Abstract
Background
Dental hygiene is a physically demanding profession that places dental hygienists at risk of musculoskeletal disorders (MSDs). Study objectives were to establish the patterns and frequencies of self-reported occupation-related MSDs among dental hygienists in Canada and determine what MSD prevention training is provided in the curricula of accredited dental hygiene schools in Canada.
Methods
An online, quantitative cross-sectional survey was distributed to registered dental hygienists in Canada to assess prevalence and types of occupational MSDs. Additionally, a phone/email qualitative structured interview was conducted with 8 accredited English-speaking dental hygiene schools across Canada.
Results
Of all respondents (N = 647), 83% (n = 534) reported a work-related MSD. The most common disorders were carpal tunnel syndrome and tendonitis. There was a positive correlation between number of years in practice and the incidence of MSDs. Half of the respondents felt they had received adequate training on injury prevention. Most schools interviewed felt their injury prevention training was adequate.
Discussion
Despite the majority of dental hygiene programs in Canada feeling they provide adequate training for injury prevention, an alarmingly high prevalence of occupation-related MSDs was found among dental hygienists in Canada. This finding is concerning given that 61% (n = 396) of respondents had practised for less than 10 years.
Conclusion
The high prevalence of MSDs among dental hygienists in Canada indicates the need for further exploration of ergonomics in the work environment and possible individual predisposing factors for MSDs. Additionally, dental hygiene programs should conduct an in-depth examination of their curricula as it relates to ergonomics and injury prevention.
Keywords: Canada, curriculum, dental hygiene, injury, musculoskeletal disorder, occupational health
Abstract
Contexte
La profession d’hygiéniste dentaire est exigeante sur le plan physique et met à risque les hygiénistes dentaires de troubles musculosquelettiques (TMS). Les objectifs de l’étude étaient d’établir les profils et la fréquence autodéclarés des TMS liés à la profession par les hygiénistes dentaires au Canada et de préciser la formation en matière de la prévention des TMS qui est fournie dans les programmes d’hygiène dentaire d’écoles agréées au Canada.
Méthodologie
Un sondage quantitatif et en coupe transversale mené en ligne a été distribué à des hygiénistes dentaires autorisés au Canada pour évaluer la prévalence et les types de TMS professionnels. De plus, une entrevue qualitative et structurée a été menée par téléphone ou par courriel auprès de 8 écoles d’hygiène dentaire de langue anglaise partout au Canada. Résultats : Parmi tous les répondants (N = 647), 83 % (n = 534) ont signalé un TMS lié au travail. Les troubles les plus communs étaient le syndrome du canal carpien et la tendinite. Il y avait une corrélation positive entre le nombre d’années de pratique et l’incidence des TMS. La moitié des répondants étaient d’avis qu’ils avaient reçu une formation adéquate sur la prévention des blessures. La plupart des écoles interrogées estimaient que leur formation sur la prévention des blessures était adéquate.
Discussion
Malgré que la majorité des programmes d’hygiène dentaire au Canada étaient d’avis qu’ils fournissaient une formation adéquate sur la prévention des blessures, une prévalence très élevée et inquiétante de TMS liés à la profession a été trouvée chez les hygiénistes dentaires au Canada. Cette constatation est inquiétante étant donné que 61 % (n = 396) des répondants avaient exercé l’hygiène dentaire pendant moins de 10 ans.
Conclusion
La prévalence élevée de TMS chez les hygiénistes dentaires au Canada démontre le besoin d’explorer davantage l’ergonomie dans l’environnement de travail et les facteurs de prédisposition individuels possibles de TMS. De plus, les programmes d’hygiène dentaire devraient effectuer un examen approfondi du programme par rapport à l’ergonomie et à la prévention des blessures.
PRACTICAL IMPLICATIONS OF THIS RESEARCH .
Practitioners who are more aware of their musculoskeletal health may choose to alter their daily work schedule or break time(s) and seek out other health professionals to help prevent MSDs.
