Abstract
Objective:
The aim of this study was to define whether rapidly reallocating health care workers not experienced with PP for performing PP in ICU is feasible and safe.
Summary Background Data:
In the setting of severe acute respiratory distress syndrome (ARDS), the use of prone and supine positioning procedures (PP) has been associated with improved oxygenation resulting in decreased mortality. Nevertheless, applying PP is time consuming for ICU staffs that are at risk of mental of physical exhaustion, especially with the constant surge of admitted COVID-19 patients with severe ARDS.
Methods:
This prospective cohort study conducted at a single regional university hospital between March 27 and April 15, 2020. Among 117 patients admitted to ICU, 67 patients (57.3%) presented with proven SARS-CoV-2 infection with severe ARDS requiring PP. After accelerated simulation training, 109 volunteers including surgeons, physicians, nurses and physiotherapists, multiple dedicated teams performed daily multiple PP following a systematic checklist. Patient demographics and PP data were collected. Patient safety and health care workers safety were assessed.
Results:
Among 117 patients admitted to ICU, 67 patients (57.3%) required PP. Overall, 53 (79%) were male, with a median age of 68.5 years and median body mass index of 29.3 kg/m2. A total of 384 PP were performed. Overall, complication occurred in 34 PP (8.8%) and led to PP cancelation in 4 patients (1%). Regarding health care workers safety, four health care workers presented with potential COVID-19 related symptoms and none was positive.
Conclusions:
To overcome the surge of critically ill COVID-19 patients, reallocating health care workers to targeted medical tasks beyond their respective expertise such as PP was safe.
Keywords: COVID-19, Prone Positioning, Surgeon reallocation, Workforce
Coronavirus Disease 2019 (COVID-19) is a novel viral disease that currently spreads worldwide becoming a pandemic. To date, the case-fatality rate has been reported up to 7.2% mainly owing to the development of severe acute respiratory distress syndrome (ARDS).1,2 Among infected patients, around 20% to 30% of patients will require intensive care unit (ICU) admission due to ARDS associated with a mortality rate nearing 50%.3,4,5 In severe ARDS, the use of prone positioning has been associated with improved oxygenation resulting in decreased mortality.6 However, in the context of the current outbreak, applying prone positioning on a daily basis to all patients is time consuming, especially with the constant surge of admitted patients with severe ARDS. Additionally, in the setting of viral outbreak, medical staff work load and anxiety are already increased by the need of complying with strict infection control measures given the risk of contamination.7 In contrast, some non-ICU staffs were rendered out-of-work as elective surgical caseload has been substantially decreased to allow for better ICU and hospital bed capacity.
Consequently, non-ICU staffs including surgeons and OR staffs have spontaneously offered their help to avoid mental and physical exhaustion of ICU staffs. Prone positioning has been then targeted as part of the ICU patient management that could be managed by non-ICU staffs. Volunteer physicians, nurses, and physiotherapists have followed an accelerated training to form a dedicated team, called as “Team DV” (Team Decubitus Ventral) for performing multiple positioning procedures (PP) on a daily basis.
We report here our experience in terms of feasibility, patient safety, and staff safety, at an institutional level.
METHODS
Study Population
All patients admitted in ICU for severe ARDS (according to Berlin criteria8) with a RT-PCR diagnosis (NucleoSpin RNA Virus kit, Macherey-Nagel Inc., Bethlehem, PA) of SARS-CoV-2 and/or typical chest CT features of COVID-19 and who required prone and supine positioning (persistent PaO2/FiO2 ratio <150 mm Hg despite mechanical ventilation, sedation, and curarization) by a dedicated team between March 27and April 15, 2020 at a single university hospital were prospectively included. Positioning procedure (PP) corresponded to any procedure consisting in placing the patient in prone or supine position. Patients with severe ARDS due to an identified cause other than COVID-19 were excluded. Over the study period, the number of ICU beds has been extended from 40 to a maximum of 92 beds to anticipate the surge.
