Dear Editor,
Continuous positive airways pressure (CPAP) treatment was used increasingly in the UK and elsewhere for coronavirus disease 2019 (COVID-19) to avoid the need for mechanical ventilation [1–3]. Early identification of patients benefitting from CPAP would assist decision making however we found that intensive care unit (ICU) admission respiratory parameters (rate, PaO2/FiO2 ratio) were poorly discriminatory. Using electronic healthcare records we retrospectively studied COVID-19 patients admitted to the University College London Hospital ICU between 8 March and 5 June 2020 in moderate-to-severe respiratory failure who received initial management with CPAP to see whether better prognosticators could be identified.
Comparison of demographic, clinical and biochemical parameters measured on ICU admission was made between patients adjudged CPAP success (hospital survival with CPAP alone) or failure (either death where CPAP was a ceiling of treatment, or need for mechanical ventilation regardless of hospital outcome). Requirement for other organ support was also compared. Patients managed on CPAP in non-ICU wards were excluded as detailed clinical and lab data were often lacking.
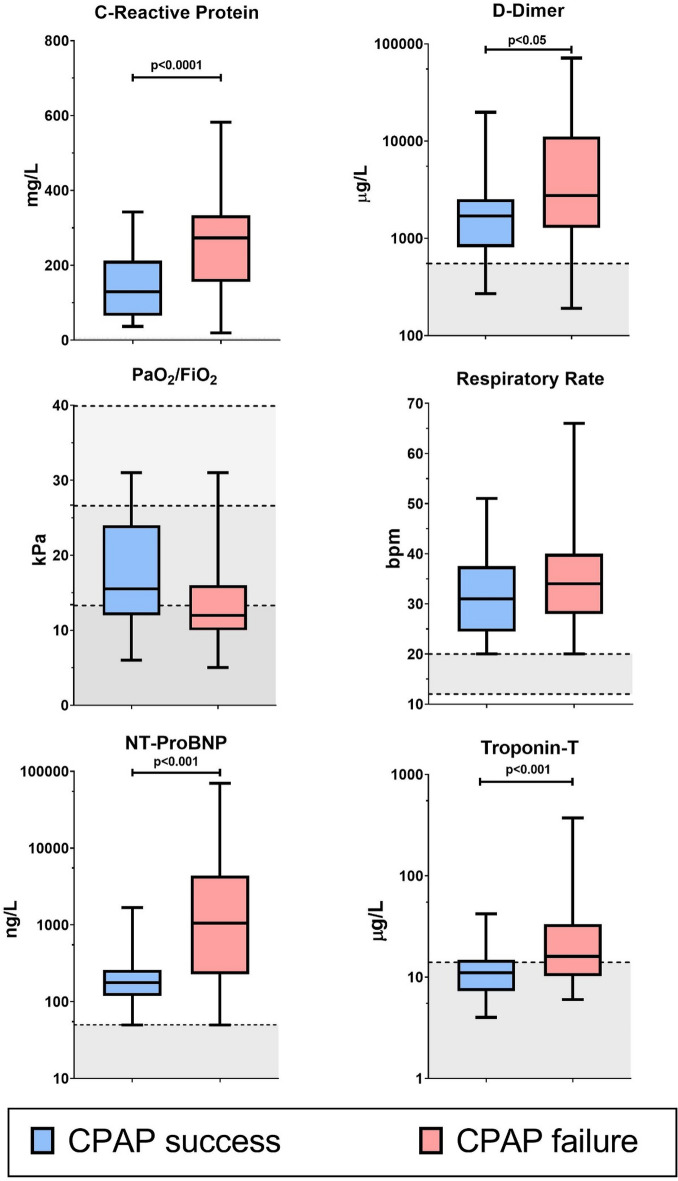
Of 108 within-hospital admissions, 93 (86%) received CPAP as initial respiratory failure management (median[IQR] PaO2/FiO2 ratio 13 [10–18] kPa) (Supplementary Fig. 1). Thirty-two (34%) were adjudged CPAP successes and 61 (66%) failures (14 deaths (23%) with CPAP as the ceiling of treatment, 47 (77%) requiring invasive ventilation of whom 26 died). Demographics and ICU admission values of respiratory rate, inspired oxygen concentration (FiO2) and PaO2/FiO2 ratio were similar between groups (Supplementary data). Admission values of C-reactive protein (CRP) (p < 0.0001), N Terminal-pro-B-type natriuretic peptide (NT-proBNP) (p < 0.001), troponin-T (p < 0.001) and d-dimers (p < 0.05) were significantly higher in CPAP failure patients (Fig. 1). Other organ support was only required for CPAP failure patients receiving invasive ventilation (46 vasopressors, 28 renal replacement therapy), but none for CPAP successes. At 6 h post-CPAP the PaO2/FiO2 ratio rose by 76.7% (37.9 to 99.8%) in CPAP success patients but only by 38.1% (−24.4 to 100.5) in the failure group (p = 0.015).