Dental hygiene faculty and program directors may wish to collaborate with other health professions to improve the musculoskeletal health of their students.
Educational institutions may decide to provide more in-depth courses on musculoskeletal health and injury prevention techniques.
INTRODUCTION
Dental professionals face a number of occupational health issues including physical, biological, chemical, and psychosocial hazards, 1 as well as ergonomic hazards which can lead to musculoskeletal disorders (MSDs). 2 MSDs are injuries affecting movement of the musculoskeletal system, which includes muscles, tendons, ligaments, nerves, discs, and blood vessels. 3, 4 Wide-ranging research has recognized MSDs in the dental profession as a significant occupational health issue. 4 These disorders are often caused by awkward postures, standing or sitting for long periods of time with infrequent breaks, prolonged repetitive and/or forceful movements, improper design of the dental chair and magnification tools, poor lighting, stress, and genetics. 3,4,5 In addition, productivity demands and psychosocial considerations may aggravate these risks. 5 A 2009 systematic review found the prevalence of general musculoskeletal pain in dental professionals ranged from 64% to 93%, representing a significant proportion of the workforce. 3 Compared to other dental professionals, dental hygienists have been recognized as having unique occupational health concerns, in part due to performing repetitive fine-tuned actions, which seems to place them at higher risk of MSDs. Studies of dental hygienists have found prevalence rates of MSD-related pain as high as 96%. 4
Symptoms of MSDs include discomfort, aching, numbness, tingling, burning, stiffness, and fatigue. Signs of MSDs include decreased range of motion and grip strength, loss of normal sensation, movement, and coordination. 6 Pain from MSDs can occur in the neck, shoulder, arm, wrist, hands, upper and lower back, hips, knees, and feet. 3 Back pain in particular has been found to be a major health problem for dental professionals. 3 Carpal tunnel syndrome (CTS) is one of the most common MSDs in dental hygienists causing numbness, tingling, and pain in the hand and wrist. 7 A 2001 study conducted in the United States found that 75.1% of 177 dental hygienists in US army dental offices reported having hand problems, with 56.5% experiencing probable CTS symptoms. 7 Compared to dentists, dental hygienists are at a greater risk of developing an MSD in the upper extremities and lower back due to scaling and root planing over long hours. 8 Additionally, dental hygienists have a higher prevalence of MSDs in the wrists and hands compared to dentists. 1,9 Other specific MSDs affecting dental hygienists include tension neck syndrome, thoracic outlet compression syndrome, pronator syndrome, tendonitis, lateral epicondylitis, trigger thumb, De Quervain’s tenosynovitis, carpometacarpal osteoarthritis, and vibration-induced neuropathy. 4
MSDs contribute to sick leave and reduced productivity. 3,10 Symptoms can vary from mild and recurring to severe and career ending. 3 Some dental hygienists will continue to work in pain due to financial constraints but must decrease their number of workdays. MSDs, long working hours, and working without an assistant are causes of work-related stress and burnout. 10
Symptoms of MSDs seem to begin very early in careers, with a high prevalence occurring in students during training as clinical hours increase. 5 A study among Australian dental hygiene students found neck pain was reported most often, followed by shoulder, wrist/hand, and lower back pain. Clinical hours and computer usage among students were identified as risk factors for shoulder and upper back pain. 11 With many dental offices transitioning to digital and computerized systems, this may be an added MSD risk factor for practising hygienists.
