“Never let a good crisis go to waste”
– Winston Churchill
The global COVID-19 pandemic has had dramatic effects on healthcare systems worldwide, being described as a “black swan,” a rare and unexpected event whose magnitude will likely have a severe impact on history.1 The COVID-19 emergency has pushed healthcare and surgical institutions to adapt, changing the conventional ways that clinicians have been used to working. In many parts of the world, the worst of the initial surge in cases has waned, and many institutions have entered the transition phase.2 Although the full recovery phase in a COVID-free era seems still far away, there are increasing calls for surgical systems to address some issues and concerns and rethink the “new normal” once the pandemic is over.
Recent literature has suggested the need for surgical systems to develop antifragile strategies, meaning that the systems can become stronger after a black swan event such as the current pandemic by “addressing all challenges posed by the enforced circumstances for successful management of the Transition Phase while on guard against another pandemic.”2 To apply an antifragile approach to surgery, it is necessary to consider principles3 that can lead to the identification of essential topics and practical recommendations.
Building on the crisis management literature, we aim in the paragraphs below to investigate the meaning of antifragility, raise some questions about how surgery can employ such strategies, and identify important traits for surgical leaders of the future. Specifically, the purpose of this paper is to propose the applicability of principles borrowed from the crisis management sphere to a surgical context. We will address the following topics that will be essential for surgical programs to move to full recovery:
-
1.
Cognitive biases
-
2.
Optionality
-
3.
Redundancy
-
4.
Barbell strategy
-
5.
Hormesis strategy
-
6.
Balancing feedback loops.
Figure 1 and Table 1 summarize these main concepts and identify some tentative strategies.
FIGURE 1.
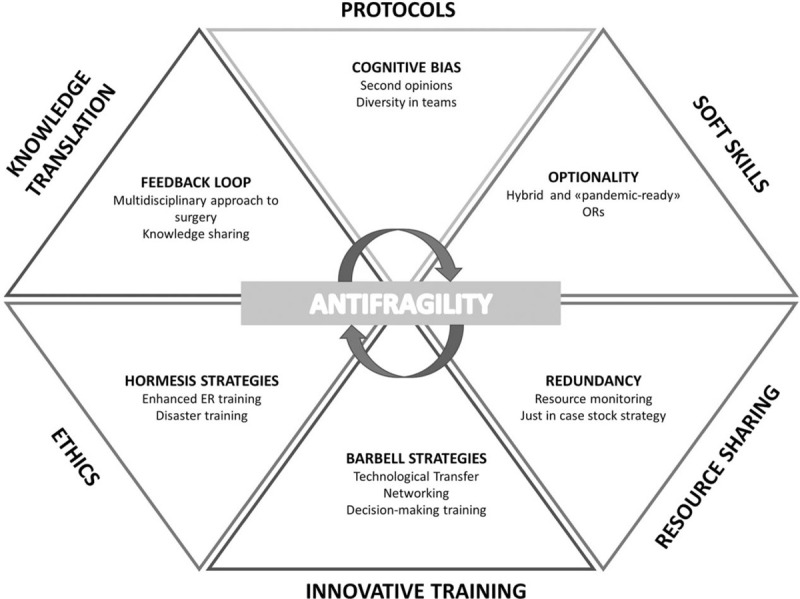
Antifragility in Surgery. A roadmap.
TABLE 1.
