59 | 548,530 | 998 | None vs 1–24, 25–49, 50–99, ≥100 g/day | Age, fasting serum glucose, BMI, alcohol intake and tobacco smoking, HBsAg | |||
| Jung (2012)40 | Korea | Cohort | 9.3 | M/F | >20 | 15,683 | 85 | ≤90 vs none, 90.01–252, 252.01–504, >504 g/wk | Age, sex, BMI, smoking habit, geographic area, and educational attainment | |||
| Kono (1986)41 | Japan | Cohort | 19 | M | 5,135 | 51 | 1,283 | None/past vs occasional, <2, ≥2 go of sake/day | Age, smoking | |||
| Park (2006)42 | Korea | Cohort | 7 | M | 50.8 | 14,578 | 2,013 | None vs 1–124.1 ≥124.2 g/wk | Age, alcohol consumption, BMI, fasting serum glucose level, cholesterol level, physical activity, food preference, blood pressure, and other comorbidities (heart disease, liver disease, and cerebrovascular disease) | |||
| Shih (2012)43 | Taiwan | Cohort | 10 | M/F | 20–75 | 2,273 | 1,488 | None vs ex-drinker, <19.4, 19.5–46.1, 46.2–106.9, ≥107 g/day | Adjusted for age at recruitment, sex, maximum tumor size (<3, 3 to <5 or 5 cm), number of lesions (1, 2–3 or 4), serum a-fetoprotein levels (<20, 20–151, 152–1,519 or 1,520 ng/mL), cigarette smoking (yes or no), history of liver cirrhosis and status of HBsAg and anti-HCV | |||
| Yi (2016)44 | Korea | Cohort | 6 | M | 58.8 | 187,897 | 338 | <1 vs 1–6, 7–13, 14-27, ≥28 drinks/wk | Adjusted for age at entry, smoking status, physical activity, household income, and BMI | |||
| Younoszai (2014)45 | USA | Cohort | 14.6 | M/F | 20–74 | 8,966 | 26 | 1,130 | <20 (M) (10 [F]) vs >20 g/day | Statin use, age, male, race, alcohol consumption, obesity, diabetes, HTN, cancer, elevated liver enzyme | ||
| Fuchs (1995)46 | USA | Cohort | 12 | F | 30–55 | 85,709 | 836 | 0 vs 0.1–1.4, 1.5–4.9, 5.0–14.9, 15.0–29.9, ≥30 g/day | Adjusted for age (in 5-yr categories), smoking status, BMI (in quintiles), regular aspirin use (2 days/wk), regular vigorous exercise (1 day/wk), high plasma cholesterol level, diabetes, HTN, myocardial infarction in a parent at 60 yr of age, past or present oral-contraceptive use, menopausal status, past or present postmenopausal hormone use, and energy-adjusted intake of dietary fiber and saturated fat | |||
| Marugame (2007)47 | Japan | Cohort | 11.9 | M/F | 40–69 | 41,702 (M)/ 47,044 (F) | 2,658 (M)/ 9,338 (F) | Occasional drink vs 1–149, 150–299, 300–449, 450 g/wk | Adjusted for age at baseline (continuous), study area (nine public health center areas), smoking status, BMI, green vegetable intake (3–4 times/wk and almost every day), and leisure-time physical activity | |||
| Ferrari (2014)48 | Europe | Cohort | 12.6 | M | 25–70 | 101,935 (M)/247,795 (F) | 8,964 (M)/11,492 (F) | 0.1–4.9 vs never, 5–14.9, 15–29.9, 30–59.9, ≥60 g/day | Age at recruitment, BMI and height, former drinking, time since alcohol quitting, smoking status, duration of smoking, age at start smoking, educational attainment and energy intake | |||
| Saito (2018)49 | Japan | Cohort | 18.2 | M/F | 40–69 | 102,849 | 15,203 | Never vs 1–149, 150–299, 300–449, 450–599, ≥600 g/wk | Adjusted for age, smoking status (never, former, <20, ≥20 cigarettes/day), BMI (<18.5, 18.5 to <25, 25 to <30, ≥30), history of HTN, flushing response, history of diabetes, leisure-time sports or physical exercise, intake of coffee and green tea (almost never, ≥1 cup/wk, and ≥1 cup/day), energy intake, intakes of fruits, vegetables, fish, meat, dairy products, and job status |
HCC, hepatocellular carcinoma; M, male; F, female; BMI, body mass index; AST, aspartate aminotransferase; ALT, alanine aminotransferase; LDH, lactic dehydrogenase; G-GTP, gamma glutamyl transpeptidase; PLT, platelet count; DM, diabetes mellitus; TG, triglyceride; LDL, low density lipoprotein; HDL, high density lipoprotein; HBsAg, hepatitis B surface antigen; HTN, hypertension.
*Mean or range.
Tables 2 and 3 shows the methodological qualities of the cohort and nested case-control studies. The average score was 7.5 for case-control studies and 8.5 for cohort studies (range, 7–9). All included studies were of high quality (NOS score ≥7). Quality assessment regarding alcohol and mortality from liver cancer, all-cause, and liver diseases was also performed (Supplement Tables 1-3).
