The main manifestation of the coronavirus disease 2019 (COVID-19) is the viral pneumonia, but several manifestations have been also observed in the cardiovascular system. Therefore, a higher risk of cardiac arrhythmias is not unexpected in patients with COVID-19, but data are scant.1,2
We investigated the arrhythmic complications in all patients hospitalized for COVID-19 pneumonia at the Intensive Care Unit or the general Medicine Department of our Institution between April 1 and April 26, 2020. This analysis was approved by the Institutional Review Committee, and subjects gave informed consent. The data that support the findings of this study are available from the corresponding author upon reasonable request.
We collected baseline characteristics, laboratory findings, and therapy. All patients were on continuous telemetry during hospitalization. New diagnosis of atrial fibrillation (AF) lasting >30 s, atrial tachycardia lasting >30 s, sustained (>30 s), or nonsustained (>3 beats) ventricular tachycardia and symptomatic bradycardia requiring permanent cardiac pacing that occurred during hospitalization were verified. A daily ECG was also analyzed to measure corrected QT interval (cQT) and evaluate its potential prolongation (cQT>500 ms).
Continuous variables were reported as mean±SD or median (interquartile range). Categorical data were expressed as number (percentage) and proportion of patients reported with the 95% CI. Variables were compared using the Fisher exact or the Mann-Whitney U test as appropriate.
The cohort included 30 patients (33% female; mean age 75.2±9.5 years). Baseline characteristics are reported in Table. Three patients (10%) did not undergo any specific pharmacological treatment and 2 (7%) needed only antibiotic therapy. Hydroxychloroquine was largely used (n=25, 83%): alone (n=9, 30%), combined with antiviral drugs (n=14, 46%), or in few cases with antiviral and azithromycin (n=2, 7%). During hospitalization, the mean value of cQT was 454±44 ms. Five cases (17%) of cQT>500 ms were observed, but only in 1 patient (3%), this led to therapy modification.
Table.
Patients Characteristics at Hospital Admission, Findings, Therapy, and Outcomes During Hospitalization by Occurrence of New-Onset Cardiac Arrhythmias
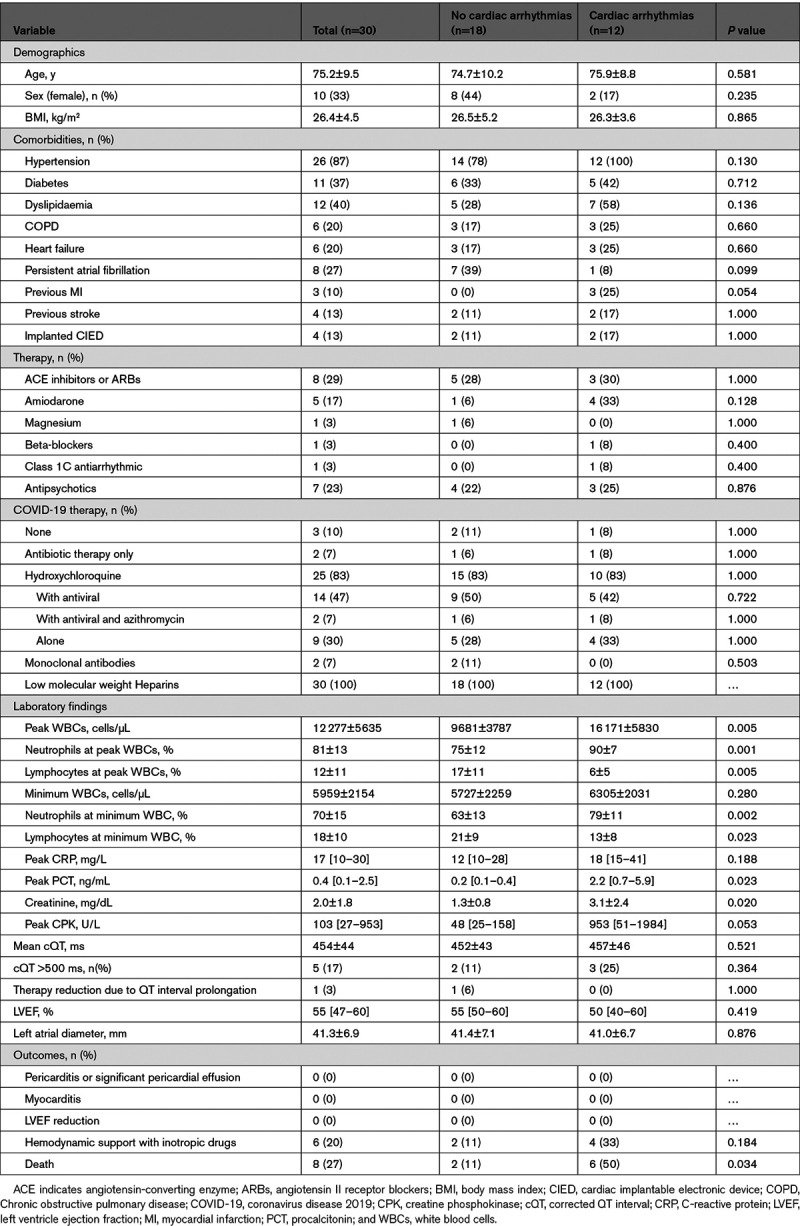
In 12 patients (40%), we observed new diagnosis of cardiac arrhythmia during hospital stay. Among 22 patients in sinus rhythm at admission, the proportion of new-onset AF was 45% (95% CI, 23%–68%). Episodes of atrial tachycardia were also recorded in 2 patients with AF (9%, 95% CI, 1%–29%). Recurrent nonsustained ventricular tachycardias were also detected in 2 patients without AF (7%, 95% CI, 1%–22%). We did not observe any sustained ventricular tachycardia or symptomatic bradycardia.