Antifragility in Surgery. COVID-related Examples and Recommended Strategies
| Feature | Definition | COVID-related Examples | References | Suggested Strategies |
| Cognitive biases | Errors in the decision-making when the brain simplifies information processing | Lack of protection due to underestimationDiscrimination | Garcia-Alamino, 2020Bonner et al, 2020 | New protocolsKnowledge sharingSecond opinionsMultidisciplinarityDiversity in teams |
| Optionality | Presence of flexible resources that might be activated when needed | Transforming ORs into ICUs | Peters et al, 2020Liang et al, 2020 | Hybrid or pandemic-ready ORs |
| Redundancy | Extra stock availability | Unredundant surgical resources like ICUs | Liang et al, 2020Cobianchi et al, 2020 | NetworkingResource monitoring and sharing“Just in case” stock strategies |
| Barbell strategies | Reduced exposure to adverse outcomes due to a balanced portfolio | Enhanced training | Cobianchi et al, 2020Garcia Vasquez et al, 2020 | New paradigms in surgical educationOpen innovationTechnological transfer |
| Hormesis strategy | Repeated stimulation or stress that ultimately augments an organism's defences against potentially harmful influences | Triage and changes in the job tasks | Brindle et al, 2020 | Training in other departmentsOverseas TrainingInnovative training (eg, gaming)Protocols |
| Balancing feedback loops | Circles of cause and effect that counter a change with a push in the opposite direction: the harder the push, the harder the system pushes back | Multidisciplinarity vs specialization (eg, MGH COBRA experience) | Albutt et al, 2020 | Hybrid MDsKnowledge translation tools |
COBRA indicates COVID-19 bundled response for access; ICUs, intensive care unit; ORs, operating rooms.
COGNITIVE BIASES
Cognitive biases are errors in the decision-making occurring when the brain simplifies information processing. They are frequent in any field, generated by the knowledge that a person has and limits the will to consider a more comprehensive portfolio of options leading to risk underestimation. According to medical literature, up to 75% of all clinical errors have cognitive origins.4
The COVID-19 crisis showed the risk of cognitive biases in the clinical setting and surgery. For instance, in the initial phases of the emergency, the underestimation of the virus and its morbidity led to a lack of adequate protection of clinicians exposed to critically infected patients,5 with several hundred healthcare workers dying from COVID-19.6 Biases also involved the relationships between medical doctors and patients. Although unconscious bias can lead to discrimination between surgical and medical teams and their patients,7 the COVID-19 pandemic has highlighted the tragic disparities in death rates among African American and Latinx communities, resulting in worse surgical outcomes for racial minorities.8
Practical strategies for the future may include the set up of new knowledge sharing and decision-making protocols, requiring multidisciplinary teams9 or second opinions in the diagnosis or operative and treatment plans. According to the literature and scientific societies,10 diversity in surgical teams may also enhance the global performance, the outcome of the cure,11 and the patients’ satisfaction,10 helping to overcome biases.
OPTIONALITY
Optionality refers to the presence of flexible resources, that can easily be used or converted in case of need. COVID-19 forced healthcare institutions to build optionality that led to flexibility. In China, a brand-new COVID-19 hospital was built in only 10 days, whereas everywhere in the world, former trade fairs and sports facilities were quickly converted into intensive care units (ICUs) and medical centers for COVID-19 patients. In New York, one of the global epicenters of the pandemic, innovative solutions were required to turn operating rooms (ORs) and postanesthesia care units into ICUs.12 In the New York experience, ORs and postanesthesia care units to be converted were selected based on “their size, location, and available infrastructure, while preserving some ORs for emergency surgeries”.12 (p1)
Modern hospital design should include hybrid ORs, meaning ORs that are suitable for multiple medical imaging methods, techniques to be performed simultaneously, team coverage, and quickly convertible in terms of scope (eg, into ICUs) and size (eg, using moving walls). Defining some “pandemic-ready ORs” can also represent a winning strategy.13 Still, the flexibility necessary for optionality goes beyond tangible resources, requiring surgeons to develop dedicated non-technical skills,14 such as change management, adaptability and problem-solving attitudes.
REDUNDANCY
Redundancy refers to the availability of extra stock and resources. As humans have redundancy of some key organs (like the kidneys),1 having unused capacity can help to overcome a crisis. However, accepting redundancy is difficult since “redundancy is ambiguous because it seems like a waste if nothing unusual happens. Except that something unusual happens — usually.”1
The COVID-19 crisis has shown how countries with higher resources performed better. The lack of redundant surgical resources like ICU beds caused the cessation of non-urgent surgical activities, leading to unmet medical needs.2 Understanding and planning the available resources for preoperative, intraoperative and postoperative surgical precautions (including ICU beds, drugs, PPE) is thus strategic.13
Resource monitoring,13 “just in case” stock strategies, and networking among different surgical departments or healthcare institutions2 can help to gather the required resources when needed, enabling institutions to plan the investments on a more comprehensive basis.