Table 2.
Methodological Quality of the Cohort Study Included in the Final Analysis of Hepatocellular Carcinoma Incidence Based on the Newcastle-Ottawa Scale
| Cohort study | Selection | Comparability | Outcome | Score | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the exposed cohort | Selection of the non-exposedcohort | Ascertainmentof exposure | Demonstration that outcome of interest was not present at start of study | Comparability of cohorts on the basis of the design or analysis | Assessment of outcome | Was follow-up long enough for outcomes to occur | Adequacy of follow-up of cohorts | Total (0–9) | ||||
| Allen (2009)23 | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 | |||
| Persson (2013)22 | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 | |||
| Kawamura (2016)25 | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 | |||
| Schwartz (2013)24 | - | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |||
| Setiawan (2016)26 | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8 | |||
| Michikawa (2012)27 | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 | |||
Table 3.
Methodological Quality of the Case-Control Study Included in the Final Analysis of Hepatocellular Carcinoma Incidence Based on the Newcastle-Ottawa Scale
| Case-control study | Selection | Comparability | Outcome | Score | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Is the case definition adequate? | Representativeness of the cases | Selection of controls | Definition of controls | Comparability of cases and controls on the basis of the design or analysis | Ascertainment of exposure | Same method of ascertainment for cases and controls | Total (0–9) | ||||
| Chen (1996)28 | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |||
| Ohishi (2008)29 | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |||
| Koh (2011)30 | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |||
| Trichopoulos (2011)31 | - | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 7 | |||
| Yuan (2004)32 | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | - | 7 | |||
| Loftfield (2016)33 | ☆ | - | ☆ | ☆ | ☆☆ | ☆ | ☆ | 7 | |||
| Yi (2018)34 | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |||
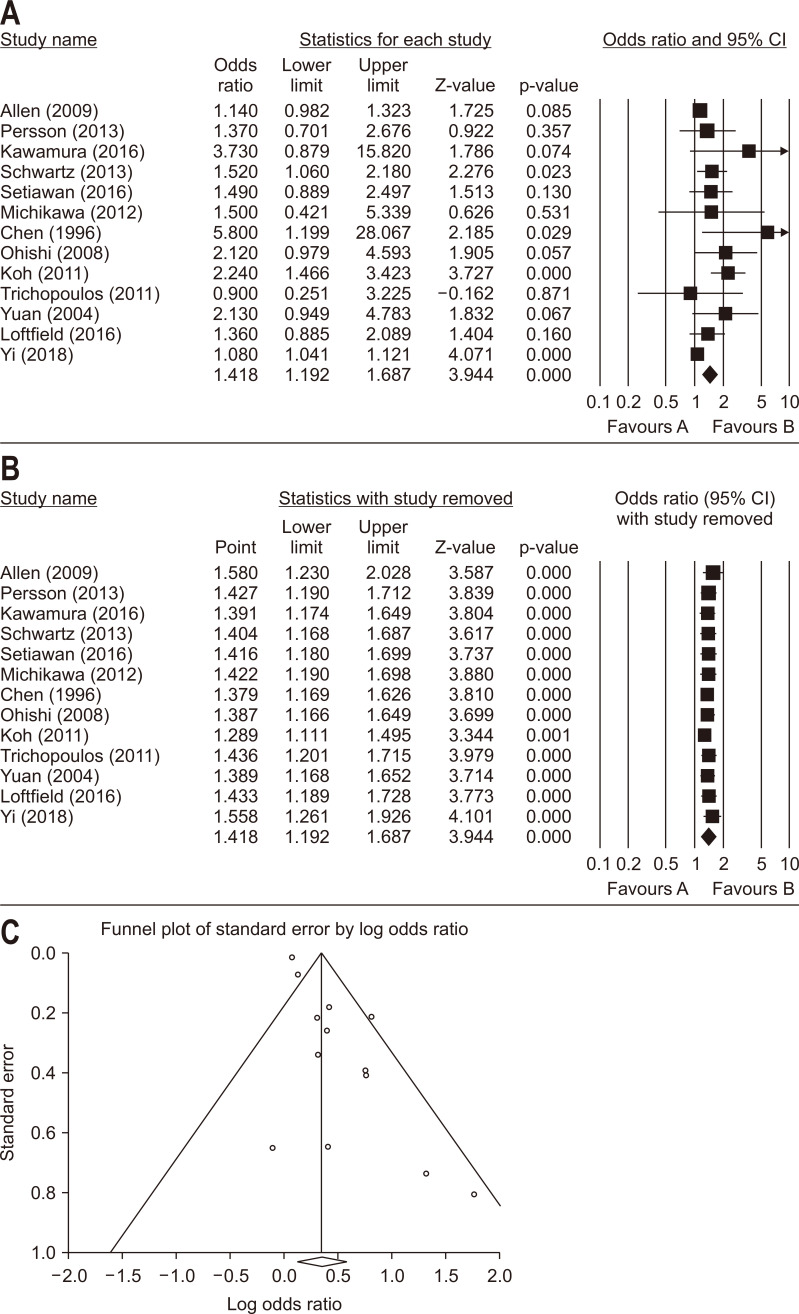
Fig. 2A shows the Forest plot regarding the relationship between the incidence of liver cancer and more than light drinking versus never or light drinking. The pooled OR was 1.418 (95% CI, 1.192 to 1.687; p<0.001; I2=60.5%) based on 13 studies. The sensitivity analysis showed that no single study had significantly affected the overall results (Fig. 2B). The funnel plot in the analysis of liver cancer incidence and more than light drinking versus never or light drinking showed evidence of publication bias in Egger test (p=0.010), but not Begg rank correlation test (p=0.502) (Fig. 2C). After using the trim-and-fill analysis to correct for this bias, a pooled OR of 1.141 (95% CI, 0.958 to 1.259) was calculated using the random-effects model.