Although similar baseline characteristics, patients with new-onset cardiac arrhythmia had higher value of peak white blood cells, higher presence of neutrophils, and higher value of peak CRP (C-reactive protein) and CPK (creatine phosphokinase).
A total of 8 patients (27%) died during hospitalization. Mortality was higher in patients who experienced new-onset cardiac arrhythmia (50% [95% CI, 21%–79%] versus 11%[95% CI, 1%–35%], P=0.034). The reason for death was acute respiratory distress syndrome (n=7, 87%), except for one cardiogenic shock in infective endocarditis.
Although myocardial injury and elevation of TnT (troponin T) levels have been observed in some studies during COVID-19 hospitalization, data on the prevalence of cardiac arrhythmias are scant. A study on 138 patients from Wuhan, China, reported that 16.7% of hospitalized and 44.4% of intensive care unit patients with COVID-19 had arrhythmias without further details.3 Guo et al4 stratified 187 patients by elevated TnT levels and found more frequent ventricular arrhythmias in the group with high TnT (11.5% versus 5.2%). Kochav et al2 described case reports of high-grade atrioventricular block, AF onset, and polymorphic ventricular tachycardia. In our registry, 40% of patients developed new-onset arrhythmias during hospitalization. Interestingly, AF was very common with a prevalence of 45% considering patients without AF history. We found that patients with arrhythmias had higher inflammatory markers, such as peak white blood cells, CRP, and CPK, suggesting a more extended inflammatory stress that probably also affected the cardiovascular system. In-hospital mortality was also found significantly higher in these patients (50% versus 11%). With the limited number of patients, our findings should be considered as preliminary observations that need to be confirmed in larger controlled studies.
Many causes should probably call into question: sepsis, neurohormonal and inflammatory stress, fever, abnormal metabolism, hypoxia, anxiety, and concomitant pharmacological therapy.
Patients with cardiovascular disease could particularly suffer the infection due to the imbalance between inflammatory increase and reduced cardiac reserve. More in general, other mechanisms, such as ACE (angiotensin-converting enzyme) 2–related downregulation, cytokine storm, and hypoxemia, could trigger arrhythmias in patients without history of cardiovascular disease.1
Side effects of drugs for COVID-19 treatment could also play a role. The use of hydroxychloroquine (or chloroquine), azithromycin, and antiviral drugs could cause prolongation of the QT interval with an increased risk of arrhythmias. We observed cQT prolongation in 5 patients (17%), similar to a previous study,5 but no sustained ventricular tachycardias were observed.
In our small cohort of consecutive patients hospitalized for COVID-19 pneumonia and continuously monitored using telemetry, new-onset cardiac arrhythmias were frequent, particularly AF. Further studies should focus on COVID-19 arrhythmogenic effects and close heart rhythm monitoring after hospital discharge could be advisable to detect potential silent arrhythmias.
Sources of Funding
None.
Disclosures
D. Giacopelli is employee of BIOTRONIK Italia. The other authors report no conflicts.
Footnotes
Nonstandard Abbreviations and Acronyms
- ACE
- angiotensin-converting enzyme
- AF
- atrial fibrillation
- COVID-19
- coronavirus disease 2019
- CPK
- creatine phosphokinase
- cQT
- corrected QT interval
- CRP
- C-reactive protein
- TnT
- troponin T
For Sources of Funding and Disclosures, see page 1389.
Contributor Information
Filippo Placentino, Email: filippo.placentino@gmail.com.
Jacopo Colella, Email: jacopocolella89@gmail.com.
Francesca Pesce, Email: francescapesce.fp@gmail.com.
Antonino Pardeo, Email: antonino.pardeo@gmail.com.
Pasquale Filannino, Email: pasfil@libero.it.
Paolo Artale, Email: paolo.sorrenti@alice.it.
Dalila Desiro, Email: dalila.desiro@gmail.com.
Paolo Sorrenti, Email: paolo.sorrenti@alice.it.
Giuseppe Campagna, Email: g.champagna@gmail.com.
Gennaro Fabiano, Email: fabianogennaro@gmail.com.
Gianluca Peluso, Email: gianlucapeluso.tc@gmail.com.
Daniele Giacopelli, Email: apetretta@gvmnet.it, daniele.giacopelli@biotronik.com.
References
- 1.Kochi AN, Tagliari AP, Forleo GB, Fassini GM, Tondo C. Cardiac and arrhythmic complications in patients with COVID-19. J Cardiovasc Electrophysiol. 2020;31:1003–1008. doi: 10.1111/jce.14479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kochav SM, Coromilas E, Nalbandian A, Ranard LS, Gupta A, Chung MK, Gopinathannair R, Biviano AB, Garan H, Wan EY. Cardiac arrhythmias in COVID-19 infection. Circ Arrhythm Electrophysiol. 2020;13:e008719. doi: 10.1161/CIRCEP.120.008719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jain S, Workman V, Ganeshan R, Obasare ER, Burr A, DeBiasi RM, Freeman JV, Akar J, Lampert R, Rosenfeld LE. Enhanced electrocardiographic monitoring of patients with Coronavirus Disease 2019. Heart Rhythm. 2020;17:1417–1422 [DOI] [PMC free article] [PubMed] [Google Scholar]


