Abstract
Objective:
This study aims to show how full-time telemedicine adoption has impacted patient visit volume and attendance in a comprehensive metabolic and weight loss center.
Summary Background Data:
Elective surgical practices have been profoundly impacted by the global COVID-19 pandemic, leading to a rapid increase in the utilization of telemedicine. The abrupt initiation of audio-video telehealth visits for all providers of a multidisciplinary clinic on March 19th 2020 provided unique circumstances to assess the impact of telemedicine.
Methods:
Data from the clinical booking system (new patient and follow-up visits) for all clinical provider types of the multidisciplinary metabolic center from the pre-telehealth, post-telehealth, and a 2019 comparative period were retrospectively reviewed and compared. The primary outcome is the change in patient visit volume for all clinical providers from before to after the initiation of telemedicine for both new patient, and follow-up visits.
Results:
There were a total of 506 visits (162 new patient visits, and 344 follow-ups) in the pre-telehealth period, versus 413 visits (77 new patient visits, and 336 follow-ups) during the post-telehealth period. After telehealth implementation, new visits for surgeons decreased by 75%. Although follow-up visits decreased by 55.06% for surgeons, there was an increase by 27.36% for advanced practitioners. When surgeons were separated from other practitioners, their follow-up visit rate decrease by 55.06%, compared to a 16.08% increase for the group of all other practitioners (P < 0.0001). Dietitians experienced higher rates of absenteeism with new patient visits (10.00% vs 31.42%, P = 0.0128), whereas bariatricians experienced a decrease in follow-up visit absenteeism (33.33% vs 0%, P = 0.0093).
Conclusions:
Although new patient visit volume fell across the board, follow-up visits increased for certain nonsurgical providers. This provides a template for adoption of a multidisciplinary telehealth clinic in a post-pandemic world.
Keywords: COVID-19, multidisciplinary clinic, telemedicine
The COVID-19 pandemic has dramatically altered the inpatient and outpatient care of surgical patients. Although emergency surgeries continued, the immediate impact on elective surgical practices was profound, with the American College of Surgeons and other organizations publishing guidelines on how to stratify elective surgery patients.1 Additionally, outpatient interactions for patients and providers have changed. Providers had to rapidly adjust to utilization of telemedicine to maintain access and continuity of care, while minimizing potential disease transmission.2
Telemedicine with video technology was first utilized in the late 1950s for long-distance psychiatric services. However, its widespread employment was not seen until the 1990s when there was a recognized need to serve rural communities.3 Telemedicine can be seen in almost any specialty today and has shown promising results in treating patients with chronic diseases such as congestive heart failure and diabetes mellitus.4,5 However, no strong consensus exists regarding the effectiveness of telemedicine, particularly in surgical fields. Questions remain regarding its efficacy in improving patient health, cost-effectiveness, and user satisfaction, as different institutions continued to have mixed results when studying the use of telemedicine in their practices.6,7
Surgical clinics have implemented the use of telehealth for a diverse set of surgical patients in a variety of patient encounter types.8,9 Adoption of the platform has steadily grown, as for example, Nandra et al8 described 655 patient encounters over a 10-month period for a single department of surgery.
Bariatric surgical practices are relatively unique in the surgical world due to the multidisciplinary nature of the care teams and frequent visits in the pre- and postoperative time periods. Preoperative care often includes visits with a surgeon, a psychological assessment, and evaluation by a registered dietician. Postoperative care with the multidisciplinary team is lifelong. Education and support from health care providers are significant factors in the preoperative and postoperative achievement of weight loss and adherence to new lifestyle regimens.10 In addition, adherence to follow-up appointments is associated with improved weight loss and comorbidity control.11,12 Few studies have been done to assess the feasibility and effectiveness of incorporating telehealth specifically for preoperative and postoperative bariatric patients. One study used teleconsultation for pre- and post-bariatric surgery patients living remotely from their bariatric surgery center, whereas another matched case–control study compared telehealth to in-person visits.13,14
The COVID-19 global pandemic has created a unique situation where outpatient surgical practices are forced into adopting alternatives to in-person visits to continue patient care and minimize exposures. Herein, the authors aim to show how the COVID-19 pandemic and the subsequent rapid conversion to a full-time telemedicine practice has impacted patient visit volume and attendance in a comprehensive metabolic and weight loss center.