Fig. 2.
Meta-analysis of studies examining the relationship between the incidence of liver cancer and moderate/heavy light alcohol consumption versus never or a low level of alcohol consumption. (A) Forest plot; (B) sensitivity test; (C) funnel plot.
CI, confidence interval.
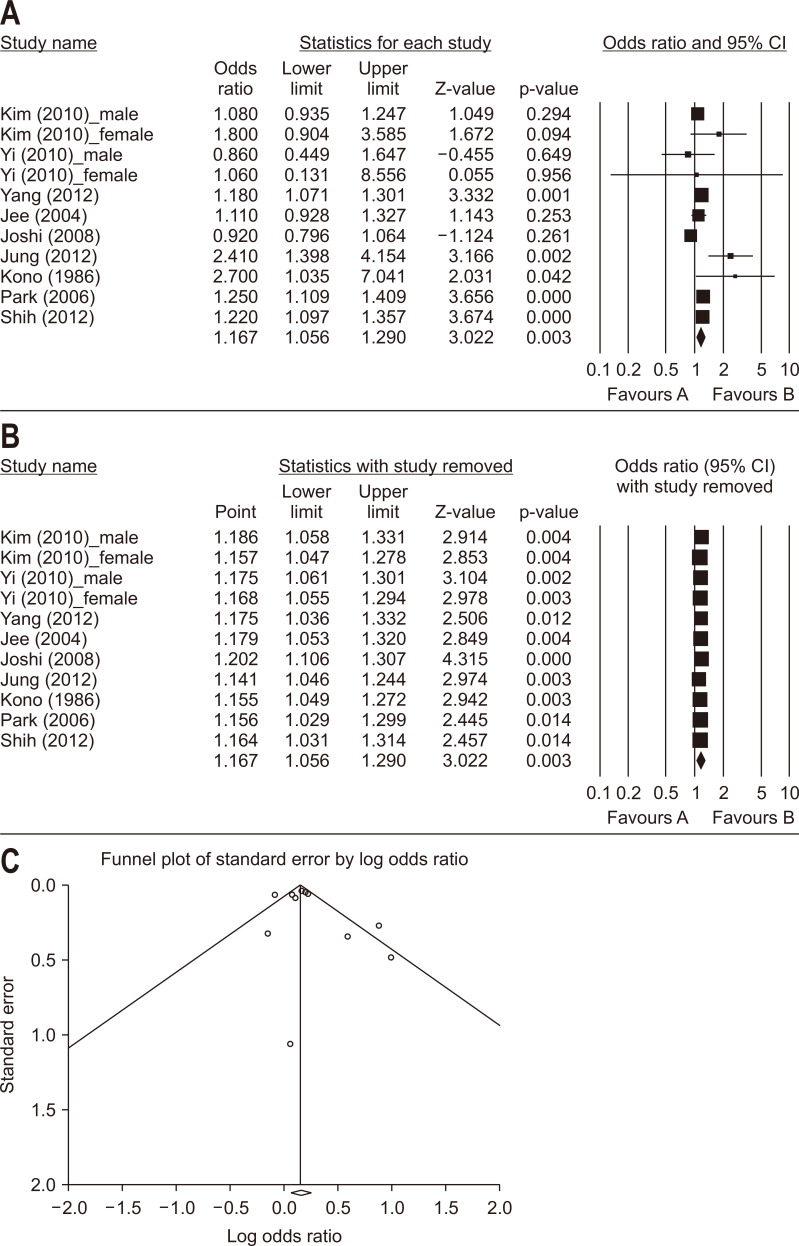
The pooled OR for mortality from liver cancer for more than light drinking versus never or light drinking was 1.167 (95% CI, 1.056 to 1.290; p=0.003; I2=61.1%) based on nine studies (11 cohorts) (Fig. 3A). The sensitivity analysis demonstrated that no single study conferred a significant impact on the pooled OR (Fig. 3B). The funnel plot, Egger (p=0.409) and Begg rank correlation test (p=0.640) indicated no overt indication of publication bias in the analysis of liver cancer mortality (Fig. 3C).