BARBELL STRATEGIES
Barbell strategies refer to the ability to reduce the exposure to adverse outcomes, for example, portfolio balancing in finance, which increases the opportunity for gains if the more aggressive investments work, but limits those risks due to the weighing activity. The COVID-19 emergency required surgeons to develop special skills and be trained on the job.2
Education is expensive in terms of money and time, but when needed, the outcome can be strategic. Relationships with private healthcare organizations, universities and research centers, leading to open innovation and technological transfer may help. New paradigms in surgical and emergency education could be rethought, even using online and e-sources.15 Despite the higher management costs, barbell strategies proved to be the winning choice in times of crisis.
HORMESIS STRATEGY
Hormesis is a term describing the beneficial effects of repeated stimulation or stress that ultimately augments an organism's defenses against potentially harmful influences. Organisms that are exposed to toxins tend to overcompensate in their response. The COVID-19 pandemic has highlighted the need for healthcare and surgical professionals to be trained to deal with disasters, no matter what their specialities are; as surgeons often had to change their usual tasks and approach challenging triage decisions.16
Modern clinical education should keep this in mind, not only in medical schools and residency programs but also during lifelong learning plans for surgeons and clinicians in general. Practical educational strategies to help surgeons learn to make difficult triage decisions when resources are scarce may include spending training time in other departments, overseas experiences in resource-poor clinical environments, and whenever possible, employing innovative educational techniques like gaming.15
BALANCING FEEDBACK LOOPS
Focusing on the best practices and lesson learned2 might lead to organizational improvements that work better than highlighting the losses and damages caused by a crisis. The COVID-19 crisis showed that a system strongly focused on efficiency creates specializations generating a loop by which more specialization leads to more efficiency. However, when new challenges are posed, specialization can be tricky. Enhancing open innovation might work as balancing feedback since multidisciplinary experiences are brought together to improve problem-solving. Examples from the COVID-19 era come, for instance, from the case of the Decathlon snorkelling mask converted into a ventilation device for COVID-19 patients or the recently developed open-access project for mechanical lung ventilator based on simple design and easy-to-find components that can be produced anywhere with a rapid manufacturing process. A multidisciplinary approach is also recommended in surgery, as highlighted by experiences like the COVID-19 Bundled Response for Access team of the Massachusetts General Hospital.17
The hybrid role of medical doctors has inspired the establishment of new clinical curricula, like the Technical Medicine one for Technical Physicians.18 The multidisciplinary nature of the various stakeholders involved increases the need for effective knowledge translation tools19 to allow the transfer, sharing and creation of new knowledge.
CONCLUSIONS AND FUTURE PERSPECTIVES
The COVID-19 crisis has revealed how many communities across the globe were unprepared for the unpredictable chaos that emerges from black swan events, even when people had engaged in pre-disaster planning.20 The central lesson learned is that the healthcare systems of many countries were set to handle typical situations but not the chaos of a black swan event. A different approach is required both for allowing the long-term recovery and for preventing similar circumstances from happening again. The adverse outcomes of the COVID-19 pandemic must be the starting point for a reorganization of the entire healthcare system to prevent such deleterious impacts in the future and thereby not to let the crisis be wasted.
Planning for long-term recovery seems a challenging task when there are pressing humanitarian, reorganization, and rebuilding needs to address. The speed and the quality of recovery matter. Applying an interdisciplinary approach, which includes crisis management, to an understanding of resources is challenging, given the complexities of delivering health care in a modern hospital. Still, it is essential for healthcare and surgical systems to overcome the COVID-19 crisis stronger than before, being inspired by an antifragile perspective. Through the application of the above-described management principles, an antifragile standpoint can be successfully applied to surgical departments. A call for an interdisciplinary decision-making process becomes imperative in the current transition phase to prioritize and better distribute resources to allow for full recovery.
