Abstract
Background:
Acute mountain sickness (AMS) is the effect when people accessing high altitude in a short period of time. As a cyclooxygenase (COX) inhibitor, ibuprofen could alleviate the symptoms of AMS. However, whether it can prevent AMS or not is still controversial. It is necessary to perform a meta-analysis to evaluate the role of ibuprofen in AMS prophylaxis.
Methods:
PubMed, EMBASE, Medline, ISI Web of Science, Cochrane Library, China National Knowledge Infrastructure (CNKI) will be searched for the relevant published studies that explored the value of ibuprofen in AMS prophylaxis from inception to October 2020. The data will be independently extracted by 2 researchers. Risk of bias will be evaluated based on Cochrane risk of bias assessment tool. Heterogeneity among the included studies will be evaluated by χ2 and I2 values. The meta-analysis was conducted by RevMan software version 5.3.
Results:
This study will evaluate the role of ibuprofen in AMS prophylaxis.
Conclusion:
This study will summarize the current evidence of ibuprofen in AMS prophylaxis, which could further guide the recommendation in prevention of AMS.
Open Science Framework (OSF) registration number: October 8, 2020. osf.io/n3mjt.
Keywords: acute mountain sickness, ibuprofen, prophylaxis, systematic review, meta-analysis
1. Background
Acute mountain sickness (AMS) is the effect when people accessing high altitude (>2500 meters) in a short period of time, which is characterized by a group of symptoms such as headache, fatigue, shortness of breath, dizziness, nausea and vomiting, diarrhea, disturbed sleep, et al.[1,2] Also, it might progress to encephaledema or pneumonedema,[3,4] which are life-threatening medical conditions. The pathogenesis of AMS is not well understood. Until now, limited drugs are recommended to AMS prophylaxis.[5–7] Acetazolamide, which is a carbonic anhydrase inhibitor, has been proven to prevent AMS in a large number of studies.[8,9] Due to the certain side effects such as gastrointestinal reactions, abnormal urination and electrolyte disorders,[10–12] it is not suitable for certain people. Dexamethasone, which is a long-acting glucocorticoid, can also prevent and alleviate the symptoms of AMS.[13] But it is not suitable for people with hypertension or diabetes mellitus.[14] New therapeutic agents are urgently needed.
Recently, emerging data showed that hypoxia was associated with inflammation.[15,16] Also our data shows that AMS is related to elavated inflammatory cytokines (Hai Yi, MD, unpublished data, October 2020), indicate that inflammation might mediate the pathophysiology of AMS. When expose to hypoxia, the arachidonic acid (AA) metabolism pathway was excessively enhanced.[17] Cyclooxygenase (COX) inhibitor ibuprofen could effectively target AA pathway and alleviate the symptoms of AMS.[15,18,19] However, whether it can prevent AMS or not is still controversial.[20] It is necessary to perform a meta-analysis to evaluate the role of ibuprofen in AMS prophylaxis.
2. Methods
2.1. Study registration
The protocol of the systematic review has been registered. Registration: OSF registration. October 8, 2020. URL: https://osf.io/n3mjt. It has been reported following the guideline of Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocol statement.
2.2. Ethics
This study is a systematic review; the outcomes are based on the published evidence, so examination and agreement by the ethics committee are not required. We plan to publish the results in a journal or conference presentation.
2.3. Eligibility criteria
2.3.1. Type of study
This review will include randomized controlled trials of ibuprofen for AMS prevention. Language is limited in English and Chinese. Non-RCTs, observational studies, case reports, crossover studies and laboratory studies will be excluded.
2.3.2. Participants
We will include participants of 18 years or older, of any sex and ethnicity. All the participants following rapid ascent (in 3 days) to a high altitude (>2500 meters) were assessed the systems of AMS, according to the Lake Louise criteria.[21] The participants who had underlying diseases or complications would be excluded.
2.3.3. Interventions
The experiment group use ibuprofen, with no limit of dose and frequency. Any other drug could not be used. The control group use other medicine, placebo or none.
2.3.4. Outcome measurements
Our primary objective was to assess the effect of ibuprofen in AMS prophylaxis. The symptoms of AMS were assessed using the Lake Louise criteria[21] or Alternative methods,[22] such as the Environmental Symptoms Questionnaire, Symptom Questionnaire of AMS, General High-Altitude Questionnaire (GHAQ), or clinical examination, for instance, peripheral oxygen saturation.
2.4. Data sources and search strategy
A literature search will be performed in PubMed, Medline, EMBASE, Cochrane Library, Web of Science and CNKI from their inception to October 10, 2020. We will limit our search in English and Chinese. The search strategy of Medline was shown in Table 1. Other electronic databases will be used by the similar retrieval strategy.