Fig. 1.
Biomarkers and variables recorded on ICU admission in patients receiving CPAP. Shaded area denotes normal range. The normal range for C-Reactive Protein (≤ 5 mg/L) is not indicated, FiO2 fraction of inspired oxygen concentration; PaO2/FiO2 ratio of arterial partial pressure to the fraction of inspired oxygen concentration. Shaded area denotes normal range except for PaO2/FiO2 where the increasing shades of grey denotes mild, moderate and severe respiratory failure according to the Berlin definition, NT-proBNP N terminal-pro B-type natriuretic peptide
For outcome prediction (CPAP failure), sixteen potential predictor physiological or biochemical variables were assessed. Details are provided in the Supplementary Index. In brief, separate univariable logistic regression models were fitted for each predictor, with p values < 0.05 determining variables entered into a multivariable logistic regression model. A model combining elevated CRP and NT-proBNP predicted CPAP failure with a sensitivity of 0.75 (95% CI 0.62–0.86), specificity of 0.83 (0.61–0.95), positive predictive value of 0.91 (0.78–0.97) and negative predictive value of 0.59 (0.41–0.76).
Failure of CPAP to avert death or invasive mechanical ventilation was associated with increased blood levels of thrombo-inflammatory and cardiac injury/dysfunction biomarkers on ICU admission. This may reflect an increased incidence of pulmonary thrombi either identifiable on imaging or multiple microthrombi, with subsequent right heart strain. The much-increased requirement for vasopressor and renal support in invasively ventilated patients reflects disease severity, but a significant iatrogenic contribution from high airway pressures, heavy sedation and hypovolaemia cannot be excluded. The high positive predictive value using elevated CRP and NT-proBNP may identify patients likely to fail CPAP. If validated, this could be gainfully used in management pathways and to stratify patients for intervention studies.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The UCL Critical Care COVID-19 Research Group members involved in this research comprised: Petra Voegele: Intensive Care Unit, University College London Hospitals NHS Foundation Trust, London UK; Nishkantha Arulkumaran: Intensive Care Unit, University College London Hospitals NHS Foundation Trust, London UK, Bloomsbury Institute of Intensive Care Medicine, Division of Medicine, University College London, London, UK; David Brealey: Intensive Care Unit, University College London Hospitals NHS Foundation Trust, London UK, Bloomsbury Institute of Intensive Care Medicine, Division of Medicine, University College London, London, UK, NIHR UCLH/UCL Biomedical Research Centre, London, UK; Mervyn Singer: Intensive Care Unit, University College London Hospitals NHS Foundation Trust, London UK, Bloomsbury Institute of Intensive Care Medicine, Division of Medicine, University College London, London, UK.
Funding
GA and DB received funding from the NIHR UCLH/UCL Biomedical Research Centre.
Compliance with ethical standards
Conflicts of interest
M Singer and D Brealey were involved in the development of the UCL Ventura CPAP device funded by the UK Department of Health and Social Care.
Ethical approval
Approval received from the London-Westminster Research Ethics Committee (REC ref 20/HRA/2505, IRAS ID 284088) and the Health Research Authority on 2nd July 2020.
Footnotes
The members of the UCL Critical Care COVID-19 Research Group are listed in Acknowledgements.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
on behalf of the UCL Critical Care COVID-19 Research Group:
Petra Voegele, Nishkantha Arulkumaran, David Brealey, and Mervyn Singer
References
- 1.Sun Q, Qui H, Huang M, Yang Y. Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu Province. Ann Intensive Care. 2020;10:33. doi: 10.1186/s13613-020-00650-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Radovanovic D, Rizzi M, Pini S, Saad M, Chiumello DA, Santus P. Helmet CPAP to treat acute hypoxemic respiratory failure in patients with COVID-19: a management strategy proposal. J Clin Med. 2020;22:1191. doi: 10.3390/jcm9041191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doidge JC, Mouncey PR, Thomas K, Gould DW, Ferrando-Vivas P, Shankar-Hari M, Harrison DA, Rowan KM. Trends in intensive care for patients with COVID-19 in England, Wales and Northern Ireland. Preprints doi:10.20944/preprints202008.0267.v1 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.