Abstract
In the unprecedented times of Corona Pandemic (CP), each individual is facing uncertainty and stress. Presence of cancer during these times compounds the troubles. The changing scenario of consultation and treatment during pandemic, logistic issues, dwindling finances and fear are making a negative impact on the mental health of cancer patients. In a qualitative analysis conducted in a tertiary oncology hospital from 1st June to 6th July on the recently diagnosed or under treatment cancer patients. The face to face interview was conducted using a semi structured questionnaire specific to Cancer amid CP, General Anxiety Disorder Item Scale 7 and Physical Health Questionnaire 9 (PHQ-9). There were total 294 patients, mean age around 51 years with a male female ratio of 3:2, 40% were suffering from head and neck malignancy. There was a delay initiating cancer treatment in 22.4% of patients and three fourths of them attributed it to CP. Almost 80% of patients perceived that pandemic has adversely affected their treatment and 50% thought they would have had a better chance of cure. Half of our cohort stated that due to social distancing and usage of masks, there is a communication gap between them and the doctors. They also felt that now, with decreased nonverbal communication; they felt lack of empathy. 14.9% patients were more concerned about corona pandemic as compared to malignancy. This study is about the challenges and perspective of cancer patients during the CP. It indicates a need for more systematic and patient friendly approach by the regulatory authorities, hospital management and staff. Timely intervention of those under stress is recommended more frequently during CP.
Keywords: Cancer, Corona pandemic, Psychological impact, Mental health
Introduction
COVID-19 has affected the globe since December 2019 by causing infection, morbidity, mortality; mental ailments due to medical, social, and financial issues; delay in the diagnosis and treatment of non COVID illnesses. Since we are encountering this epidemic for the first time, there are many uncertainties for obvious reasons.
Many clinical oncology associations of repute have issued recommendations for managing malignancy during COVID-19.1, 2, 3, 4 Cancer, one of the worst maladies, leads to a myriad of psychological issues – denial, self-pity, guilt, change in interpersonal relationships, loss of job, self-image, fear of lifelong morbidity, fear of death, managing logistics of treatment, and prolonged follow-up. The plight of cancer patients has further increased due to the ongoing COVID-19. A lot has been said about this by the healthcare professionals and policymakers but there is no first hand record of what the cancer patients are experiencing during this pandemic to the best of our knowledge. Considering the pervasive and diverse effect COVID-19 is having on cancer patients, we decided to perform a systematic qualitative analysis addressing the above issue.
Aims and objectives
To assess the psychological impact of COVID-19 on recently diagnosed and under treatment cancer patients at Bhagwan Mahaveer Cancer Hospital and Research Centre, Jaipur.
Methods
Study Design
This cross sectional, descriptive, and hospital based study has been conducted at the 200 bedded tertiary care, oncology super speciality hospital in west India after approval by Institutional Ethics Committee.
Random sampling method was used to collect the data. Eligible patients (≥18yrs of age, newly diagnosed and those on active treatment, cognitively functional, and physically stable) were approached. The purpose of the study was explained and those interested were enrolled after their consent.
Data Collection and Analysis
Data was collected in a face to face interview by a Psychologist and a Radiation Oncologist maintaining the privacy and confidentiality. Each interview lasted for 20-25 minutes. Information/statements given by the participants were written verbatim. Most of the interviews were conducted in Hindi and were translated and back translated in English. Total 294 participants with confirmed diagnosis of cancer were included in the study from June 1, 2010 to July 6, 2020.
Theme analysis and coding were done by 2 researchers independently. Descriptive statistical analysis has been used.
Numbers (n) and percentage (%) were calculated for the categorical variables of the socio demographic data such as age, domicile, education, gender, family structure, diagnosis etc. Mean, standard deviation, mode has been calculated by descriptive statistical analysis for psychological distress.
For the analysis of responses of open-ended questions, content analysis method has been used. Below mentioned steps used for content analysis
![]()
Instruments
Demographic Data
Participants reported their age, gender, education, employment, marital status, structure of family, economic condition before and after COVID-19.
Medical History
The complaints and their duration were recorded.
COVID Specific Information
The experience of cancer patients during COVID-19 was evaluated by drafting a semi structured questionnaire in both, Hindi and English. Questions of qualitative interview were hypothetical, leading, provocative and interpretative where participants responded to the following:
-
•
Was there any delay in starting the treatment after diagnosis? If yes, why?