Fig. 3.
Meta-analysis of studies examining the relationship between mortality from liver cancer and moderate/heavy alcohol consumption versus never or a low level of alcohol consumption. (A) Forest plot; (B) sensitivity test; (C) funnel plot.
CI, confidence interval.
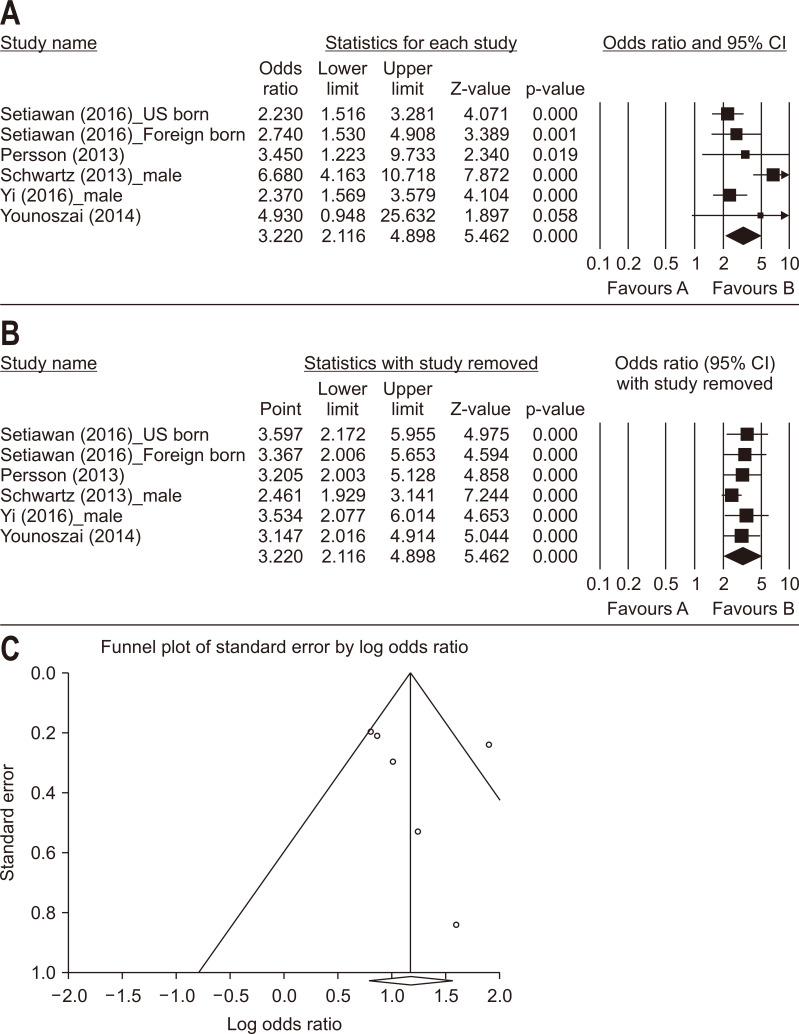
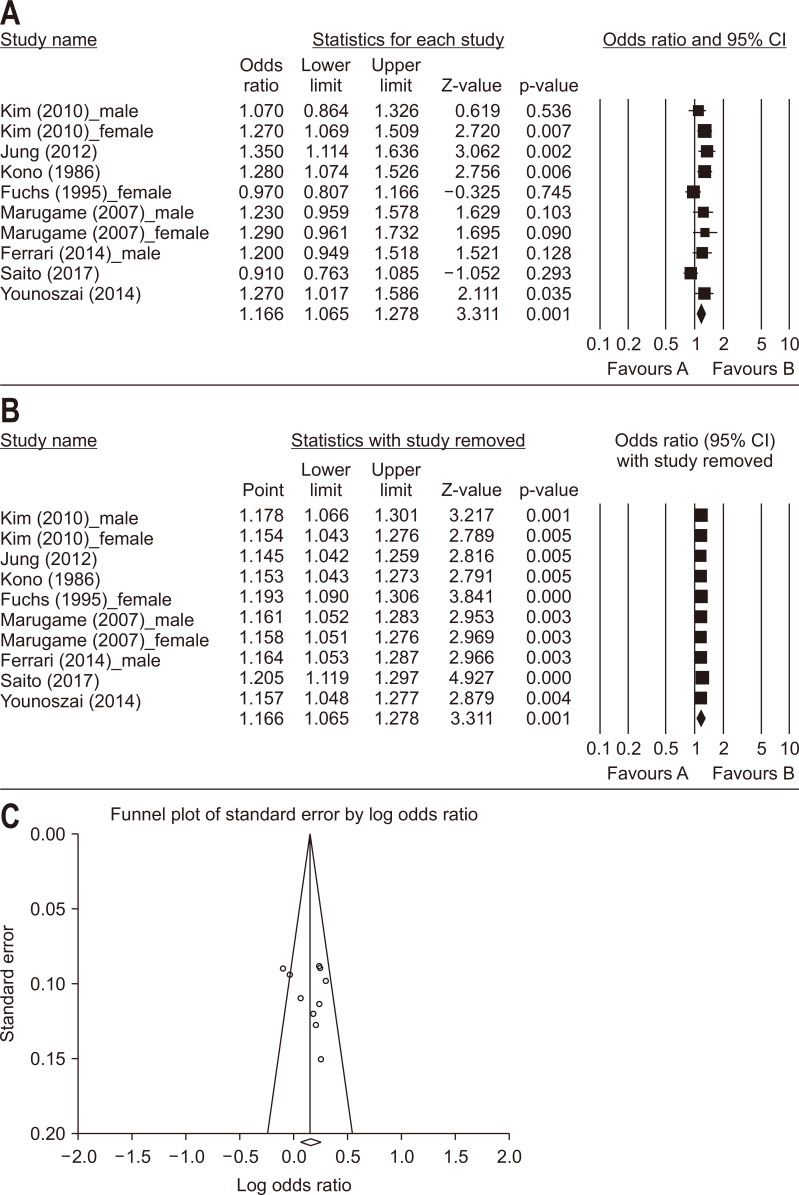
The pooled OR of liver disease-related mortality for more than light drinking versus never or light drinking was 3.220 (95% CI, 2.116 to 4.898; p<0.001; I2=66.7%) based on five studies (six cohorts) (Fig. 4A). The pooled OR for all-cause mortality for more than light drinking versus never or light drinking was 1.166 (95% CI, 1.065 to 1.278; p=0.001; I2=48.9%) based on eight studies (10 cohorts) (Fig. 5A). In both analyses, the sensitivity analysis demonstrated that no single study conferred a significant impact on the pooled OR (Figs. 4B, 5B), and the funnel plot, Egger (p=0.603 and p=0.466, respectively) and Begg rank correlation test (p=0.133 and p=1.000, respectively) indicated no overt indication of publication bias (Figs. 4C, 5C).
Fig. 4.
Meta-analysis of studies examining the relationship between liver disease-related mortality and moderate/heavy alcohol consumption versus never or a low level of alcohol consumption. (A) Forest plot; (B) sensitivity test; (C) funnel plot.
CI, confidence interval.
Fig. 5.
Meta-analysis of studies examining the relationship between all-cause mortality and moderate/heavy alcohol consumption versus never or a low level of alcohol consumption. (A) Forest plot; (B) sensitivity test; (C) funnel plot.
CI, confidence interval.
DISCUSSION
We investigated the relationship between liver cancer and alcohol consumption. Most previous studies of the incidence and mortality of liver cancer have been conducted on people who drink more than 40–69 g of alcohol per day for both genders. In this study, however, light alcohol consumption standards of less than two drinks/day for males and one drink/day for females were used for analysis. We also assessed the overall relationship between alcohol and liver disease based not only on the incidence of liver cancer and the associated mortality rates but also on the mortality rate of liver disease and the all-cause mortality rate.