Positioning Team
Volunteers were searched among physicians, operating room nurses that were not yet involved in non-ICU and ICU dedicated to COVID-19 patients. Physiotherapists were also involved owing to their ability to position patients safely. Within 1 day, 212 volunteers were identified and trained through 15 training sessions within 3 days. Ninety-minute training sessions were delivered by simulation educators under supervision of an anesthesiologist (F.C.) and 1 surgeon (L.S.D.) using the educational platform of the university medical simulation center. Briefly, rationale, technical aspects, and specific complications of prone and supine positioning were reviewed. The simulation sessions followed the usual structure of simulation-based learning, namely: briefing with presentation of the training program and a checklist (Fig. 1); practical prone and supine positioning simulation; debriefing with reflective analysis.9 Additionally, each member was trained regarding the use of full personal protective equipment (PPE) including FFP2 particle filtering face mask with protective eyewear and disposable surgical gown, cap, and gloves. Each positioning team consisted of 1 physician, 1 OR nurse, and 1 physiotherapist along with 1 ICU nurse and 1 anesthesiologist/intensivist. The checklist was systematically applied before initiating PP to facilitate communication between all team members. The main objective of this checklist was to prevent the occurrence of PP-related complications such as nonscheduled extubation or removal of intravenous or intra-arterial lines during the procedure, and the development of pressure sores between the procedures. Additionally, the procedure could be cancelled or aborted in case of respiratory or hemodynamic instability before or during prone or supine positioning. Each patient was placed prone 1 day for a maximal duration of 16 hours and then replaced supine for 8 hours. This was repeated until clinical improvement indicating that prone positioning was no more needed or stopped in case of occurrence of any PP-related complications precluding new PP.
FIGURE 1.
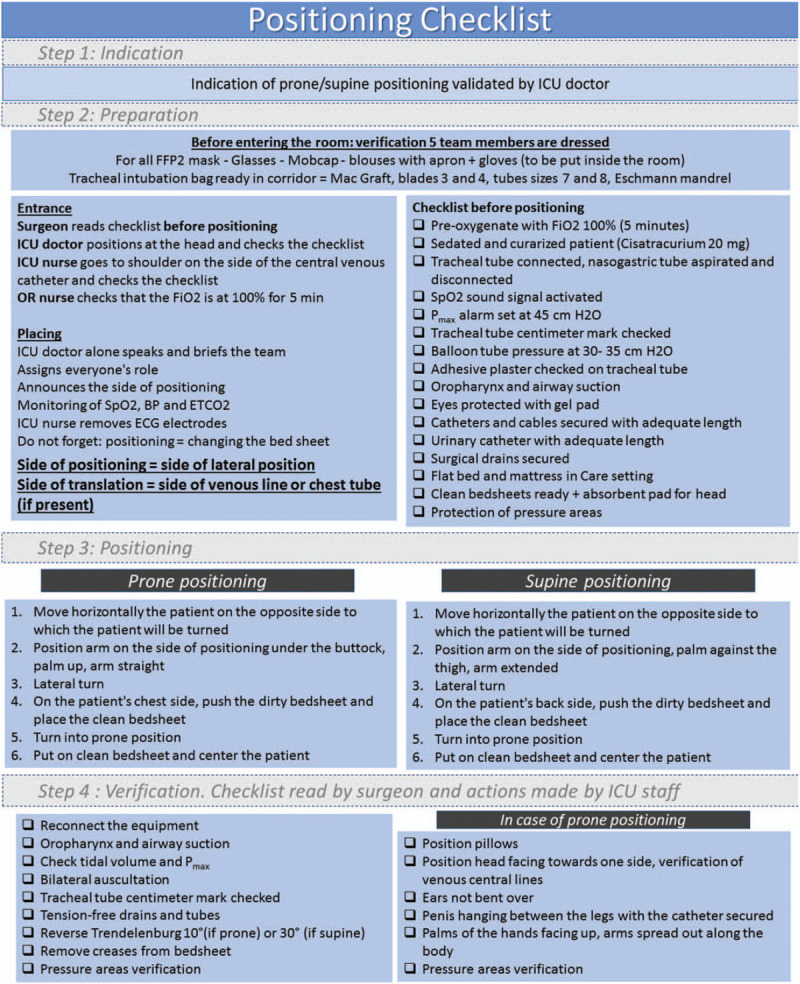
Procedure positioning checklist.
Data Collection
Patients’ demographics such as sex, age, body mass index, and significant medical history were collected. Duration of ICU stay was calculated as the time between the ICU admission date and the date of death or the date of ICU discharge whether to an outside ICU at another hospital or to a post-ICU ward. The median number of PP for each patient, both prone and supine positioning, during the study period was recorded. During each PP, patient weight, PP duration, pre- and post-PP oxygenation monitoring data and the occurrence of complications as detailed above were prospectively collected.