It is widely suggested that risk factors for MSDs can be reduced with proper ergonomics.5 The goal of ergonomics is to find the best fit between workers and their work space. 5 In dentistry, recommendations for proper ergonomics include using adjustable and supportive seating, proper positioning of the clinician and client, proper lighting, indirect mirror viewing, magnification (using loupes), using ergonomic instruments, and taking regular rest breaks with exercise/stretching during breaks. 5 Exercise during leisure time can also prevent injury, promote health, and increase the longevity of dental hygienists’ careers. 5,12 A recent study conducted at the University of Manitoba found that physical health in dental hygiene students improved with participation in functional fitness classes. 13
Education on musculoskeletal health and injury prevention may be beneficial in reducing the number of dental hygienists who suffer from an MSD. However, many dental hygienists report that their educational training did not prepare them for the physical demands they face when working full time.10
Research is lacking on occupational injuries among dental hygienists in Canada and there is little information on the MSD prevention curricula in Canadian dental hygiene schools. 14 The objectives of this study were to establish the patterns and frequencies of self-reported occupation-related MSDs among dental hygienists in Canada and to determine what MSD prevention training is provided in the curricula of accredited dental hygiene schools in Canada. The purpose of this research is to identify the gaps in training and prevention of MSDs to offer strategies and suggestions for improving dental hygiene training.
METHODS
Ethics approval
The study was approved by the Dalhousie University Faculty of Dentistry Unit Level Ethics Review (REB file # DENTUNIT2018-04).
There were 2 components to this study: a quantitative cross-sectional survey of dental hygienists in Canada and a qualitative structured interview of academics in Canadian schools of dental hygiene.
Survey of dental hygienists
The study population for the survey included all practising or non-practising registered dental hygienists in Canada. Students, non-registered dental hygienists, and respondents who did not answer any questions were excluded from this survey. There were 29,246 registered dental hygienists in Canada at the time this survey took place. A sample size calculation resulted in a target sample of 379 respondents to achieve a maximum margin of error of 5% with a 95% confidence level. The Canadian Dental Hygienists Association (CDHA) distributed the survey invitation via its social media platforms (Facebook and Twitter). The survey was conducted online using Opinio TM Software. There were 13 multiple-choice questions and 2 open-ended questions. Topics included demographics, employment history, history of occupational MSDs, treatment and prevention of injuries, and MSD prevention education. The data were downloaded from Opinio TM and analysed using SPSS Statistics. Descriptive statistics were used to summarize the data. Number of injuries reported by right- and left-handed respondents were compared using an independent t-test. A Pearson correlation analysis between the number of years in practice and the number of injuries was conducted.
Interviews with dental hygiene schools
The study population for the interview component comprised the 27 English-speaking accredited Diploma and/or Bachelor of Dental Hygiene programs in Canada. Directors and professors of these programs were contacted by email and telephone. Responses were received from 8 schools, which led to saturation. Through initial contact, an individual knowledgeable about the program’s injury prevention training curriculum was identified to answer the interview questions. The interview consisted of 3 questions (with prompts) on injury prevention curriculum: 1) What curriculum does your institution offer on occupational injury prevention and musculoskeletal injury prevention in particular? 2) To what extent do you think your students are knowledgeable about the risk and prepared to prevent musculoskeletal injury in their profession upon graduation? 3) Do you feel your school offers enough education on proper ergonomics to prevent musculoskeletal occupational injuries?
Interviews were conducted either by telephone or email. If the interview was over the telephone, a digital recorder was used to collect data. Interview data were summarized using thematic analysis.
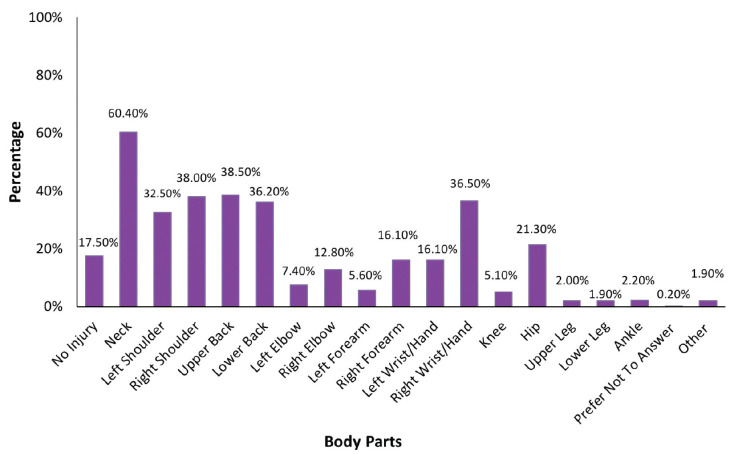
Figure 1.