-
•
Has COVID-19 affected their treatment? If yes, how?
-
•
Use of any kind of alternative medicine.
-
•
Perception about professional care during COVID-19.
-
•
What is of more concern-cancer or COVID-19?
If COVID-19 were not there, they would have had a better chance of cure?
-
•
Do they panic/have fear in coming to the hospital during COVID-19?
Psychological Distress
Anxiety and Depression was assessed using General Anxiety Disorder Item Scale 7 and Physical Health Questionnaire 9. Hindi and English versions have been used.
Results
We had interviewed a total of 294 patients of which 177 (60.20%) were males and 117 (39.80%) were females. Age ranged from 20 years to 84 years, 50.68% patients were middle aged, followed by older adults that is, 37.41%. There was no difference in the representation from rural or urban areas, 51.02% and 48.98%, respectively.
Most of the patients came from joint family 66.33%. Amongst total study population, 19.05% were illiterate, 22.45% had completed primary, and 28.23% secondary education, respectively.
Prior to the COVID Pandemic unemployment was 2.38% which drastically rose to 26.87 % after the diagnosis among the patients. Of all, 42.17% patients were from the lower income group that is, from the Below Poverty Line or Lower Income Group strata.
Among the male patients 27.11% had moderate to severe anxiety and in the females it was 31.62%. Moderate to severe depression was noted 27.67% in males and 26.5% among females, respectively.
Psychological distress was measured by General Anxiety Disorder Item Scale 7 and Physical Health Questionnaire 95, 6; data showed psychological distress was higher among middle aged adults. Of all, 58.82% suffered from moderate to severe anxiety while 55% had moderate to severe depression. When correlated with the educational status, we found that graduates and postgraduates were able to deal with the pandemic in a better way thereby resulting in lesser incidence of anxiety and depression.
Discussion
India has reported more than 2•4 million diagnosed cases and 47,000 deaths due to the COVID-19 infection as this article was being written.7
According to the GLOBOCAN 2018,8 in a population of more than 13 billion India has 2•2 million cancer prevalence, over 1•1 million incidence and 7•84 lakh deaths attributed to cancer annually. We register nearly 14,000 new cancer cases annually in our hospital. Entire spectrum of cancer management is changing rapidly. Managing such a high cancer burden during the COVID-19 has been and will continue to be a challenge, more so in a developing country like India.
Demography and Diagnosis
Females constitute 48.1% of the total cancer burden in India but our study shows that only 39.8% could reach the hospital. Though 70% of Indian population resides in villages,9 according to our study only 51.02% cancer patients reported from rural regions.
A striking observation was the drastic decline in employment after the COVID-19. The unemployment soared from 2.38 % to 26.87% after COVID-19. Patients lost their jobs (45.6%), had to wind up businesses (48.7%), could not do farming (25.6%). Daily wages laborers were the worst affected with 96.4% losing livelihood. Nearly 67% patients coming to our institute bear the treatment cost on their own. Without financial stability it is difficult to start or continue cancer treatment despite being insured, reimbursed, or supported by the government or treating institute. This is so because besides the actual treatment cost, there are other expenses like travel, lodging, day to day living. The situation becomes grimmer when the sole breadwinner is the patient or has to accompany the patient leaving his/her job (Table 1 ).
Table 1.
Socio-demographic analysis.