METHODS
A retrospective descriptive review was conducted of all synchronous audio-video telehealth visits performed in a Comprehensive metabolic and weight loss center with a large academic bariatric surgery practice from February 19th 2020 through April 16th 2020, and from March 19th 2019 to April 16th 2019. Data from the clinical booking system for surgeons, bariatricians, psychologists, advanced practitioners (nurse practitioners and physician's assistants), and registered dietitians was extracted.
The pre-telehealth time period was defined as February 19th 2020 to March 18th 2020, and the post-telehealth time period was defined as March 19th 2020 to April 16th 2020. These time periods include 4 weeks on either side of the adoption of Telehealth inflection point of March 19th 2020. A comparative time period was used and was defined as March 19th, 2019 to April 16th, 2019. New patient visits were defined as the initial consultation with a patient and a certain practitioner. Follow-up visits included all visits after the initial consultation, including: additional preoperative visits, postoperative visits, and additional follow-up visits. Bariatric follow-up “group” visits in the post-telehealth time period were conducted as one-on-one phone calls with a provider, with educational material mailed to the patient.
Telehealth Adoption
Before initiation of virtual visits, all patients were first contacted by mail to alert them of the change in visit type. One to 2 days before a patient's virtual visit, the patient was contacted by phone to review the audio-visual platform, and to provide technological support.
Primary and Secondary End Points
Primary end points included the change in patient visit volume for multiple practitioner types from the pre-telehealth period to the post-telehealth period for both new patient visits and follow-up visits. An additional primary end point was the change in no-show rates for multiple practitioner types from the pre-telehealth period to the post-telehealth period for both new patient visits and follow-up visits. From an operations management approach, no-show visits can negatively impact the efficiency of clinic, and require additional time-effort in attempts to reach and reschedule, with limited or no reimbursement for such time-effort. In addition, no-show visits are the sign of low compliance with follow-up care, which has significant negative implications for bariatric surgery patients.11,12 Secondary endpoints include the change in patient visit volume for multiple practitioner types from the comparative time period to the post-telehealth period for both new patient visits and follow-up visits. An additional secondary endpoint was the change in patient visit volume for surgeons, and for all other practitioners from the pre-telehealth period to the post-telehealth period for both new patient visits and follow-up visits.
Analysis
Statistical analyses were performed using a 2-sided chi-square test. A significance level of 0.05 for 2-sided comparisons was considered statistically significant. This study was approved by the Institutional Review Board at the authors’ institution.
RESULTS
Patient Visit Volume
There were a total of 506 visits (162 new patient visits, and 344 follow-ups) during the pre-telehealth period from February 20th 2020 to March 18th 2020 for all providers in the multidisciplinary clinic. In comparison, there were a total of 413 visits (77 new patient visits, and 336 follow-ups) during the post-telehealth implementation period from March 19th 2020, to April 16th 2020 for all providers. Total visits by type are shown in Table 1. Also included in Table 1 are total visit numbers for the comparative time period from 2019 (Table 1).
TABLE 1.
Volume of Patient Visits Across Practitioner Type in the Pre- and Post-Telehealth Adoption Time Periods, and the 2019 Comparative Period
| 2019 Comparative Period | 2020 Pre-Telehealth | 2020 Post-Telehealth | ||||
| New Visits (n = 144) | Follow-Ups (n = 301) | New Visits (n = 162) | Follow-Ups (n = 344) | New Visits (n = 77) | Follow-Ups (n = 336) | |
| Surgeons | 59 | 65 | 68 | 89 | 17 | 40 |
| Bariatrician | 8 | 4 | 8 | 6 | 3 | 18 |
| Psychologist | 30 | 15 | 35 | 13 | 32 | 17 |
| Advanced Practitioners | 0 | 102 | 6 | 106 | 1 | 135 |
| Registered Dietitians | 47 | 115 | 45 | 130 | 24 | 126 |
“Visit” denotes either that the patient attended an in-person clinic, or a telehealth visit. i.e. Not a “no-show.”