More than light alcohol drinkers had a 42% increased risk of liver cancer incidence and 17% increased risk of liver cancer death compared to those who drink less alcohol. The liver-related mortality rate was 3.2-fold higher in more than moderate drinkers compared to those who drink less alcohol, demonstrating that consumption of even one or two alcoholic drinks daily can have an adverse effect on health. The risk of all-cause mortality in more than light drinkers was 16% higher compared to those who drink less alcohol. A slight decrease in the risk of all-cause mortality compared to that of liver-related mortality can be assumed that cardiovascular diseases reported to be able to protect with a small amount of drinking was included in all-cause mortality.
Studies in animals have shown that alcohol consumption in small amounts, especially red wine, can prevent cancer and ameliorate cardiovascular disease. Indeed, some components of red wine, such as resveratrol, have anticancer activity.7 Resveratrol is also present in peanuts, grapes, raspberries, and some other plants. Resveratrol is a polyphenol antioxidant produced by various plants to defend against fungi, stress, injury, infection, and excess sunlight; moreover, its effect on cancer and heart disease is under investigation. However, clinical trials have shown that resveratrol is not effective for preventing or treating cancer.8 Alcohol was categorized as a human liver carcinogen by the International Agency for Research on Cancer in 1988.1 Alcohol can initiate the development of liver cancer and is significantly associated with tumor progression. The underlying mechanisms of the promotion by alcohol and its metabolite, acetaldehyde, of liver carcinogenesis include:10-12 (1) increased oxidative stress, which damages DNA and hampers its repair; (2) induction of liver injury, promoting fibrogenesis and cirrhosis (most alcohol-related liver cancers develop from liver cirrhosis); (3) interactions with other environmental carcinogens, such as tobacco smoke; (4) interruption of one-carbon metabolism, leading to impaired DNA methylation and altered gene expression.