| N (%age) | Mean | Mode | Standard deviation | ||
|---|---|---|---|---|---|
| Gender distribution | |||||
| Female | 117 (39.80%) | ||||
| Male | 177 (60.20%) | ||||
| Age wise distribution | 51•33 | 55 | 12•71 | ||
| Young Adults (18-35 yrs.) | 35 (11.90%) | ||||
| Middle age adults (36-55 yrs.) | 149 (50.68%) | ||||
| Older adults (>55yrs.) | 110 (37.41%) | ||||
| Marital status | |||||
| Married | 267 (90.82%) | ||||
| Unmarried | 12 (4.08%) | ||||
| Widow | 13 (4.42%) | ||||
| Separated | 2 (0.68%) | ||||
| Domicile | |||||
| Rural | 150 (51.02%) | ||||
| Urban | 144 (48.98%) | ||||
| Education | |||||
| Illiterate | 56 (19.05%) | ||||
| Primary | 66 (22.45%) | ||||
| Secondary | 83 (28.23%) | ||||
| Graduate | 53 (18.03%) | ||||
| Post Graduate | 36 (12.24%) | ||||
| N (%age) | |||||
| Employment status (before) | Employment status (present) | ||||
| Retired | 40 (13.60%) | Retired | 43 (14.63%) | ||
| Service | 46 (15.65%) | Service | 25 (8.50%) | ||
| Business | 41 (13.95%) | Business | 21 (7.14%) | ||
| Farming | 39 (13.27%) | Farming | 29 (9.86%) | ||
| House Wife | 89 (30.27%) | House Wife | 93 (31.63%) | ||
| Daily Labour | 28 (9.52%) | Daily Labour | 1 (0.34%) | ||
| Unemployed | 7 (2.38%) | Unemployed | 79 (26.87%) | ||
| Others (Student, Priest) | 4 (1.36%) | Student | 3 (1.02%) | ||
| Family Structure | |||||
| Joint | 195 (66.33%) | ||||
| Nuclear | 99 (33.67%) | ||||
| Economic status | |||||
| Below Poverty Line (BPL) | 23 (7.82%) | ||||
| Lower Income Group (LIG) | 101 (34.35%) | ||||
| Middle Income Group (MIG) | 142 (48.30%) | ||||
| Higher Income Group (HIG) | 28 (9•52%) | ||||
During COVID-19, twice the percentage of head and neck cancers reported to us than our usual head and neck malignancy burden implying that the signs and symptoms of head and neck cancers were not ignored during COVID-19 as compared to those of other sites.
Delay in initiating treatment
There is clear evidence that delay in starting treatment adversely affects the outcomes.10, 11, 12 Most common reasons for delay are lack of awareness, consultation with unqualified local practitioners, use of alternative medication, poor socio-economic conditions and lack of a proper referral infrastructure. These have been well documented in the past and are a known problem in developing nations.13 In our study 22.5% patients' treatment was delayed after the confirmation of diagnosis. Besides the above mentioned factors, lockdown (57.84%), apprehension of contracting COVID-19 infection (15.15%) and unavailability of the doctor of patient's choice (7.5%) were specific for the given circumstances. In 75.75% patients, delay was attributed to COVID-19. Apprehension of cancer treatment was the cause of delay only in 4.54%, which, otherwise, is one of the main reasons. Undergraduates or illiterate middle aged males from joint families were affected the most.
A retired gentleman said that “I went to 2-3 hospitals, but was denied the planned surgery. I was scared of the Corona infection.”[Respondent (R)-147].
A 50 years old lady living all by herself had renal cancer. She said “my children were away so there was nobody to accompany me to the hospital”(R-169).
“Cancer is incurable then why subject myself to risk of contracting corona infection by travelling for its treatment” were the words of an illiterate breast cancer patient from rural domicile.(R-164)
Do you think COVID-19 has affected your treatment?
A total of 78.57% patients believed that COVID-19 has affected the management of cancer. There were 471 responses because many patients chose more than one reason which, they thought, impacted their treatment. Since ours is a tertiary referral centre, most of the patients are referred to us after the diagnosis of cancer. The diagnostic delays can occur due to patients not reaching the doctor or due to inappropriate referrals by the clinicians, but the former has more profound effects. In our study diagnosis was delayed in 74 patients. But unfortunately, 182 patients’ treatment was delayed despite confirmed diagnosis.
“My surgery was scheduled for 31st March but lockdown was implemented from 21st. My disease was in the mouth in the early stage but gradually my cheek became stony hard. It was then that I realised that it has progressed. The hospitals close to my place were accepting only emergency cases and not the routine ones. I could make it after the lockdown was lifted.” (R-147).
Equal number of patients hailing from rural and urban areas, 70.56% less or uneducated and 65.8 % coming from joint families thought that COVID-19 had affected their treatment. Socioeconomically privileged class was as badly affected by COVID-19 as the underprivileged as far as cancer treatment was concerned.
“My treatment got delayed by 3 months due to COVID-19, transport was unavailable, doctor was on leave. I would have been cured if it were not for COVID-19, but now I am not sure.”(R-60)
Financial impact was observed by 12.55%, social impact by 6.49% and medical impact by 26.40%.
“I could not get permission to move from my town and there was some financial problem as well. My treatment got delayed by one and half months because surgery was not being done at that point of time when I had come soon after the lockdown”(R-90).