Location(s) of musculoskeletal injury(ies) experienced by dental hygienists (N = 647) as a result of their occupation
RESULTS
Survey of dental hygienists
There were 656 responses to the online survey; however, 9 respondents were removed because they did not complete the survey or did not meet the inclusion criteria. Assuming all registered dental hygienists had access to the survey, the response rate was 2.24%. The maximum margin of error achieved was 3.81% with a 95% confidence level.
The majority of survey respondents identified as female (98.8%, n = 639); approximately 90% (n = 584) were right-handed. Years in practice ranged from 1 to 21, with approximately 61% (n = 396) of the respondents working for 10 years or less. About 60% (n = 394) of respondents worked full time (more than 32 hours per week) and over 95% (n = 622) were working within a general dental practice. Approximately 30% (n = 194) of respondents worked part time (8 to 31 hours per week); less than 10% of the participants indicated that they were retired (n = 4), off work due to an MSD (n = 14), unemployed (n = 3) or other (n = 30).
Respondents were asked to indicate the location(s) of any musculoskeletal injury(ies) they had experienced as a result of their occupation (Figure 1). In all, 83% (n = 534) of respondents indicated that they had suffered an MSD related to their occupation. The most common regions of pain reported were neck (60.4%, n = 391), followed by upper back (38.5%, n = 249), right shoulder (38%, n = 246), right wrist/hand (36.5%, n = 237), and lower back (36.2%, n = 234).
There was no significant difference in the mean number of locations injured reported by right- and left-handed respondents (mean ±SD: 3.36 ±2.66 versus 3.37 ±2.74; t = –0.021; df = 634, p = 0.984). There was a positive correlation between years in practice and the number of locations injured (r = 0.238; p < 0.001), with the number of locations injured increasing as years in practice increased.
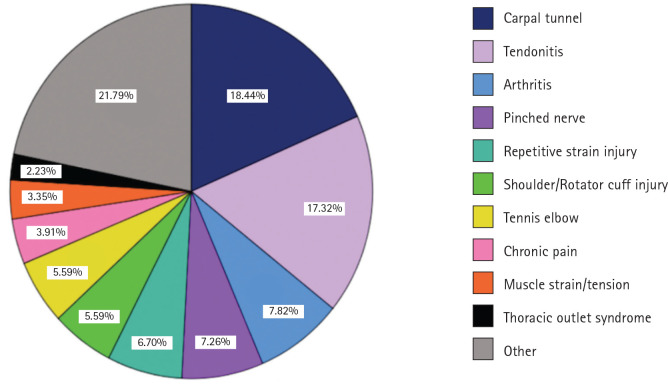
Those respondents who indicated they had received a medical diagnosis (n = 184) were asked to specify what their diagnosis was as a free-text response. A thematic analysis of these responses identified 10 common groups of diagnoses. Diagnoses that did not fit within the groups were classified as “other.” The 2 most common diagnoses were CTS (18.4%, n = 119) and tendonitis (17.3%, n = 112) (Figure 2).
When respondents were asked about what measures they used to prevent MSDs, the 3 most common responses were daily stretching (69%, n = 448), use of magnification loupes (49%, n = 320), and yoga (37%, n = 242). Those who reported seeking treatment for their MSDs (n = 505) most often sought treatment from massage therapists (67%, n = 436), chiropractors (49%, n = 319), and physiotherapists (39%, n = 254).
Respondents were asked whether or not they felt they were properly educated on preventing MSDs during their dental hygiene training. Fifty percent (n = 323) responded yes, 43% (n = 279) responded no, and the remaining 7% (n = 45) preferred not to answer. Respondents were also asked if they had taken any continuing education courses on ergonomics and injury prevention; the responses were fairly even with 50% (n = 321) saying yes, 47% (n = 304) saying no, and the remaining 3% (n = 22) preferring not to answer.