Previous meta-analyses have reported that regular consumption of 40–60 g of alcohol is related to a higher risk of liver cancer and proposed a lower level of safe alcohol consumption for women.12,13 Turati et al.14 systematically reviewed and meta-analyzed the relation between alcohol intake and the incidence of liver cancer and death by including 16 articles (19 cohorts) that comprised a total of 4,445 incident cases and 5,550 liver cancer-related deaths; as a results, the authors found a significant linear association between alcohol consumption and liver cancer risk (excess risk 46% for 50 g of alcohol per day and 66% for 100 g per day). Although the authors reported a dose-risk association between alcohol consumption and liver cancer risk, they did not evaluate the risk of consumption of smaller amounts of alcohol and did not analyze gender standards separately. Additionally, the risk of liver cancer comprised both the incidence and mortality rates of liver cancer; these were not evaluated separately. Another recent meta-analysis demonstrated that alcohol consumption is associated with a higher risk of liver cancer in a dose-dependent manner (8% for 12 g alcohol per day, 54% for 50 g per day, and 3.2-fold for 100 g per day).50 Moreover, synergistic effects with other risk factors such as hepatitis and diabetes were detected. However, the enrolled studies showed significant heterogeneity as well as publication bias.
This study had the following limitations. First, we may have omitted the liver cancer data included in the results of our study with all kinds of cancer since we found a paper exclusively for the event in livers. Secondly, there was some heterogeneity among the articles, as with most meta-analyses. However, we overcame this limitation by applying random-effects and fixed-effects models according to heterogeneity. Sensitivity analyses supported the robustness of our study results. Moreover, Egger tests for funnel plot asymmetry and the funnel plot did not indicate the presence of major publication bias.
In conclusion, this meta-analysis supports previous reports of the association between alcohol consumption and the risk of liver cancer. Furthermore, our research shows that continuous consumption of even a small amount of alcohol is related to liver cancer risks. Based on this analysis, more than light alcohol consumption should be considered harmful as it not only increases the incidence of liver cancer but also increases liver disease and overall mortality.
Supplementary material
ACKNOWLEDGEMENTS
This study project was supported by The Korean Liver Cancer Association.
We thank Professor Hyeon Woo Yim (Catholic University of Korea), Hyunsuk Jeong (Catholic University of Korea), Kwang-Pil Ko (Gachon University College of Medicine) and Seokyung Hahn (Seoul National University College of Medicine) for their helpful statistical assistance. The statistical consultation was supported by Catholic Research Coordinating Center of the Korea Health 21 R&D Project (A070001), Ministry of Health & Welfare, and Republic of Korea.
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Study concept and design: H.P., S.K.S., I.J., D.S.S., J.W.J. Data acquisition; data analysis and interpretation: H.P., S.K.S., J.W.J. Drafting of the manuscript; critical revision of the manuscript for important intellectual content: H.P., S.K.S. Statistical analysis: H.P., S.K.S. Study supervision: J.W.J., J.W.P.
REFERENCES
- 1.Alcohol drinking, author. IARC Working Group, Lyon, 13-20 October 1987. IARC Monogr Eval Carcinog Risks Hum. 1988;44:1–378. [PMC free article] [PubMed] [Google Scholar]
- 2.IARC Working Group on the Evaluation of Carcinogenic Risks to Humans, author. Alcohol consumption and ethyl carbamate. IARC Monogr Eval Carcinog Risks Hum. 2010;96:3–1383. [PMC free article] [PubMed] [Google Scholar]
- 3.Cogliano VJ, Baan R, Straif K, et al. Preventable exposures associated with human cancers. J Natl Cancer Inst. 2011;103:1827–1839. doi: 10.1093/jnci/djr483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- 5.Liang H, Wang J, Xiao H, et al. Estimation of cancer incidence and mortality attributable to alcohol drinking in China. BMC Public Health. 2010;10:730. doi: 10.1186/1471-2458-10-730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nelson DE, Jarman DW, Rehm J, et al. Alcohol-attributable cancer deaths and years of potential life lost in the United States. Am J Public Health. 2013;103:641–648. doi: 10.2105/AJPH.2012.301199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Athar M, Back JH, Tang X, et al. Resveratrol: a review of preclinical studies for human cancer prevention. Toxicol Appl Pharmacol. 2007;224:274–283. doi: 10.1016/j.taap.2006.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel KR, Scott E, Brown VA, Gescher AJ, Steward WP, Brown K. Clinical trials of resveratrol. Ann N Y Acad Sci. 2011;1215:161–169. doi: 10.1111/j.1749-6632.2010.05853.x. [DOI] [PubMed] [Google Scholar]
