ABSTRACT
Background:
Cholangiocarcinoma is an aggressive neoplasm that usually requires palliative biliary drainage. Photodynamic therapy (PDT) has been described as a successful adjunct treatment to malignant biliary obstruction.
Aim:
To describe the use of digital cholangioscope to help provide laser light during biliary PDT session using locally developed light source.
Method:
Patient receives intravenous photosensitizer 24 h before the procedure. It starts with a regular duodenoscopy. After identification of the major papilla and retrograde cannulation, the digital cholangioscope is introduced into the common bile duct. Then, the cholangioscopic examination helps to identify the neoplastic stricture. Under direct visualization lighting catheter is advanced through the cholangioscope. Repositioning is recommended every centimeter to cover all strictured area. At the end of the procedure, a final cholangioscopy assesses the bile duct for the immediate result and adverse events.
Result:
This procedure was applied in one 82-year-old male due to obstructive jaundice in the last two months. EUS and ERCP revealed a severe dilation of the common bile duct associated with choledocholithiasis. Besides, was revealed dilation of hepatic duct up to a well-circumscribed hypoechoic solid mass measuring 1.8x2 cm compressing the common hepatic duct. The mass was deemed unresectable and the patient was referred for palliative treatment with PDT. He remained asymptomatic for three months. He perished due to complications 15 months after the PDT session.
Conclusion:
Digital cholangioscopy-guided biliary PDT is feasible and seems safe and effective as an adjunct modality in the palliation of extrahepatic cholangiocarcinoma.
HEADINGS: Endoscopy; Cholangiocarcinoma; Jaundice; Cholangiopancreatography, endoscopic retrograde
Graphical Abstract
Photodynamic therapy (PDT) of an extrahepatic cholangiocarcinoma using a digital cholangioscopy to deliver the laser.
RESUMO
Racional:
Colangiocarcinoma é neoplasia agressiva que geralmente exige drenagem biliar paliativa. A terapia fotodinâmica (TFD) tem sido descrita como tratamento adjunto bem-sucedido para tratar obstrução biliar maligna.
Objetivo:
Descrever o emprego do colangioscópio digital para ajudar a fornecer luz de laser durante sessão de TFD biliar usando fonte de luz desenvolvida localmente.
Método:
Paciente recebe fotossensibilizador intravenoso 24 h antes do procedimento que começa com duodenoscopia regular. Após a identificação da papila principal e da canulação retrógrada, o colangioscópio digital é introduzido no ducto biliar comum. Em seguida, o exame colangioscópico ajuda a identificar a estenose neoplásica. Sob visualização direta, o cateter de iluminação avança através do colangioscópio. Reposicionamento é feito a cada centímetro. Ao final colangioscopia avalia o ducto biliar quanto ao resultado imediato e a eventos adversos.
Resultado:
Este procedimento foi aplicado em um homem de 82 anos devido à icterícia obstrutiva nos últimos dois meses. EUS e CPRE revelaram dilatação grave do ducto biliar comum associada à coledocolitíase. Além disso, havia dilatação do ducto hepático até massa sólida hipoecóica bem circunscrita, medindo 1,8x2 cm, comprimindo o ducto hepático comum. Ela foi considerada irressecável e paciente encaminhado para tratamento paliativo com TFD que permaneceu assintomático por três meses. Morreu devido a complicações 15 meses após a sessão de TFD.
Conclusão:
A TFD biliar guiada por colangioscopia digital é viável e parece segura e eficaz como modalidade auxiliar na paliação de colangiocarcinoma extra-hepático.
DESCRITORES: Endoscopia, Colangiocarcinoma, Icterícia, CPRE
Graphical Abstract
Terapia fotodinâmica (TFD) de colangiocarcinoma extra-hepático utilizando colangioscopia digital para fornecer o laser.
DESCRITORES: Endoscopia, Colangiocarcinoma, Icterícia, CPRE
INTRODUCTION
The cholangiocarcinoma (CC) is a rare but aggressive neoplasm originating from the biliary epithelial cells 2 , 4 . Its treatment is complex and multidisciplinary 5 but surgical resection is still the only curative option. Unfortunately, most cases present with unresectable masses at diagnosis 4 , 6 , 14 .