Interviews with dental hygiene schools
Interviews were conducted with representatives from 8 accredited dental hygiene schools in Canada. Respondents were dental hygiene faculty and included full-time associate professors (n = 5) and program directors (n = 3). Most respondents felt their stu,dents are very knowledgeable about the risk of MSDs, although some remarked that their students do not think they will incur an MSD. When asked if they thought their school offers enough education on proper ergonomics to prevent MSDs, 37.5% (n = 3) said their school could offer more education, while 62.5% (n = 5) said their school offers enough. Some representative comments follow:
We’ve had mandatory loupes program for about 10–12 years now, which I think helps the students work ergonomically.
I think we do a good job of educating our students about musculoskeletal injury prevention; the information is there and so is the follow through in both theory and lab courses.
Our students are extremely knowledgeable with regard on how to prevent musculoskeletal injuries as they are not only examined on this information, but are assessed every clinical session over the 2-year clinical courses of our program[…] The students must also self-evaluate their ergonomics as well as the other criteria for each clinical assessment.
Respondents were asked what injury prevention measures are currently included in their curricula. Themes included the importance of proper ergonomics for injury prevention; observation of students in clinic during client treatment to ensure proper ergonomics; stretching techniques and exercises to strengthen muscles; loupes program; and collaborations with occupational therapy students.
Figure 2.
Medical diagnoses of musculoskeletal injuries experienced by dental hygienists (n = 184) as a result of their occupation
Both the interview and the survey asked respondents to suggest ways to improve the injury prevention curriculum in dental hygiene training. Because the suggestions were similar from both the surveyed dental hygienists and the interviewed faculty, they were combined for thematic analysis (Table 1). The themes include providing education on specific types of injuries and ways to prevent them; a focus on physical activity (stretching, core exercises, and yoga); providing ergonomic tools such as magnification loupes; and providing a dedicated course on ergonomics. Some representative comments follow:
Taking a course on the probability of work-related injuries and learning ways to prevent them. Teaching the importance of all hygienists using loupes.
(Dental hygienist)
Bring in hygienists who have had to stop working for various musculoskeletal issues for a round table discussion with students. It would also help to have faculty from other disciplines come in to discuss their unique viewpoints (chiro, physio, kinesiology, surgeons, massage). I believe that hearing from peers and surgeons would likely have the biggest impact.
(Dental hygienist)
More focus on physical activity and the importance of staying fit and strength exercises throughout the day. I remember in college; it was a very short time spent on possible injury and it was not taught as if it was a very serious issue. Prevention is key.
(Dental hygienist)
1. More information on health and wellness with regards to maintaining core strength. 2. Interdisciplinary opportunities with massage therapy programs. 3. Interdisciplinary opportunities with occupational therapists and physiotherapists.”
(Faculty member)
DISCUSSION
This study found a high prevalence of MSDs among Canadian dental hygienists, with 83% reporting an MSD related to their dental hygiene career. This rate falls within the ranges reported by previous studies of dental hygienists’ MSDs in other countries. 4,15
The neck and upper back were the most commonly reported areas of pain followed by shoulder and wrist/hand. This is consistent with a 2010 review of the literature on MSDs in dental hygienists and a 2013 Australian study that found high prevalence of MSDs in these areas. 4,9 It is important that dental hygienists be educated on correct posture and back care, including the use of equipment to support ideal posture in order to reduce or eliminate pain. 9,16
Table 1.