“Though I was ready to come to the hospital, the only mode of transport was jeep and the drivers were apprehensive of ferrying me.”(R-143)
Treatment breaks adversely affect the survival and QOL in cancer patients.14, 15 A total of 9.95% of patients had interruption in chemotherapy or radiation therapy schedules due to COVID-19.
5.4. Alternative treatment
According to the literature, 25%-38% of cancer patients opt for alternative treatment at some point during their lifetime.16 , 17 During the COVID-19 only 12.9% of the study population took alternative treatment-homeopathic-60%, ayurvedic-16.67%, and others- 23.33%. Drastically reduced percentage suggests that probably patients did not have access to alternative treatment also during the lockdown.
Perception about cancer treatment during COVID-19
Nearly two thirds of patients thought that their cancer management would have been better if it were not for COVID-19. Of these, more than twice were from rural (68.27% vs 31.73%) background. Of all, 37.93% felt that the logistics were difficult for them because of COVID-19. With the growing concerns amongst the medical fraternity and safeguarding policies of the medical institutes, various measures were taken at our institute also for the safety of the patients, caregivers and hospital staff.
One of our patients shared that “I did not like the distance between myself and my treating clinician. I felt that the registration process had become longer after COVID-19 and so I had to get my driver along with me to stand in the queue which I did not like.”(R-5)
During lockdown commuting was difficult, there was reduced workforce due to illness and self-isolation, duty were on a rotation basis to have minimum numbers of staff being exposed to a potential COVID-19 positive patient. The consultations have become quick and crisp so that the contact time and hospital stay of the patient is minimized thereby minimizing the risk of exposure to the virus. A total number of 8.28% of patients were not satisfied with the clinical examination.
With the PPEs, masks, and face shields, increased distance between the staff and patients, outside noise entering through the open doors in the OPDs, communication is difficult. It is difficult to hear, lip reading is not possible and expressions are not seen because of the mask. Of all, 6.21% patients complained of communication gap and they felt that the warmth was lacking.
A gentle touch conveys more than a hundred words. Cancer patients need this more than anybody else. The expression of empathy and compassion was unintentionally lost because of increased distance, lack of time and inhibition in the minds of staff and patients. A study by Leong et al18 identified adverse emotional responses including anger, frustration, powerlessness and fear amongst patients and staff during epidemic. Our study noted that 39.31% of the patients were unhappy about the distancing between them and the doctors.
“Before COVID-19, my doctor used to make me sit close to him and examine me, he used to talk to me till I was satisfied. Now I find it difficult to convey my problems and to understand what he says”(R-132).
Another patient complained about the same issue of difficulty in communication and was upset about the fact that “my money was being wasted in testing me for Corona. I also felt that doctors don't examine me thoroughly now”(R-176)
A total of 8.28% of patients were planned for a particular treatment but because of the lockdown there was disease progression and the treatment plan had to be changed.
What bothers you more – cancer or COVID-19 infection?
Of all, 59.8 % respondents were more concerned about cancer. This belief was not affected by the domicile or financial status of the patient but illiterate and under graduate were more concerned (72.72% vs 27.28%). Concerns were the same that we find in literature – fear, uncertainty, fear of worsening of symptoms, death, why me, and economic burden.19 However, 6.25% patients were apprehensive of cancer during COVID-19 because they were aware that cancer treatment and multiple visits to the hospital will make them more vulnerable to COVID-19 infection.20 The COVID-19 has a profound psychological impact and fear is its one of the most important aspects. Its incidence ranges from 33% to 56%.21 In our study 14.9% cancer patients kept COVID-19 above malignancy as their cause of concern.
A patient was apprehensive and he said that “my cancer surgery will be deferred if the Corona report came positive” (R-252).
Another was worried that “I have heard that corona makes a person sick. I am already suffering from cancer and am weak. What will happen if I acquire infection?” (R-223)
One patient said “if I get Corona positive and am denied treatment for cancer, I will die due to lack of cancer treatment” (R-205)
Of all, 17% respondents were concerned about both, COVID-19 and cancer. A statement by an ovarian cancer patient sums it all. The Guardian quoted her “ sometimes it feels like there's a cruel race being run to see what will kill me first – cancer, corona virus, or stress.22
“My immunity is low because of cancer and I should not come out of my house but I have to expose myself to this risk while commuting to reach the cancer hospital. Cancer is a deadly disease, what to do?”(R-50)
“I am already depressed since cancer was diagnosed and following the Corona updates, my worries have multiplied. I know it is even infecting healthy individuals, my immunity is already low.”(R-165)
Better chance of cure from cancer if COVID-19 were not there
Of all, 63.2% patients thought that they would have had better chances of cure if it were not for COVID-19. Most of them attributed it to the delay in diagnosis and treatment; many said that “we would have completed the treatment by now, if there was no COVID-19.” They shared their concern about increased symptoms and more extensive treatments being charted out now due to the progression of disease during COVID-19.