For new patient visits, surgeons saw a 75% decrease in volume from the pre-telehealth to post-telehealth period, compared to only an 8.57% decrease in volume for the psychologist. Additional new patient volume decreased by 62.5% for the bariatrician, 83.33% for the advanced practitioners, and 46.67% for the dietitians. Follow-up visit volume showed demonstrably different rates of change. Notably, surgeons experienced a 55.1% decrease in follow-up visit volume, whereas the advanced practitioners saw a 27.4% increase in volume. Additionally, the psychologist saw a 30.77% increase in volume, the advanced practitioners saw a 27.36% increase in volume, and the dietitians saw a 3.08% decrease in volume.
When surgeon volume is separated, and compared to the group of other providers as a whole, stark differences are noted. For new patient visits, although there is a 75% decrease in volume for the surgeons (68 vs 17), the group of all other providers experienced a 36.17% decrease (94 vs 60) (P = 0.0027). Furthermore, for follow-up visits, the 55.1% decrease (89 vs 40) in volume that the surgeons’ experienced was contrasted by the 16.08% increase (255 vs 296) (P < 0.0001) in visits by all other providers. These data appear graphically in Figure 1. Bariatric educational “group” support classes saw a 9.45% decline in visit volume (127 vs 115).
FIGURE 1.
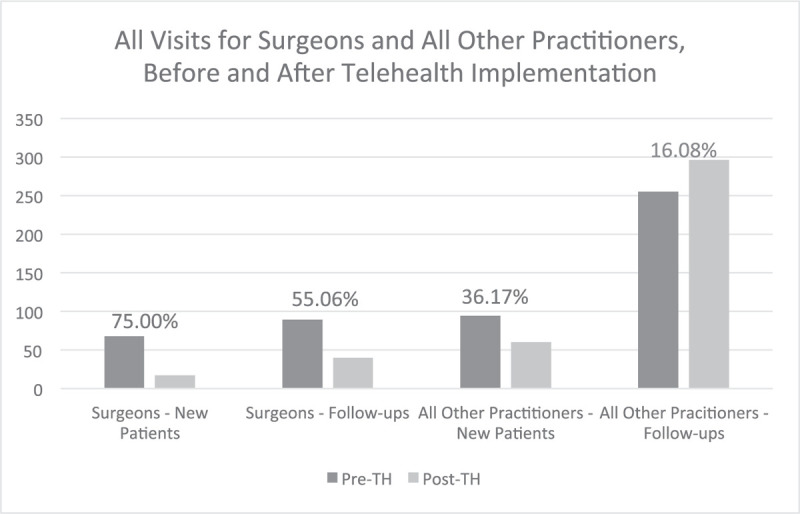
All visit type volume and rates before and after telehealth implementation for surgeons and nonsurgeons. Red text indicates a decreasing rate, whereas green text indicates an increasing rate.
Absenteeism (“No-Shows”)
The rate of no-shows for new patients, and follow-up visits in the pre- and post-telehealth implementation periods are shown in Table 2. Of note, the dietitians experienced a higher rate of no-shows with new patient visits (10% vs 31.4%, P = 0.0128) in the post-telehealth implementation time period. Additionally, with a small volume of patients, the bariatrician experienced a lower rate of follow-up visit no-shows (33.33% vs 0%, P = 0.0093) in the post-telehealth period. The bariatric group visit no-show rate decreased after telehealth implementation, but was not statistically significant (16.45% vs 11.54%, P = 0.2388).
TABLE 2.