- 9.Choi YJ, Lee DH, Han KD, et al. The relationship between drinking alcohol and esophageal, gastric or colorectal cancer: a nationwide population-based cohort study of South Korea. PLoS One. 2017;12:e0185778. doi: 10.1371/journal.pone.0185778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Testino G. The burden of cancer attributable to alcohol consumption. Maedica (Buchar) 2011;6:313–320. [PMC free article] [PubMed] [Google Scholar]
- 11.Stickel F, Schuppan D, Hahn EG, Seitz HK. Cocarcinogenic effects of alcohol in hepatocarcinogenesis. Gut. 2002;51:132–139. doi: 10.1136/gut.51.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singal AK, Anand BS. Mechanisms of synergy between alcohol and hepatitis C virus. J Clin Gastroenterol. 2007;41:761–772. doi: 10.1097/MCG.0b013e3180381584. [DOI] [PubMed] [Google Scholar]
- 13.Donato F, Gelatti U, Limina RM, Fattovich G. Southern Europe as an example of interaction between various environmental factors: a systematic review of the epidemiologic evidence. Oncogene. 2006;25:3756–3770. doi: 10.1038/sj.onc.1209557. [DOI] [PubMed] [Google Scholar]
- 14.Turati F, Galeone C, Rota M, et al. Alcohol and liver cancer: a systematic review and meta-analysis of prospective studies. Ann Oncol. 2014;25:1526–1535. doi: 10.1093/annonc/mdu020. [DOI] [PubMed] [Google Scholar]
- 15.Dietary guidelines for American 2015-2020 [Internet] U.S. Department of Health and Human Services and U.S. Department of Agriculture; Rockville: c2015. [cited 2020 Feb 10]. Available from: https://health.gov/dietaryguidelines/2015/guidelines/ [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group, author. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 18.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shimazu T, Sasazuki S, Wakai K, et al. Alcohol drinking and primary liver cancer: a pooled analysis of four Japanese cohort studies. Int J Cancer. 2012;130:2645–2653. doi: 10.1002/ijc.26255. [DOI] [PubMed] [Google Scholar]
- 22.Persson EC, Schwartz LM, Park Y, et al. Alcohol consumption, folate intake, hepatocellular carcinoma, and liver disease mortality. Cancer Epidemiol Biomarkers Prev. 2013;22:415–421. doi: 10.1158/1055-9965.EPI-12-1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Allen NE, Beral V, Casabonne D, et al. Moderate alcohol intake and cancer incidence in women. J Natl Cancer Inst. 2009;101:296–305. doi: 10.1093/jnci/djn514. [DOI] [PubMed] [Google Scholar]
- 24.Schwartz LM, Persson EC, Weinstein SJ, et al. Alcohol consumption, one-carbon metabolites, liver cancer and liver disease mortality. PLoS One. 2013;8:e78156. doi: 10.1371/journal.pone.0078156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kawamura Y, Arase Y, Ikeda K, et al. Effects of alcohol consumption on hepatocarcinogenesis in Japanese patients with fatty liver disease. Clin Gastroenterol Hepatol. 2016;14:597–605. doi: 10.1016/j.cgh.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 26.Setiawan VW, Wei PC, Hernandez BY, et al. Disparity in liver cancer incidence and chronic liver disease mortality by nativity in Hispanics: the multiethnic cohort. Cancer. 2016;122:1444–1452. doi: 10.1002/cncr.29922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Michikawa T, Inoue M, Sawada N, et al. Development of a prediction model for 10-year risk of hepatocellular carcinoma in middle-aged Japanese: the Japan Public Health Center-based Prospective Study Cohort II. Prev Med. 2012;55:137–143. doi: 10.1016/j.ypmed.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 28.Chen CJ, Wang LY, Lu SN, et al. Elevated aflatoxin exposure and increased risk of hepatocellular carcinoma. Hepatology. 1996;24:38–42. doi: 10.1002/hep.510240108. [DOI] [PubMed] [Google Scholar]
- 29.Ohishi W, Fujiwara S, Cologne JB, et al. Risk factors for hepatocellular carcinoma in a Japanese population: a nested case-control study. Cancer Epidemiol Biomarkers Prev. 2008;17:846–854. doi: 10.1158/1055-9965.EPI-07-2806. [DOI] [PubMed] [Google Scholar]
- 30.Koh WP, Robien K, Wang R, Govindarajan S, Yuan JM, Yu MC. Smoking as an independent risk factor for hepatocellular carcinoma: the Singapore Chinese Health Study. Br J Cancer. 2011;105:1430–1435. doi: 10.1038/bjc.2011.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trichopoulos D, Bamia C, Lagiou P, et al. Hepatocellular carcinoma risk factors and disease burden in a European cohort: a nested case-control study. J Natl Cancer Inst. 2011;103:1686–1695. doi: 10.1093/jnci/djr395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yuan JM, Govindarajan S, Arakawa K, Yu MC. Synergism of alcohol, diabetes, and viral hepatitis on the risk of hepatocellular carcinoma in blacks and whites in the U.S. Cancer. 2004;101:1009–1017. doi: 10.1002/cncr.20427. [DOI] [PubMed] [Google Scholar]