“If I would have come earlier, maybe only tablets would have sufficed. The delay has happened because of lockdown so my condition has worsened”(R-132).
“Due to lockdown, my cancer, which was operable, has become inoperable. Now I've been advised to go for chemoradiation and surgery will be done later”(R-181).
Yet another mentioned that “if it were not for COVID-19, I would have come earlier and such an extensive surgery could have been avoided”(R-196).
Panic and fear in attending hospital
In a community based survey carried out in India in the last week of March’20, approximately one third of the respondents had significant psychological impact (IES-R score>24).23
Some patients were felt burdened with the extra precautions they have to take during COVID-19 and others were worried that their treatment may be discontinued if they get infected.
In the words of a 60 years old lady, “Situation is so grim that one has to think twice whether to sit or not at a given place”(R-24).
A literate housewife said “Look at the irony! When we are supposed to stay indoors to save ourselves from Corona virus, I have to come out of my home to get cancer treatment. What if I get infected in the hospital?”(R-190)
Change in support system
Of all, 58.1% patients noted that there was worsening of their instrumental and/or emotional support system after COVID-19. Male patients were more adversely affected than females. Surprisingly, patients hailing from joint families were more distressed than nuclear families after COVID-19.
A breast cancer patient was worried that “my sister is unable to come to be with me. I am unable to get fruits and proper diet due to lockdown so my haemoglobin has dropped. I feel suffocated and nauseated on using mask and sanitizer”(R-50).
“There is an increased financial crisis after COVID-19 and helping hands are facing the same challenges” (R-79).
One patient who is a tea vendor says that “due to lockdown I am not allowed to open my tea stall” (R-87).
Another small time businesswoman said that “I am not able to earn these days, how will I repay the loan?” (R-115).
A young lady, a case of breast cancer, was an exception. She was recently enrolled for postgraduation in medicine and was relieved that due to COVID-19 there was procedural delay in her joining therefore she could take the treatment without missing her duties.
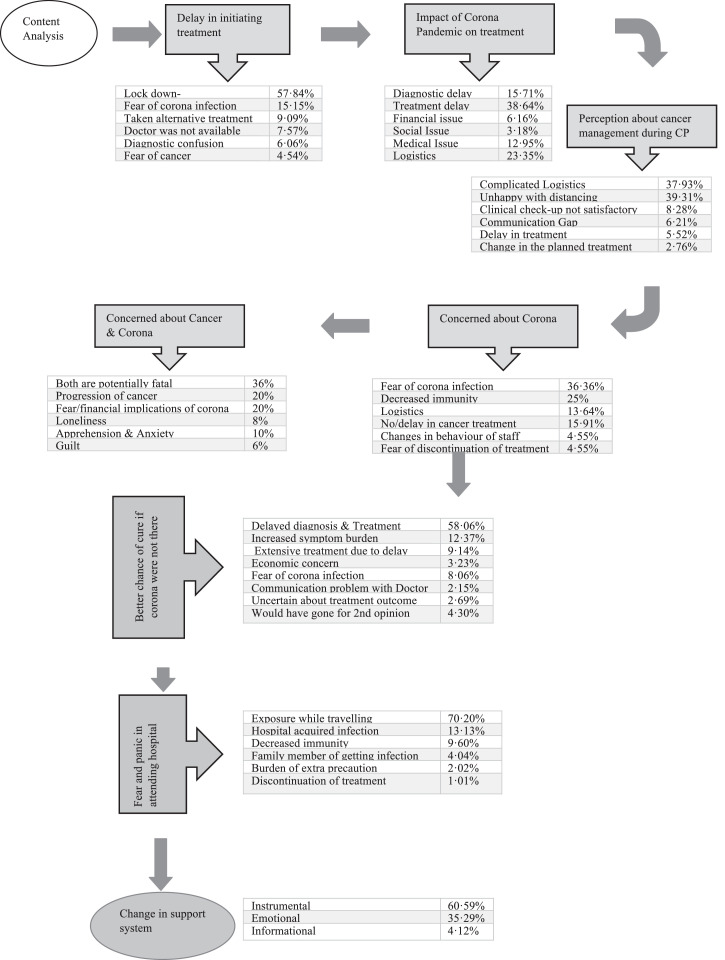
The qualitative data analysis of patients’ perspectives on COVID-19 discussed above has been charted out in Figure 1 .