Table 1.
Search strategy applied in MEDLINE database.
| Number | Search terms |
| 1 | acute mountain sickness |
| 2 | acute mountain illness |
| 3 | acute mountain headache |
| 4 | altitude headache |
| 5 | altitude sickness |
| 6 | high altitude cerebral edema |
| 7 | high altitude pulmonary edema |
| 8 | encephaledema |
| 9 | pneumonedema |
| 10 | or 1–9 |
| 11 | ibuprofen |
| 12 | randomized controlled trial |
| 13 | controlled clinical trial |
| 14 | single blind |
| 15 | double blind |
| 16 | clinial trials |
| 17 | RCT |
| 18 | or 12–17 |
| 19 | 10 and 11 and 18 |
2.5. Data collection and analysis
2.5.1. Studies selection
Two reviewers (HY and KW) will preliminarily screen the titles and abstracts independently. Then, the full text of the relavant studies will be downloaded for further selection according to the inclusion criteria. Any disagreements will be discussed and agreement will be reached. However, if a consensus can not be made, a third researcher (XG) will make the final decision. The selection process is displayed in the PRISMA flow chart (Figure 1).
Figure 1.
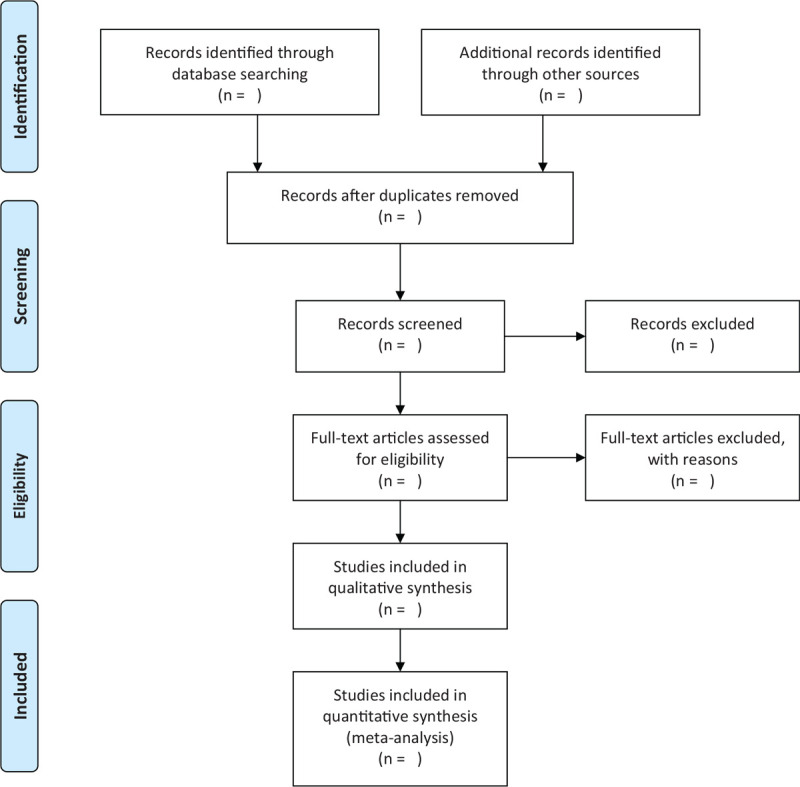
Flow chart of the study selection. This figure shows the Identification, Screening, Eligibility and Included when we searching articles.
2.5.2. Data extraction and management
Two reviewers will extract the data independently using a standardized excel form and confirm by a third researcher. The following items will be extracted: first author, year of publication, regions, sample size, sample types, year of data collection, ages, genders and ethnicity of participants, intervention of control group, dose and frequency of intervention, adverse effects. If there is missing information, we will contact the corresponding author for more details.
2.5.3. Assessment of risk of bias in included studies
Two reviewers will assess the risk of bias of included studies independently by using the Cochrane risk of bias assessment tool.[23] The following items, random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias, are judged to be low-risk grade, high-risk grade and unclear grade. Two reviewers will assess the risk of bias independently and any disagreements between the 2 reviewers will be resolved by a discussion of all reviewers.
2.5.4. Dealing with missing data
If the relevant data in the study is incomplete, the reviews will contact the corresponding author via email for more information. If the missing data cannot be obtained, sensitivity analysis will be conducted to evaluate the impact of missing data on the conclusions of the study.
2.5.5. Data analysis
The RevMan 5.3 software (The Cochrane Collaboration) was used for statistical analysis. The heterogeneity was determined by χ2 and I2 values. If there is no heterogeneity (I2 < 50%, P > .05), the data are synthesized by fixed-effects model; otherwise, the random-effects model would be considered.[13] An unadjusted odds ratios (OR) with 95% confidence intervals (CI) was used to evaluate the effect between the 2 groups.