The non-curative systemic treatment involves chemotherapy, plus radiation therapy in selected cases. Symptomatic relief is central as well, that is, optimized clinical support. The extrahepatic CC typically presents with obstructive jaundice 12 , rendering biliary drainage also necessary. Besides relieving symptoms and preventing cholangitis, drainage is also mandatory prior to the beginning of systemic chemotherapy 1 .
The endoscopic retrograde cholangiopancreatography (ERCP) is the preferred route for biliary drainage in the palliative setting 12 . It involves the removal of debris and biliary stent placement, using a self-expandable metallic stent. Local ablative methods such as radiofrequency and photodynamic therapy (PDT) may be also associated 16 .
The PDT is a neoplastic-specific laser-based modality that has been introduced as adjunctive therapy to biliary stenting. It requires a previous intravenous infusion of a photosensitizing agent that concentrates in neoplastic cells. During the PDT session, the tumor is exposed to a specific wavelength of light that interacts with the photosensitizer. Such interaction creates highly cytotoxic oxygen-free radicals thus leading to the destruction of tumor cells while sparing healthy ones 3 , 8 .
Recently, the single-operator cholangioscopy has been described in helping deliver light for biliary PDT. Some authors advocate it allows precise targeting, hypothetically improving outcomes 10 , 15 . However, those are scattered reports and most describe the use of the first-generation cholangioscope.
The aim of this paper is to describe the use of a digital cholangioscope to direct lighting during a PDT session in extrahepatic CC using a locally-developed laser source.
METHOD
Technique
PDT procedure information
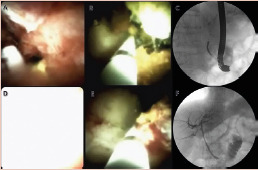
The patient receives an intravenous photosensitizer (Photogen®, King of Prussia, PA, USA - 1.5 mg/kg) 24 h before the procedure. Its peak of light absorption is at 630 nm wavelength. The procedure starts with a regular duodenoscopy (Olympus TJF-180) under general anesthesia. After identification of the major papilla and retrograde cannulation, the digital cholangioscope (SpyGlassTM DS, Boston Scientific, Natick, MA) is introduced into the common bile duct. Then, the cholangioscopic examination helps to identify the neoplastic stricture. Under direct visualization, the lighting catheter (Medlight S.A., RD10-323, Switzerland) is advanced through the cholangioscope. It consists of a typical 3-way ERCP cannula. The first port carries a 1 cm-long cylindrical light diffuser at its end. Two black radiopaque marks demarcate the limits of the diffuser. The second port accommodates a 0.025-inch guidewire and the third is an injection port (Figure 1). After positioning under cholangioscopic guidance, the lighting initiates. The dose is 90 J/cm² with a power of 70 mW/cm² (Figure 2). Repositioning is recommended every centimeter to cover all strictured area. At the end of the procedure, a final cholangioscopy assesses the bile duct for the immediate result and adverse events.
FIGURE 1. A) Fiber with enclosure; B) fiber without enclosure; C) proximal end of the lighting catheter; D) distal end of the fiber and between the two metal marks is the 1 cm laser diffuser.
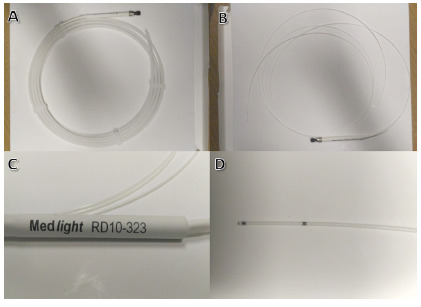
FIGURE 2. The handheld controller of the light source.
Post-procedure care
The patient is kept fasting for the following 24 h. If no adverse event is detected, the oral diet is initiated. Discharge is done under strict orientation on photoprotection (avoidance of light exposure and wearing sunglasses), especially during the first week after the PDT session.
RESULTS
This procedure was applied in one 82-year-old male referred to our tertiary center due to obstructive jaundice and weight loss in the last two months. An endoscopic ultrasound (EUS) revealed a severe dilation of the common bile duct associated with choledocholithiasis. The ERCP confirmed those findings but was not able to remove the stones due to disproportionate dilatation of the common bile duct. Therefore, we opted for biliary plastic stenting. The patient experienced improvement in his clinical condition but the cholestasis recurred 45 days after the first procedure. Two further ERCPs failed to remove the stones. During his third procedure, a long irregular stricture of the common hepatic duct became clear and he was referred to another sonographic evaluation.