Attendance at Appointments for Various Practitioners Before and After Telehealth Implementation for New Visits and Follow-Up Visits
| No-Show Rate for New Visits and Follow-Up Visits before and After Telehealth | |||
| New Visits Pre-TH, n (%) | New Visits Post-TH, n (%) | P | |
| Surgeons | 11 (13.92%) | 3 (15.05%) | 0.9025 |
| Bariatrician | 2 (20%) | 0 (0%) | 0.3998 |
| Psychologist | 9 (20.45%) | 9 (21.95%) | 0.8671 |
| Advanced Practitioners | 0 (0%) | 0 (0%) | 1.0000 |
| Registered dietitians | 5 (10%) | 11 (31.42%) | 0.0128 |
| Follow-Up Visits Pre-TH, n (%) | Follow-Up Visits Post-TH, n (%) | P | |
| Surgeons | 7 (7.29%) | 3 (6.98%) | 0.9496 |
| Bariatrician | 3 (33.33%) | 0 (0%) | 0.0093 |
| Psychologist | 4 (23.53%) | 6 (26.09%) | 0.8537 |
| Advanced Practitioners | 20 (15.87%) | 20 (12.90%) | 0.4786 |
| Registered dietitians | 12 (8.45%) | 13 (9.35%) | 0.7913 |
No-show rate calculated as a percentage of noncompleted visits as it relates to total appointments scheduled. P value <0.05 indicates statistical significance. TH indicates Telehealth.
DISCUSSION
After the conversion of in-person visits to telehealth visits throughout the multidisciplinary outpatient clinic there was a decrease in new patient visits for all practitioners. This is likely multifactorial, as the COVID-19 global pandemic's impact on unemployment and health insurance status has likely led to patients not seeking nonemergent medical care. Additionally, technological limitations may prevent some patients from access to telehealth care. In addition, some patients may elect to defer consultation until an in-person option is available due to convention or preference.
Interestingly, the same cannot be said for follow-up visits, which have increased in virtually all the other specialty providers. Taken together, the other specialty providers saw greater than 16% growth in their follow-up visit volume. Specifically, the bariatrician, the psychologist, and the advanced practitioners all saw an increase in their follow-up visit volume.
The impact of this growth in follow-up volume is particularly noted with the advanced practitioners. Bariatric surgery patients undergo an intensive preoperative workup with multiple visits and require lifelong follow-up to avoid complications and monitor weight loss. Often, as is the case in the authors’ clinic, the burden of this tremendous patient volume falls to the advanced practitioners. These Physicians Assistants and Nurse Practitioners review laboratory work, monitor dietary compliance and food logging, go over medications, address complications, and deal with other patient concerns. The growth in follow-up volume in these advanced practitioners combined with a comparable no-show rate (15.9% vs 12.9%) cannot be overstated. Postoperative attendance rates have been shown to have a positive relationship with weight loss outcomes.11,12,15 Therefore, the ability to capture these patients and ensure stability following bariatric surgery, even in this tumultuous health care landscape, will likely positively impact these patients’ outcomes.
Bariatric group sessions are often employed in the preoperative setting to improve education, provide support, and assess program compliance. Following the rapid adoption of a telemedicine platform for patient visits, there was a slight decrease in visit volume, with a slight increase in attendance. However, these visits were conducted as one-on-one telephone consults, which differs from the in-person group format formally employed, due to the authors’ institution having concerns with privacy for virtual group sessions. Although these visits were not entirely similar, these data do provide some insight into patient commitment during the preoperative process. These are patients who began the bariatric surgery process pre-pandemic, but still attended virtual monthly “group” sessions during the pandemic, and at a similar rate. Long-term follow-up of these patients will reveal whether participation yielded improved outcomes or greater weight loss.
The rates of absenteeism for new visits and follow-ups were relatively stable across practitioner type. Although the dietitians saw an increase in no-show rates for new patient visits, and the bariatrician saw a decrease in follow-up no-show rate, these involve small numbers of visits and are likely not representative of what long-term adoption of telehealth would represent. No show visits can also be minimized by real-time phone call reminders. Patients are able to join a telehealth visit regardless of location.
To establish whether existing patients were more likely to attend their visits than new patients, the authors compared attendance data between new visits and follow-up visits after the adoption of telehealth. This shows an almost 3-fold decrease in no-show rates for surgeons and the registered dietitians in favor of follow-up visits. This suggests that patients who were already enrolled in the bariatric program may have been more likely to attend their virtual visits than patients who were brand new to the program.