Fig. 1.
Qualitative data analysis - patient's perspectives on corona pandemic.
Psychological distress
Significant levels of distress was experienced by 20%-52% cancer patients.24, 25, 26 In our study significant levels of anxiety and depression were noticed in 31.62% and 26.50% patients, respectively (Table 2 ). These were pronounced in middle aged, undergraduate or illiterate males. Highest prevalence of depression (22%-57%) was seen in oropharyngeal cancers by Massie et al.27 Our findings are the same with head and neck cancers constituting 45 % of the total patients facing depression (Table 3 ).
Table 2.
Psychological distress among cancer patients.
| Overall – N (%age) | Male – N (%age) | Female – N (%age) | |
|---|---|---|---|
| GAD – 7 | |||
| Mean | 6•06 | 6•05 | 6•07 |
| Mode | 0 | 0 | 0 |
| Standard Deviation | 4•65 | 4•54 | 4•83 |
| Severity | |||
| Minimal (0-4) | 134 (45.57%) |
82 (46.33%) | 52 (44.44%) |
| Mild (5-9) | 75 (25.51%) |
47 (26.55%) | 28 (23.93%) |
| Moderate (10-14) | 76 (25.85%) | 41 (23.16%) | 35 (29.91%) |
| Severe (15-21) | 9 (3.06%) |
7 (3.95%) | 2 (1.71%) |
| PHQ – 9 | |||
| Mean | 6.48 | 6.57 | 6.36 |
| Mode | 0 | 5 | 0 |
| Standard deviation | 4.73 | 4.63 | 4.89 |
| Severity | |||
| Minimal (1-4) | 113 (38.44%) | 63 (35.59%) | 50 (42.74%) |
| Mild (5-9) | 101 (34.35%) | 65 (36.72%) | 36 (30.77%) |
| Moderate (10-14) | 64 (21.77%) | 41 (23.16%) | 23 (19.66%) |
| Moderately Severe (15-19) | 13 (4.42%) | 7 (3.95%) | 6 (5.13%) |
| Severe (20-27) | 3 (1.02%) | 1 (0.56%) | 2 (1.71%) |
Table 3.
Comparative analysis of anxiety & depression (moderate to severe) with socio demographic variables.
| GAD – 7 N (%age) | PHQ – 9 N (%age) | ||
|---|---|---|---|
| Gender | |||
| Female | 37 (43.53%) | 31 (38.75%) | |
| Male | 48 (56.47%) | 49 (61.25%) | |
| Domicile | |||
| Rural | 41 (48.24%) | 39 (48.75%) | |
| Urban | 44 (51.76%) | 41 (51.25%) | |
| Marital Status | |||
| Married | 76 (89.41%) | 73 (91.25%) | |
| Unmarried | 5 (5.88%) | 3 (3.75%) | |
| Divorce | 1 (1.18%) | .. | |
| Widow | 3 (3.53%) | 4 (5.00%) | |
| Education | |||
| Illiterate | 12 (14.12%) | 11 (13.75%) | |
| Primary | 15 (17.65%) | 20 (25.00%) | |
| Secondary | 30 (35.29%) | 24 (30.00%) | |
| Graduate | 15 (17.65%) | 16 (20.00%) | |
| Post Graduate | 13 (15.29%) | 9 (11.25%) | |
| Age grouping | |||
| Yong Adults (0-35 yrs) | 12 (14.12%) | 7 (8.75%) | |
| Middle Age Adults (36-55 yrs) | 50 (58.82%) | 44 (55.00%) | |
| Older Adults (56 and Above) | 23 (27.06%) | 29 (36.25%) | |
| Family structure | |||
| Joint | 59 (69.41%) | 58 (72.50%) | |
| Nuclear | 26 (30.59%) | 22 (27.50%) | |
| Economic status | |||
| BPL | 6 (7.06%) | 10 (12.50%) | |
| LIG | 34 (40.00%) | 28 (35•00%) | |
| MIG | 38 (44.71%) | 37 (46.25%) | |
| HIG | 7 (8.24%) | 5 (6.25%) | |
Conclusion
Among the cancer patients, recently diagnosed and under treatment patients were the worst affected. The logistics are most difficult and emotionally they are most challenged. It is important to reassure the public that it is safe and essential to seek medical advice for cancer with strict infection prevention and control policy. Urgent policy interventions are necessary at the level of government and oncology centers to manage the backlog. If required, remote consultations may be done with the experts. With COVID-19 infection looming all over, the psychological issues of cancer patients have exacerbated. The enormous backlog in the hospitals with multiple logistic and socioeconomic issues will increase the stress upon the cancer patients. So, the mental health of cancer patients has to be addressed to mitigate their anxiety and depression. This research will help us formulate early steps to reach out to those requiring intervention during COVID-19. Continued and regular counseling will help them cope better with the dual stress of cancer and COVID-19 pandemic.