Besides choledocholithiasis, the new EUS revealed dilation of hepatic duct up to a well-circumscribed hypoechoic solid mass measuring 1.8x2 cm compressing the common hepatic duct. The mass seemed to involve the common hepatic artery as well. The EUS-guided fine-needle aspiration confirmed the diagnosis of moderately differentiated cholangiocarcinoma (Bismuth I).
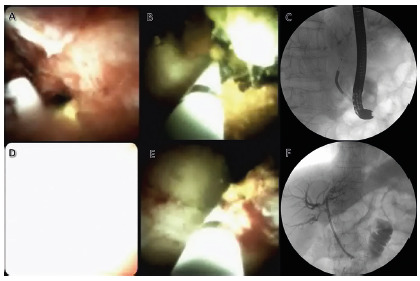
After staging, the mass was deemed unresectable and the patient was referred for palliative treatment. After multidisciplinary meeting with the oncology team, was proposed an adjunct PDT to address the recurrent biliary obstruction. The procedure was uneventful and had duration of 150 min (Figure 3). At the end, was performed biliary drainage with a 10 Fr plastic stent, since self-expandable metallic stent was not available at that moment.
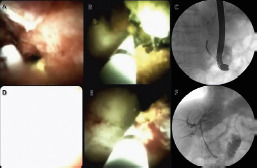
FIGURE 3. Photodynamic therapy (PDT) of an extrahepatic cholangiocarcinoma using a digital cholangioscopy to deliver the laser: A) cholangioscopic identification of the neoplastic stricture; B) placement of the lighting catheter across the neoplastic stricture; C) fluoroscopic control of the PDT catheter positioning; D) cholangioscopic appearance during lighting; E) repositioning of the fiber after the first lighting; F) final fluoroscopic control after the PDT session and plastic stenting.
In the following week, the patient did not report any photosensitivity. There was, however, an early recurrence of the cholestasis complicated with cholangitis. The ERCP revealed obstruction of the stent with debris and biliary sludge secondary to tumor necrosis. Biliary sweeping followed by new drainage resolved the patient’s acute condition. Thereafter, he remained asymptomatic for three months, the longest period since the onset of the disease. At his next recurrence, he underwent drainage with a self-expandable metallic stent.
The patient kept on with systemic treatment and ultimately required duodenal stenting for palliation of dysphagia. He perished due to complications of lung metastases two years after the onset of symptoms and 15 months after the PDT session.
DISCUSSION
This is the first report of a digital cholangioscopy-guided biliary PDT outside the USA. Moreover, the employment of a Brazilian laser source and the good clinical outcome make this report unique and relevant.
The PDT has been widely employed over the last decade for local specific treatment of unresectable biliary neoplasia. In fact, several studies have already evaluated the effectiveness of PDT plus biliary drainage and demonstrated the superiority of this association in comparison with sole drainage 3 , 9 , 18 . Also, some publications have demonstrated PDT plus chemotherapy to be superior to chemotherapy alone 13 . In this sense, Moole et al 7 recently published a meta-analysis pooling 10 studies and 402 patients comparing PDT plus biliary stenting vs. only biliary stenting. The authors demonstrated that patients undergoing adjunct PDT had a higher success rate of biliary drainage (defined as >50% decrease in bilirubin levels within seven days), increased survival rates, significant improvement in Karnofsky score, and lower rates of post-procedure cholangitis. Despite the high heterogeneity, a subgroup analysis involving only prospective studies confirmed all these findings except for the reduction in the rate of cholangitis 7 .
As the main side effect, photosensitivity occurs in about 11% of patients 7 . However, it can be effectively prevented with simple recommendations such as to avoid exposure to natural and artificial lights, and wearing sunglasses. Other factors that hampered the wide acceptance of PDT are high costs and limited availability of equipment and expertise 11 . The use of local technology may significantly reduce costs, allowing wider availability of equipment and ultimately helping to nurture local expertise. Such information emphasizes the importance of the present report.