The downstream impact of transitioning to telemedicine has been felt acutely, with an increased volume of follow-up visits, but the impact may persist beyond the end of the global pandemic. The adoption of routine telehealth follow-up for certain practitioners and certain patients can have numerous positive impacts as highlighted below. First, patients save time and cost by not having to drive to and from a physical clinic.13,16 Additionally, patients who participate in telehealth may avoid taking time off of work and avoid having to have a person accompany them who also was taken away from personal responsibilities.16,17,18
Practitioner satisfaction and efficiency could improve with the ability to work from home during certain days of the week or limit the travel between various physical clinic sites. This is highlighted with these data with follow-up visits for the bariatrician. The ability to not have to drive from clinic site to clinic site increased the available clinic times for this practitioner, and likely increased her follow-up volume. Similarly, Hwa and Wren reported that using telehealth for postoperative visits instead of in-person clinic made 110 additional clinic slots for new patients over a 10-month period.16,19 Finally, the financial ramifications do not end on the patient side of the equations. Clinical practices that have a growing telemedicine clinic filled with long-term follow-up patients, can decrease physical clinic space over time, leading to financial savings for the health system.16,19
The applicability of telehealth usage is well seen in multidisciplinary practices outside of the bariatric realm, particularly involving cancer care. Grenda et al describe the usage of telemedicine in a Multidisciplinary Lung Cancer Clinic where patients are able to be evaluated by a thoracic surgeon, medical oncologist, and radiation oncologist all in a single visit.20 These authors provide a blueprint for the development and initiation of a multidisciplinary virtual clinic, with a single encounter for the patient mimicking the experience of in-person attendance to a comprehensive cancer center.
The concept of utilizing telehealth in a bariatric surgical clinic is not without challenges. Relying on self-reported weights, and insurance authorization for virtual visits are issues that will need to be addressed. The Centers for Medicare and Medicaid Services have expanded reimbursement and access for telehealth during the pandemic, but this is an issue that will need to be resolved once care returns to normal.20,21 Despite this, the high clinic attendance and undisturbed volume for several types of visits, as illustrated herein, suggest that a long-term change in practice is feasible and likely, even during routine nonpandemic operations. Advanced practitioners, bariatricians, psychologists, and dietitians may transition to telehealth visits for a large segment of our patient population for both new patient visits and follow-up visit. Additionally, surgeons will continue to incorporate telehealth visits for follow-ups as well. These data suggest that other multidisciplinary clinics, including bariatric practices, should strongly consider increased telehealth usage during and at the conclusion of the pandemic.
Limitations
There are several limitations to this study. First, the sample size is quite small, with only 4 weeks of accrued data before and after the adoption of telehealth. With only slightly >400 visits in the weeks before and after adoption, this amount of time is likely not long enough to get a true sense of the trends on patient visits, and absenteeism.
Second, some of the new patient visits in the post-telehealth period could have been scheduled before the adoption of telehealth, which is confounding. This likely falsely elevated the new patient visit volume in the telehealth period, and does not accurately reflect the ability to bring in new patients into clinic on the telehealth platform. However, given the circumstances of the pandemic, the authors are unconcerned with new patient volume at this time, and highlight that the platform is particularly attractive for follow-up visits.
Third, the bariatric group sessions were conducted in a purely audio, one-on-one fashion, which differed dramatically from the pre-health, in-person group sessions. Data on visit volume and attendance are not necessarily reflective of what integrating fully virtual group sessions might look like moving forward.
Fourth, the authors have solely focused on patient visit volume and attendance. Lacking are data on patient clinical outcomes, patient financial implications and satisfaction, and implications to providers and the health system. Additional longer-term follow-up data with these factors are imperative to draw comprehensive conclusions regarding telehealth adoption.
CONCLUSIONS
The abrupt onset of the COVID-19 global pandemic forced a dramatic shift from in-person clinic visits to entirely virtual telehealth clinics in a comprehensive, multidisciplinary, bariatric clinic. Although new patient visit volume decreased across the board, follow-up visits increased for certain nonsurgical providers, providing a template for adoption of a multidisciplinary telehealth clinic in a post-pandemic world.
Footnotes
A.D.P. is a speaker Ethicon, Medtronic, Stryker, and Gore; receives grants from Baranova, and from Obalon, all of which are unrelated to the submitted work. K.S. receives speaker honorarium from Gore, has received research grants from Merck, and is on the Advisory board from Biom Up, all of which are unrelated to the submitted work. All other authors have nothing to disclose.