References
- 1.American Society of Clinical Oncology . A guide to cancer care delivery during the Covid-19 pandemic. 2020. https://www.asco.org/sites/new-www.asco.org/files/content-files/2020-ASCO-Guide-Cancer-COVID19.pdf Available from. [Google Scholar]
- 2.Cancer patient management during the COVID-19 pandemic | ESMO [Internet]; 2020 [cited Jul 30]. Available from: https://www.esmo.org/guidelines/cancer-patient-management-during-the-covid-19-pandemic.
- 3.COVID-19 recommendations and information - American Society for Radiation Oncology (ASTRO) - American Society for Radiation Oncology (ASTRO) [Internet]; 2020 [citedJul 30]. Available from: https://www.astro.org/Daily-Practice/COVID-19-Recommendations-and-Information/Clinical-Guidance.
- 4.Pramesh CS, Gupta S, Laskar SG, Sengar M, Chinnaswamy G, Khattry N, et al. The COVID-19 pandemic and the Tata Memorial Centre response. Indian J Cancer. 2020;57:123–128. doi: 10.4103/ijc.IJC_250_20. [DOI] [PubMed] [Google Scholar]
- 5.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]; PMID: 16717171.
- 6.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]; PMID: 11556941; PMCID: PMC1495268.
- 7.WHO Coronavirus Disease (COVID-19) Dashboard | WHO Coronavirus Disease (COVID-19) Dashboard [Internet], 2020. [cited 2020 Jul 30]. Available from: https://covid19.who.int/.
- 8.Globocan 2018: India factsheet - India Against Cancer [Internet]. [cited 2020 Jul 30]. Available from: http://cancerindia.org.in/globocan-2018-india-factsheet.
- 9.Chandramouli C. 2014. Report on Post Enumeration Survey. [Google Scholar]
- 10.Chen Z, King W, Pearcey R, Kerba M, Mackillop WJ. Vol. 87. Elsevier; 2008. The relationship between waiting time for radiotherapy and clinical outcomes: a systematic review of the literature [Internet]http://www.thegreenjournal.com/article/S0167814007005889/fulltext (Radiotherapy and Oncology). [cited 2020 Jul 26]. p. 3–16. Available from: [DOI] [PubMed] [Google Scholar]
- 11.Biagi JJ, Raphael MJ, Mackillop WJ, Kong W, King WD, Booth CM. Association between time to initiation of adjuvant chemotherapy and survival in colorectal cancer a systematic review and meta-analysis. JAMA - J Am Med Assoc. 2011;305:2335–2342. doi: 10.1001/jama.2011.749. [DOI] [PubMed] [Google Scholar]
- 12.Raphael MJ, Biagi JJ, Kong W, Mates M, Booth CM, Mackillop WJ. Vol. 160. Springer New York LLC; 2016. The relationship between time to initiation of adjuvant chemotherapy and survival in breast cancer: a systematic review and meta-analysis [Internet]https://link.springer.com/article/10.1007/s10549-016-3960-3 (Breast Cancer Research and Treatment). [cited 2020 Jul 26]. p. 17–28. Available from. [DOI] [PubMed] [Google Scholar]
- 13.Tiwari V, Yogi V, Ghori HU, Singh OP, Peepre K, Yadav S, et al. Identifying the factors causing delayed presentation of cancer patients to a government medical college of central India. J Clin Diagnostic Res. 2015;9(9):XC09–XC12. doi: 10.7860/JCDR/2015/15104.6512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Russo G, Haddad R, Posner M, Machtay M. Radiation treatment breaks and ulcerative mucositis in head and neck cancer. Oncologist. 2008;13:886–898. doi: 10.1634/theoncologist.2008-0024. [DOI] [PubMed] [Google Scholar]
- 15.Groome PA, O'Sullivan B, Mackillop WJ, Jackson LD, Schulze K, Irish JC, et al. Compromised local control due to treatment interruptions and late treatment breaks in early glottic cancer: population-based outcomes study supporting need for intensified treatment schedules. Int J Radiat Oncol Biol Phys. 2006;64:1002–1012. doi: 10.1016/j.ijrobp.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 16.Kumar D, Goel NK, Pandey A.K., Sarpal SS. Complementary and alternative medicine use among the cancer patients in Northern India. South Asian J Cancer. 2016;5(1):8–11. doi: 10.4103/2278-330X.179689. [DOI] [PMC free article] [PubMed] [Google Scholar]; PMID: 27169110; PMCID: PMC4845611.