Some studies have already described the use of cholangioscopy to target the delivery of light energy. In 2011, Talreja et al 17 published a retrospective cohort study reporting a significant reduction in the fluoroscopy exposure time of patients undergoing cholangioscopy-guided PDT compared to those undergoing standard PDT. Although the difference did not reach statistical significance, the authors also found improvement in overall survival: the intervention group (PDT + cholangioscopy) had an average increase of 186 days in survival.
Hypothetically, visual control of the laser delivery might optimize treatment, leading to increased tumor necrosis and less exposure of healthy tissue to light explaining the increase in mean survival found by Talreja et al 17 . Of note, the authors employed the first generation cholangioscope. The second generation, named digital cholangioscope, carries significant improvement in both image quality and handling, which could further enhance the benefit of the association. To date, only one case of PDT with digital cholangioscopy has been reported 15 . The present study is, therefore, the second report in the world, the first outside the USA, and the only one to employ a locally-developed light source.
Our report is not exempt from limitations. The level of evidence is low and generalization of these results is not advisable. However, it can and should be used to support robust prospective studies that might refine the method and standardize the procedure. Moreover, our patient was not procedure-naïve. If he were, the outcome of the PDT might have been better once usually the earlier the treatment, the better the outcome. Finally, we did not have a self-expandable metallic stent for immediate drainage after the PDT session. The use of a plastic stent probably explains the early recurrence of the cholestasis, which could have been avoided if a larger metallic stent had been employed at first.
CONCLUSION
Digital cholangioscopy-guided biliary PDT is feasible and seems safe and effective as an adjunct modality in the palliation of extrahepatic cholangiocarcinoma.
Footnotes
Financial source: none
Central message: The clinical application of photodynamic therapy using a locally-developed laser source is feasible in the palliative setting of a cholangiocarcinoma
Perspective: This case report demonstrates the clinical application of photodynamic therapy in the palliative treatment of cholangiocarcinoma using a Brazilian laser source. The outcome was appropriate with no relevant adverse events. This favorable clinical outcome highlights the importance of such a report due to the perspective of cost reduction and the consequent broader availability of the method
REFERENCES
- 1.Benson Ab 3Rd, D'angelica Mi, De Abbott, Ta Abrams, Sr Alberts, Da Saenz, Are C, Db Brown, Dt Chang, Am Covey, Hawkins W, Iyer R, Jacob R, Karachristos A, Rk Kelley, Kim R, Palta M, Jo Park, Sahai V, Schefter T, Schmidt C, Jk Sicklick, Singh G, Sohal D, Stein S, Gg Tian, Vauthey J-N, Ap Venook, Ax Zhu, Kg Hoffmann, Darlow S. Nccn Guidelines Insights Hepatobiliary Cancers, Version 1.2017. J Natl Compr Canc Netw. 2017;15:563–573. doi: 10.6004/jnccn.2017.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chedid Marcio F. Hepatocellular Carcinoma: Diagnosis And Operative Management. Abcd, Arq. Bras. Cir. Dig. 2017;30(4):272–278. doi: 10.1590/0102-6720201700040011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dolak W, Schwaighofer H, Hellmich B, Stadler B, Spaun G, Plieschnegger W, Hebenstreit A, Weber-Eibel J, Siebert F, Emmanuel K, Knoflach P, Gschwantler M, Vogel W, Trauner M, Puspok A. Photodynamic Therapy With Polyhematoporphyrin For Malignant Biliary Obstruction A Nationwide Retrospective Study Of 150 Consecutive Applications. United Eur Gastroenterol J. 2017;5:104–110. doi: 10.1177/2050640616654037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gatto M, Bragazzi Mc, Semeraro R, Napoli C, Gentile R, Torrice A, Gaudio E, Alvaro D. Cholangiocarcinoma Update And Future Perspectives. Dig Liver Dis. 2010;42:253–260. doi: 10.1016/j.dld.