Recommendations for improving dental hygiene curriculum to prevent MSDs
|
Themes |
Subthemes/Recommendations |
Recommended by |
|
Education/prevention techniques for all types of MSDs |
Emphasis on ergonomics |
Faculty, dental hygienists |
|
|
Demonstrate ways to position oneself and client for when the supine position is contraindicated |
Dental hygienists |
|
Focus on physical activity |
Self-care (yoga, meditation) |
Faculty, dental hygienists |
|
|
Preventive exercises, stretching, core strength |
Faculty, dental hygienists |
|
Injury prevention items |
Mandatory loupes |
Dental hygienists |
|
|
Ergonomic chairs/workstations |
Dental hygienists |
|
|
Teach left-handed students to adapt to right-handed workstations |
Dental hygienists |
|
|
Improve instructor calibration to assess ergonomics |
Faculty |
|
Dedicated ergonomics course |
Education on all types of injuries and ways to prevent them |
Faculty, dental hygienists |
|
|
Collaboration with other health professionals (OT, PT, MT, chiropractor, other)a |
Faculty, dental hygienists |
|
|
Class discussion with dental hygienists who have experienced an MSD; show rate of injury statistics |
Dental hygienists |
|
|
Fitness component |
Dental hygienists |
|
|
Students self- and/or peer ergonomic assessment |
Faculty |
|
Post-graduation |
Follow up with students after graduation |
Faculty |
aOT: occupational therapy; PT: physiotherapy; MT: massage therapy
Long working periods and the greater amount of clients treated per day or per week may be associated with an increased risk of developing CTS. 17,18 CTS can make practising as a dental hygienist difficult and can result in the need for extensive treatment with a therapist, over-the-counter pain medication, a decrease in working hours, bracing or splinting, or even surgery. 19
This study found a positive correlation between number of injured locations and years in practice. Previous studies have found years in practice to be correlated and/or predictive of CTS and shoulder pain. 4,7,14 Although this current survey did not include questions pertaining to the difficulty of debridement of clients treated by the dental hygienists, Lalumandier and McPhee found that treating clients with heavy calculus and working for over 10 years doubled the risk for developing a hand-related MSD or CTS. 7
In terms of prevention, a 2014 study conducted in North America found 50% of dental hygienists stretch throughout the day to alleviate discomfort. 20 The present survey found a higher rate (69%) of respondents reporting stretching throughout the day. It is encouraging to see that many dental hygienists are stretching regularly. A significant proportion (37%) of respondents also reported practising yoga regularly. About half of respondents (49%) reported using magnification loupes.
Despite the high prevalence of MSDs found in this study, half of the respondents (50%) surveyed believed they were properly educated on prevention of MSDs and more than half the schools (62.5%) interviewed believed they were offering enough education on prevention of MSDs. Some schools have implemented injury prevention curricula, such as a mandatory loupes program, a focus on fitness, and student self- and/or peer ergonomics assessments. It has been shown that ergonomics improved when dental hygiene students self-assess using photographs. 21 Another interesting finding was that schools are collaborating with occupational therapists. Our results indicate, however, that occupational therapists are rarely sought out for treatment of MSD post-graduation. A study by Moodley and Van Wyk suggests that dental curriculum be redesigned to include a focus on occupational health with input from a multidisciplinary team. 22
Limitations
There are limitations to this study. One such limitation is the low response rate to the survey. However, the addition of a qualitative component adds rigour to the study. Our survey did not include questions about confounding variables that may have increased the likelihood of developing an MSD. It also did not include questions related to the severity of the MSD or how the injury affected their work. Our survey did not include dental hygienists who may not be registered and have left the profession due to MSDs. The prevalence of injury may have been overestimated as dental hygienists with a diagnosed MSD may have been more likely to participate in the survey as they are knowledgeable about the topic. Conversely, the prevalence of injury may have been underestimated as the survey was distributed via social media, which may have biased the sample to a younger demographic who tend to have fewer injuries. In addition, the survey and interviews were only offered in English. As a result, French-speaking schools were not represented, and French-speaking dental hygienists may not have participated in the survey.
CONCLUSION
This survey found an alarmingly high prevalence of MSDs among Canadian dental hygienists. This finding is particularly concerning given the relatively low number of years in practice of the respondents. Despite generally positive views on the current state of injury prevention training, these data suggest improvements are needed.
Recommendations for dental hygienists include entering into discussions with employers regarding scheduled length of time for client appointments, the need for multiple breaks throughout the day as opposed to one longer break, and the need for proper ergonomic equipment and workstations. Physical activity is also highly suggested as it has been proven to reduce the risk o,f MSDs. 12 Implementing an ergonomics and injury prevention course in all accredited dental hygiene schools may be beneficial for all future dental hygienists. The course could contain topics from the suggested improvements found in Table 1. It is recommended that the Commission on Dental Accreditation of Canada (CDAC) review its curriculum requirements and consider the provided suggestions.