- 17.Chaturvedi P, Chaturvedi U, Sanyal B. Alternative medicine and cancer patients in less developed countries. Lancet Oncol. 2002;3:10. doi: 10.1016/s1470-2045(01)00615-5. [DOI] [PubMed] [Google Scholar]
- 18.Leong IY, Lee AO, Ng TW, Lee LB, Koh NY, Yap E, et al. The challenge of providing holistic care in a viral epidemic: opportunities for palliative care. Palliat Med. 2004;18(1):12–18. doi: 10.1191/0269216304pm859oa. [DOI] [PubMed] [Google Scholar]; PMID: 14982202.
- 19.Singer S, Das-Munshi J, Brähler E. Prevalence of mental health conditions in cancer patients in acute care-a meta-analysis. Ann Oncol. 2009;21:925–930. doi: 10.1093/annonc/mdp515. [DOI] [PubMed] [Google Scholar]
- 20.Gregucci F, Caliandro M, Surgo A, Carbonara R, Bonaparte I, Fiorentino A. Cancer patients in Covid-19 era: swimming against the tide. Radiother Oncol. 2020;149:109–110. doi: 10.1016/j.radonc.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]; Epub 2020 Apr 4. PMID: 32342866; PMCID: PMC7129219.
- 21.Pakpour AH, Griffiths MD. The fear of COVID-19 and its role in preventive behaviors. J Concurr Disord. 2020;2:58–63. [Google Scholar]
- 22.Chaney H. “What a terrible time to have cancer”: falling ill during the coronavirus crisis | US news | The Guardian. [cited 2020 Jul 30]; Available from: https://www.theguardian.com/us-news/2020/mar/30/what-a-terrible-time-to-have-cancer-falling-ill-during-the-coronavirus-crisis.
- 23.Varshney M, Parel JT, Raizada N, Sarin SK. Initial psychological impact of COVID-19 and its correlates in Indian Community: An online (FEEL-COVID) survey. PLoS One [Internet] 2020;15 doi: 10.1371/journal.pone.0233874. https://pubmed.ncbi.nlm.nih.gov/32470088/ May 1 [cited 2020 Jul 14]Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Funk R, Cisneros C, Williams RC, Kendall J, Hamann HA. What happens after distress screening? Patterns of supportive care service utilization among oncology patients identified through a systematic screening protocol. Support Care Cancer. 2016;24:2861–2868. doi: 10.1007/s00520-016-3099-0. [DOI] [PubMed] [Google Scholar]
- 25.Krebber AMH, Jansen F, Cuijpers P, Leemans CR, Verdonck-de Leeuw IM. Screening for psychological distress in follow-up care to identify head and neck cancer patients with untreated distress. Support Care Cancer [Internet] 2016;24:2541–2548. doi: 10.1007/s00520-015-3053-6. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mehnert A, Hartung TJ, Friedrich M, Vehling S, Brähler E, Härter M, et al. One in two cancer patients is significantly distressed: Prevalence and indicators of distress. Psychooncology. 2018;27:75–82. doi: 10.1002/pon.4464. [DOI] [PubMed] [Google Scholar]
- 27.Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004;10021:57–71. doi: 10.1093/jncimonographs/lgh014. [DOI] [PubMed] [Google Scholar]