2.5.6. Subgroup analysis
If the results of the studies are heterogeneous, a subgroup analysis will be conducted to investigate the differences in age, gender, race, altitude, dose and frequency of ibuprofen, et al.
2.5.7. Sensitivity analysis
In order to determine the stability of study finding, sensitivity analysis will be performed.
2.5.8. Publication bias assessment
If no few than 10 studies were included, funnel plots will be used to assess publication bias.[13]
2.5.9. Grading the quality of evidence
The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) will be used to assess the quality of evidence. The quality of evidence will be indicated as high, moderate, low, and very low. Disagreements between the 2 reviewers will be resolved by a discussion of all reviewers during the quality grading.
3. Discussion
The incidence of AMS is relatively high, from 23.9% to 53%,[24–26] in people accessing high altitude in a short period of time. Also, high altitude encephaledema or pneumonedema, which is a potentially fatal condition, is seen in 0.1% to 10% of people with AMS.[27] That situation has a high mortality if untreated. For people accessing high altitude, prevention of AMS can alleviate the symptoms and improve performance of climbers, which has great social significance. Acetazolamide and dexamethasone are the only 2 drugs that are currently recommended for the prevention of AMS.[8,13] As a COX inhibitor, ibuprofen can effectively prevent AMS according to some literature.[18,19] However, negative results also been made in some studies.[20,28] So ibuprofen has not been recommended so far. It is important to clarify the effect of ibuprofen in AMS prevention.
This systematic review from randomised-controlled trials might give a detail analysis evaluating the use of ibuprofen in AMS prophylaxis. Also, we will explore the best dosage and course of ibuprofen. The findings of this review will be widely disseminated through peer-reviewed journal and conference presentation. The conclusion of this review will provide valuable evidence of ibuprofen for routine practice to prevent AMS.
Author contributions
Conceptualization: Xiuwei Yuan, Yugang Zhang, Yonghua Wang.
Funding acquisition: Hai Yi.
Methodology: Hai Yi, Kuiying Wang, Xinyu Gan, Li Li, Qian Zhang, Jiao Xiang.
Project administration: Xiuwei Yuan, Yugang Zhang, Yonghua Wang.
Writing – original draft: Hai Yi.
Writing – review & editing: Yonghua Wang.
Footnotes
Abbreviations: AA = arachidonic acid, AMS = acute mountain sickness, CI = confidence interval, CNKI = China National Knowledge Infrastructure, COX = cyclooxygenase.
How to cite this article: Yi H, Wang K, Gan X, Li L, Zhang Q, Xiang J, Yuan X, Zhang Y, Wang Y. Prophylaxis of ibuprofen in acute mountain sickness: a protocol for systematic review and meta-analysis. Medicine. 2020;99:46(e23233).
This project is funded by the Hospital Management Research Foundation of the General Hospital of Western Theater Command (No.2019ZY06).
If amendments are needed, the authors will update their protocol to include any changes in the whole process of research.
The sponsors are not involved in design, execution, or writing the study.
All authors involved in this work have no conflicts of interest.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Garrido E, Botella de Maglia J, Castillo O. Acute, subacute and chronic mountain sickness. Rev Clin Esp 2020;17:S0014-2565(20)30064-3. [DOI] [PubMed] [Google Scholar]
- [2].Li Y, Zhang Y, Zhang Y. Research advances in pathogenesis and prophylactic measures of acute high altitude illness. Resp Med 2018;145:145–52. [DOI] [PubMed] [Google Scholar]
- [3].Dawadi S, Basnyat B, Adhikari S. A review of medical problems in himalayan porters. High Alt Med Biol 2020;21:109–13. [DOI] [PubMed] [Google Scholar]
- [4].Richalet JP, Larmignat P, Poignard P. Transient cerebral ischemia at high altitude and hyper-responsiveness to hypoxia. High Alt Med Biol 2020;21:105–8. [DOI] [PubMed] [Google Scholar]
- [5].Metrailler P, Greiser J, Dietrich G, et al. Swiss mountain guides: medical education, knowledge, and practice. High Alt Med Biol 2019;20:251–61. [DOI] [PubMed] [Google Scholar]
- [6].Joyce KE, Lucas SJE, Imray CHE, et al. Advances in the available non-biological pharmacotherapy prevention and treatment of acute mountain sickness and high altitude cerebral and pulmonary oedema. Expert Opin Pharmacother 2018;19:1891–902. [DOI] [PubMed] [Google Scholar]