Future research should explore why there is such a high prevalence of MSDs among dental hygienists to better understand the causes of MSDs. Controlled studies are needed to ascertain the effectiveness of ergonomic interventions in the dental practice setting as well as educational interventions in the training setting.
CONFLICT OF INTEREST
The authors declare no conflicts of interest
Acknowledgments
The authors acknowledge Dalhousie University Faculty of Dentistry for providing funding and the Canadian Dental Hygienists Association for distributing the survey through its social media platforms
Footnotes
CDHA Research Agenda category: capacity building of the profession
REFERENCES
- 1. Moodley R, Naidoo S, Wyk JV. The prevalence of health-related problems in dentistry: A review of the literature. J Occup Health 2018;60(2):111–25 [cited 2018 Sept 30] Available from: https://www ncbi nlm nih gov/pubmed/29213011/ doi: 10 1539/joh 17-0188-RA [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ontario Ministry of Labour. Section 8: Occupational Illness: Occupation Health and Safety Guidelines for Farming in Ontario. Ontario: Government of Ontario; 2016 Apr 12 [cited 2018 Oct 11]. Available from: https://www.labour.gov.on.ca/english/hs/pubs/farming/gl_illness.php
- 3. Hayes MJ, Cockrell D, Smith DR. A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hyg 2009;7(3):159–65 [cited 2018 Oct 11] Available from: https://pubmed ncbi nlm nih gov/19659711/ doi: 10 1111/j 1601-5037 2009 00395 x [DOI] [PubMed] [Google Scholar]
- 4. Hayes MJ, Smith DR, Cockrell D. An international review of musculoskeletal disorders in the dental hygiene profession. IntDentJ 2010Dec;60(5):343–52 [cited 2018 October1] Available from: https://onlinelibrarywileycom/doi/epdf/101922/IDJ_2514Hayes10 [PubMed] [Google Scholar]
- 5. Gupta A, Ankola AV, Hebbal M. Dental ergonomics to combat musculoskeletal disorders: A review. Int J Occup Saf Ergon 2013;19(4):561–71 [cited 2018 October 1] Available from: https://www tandfonline com/doi/pdf/10 1080/10803548 2013 11077005?need Access=true doi: 10 1080/10803548 2013 11077005 [DOI] [PubMed] [Google Scholar]
- 6. Jodalli PS, Kurana S, Ragher M, Khed J, Prabhu V. Posturedontics: How does dentistry fit you? J Pharm Bioallied Sci. 2015;7(2):S393–S397 [cited 2018 Sept 30]. Available from: doi: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4606627/ doi: 10.4103/0975-7406.163463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lalumandier J, McPhee S. Prevalence and risk factors of hand problems and carpal tunnel syndrome among dental hygienists. J Dent Hyg 2001;75(2):130–34 [cited 2018 Oct 13] Available from: [PubMed] [Google Scholar]
- 8. Noh H, Roh H. Approach of industrial physical therapy to assessment of the musculoskeletal system and ergonomic risk factors of the dental hygienist. J Phys Ther Sci 2013Jul;25(7):821–26 [cited 2020 Feb 3] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hayes MJ, Smith DR, Taylor JA. Musculoskeletal disorders and symptom severity among Australian dental hygienists. BMC Research Notes 2013;6(1):250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chismark A, Asher G, Stein M, Tavoc T, Curren A. Use of complementary and alternative medicine for work-related pain correlates with career satisfaction among dental hygienists. J Dent Hyg 2011 85(4):273–84 [cited 2018 Oct 2] Available from: http://web a ebscohost com ezproxy library dal ca/ehost/pdfviewer/pdfviewer?vid=2&sid=21efa816-7718-4f1d-afed-432615795a14%40sessionmgr4007 [PubMed] [Google Scholar]