Regarding medical staff safety, a 6-question survey was administered by email 15 days after the last day of the study period, to all team members who performed at least 1 PP during the study period. All surveys were anonymous. The survey was created using a widely available internet tool (http://www.googleforms.com). Questions related to volunteers’ background (nurse or physician or physiotherapist), number of performed PPs, COVID-19-related symptoms, and testing and PP-related symptoms.
Statistical Analysis
Utilizing SPSS Statistics software (version 22.0, IBM, Armonk, NY), continuous variables were expressed as median (range) or mean (standard deviation) unless otherwise specified. Continuous variables were compared using an independent samples t test or a Mann-Whitney U test as appropriate. Categorical variables were compared using a Chi-square test or a Fisher exact test as appropriate. This study was conducted according to the ethical standards of the Committee on Human Experimentation institutionally approved and reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.10
RESULTS
Study Population
Over the study period, 660 patients with suspected SARS-CoV-2 infection were hospitalized at a tertiary regional university hospital, of which 371 had a RT-PCR-proven SARS-CoV-2 infection or typical chest CT features of COVID-19. Among 117 patients admitted to ICU, 67 patients (57.3%) developed severe ARDS requiring PP. Most were male (n = 53, 79%), median age was 68.5 years [interquartile range (IQR), 61.5–72.5], and median body mass index was 29.3 (IQR, 26.3–34.4). Demographics and baseline characteristics of the 67 included patients are listed in Table 1. Median ICU stay was 16 days (IQR, 10–22). One patient required extracorporeal membrane oxygenation. After a median follow-up of 28 days (IQR, 21–35) from the ICU admission date, 32 patients (48%) have been discharged home while 20 (30%) remain hospitalized in ICU. The overall mortality rate was 15% (n = 10).
TABLE 1.
Descriptive Data From 67 Consecutive Patients Who Underwent Positioning Procedures in ICU Between March 27, 2020 and April 15, 2020
| Characteristics | N = 67 |
| Sex, n (%) | |
| Male | 53 (79) |
| Female | 14 (21) |
| Age, y | 68.5 (61.5–72.5) |
| BMI, kg/m2 | 29.3 (26.3–34.4) |
| Active smoking, n (%) | 7 (11) |
| Diabetes mellitus, n (%) | 21 (32) |
| Preexisting hypertension, n (%) | 41 (61) |
| Chronic pulmonary disease, n (%) | 23 (35) |
| Active cancer, n (%) | 3 (5) |
Continuous variables are reported as median (interquartile range). BMI indicates body mass index.
PP
Overall, 384 PP were performed with a median number per patient of four (IQR, 2–8) (Table 2). Mean duration for PP was 14.5 minutes (SD, 6.3). In case of prone positioning, mean duration was 17 minutes (SD, 6.9), whereas 12.7 minutes (SD, 5.0) in case of supine positioning (P < 0.001). Overall, the complication rate was 8.8% (n = 34) and was not influenced by prone or supine positioning. PP procedure was aborted or cancelled in 4 patients (1%) owing to complications, including respiratory instability (n = 3) and pressure sores (n = 1). PP characteristics and complications are listed in Table 2.
TABLE 2.
Characteristics and Complications From 384 Positioning Procedures
| Characteristics | Overalln = 384 (100%) | Prone to Supinen = 219 (57%) | Supine to pronen = 165 (43%) | P |
| Positioning duration, min | 14.5 (6.3) | 12.7 (5.0) | 17 (6.9) | <0.001 |
| Pplat before PP, cm of water | 22.9 (4.5) | 22.8 (4.6) | 23 (4.5) | 0.136 |
| Pplat after PP, cm of water | 23.1 (4.2) | 22.6 (4.0) | 23.7 (4.4) | 0.004 |
| FiO2 before PP, % | 69.5 (24.8) | 66.5 (26.3) | 73.7 (22.1) | 0.001 |
| SpO2 before PP, % | 96 (2.9) | 96.3 (2.7) | 95.4 (3) | 0.009 |
| SpO2 after PP, % | 97.3 (4.1) | 97.4 (4.7) | 97.2 (3.0) | 0.221 |
| Positioning procedure-related complications, n (%) | 34 (8.8) | 17 (7.8) | 17 (10.3) | 0.385 |
| Respiratory or hemodynamic instability | 16 (4.1) | 7 (3.2) | 9 (5.4) | |
| Pressure sores | 11 (2.9) | 8 (3.6) | 3 (1.8) | |
| Nonscheduled extubation | 5 (1.3) | 2 (0.9) | 3 (1.8) | |
| Removal of intravenous or intra-arterial lines | 2 (0.5) | 0 (0) | 2 (1.2) |
Continuous variables are reported as mean (standard deviation) unless otherwise specified.