- [7].Simancas-Racines D, Arevalo-Rodriguez I, Osorio D, et al. Interventions for treating acute high altitude illness. Cochrane Database Syst Rev 2018;6:CD009567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Tapia L, Irarrazaval S. Acetazolamide for the treatment of acute mountain sickness. Medwave 2019;19:e7737. [DOI] [PubMed] [Google Scholar]
- [9].Lipman GS, Jurkiewicz C, Winstead-Derlega C, et al. Day of Ascent Dosing of Acetazolamide for Prevention of Acute Mountain Sickness. High Alt Med Biol 2019;20:271–8. [DOI] [PubMed] [Google Scholar]
- [10].Collier DJ, Wolff CB, Hedges AM, et al. Benzolamide improves oxygenation and reduces acute mountain sickness during a high-altitude trek and has fewer side effects than acetazolamide at sea level. Pharmacol Res Perspect 2016;4:e00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Swenson ER. Pharmacology of acute mountain sickness: old drugs and newer thinking. J Appl Physiol 2016;120:204–15. [DOI] [PubMed] [Google Scholar]
- [12].Pun M. Side-effect of acetazolamide in prevention of acute mountain sickness. S Afr Med J 2012;102(3 Pt 1):114.author reply 114. [DOI] [PubMed] [Google Scholar]
- [13].Tang E, Chen Y, Luo Y. Dexamethasone for the prevention of acute mountain sickness: systematic review and meta-analysis. Int J Cardiol 2014;173:133–8. [DOI] [PubMed] [Google Scholar]
- [14].Polderman JAW, Farhang-Razi V, van Dieren S, et al. Adverse side-effects of dexamethasone in surgical patients - an abridged Cochrane systematic review. Anaesthesia 2019;74:929–39. [DOI] [PubMed] [Google Scholar]
- [15].Chauhan G, Roy K, Kumar G, et al. Distinct influence of COX-1 and COX-2 on neuroinflammatory response and associated cognitive deficits during high altitude hypoxia. Neuropharmacology 2019;146:138–48. [DOI] [PubMed] [Google Scholar]
- [16].Zhou Y, Huang X, Zhao T, et al. Hypoxia augments LPS-induced inflammation and triggers high altitude cerebral edema in mice. Brain Behav Immun 2017;64:266–75. [DOI] [PubMed] [Google Scholar]
- [17].Liu C, Liu B, Liu L, et al. Arachidonic acid metabolism pathway is not only dominant in metabolic modulation but associated with phenotypic variation after acute hypoxia exposure. Frontiers Physiol 2018;9:236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Burns P, Lipman GS, Warner K, et al. Altitude sickness prevention with ibuprofen relative to acetazolamide. Am J Med 2019;132:247–51. [DOI] [PubMed] [Google Scholar]
- [19].Kanaan NC, Peterson AL, Pun M, et al. Prophylactic acetaminophen or ibuprofen results in equivalent acute mountain sickness incidence at high altitude: a prospective randomized trial. Wilderness Environ Med 2017;28:72–8. [DOI] [PubMed] [Google Scholar]
- [20].Lundeberg J, Feiner JR, Schober A, et al. Increased cytokines at high altitude: lack of effect of ibuprofen on acute mountain sickness, physiological variables, or cytokine levels. High Alt Med Biol 2018;19:249–58. [DOI] [PubMed] [Google Scholar]
- [21].Vann RD, Pollock NW, Pieper CF, et al. Statistical models of acute mountain sickness. High Alt Med Biol 2005;6:32–42. Spring. [DOI] [PubMed] [Google Scholar]
- [22].Wagner DR, Teramoto M, Knott JR, et al. Comparison of scoring systems for assessment of acute mountain sickness. High Alt Med Biol 2012;13:245–51. [DOI] [PubMed] [Google Scholar]
- [23].Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Hackett PH, Rennie D, Levine HD. The incidence, importance, and prophylaxis of acute mountain sickness. Lancet 1976;2:1149–55. [DOI] [PubMed] [Google Scholar]
- [25].Yang SL, Ibrahim NA, Jenarun G, et al. Incidence and determinants of acute mountain sickness in mount Kinabalu, Malaysia. High Alt Med Biol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Cheng FY, Jeng MJ, Lin YC, et al. Incidence and severity of acute mountain sickness and associated symptoms in children trekking on Xue Mountain, Taiwan. PloS One 2017;12:e0183207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Basnyat B. High altitude cerebral and pulmonary edema. Travel Med Infect Dis 2005;3:199–211. [DOI] [PubMed] [Google Scholar]
- [28].Schilling M, Irarrazaval S. Ibuprofen versus acetazolamide for prevention of acute mountain sickness. Medwave 2020;20:e7733. [DOI] [PubMed] [Google Scholar]