- 11. Hayes MJ, Smith DR, Cockrell D. Prevalence and correlates of musculoskeletal disorder among Australian dental hygiene students. Int J Dent Hyg 2009August;7(3):176–81 [cited 2018 Oct 2] Available from: https://pubmed ncbi nlm nih gov/19659713/ [DOI] [PubMed] [Google Scholar]
- 12. Nguyen C, Callahan H, Smith E, Vu J. Exercise for the dental hygienist. Access 2015Nov;29(9):16–20 [cited 2018 Oct 2] Available from: http://web a ebscohost com ezproxy library dal ca/ehost/pdfviewer/pdfviewer?vid=5&sid=f1539aef-4bfc-4e44-9cbf-6cf938569cdb%40sdc-v-sessmgr04 [Google Scholar]
- 13. Parsons JL, MacDonald L, Caver M, Hoeppner M, Titteron A, Willsie J. Functional fitness for dental hygiene students: Does it make them fit to sit? Can J Dent Hyg 2019 Oct;53(3):149–156 [PMC free article] [PubMed] [Google Scholar]
- 14. Liss GM, Jesin E, Kusiak RA, White P. Musculoskeletal problems among Ontario dental hygienists. Am J Ind Med 1995;28:521–40 10 1002/ajim 4700280408 [DOI] [PubMed] [Google Scholar]
- 15. Barry RM, Spolarich AE, Weber M, Krause D, Woodall WD, Bailey JH. Impact of operator positioning on musculoskeletal disorders and work habits among Mississippi dental hygienists. J Dent Hyg 2017Dec;91(6):6–14 PubMed PMID:29378801 Available from: https://jdh adha org/content/91/6/6 [PubMed] [Google Scholar]
- 16. Ng A, Hayes MJ, Polster A. Musculoskeletal disorders and working posture among dental and oral health students. Healthcare 2016 Mar 4;4(1) [cited 2018 Oct 20] Available from: https://www ncbi nlm nih gov/pmc/articles/PMC4934547/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Haghighi AB, Khosropanah H, Vahidina F, Esmailzadeh S, Emami Z. Association of dental practice as a risk factor in the development of carpel tunnel syndrome. J Dent (Shiraz) 2013Mar;14(1):37–40 [cited 2020 Jan 26] Available from: [PMC free article] [PubMed] [Google Scholar]
- 18. Anton D, Rosecrance J, Merlino L, Cook T. Prevalence of musculoskeletal symptoms and carpal tunnel syndrome among dental hygienists. Am J Ind Med 2002 Sept;42(3):248–57 [cited 2020 Jan 26] Available from: https://onlinelibrary-wiley-com ezproxy library dal ca/doi/epdf/10 1002/ajim 10110 [DOI] [PubMed] [Google Scholar]
- 19.OrthoInfo (American Academy of Orthopedic Surgeons). Carpal Tunnel Syndrome [Internet]. 2019 [cited 2019 Apr 2]. Available from: https://orthoinfo.aaos.org/en/diseases--conditions/carpal-tunnel-syndrome/
- 20. Guignon AN, Purdy CM. 2012 Dental hygiene practice in North America – The physical, economic and workforce impact of musculoskeletal disorders among clinical dental hygienists. J Dent Hyg 2014 Oct;88(5) [Google Scholar]
- 21. Partido B. Dental hygiene student self-assessment of ergonomics utilizing photography. J Dent Educ 2017 Oct;81(10):1194–1202 [cited 2019 Mar 30] Available from: www jdentaled org/content/81/10/1194 long doi: 10 21815/JDE 017 077 [DOI] [PubMed] [Google Scholar]
- 22. Moodley R, Van Wyk J. Multidisciplinary perspectives to prevent occupational health-related conditions among dental practitioners. BDJ Open 2019;5(6) [cited 2020 Feb 3] Available from: https://www ncbi nlm nih gov/pmc/articles/PMC6459843/ [DOI] [PMC free article] [PubMed] [Google Scholar]