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Guro H, Kim Jw, Choi Y, Cho Jy, Yoon Y-S, Han H-S. Multidisciplinary Management Of Intrahepatic Cholangiocarcinoma Current Approaches. Surg Oncol. 2017;26:146–152. doi: 10.1016/j.suronc.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Lopes Felipe De Lucena Moreira, et al. Influence Of Hepatocellular Carcinoma Etiology In The Survival After Resection. Abcd, Arq. Bras. Cir. Dig. 2016;29(2):105–108. doi: 10.1590/0102-6720201600020010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moole H, Tathireddy H, Dharmapuri S, Moole V, Boddireddy R, Yedama P, Dharmapuri S, Uppu A, Bondalapati N, Duvvuri A. Success Of Photodynamic Therapy In Palliating Patients With Nonresectable Cholangiocarcinoma A Systematic Review And Meta-Analysis. World J Gastroenterol. 2017;23:1278–1288. doi: 10.3748/wjg.v23.i7.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ortner M-A. Photodynamic Therapy For Cholangiocarcinoma. Lasers Surg Med. 2011;43:776–780. doi: 10.1002/lsm.21106. [DOI] [PubMed] [Google Scholar]
- 9.Ortner Mej, Caca K, Berr F, Liebetruth J, Mansmann U, Huster D, Voderholzer W, Schachschal G, Mossner J, Lochs H. Successful Photodynamic Therapy For Nonresectable Cholangiocarcinoma A Randomized Prospective Study. Gastroenterology. 2003;125:1355–1363. doi: 10.1016/j.gastro.2003.07.015. [DOI] [PubMed] [Google Scholar]
- 10.Patel J, Rizk N, Kedia P, Sharaiha Rz, Kahaleh M. Cholangioscopy-Assisted Photodynamic Therapy For Cholangiocarcinoma. Gastrointest Endosc. 2015;81:1012–1013. doi: 10.1016/j.gie.2014.09.060. [DOI] [PubMed] [Google Scholar]
- 11.Bt Petersen, Chuttani R, Croffie J, Disario J, Liu J, Mishkin D, Shah R, Somogyi L, Tierney W, Lm Wong Kee Song. Photodynamic Therapy For Gastrointestinal Disease. Gastrointest Endosc. 2006;63:927–932. doi: 10.1016/j.gie.2006.02.044. [DOI] [PubMed] [Google Scholar]
- 12.Qureshi K, Jesudoss R, Ams Al-Osaimi. The Treatment Of Cholangiocarcinoma A Hepatologist's Perspective. Curr Gastroenterol Rep. 2014;16:412–412. doi: 10.1007/s11894-014-0412-2. [DOI] [PubMed] [Google Scholar]
- 13.Quyn Aj, Ziyaie D, Polignano Fm, Tait Is. Photodynamic Therapy Is Associated With An Improvement In Survival In Patients With Irresectable Hilar Cholangiocarcinoma. Hpb (Oxford) 2009;11:570–577. doi: 10.1111/j.1477-2574.2009.00102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sá Gustavo Pilotto D. Liver Transplantation For Carcinoma Hepatocellular In São Paulo: 414 Cases By The Milan/Brazil Criteria. Abcd, Arq. Bras. Cir. Dig. 2016;29(4):240–245. doi: 10.1590/0102-6720201600040007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saumoy M, Kumta Na, Kahaleh M. Digital Cholangioscopy For Targeted Photodynamic Therapy Of Unresectable Cholangiocarcinoma. Gastrointest Endosc. 2016;84:862–862. doi: 10.1016/j.gie.2016.05.020. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt A, Bloechinger M, Weber A, Siveke J, Von Delius S, Prinz C, Schmitt W, Schmid Rm, Neu B. Short-Term Effects And Adverse Events Of Endoscopically Applied Radiofrequency Ablation Appear To Be Comparable With Photodynamic Therapy In Hilar Cholangiocarcinoma. United Eur Gastroenterol J. 2016;4:570–579. doi: 10.1177/2050640615621235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Talreja Jp, Degaetani M, Sauer Bg, Kahaleh M. Photodynamic Therapy For Unresectable Cholangiocarcinoma Contribution Of Single Operator Cholangioscopy For Targeted Treatment. Photochem Photobiol Sci. 2011;10:1233–1238. doi: 10.1039/c0pp00259c. [DOI] [PubMed] [Google Scholar]
- 18.Zoepf T, Jakobs R, Arnold Jc, Apel D, Riemann Jf. Palliation Of Nonresectable Bile Duct Cancer Improved Survival After Photodynamic Therapy. Am J Gastroenterol. 2005;100:2426–2430. doi: 10.1111/j.1572-0241.2005.00318.x. [DOI] [PubMed] [Google Scholar]