FiO2 indicates fraction of inspired oxygen; Pplat, end-inspiratory plateau pressure of the respiratory system; SpO2, pulsed blood oxygen saturation level.
Medical Staff Safety
Of 212 trained volunteers, 109 eventually performed PP and 95 (87%) responded to the survey. Among them, 37 (40%) were physicians or surgeons, 28 (29.5%) were nurses or OR nurses, and 29 (30.5%) were physiotherapists. Twenty-three (24.5%) respondents performed >20 PP, 27 (28.7%) between 10 and 20 PP, and 44 (46.8%) <10 PP. Additionally, 69 (72.6%) respondents found the training session helpful for PP preparation and 50 (52.6%) found it reassuring regarding the risk of SARS-CoV-2 infection.
Four (4%) respondents experienced potential COVID-19-related symptoms during the study period or within the 15 following days. Of them, 3 underwent nasopharyngeal testing for SARS-CoV-2 infection and none responded having been tested positive. None was hospitalized.
Regarding PP-related symptoms, 11 (12%) respondents responded positively reporting back pain (n = 8), joint pain (n = 2), and anxiety due to the risk of SARS-CoV-2 infection (n = 1).
DISCUSSION
This organizational initiative was spontaneously initiated by health care workers to help overcome the increasing workload in ICU and was enthusiastically received as an integral part of the institutional response to the outbreak. As the pandemic remains active but seems to slow down, health care systems have been impacted worldwide and organizational disruptions will persist for months to come. Considering further the risk of an outbreak reactivation with a so-called “second surge,” sharing this experience among others is critical to help address present and future challenges due to COVID-19.11,12
Through this experience at the scale of our institution, several lessons have been learned. First, as part of the general effort, both interdisciplinary cohesion and agility have been demonstrated with >200 health care workers from various professional backgrounds who volunteered within roughly 24 hours. Second, most volunteers were not experienced with the technical aspects of PP. Fast dissemination of the necessary knowledge has been made possible through our local medical simulation center where all volunteers had to attend 1 training session. This highlights how simulation allows targeted and accelerated training. This training has translated in safety for both health care workers and patients. Indeed, no team member reported SARS-CoV-2 infection and PP-related complication rates were similar to the available literature.13 Nevertheless, the patient safety could not be fully assessed as outcomes from patients managed by the “Team DV” were not compared to those positioned by experienced ICU staffs. Furthermore, this allowed reassuring team members regarding the risk of SARS-CoV-2 infection, as reported by more than half of respondents. Indeed, training involving simulation and debriefing was not only focused on technical aspects of PP but also provided accurate preparation to the use of PPE. This training was paramount to avoid an inappropriate use of PPE thereby reducing the risk of contamination and the risk of PPE shortage. Similarly, grouping COVID-19 patients into dedicated “COVID-19 areas” in ICU allowed reducing the risk of PPE shortage as disposing the full PPE of each team member between each patient was not necessary in such dedicated areas. Finally, although the number of patients requiring PP decreases and medical clinics and elective surgery caseload gradually resumes, all trained volunteers remain enlisted in case of new surge.
Albeit restricted to 1 particular task, the present study demonstrates the feasibility and the safety of reallocating health care work force to targeted medical tasks beyond their respective expertise. Interdisciplinary cohesion, accelerated training using simulation and procedures standardization using checklists were critical for the rapid deployment of these dedicated teams.