- 33.Loftfield E, Freedman ND, Lai GY, et al. Higher glucose and insulin levels are associated with risk of liver cancer and chronic liver disease mortality among men without a history of diabetes. Cancer Prev Res (Phila) 2016;9:866–874. doi: 10.1158/1940-6207.CAPR-16-0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yi SW, Choi JS, Yi JJ, Lee YH, Han KJ. Risk factors for hepatocellular carcinoma by age, sex, and liver disorder status: a prospective cohort study in Korea. Cancer. 2018;124:2748–2757. doi: 10.1002/cncr.31406. [DOI] [PubMed] [Google Scholar]
- 35.Kim MK, Ko MJ, Han JT. Alcohol consumption and mortality from all-cause and cancers among 1.34 million Koreans: the results from the Korea national health insurance corporation's health examinee cohort in 2000. Cancer Causes Control. 2010;21:2295–2302. doi: 10.1007/s10552-010-9656-9. [DOI] [PubMed] [Google Scholar]
- 36.Yi SW, Sull JW, Linton JA, Nam CM, Ohrr H. Alcohol consumption and digestive cancer mortality in Koreans: the Kangwha Cohort Study. J Epidemiol. 2010;20:204–211. doi: 10.2188/jea.JE20090077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang L, Zhou M, Sherliker P, et al. Alcohol drinking and overall and cause-specific mortality in China: nationally representative prospective study of 220,000 men with 15 years of follow-up. Int J Epidemiol. 2012;41:1101–1113. doi: 10.1093/ije/dys075. [DOI] [PubMed] [Google Scholar]
- 38.Jee SH, Ohrr H, Sull JW, Samet JM. Cigarette smoking, alcohol drinking, hepatitis B, and risk for hepatocellular carcinoma in Korea. J Natl Cancer Inst. 2004;96:1851–1856. doi: 10.1093/jnci/djh334. [DOI] [PubMed] [Google Scholar]
- 39.Joshi S, Song YM, Kim TH, Cho SI. Socio-economic status and the risk of liver cancer mortality: a prospective study in Korean men. Public Health. 2008;122:1144–1151. doi: 10.1016/j.puhe.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 40.Jung EJ, Shin A, Park SK, et al. Alcohol consumption and mortality in the Korean Multi-Center Cancer Cohort Study. J Prev Med Public Health. 2012;45:301–308. doi: 10.3961/jpmph.2012.45.5.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kono S, Ikeda M, Tokudome S, Nishizumi M, Kuratsune M. Alcohol and mortality: a cohort study of male Japanese physicians. Int J Epidemiol. 1986;15:527–532. doi: 10.1093/ije/15.4.527. [DOI] [PubMed] [Google Scholar]
- 42.Park SM, Lim MK, Shin SA, Yun YH. Impact of prediagnosis smoking, alcohol, obesity, and insulin resistance on survival in male cancer patients: National Health Insurance Corporation Study. J Clin Oncol. 2006;24:5017–5024. doi: 10.1200/JCO.2006.07.0243. [DOI] [PubMed] [Google Scholar]
- 43.Shih WL, Chang HC, Liaw YF, et al. Influences of tobacco and alcohol use on hepatocellular carcinoma survival. Int J Cancer. 2012;131:2612–2621. doi: 10.1002/ijc.27508. [DOI] [PubMed] [Google Scholar]
- 44.Yi SW, Hong JS, Yi JJ, Ohrr H. Impact of alcohol consumption and body mass index on mortality from nonneoplastic liver diseases, upper aerodigestive tract cancers, and alcohol use disorders in Korean older middle-aged men: prospective cohort study. Medicine (Baltimore) 2016;95:e4876. doi: 10.1097/MD.0000000000004876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Younoszai Z, Li Z, Stepanova M, Erario M, Cable R, Younossi ZM. Statin use is not associated with liver related mortality. Ann Hepatol. 2014;13:84–90. doi: 10.1016/S1665-2681(19)30908-1. [DOI] [PubMed] [Google Scholar]
- 46.Fuchs CS, Stampfer MJ, Colditz GA, et al. Alcohol consumption and mortality among women. N Engl J Med. 1995;332:1245–1250. doi: 10.1056/NEJM199505113321901. [DOI] [PubMed] [Google Scholar]
- 47.Marugame T, Yamamoto S, Yoshimi I, et al. Patterns of alcohol drinking and all-cause mortality: results from a large-scale population-based cohort study in Japan. Am J Epidemiol. 2007;165:1039–1046. doi: 10.1093/aje/kwk112. [DOI] [PubMed] [Google Scholar]
- 48.Ferrari P, Licaj I, Muller DC, et al. Lifetime alcohol use and overall and cause-specific mortality in the European Prospective Investigation into Cancer and nutrition (EPIC) study. BMJ Open. 2014;4:e005245. doi: 10.1136/bmjopen-2014-005245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saito E, Inoue M, Sawada N, et al. Impact of alcohol intake and drinking patterns on mortality from all causes and major causes of death in a Japanese population. J Epidemiol. 2018;28:140–148. doi: 10.2188/jea.JE20160200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chuang SC, Lee YC, Wu GJ, Straif K, Hashibe M. Alcohol consumption and liver cancer risk: a meta-analysis. Cancer Causes Control. 2015;26:1205–1231. doi: 10.1007/s10552-015-0615-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.