The authors report no conflicts of interest.
REFERENCES
- 1.Stahel PF. How to risk-stratify elective surgery during the COVID-19 pandemic? Patient Saf Surg 2020; 14:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 2020; [epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perednia DA, Allen A. Telemedicine technology and clinical applications. JAMA 1995; 273:483–488. [PubMed] [Google Scholar]
- 4.Weinstein RS, Lopez AM, Joseph BA, et al. Telemedicine, telehealth, and mobile health applications that work: opportunities and barriers. Am J Med 2014; 127:183–187. [DOI] [PubMed] [Google Scholar]
- 5.Lobodzinski SS, Jadalla AA. Integrated heart failure telemonitoring system for homecare. Cardiol J 2010; 17:200–204. [PubMed] [Google Scholar]
- 6.Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform 2010; 79:736–771. [DOI] [PubMed] [Google Scholar]
- 7.Wootton R. Twenty years of telemedicine in chronic disease management–an evidence synthesis. J Telemed Telecare 2012; 18:211–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nandra K, Koenig G, DelMastro A, et al. Telehealth provides a comprehensive approach to the surgical patient. Am J Surg 2019; 218:476–479. [DOI] [PubMed] [Google Scholar]
- 9.Barsom EZ, Jansen M, Tanis PJ, et al. Video consultation during follow up care: effect on quality of care and patient-and provider attitude in patients with colorectal cancer. Surg Endosc 2020; [epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coldebella B, Armfield NR, Bambling M, et al. The use of telemedicine for delivering healthcare to bariatric surgery patients: a literature review. J Telemed Telecare 2018; 24:651–660. [DOI] [PubMed] [Google Scholar]
- 11.Spaniolas K, Kasten KR, Celio A, et al. Postoperative follow-up after bariatric surgery: effect on weight loss. Obes Surg 2016; 26:900–903. [DOI] [PubMed] [Google Scholar]
- 12.Schwoerer A, Kasten K, Celio A, et al. The effect of close postoperative follow-up on co-morbidity improvement after bariatric surgery. Surg Obes Relat Dis 2017; 13:1347–1352. [DOI] [PubMed] [Google Scholar]
- 13.Sudan R, Salter M, Lynch T, et al. Bariatric surgery using a network and teleconferencing to serve remote patients in the Veterans Administration Health Care System: feasibility and results. Am J Surg 2011; 202:71–76. [DOI] [PubMed] [Google Scholar]
- 14.Wang CD, Rajaratnam T, Stall B, et al. Exploring the effects of telemedicine on bariatric surgery follow-up: a matched case control study. Obes Surg 2019; 29:2704–2706. [DOI] [PubMed] [Google Scholar]
- 15.Kaiser KA, Franks SF, Smith AB. Positive relationship between support group attendance and one year postoperative weight loss in gastric banding patients. Surg Obes Relat Dis 2011; 7:89–93. [DOI] [PubMed] [Google Scholar]
- 16.Gunter RL, Chouinard S, Fernandes-Taylor S, et al. Current use of telemedicine for post-discharge surgical care: a systematic review. J Am Coll Surg 2016; 222:915–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Viers BR, Lightner DJ, Rivera ME, et al. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol 2015; 68:729–735. [DOI] [PubMed] [Google Scholar]
- 18.Sathiyakumar V, Apfeld JC, Obremskey WT, et al. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: a pilot study. J Orthop Trauma 2015; 29:e139–e145. [DOI] [PubMed] [Google Scholar]
- 19.Hwa K, Wren SM. Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery: results of a pilot program. JAMA Surg 2013; 148:823–827. [DOI] [PubMed] [Google Scholar]
- 20.Grenda TR, Whang S, Evans NR., III Transitioning a surgery practice to telehealth during COVID-19. Ann Surg 2020; 272:e168–e169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Medicare and Medicaid Services. Medicare Telemedicine Health Care Provider Fact Sheet. Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. 2020. Accessed May 6, 2020. [Google Scholar]