Acknowledgments
The authors thank all of the healthcare workers who carried out the patients positioning as members of the “Team DV”: Sfiya Ait El Kamel, Justine Alardin, Claire Ballot, Nicolas Barbat, Lucas Barberot, Mélitine Barthelet, Ghislaine Baud, Chloé Bermont, Alexandre Bezard, Bénédicte Biansan, Claire Bodivit, Yoann BOUR, Bérangère Bourgeois, Camille Bouteille, Claire Bovidit, Amélie Camelio, Fabio Carminati, Marylène Chabauty, Hugoline Chapuis, Léna Chevalier, Marlène Chotard, Coline Cochet, Aurore D’hooghe, Thibaut Dabudyk, Tatiana Dahes, Aurélie Dauta, Loïc David, Nicolas David, Margaux Debuchy, Marc Decrock, Cécile Destynder, Leslie-Anne Dubois, Julien Fageot, Benjamin Forien, Laura Franco, Elisabeth Gachignard, Zoé Garneret, Patrice Gayet, Aurélie Gerard, Paul Girard, Eléanore Grandvoinnet, Noor Hamdan, Bruno Heyd, Olivier Hild, Jean-Yves Huart, Anne Jacquinot, Marie-Josée Jacmaire, Estelle Jeanvoine, Carole Jeancler, Clotilde Jouchoux, Emeline Lacour, Jean Lambert, Aurore Lamy, Fanny Lorandon, Sandrine Lebon, Nathalie Lecarboulek, Anna LI-Marchetti, François Loisel, Gabriel Macedo, Alexandre Mathieu, Camille Menu, Antoine Meranger, Garvey Mezepo, Stéphanie MORA, Vanessa Morel, Isabelle Moutenet, François Nobili, Narcisse Ouedraogo, Théo Paget, Thibault Pagnot, Béatrice PAGOT, Lison Pellegrini, Romain Peroz, Marion Petey, Camille Petit, Chloé Petremant, Evan Pintapary, Paul Poirier, Anne-Lise Poirot, Florence Poras, Johanna Pothin, Marie-Aline Pretot, Corinne Pussini, Anaïs Raichon, Célia Regent, François Richard, Vincenzo Ritucci, Julie Ritter, Thibault Robin, Séverin Rochet, Aloïs Ronsin, Maryse Rousselet, Lucie Rudziewik, Lauriane Salwey, Charline Sayah, Pierre-Etienne Serree, Lucie Simon, Anne-Lise Trocme, Justine Trzebowski, Uwe Studer, Marie-Cécile Vallet, Elodie van Hecke, Luca Vaubourg, Julien Vaytet, Yannick Vene, Manon VIEUXMAIRE, Alain vigier, Coralie Voisin and Edouard Woussen.
The authors thank all the members of ICU medical and nurse staff who cared for COVID-19 patients and collaborated with the “Team DV” members.
The authors would like to thank Alexandra Laithier and Elodie Parra for assistance in building, organizing and planning the teams. We thank Alain Dussaucy for his help in acquiring informative data. We also thank Chantal Carroger, Catherine Chirouze, Samuel Limat, Thierry Moulin, and Emmanuel Samain for support and comments on the manuscript.
Footnotes
Conflicts of interest and source of funding: The authors declare that they do not have anything to disclose regarding funding or conflict of interest relating to this publication.
REFERENCES
- 1.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020; Published online March 23. [DOI] [PubMed] [Google Scholar]
- 2.Marini JJ, Gattinoni L. Management of COVID-19 respiratory distress. JAMA 2020; Published online April 24. [DOI] [PubMed] [Google Scholar]
- 3.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liew MF, Siow WT, MacLaren G, et al. Preparing for COVID-19: early experience from an intensive care unit in Singapore. Crit Care 2020; 24:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; Published online February 24. [DOI] [PubMed] [Google Scholar]
- 6.Guérin C, Reignier J, Richard J-C, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013; 368:2159–2168. [DOI] [PubMed] [Google Scholar]
- 7.The Lancet. COVID-19: protecting health-care workers. Lancet 2020; 395:922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Definition Task Force ARDS, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA 2012; 307:2526–2533. [DOI] [PubMed] [Google Scholar]
- 9.Dieckmann P, Torgeirsen K, Qvindesland SA, et al. The use of simulation to prepare and improve responses to infectious disease outbreaks like COVID-19: practical tips and resources from Norway, Denmark, and the UK. Adv Simul 2020; 5:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370:1453–1457. [DOI] [PubMed] [Google Scholar]
- 11.Coons BE, Tam SF, Okochi S. Rapid development of resident-led procedural response teams to support patient care during the Coronavirus Disease 2019 epidemic: a surgical workforce activation team. JAMA Surg 2020; Published online April 30. [DOI] [PubMed] [Google Scholar]
- 12.O’Connell KM, Maier RV. Trail blazers without blades: surgeons as palliative care physicians in response to COVID-19. Ann Surg 2020; Published online April. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guérin C, Beuret P, Constantin JM, et al. A prospective international observational prevalence study on prone positioning of ARDS patients: the APRONET (ARDS Prone Position Network) study. Intensive Care Med 2018; 44:22–37. [DOI] [PubMed] [Google Scholar]