Footnotes
L.C. and F.D.M. share the first authorship.
The authors declare no conflict of interest.
REFERENCES
- 1.Taleb NN. Antifragile: Things That Gain from Disorder. New York: Penguin Random House LLC; 2012. [Google Scholar]
- 2.Cobianchi L, Pugliese L, Peloso A, et al. To a new normal: surgery and COVID-19 during the transition phase. Ann Surg 2020; 272:e49–e51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Derbyshire J, Wright G. Preparing for the future: development of an “antifragile” methodology that complements scenario planning by omitting causation. Technol Forecast Soc Change 2014; 82:215–225. [Google Scholar]
- 4.O'sullivan ED, Schofield SJ. Cognitive bias clinical medicine. J R Coll Physicians Edinb 2018; 48:225–232. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Alamino JM. Human biases and the SARS-CoV-2 pandemic. Intensive Crit Care Nurs 2020; 58:102861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Guardian. Lost in the Frontline. The Guardian. Available at: https://www.theguardian.com/us-news/series/lost-on-the-frontline. Published 2020. Accessed July 2, 2020. [Google Scholar]
- 7.The Royal College of Surgeons of England. Avoiding Unconscious Bias A Guide for Surgeons. London: The Royal College of Surgeons of England; 2015. Available at: https://www.rcseng.ac.uk/library-and-publications/rcs-publications/docs/avoiding-unconscious-bias/. Accessed May 18, 2020. [Google Scholar]
- 8.Bonner SN, Wakam GK, Kwayke G, et al. Covid-19 and racial disparities: moving towards surgical equity. Ann Surg 2020; doi: 10.1097/SLA.0000000000004111. [epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qadan M, Hong TS, Tanabe KK, et al. A multidisciplinary team approach for triage of elective cancer surgery at the massachusetts general hospital during the novel coronavirus COVID-19 outbreak. Ann Surg 2020; 272:e20–e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.ASA. Ensuring Equity, Diversity, and Inclusion in Academic Surgery. Beverly (MA): American Surgical Association; 2018. [DOI] [PubMed] [Google Scholar]
- 11.Gardner AK, Harris TB. Beyond numbers: achieving equity, inclusion, and excellence. Ann Surg 2020; 271:425–426. [DOI] [PubMed] [Google Scholar]
- 12.Peters AW, Chawla KS, Turnbull ZA. Transforming ORS into ICUs. N Engl J Med 2020; 382:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liang ZC, Seng Ye Chong M, Ka Po Liu G, et al. COVID-19 and elective surgery: 7 practical tips for a safe, successful and sustainable reboot. Ann Surg 2020; doi: 10.1097/SLA.0000000000004091. [epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yule S, Smink DS. Non-technical skill countermeasures for pandemic response. Ann Surg 2020; doi:10.1097/SLA.0000000000004107 (In press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garcia Vazquez A, Verde JM, Dal Mas F, et al. Image-guided surgical e-learning in the post-COVID-19 pandemic era: what is next? J Laparoendosc Adv Surg Tech 2020; In Press. doi: 10.1089/lap.2020.0535. [epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 16.Brindle ME, Doherty G, Lillemoe K, et al. Approaching surgical triage during the COVID-19 pandemic. Ann Surg 2020; 272:e40–e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Albutt K, Luckhurst CM, Alba GA, et al. Design and impact of a COVID-19 multidisciplinary bundled procedure team. Ann Surg 2020; 272:e72–e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Groenier M, Pieters JM, Miedema HAT. Technical medicine: designing medical technological solutions for improved health care. Med Sci Educ 2017; 27:621–631. [Google Scholar]
- 19.Dal Mas F, Biancuzzi H, Massaro M, et al. Adopting a knowledge translation approach in healthcare co-production. A case study Manag Decis 2020; doi:10.1108/MD-10-2019-1444. (In Press). [Google Scholar]
- 20.Event 201. Event 201. Johns Hopkins Center for Health Security. Published 2020. Available at: https://www.centerforhealthsecurity.org/event201/. Accessed May 13, 2020. [Google Scholar]


