Abstract
Studies about the role of self-compassion have focused primarily on psychological well-being, but there is solid evidence to suggest that self-compassion may have larger and more prominent implications in the medical world. Therefore, this systemic review aimed to investigate the effects of self-compassion on psychosocial and clinical outcomes in medically ill patients.
A comprehensive search of several databases from their inception to August 10, 2020, was conducted, which included Ovid MEDLINE(R) and Epub Ahead of Print, Ovid Embase, Ovid Cochrane Central Register of Controlled Trials, and Cumulative Index to Nursing and Allied Health Literature (CINAHL). Eligible studies needed to include psychosocial or clinical outcomes of self-compassion in medically ill patients.
Nineteen articles (n=2,713 patients; 73.3% females) met our eligibility criteria and were included in this systematic review. There was a negative correlation between self-compassion and psychosocial outcomes such as anxiety, depression, and stress. Moreover, based on self-compassion intervention, there was an improvement in clinical outcomes related to diabetes such as hemoglobin A1c (HbA1c) and blood glucose levels.
This systematic review highlights the effect of self-compassion on psychosocial and clinical outcomes. Further studies are needed to evaluate long-term outcomes of a self-compassion-based-intervention to highlight its importance in the role of disease management.
Keywords: positivepsychology, psychology, self-compassion, psychosocial, clinical, medical disease
Introduction and background
Individuals suffering from medical illnesses are affected on both physical and psychological levels. The combination of exhaustion, pain, and decreased quality of life can cause self-doubt, low self-esteem as well as an inability to complete any personal or work-related tasks [1]. Psychological symptomatology of stress, anxiety, and depression can further exacerbate existing illnesses, contributing to a decreased desire for engaging in health-promoting or disease management behaviors [2-4]. Moreover, this burden can cause further psychological damage by causing individuals to direct blame at themselves for not being able to meet expectations of managing their illness [5].
In the past decade, evidence has emerged to suggest that self-compassion can be an important tool to help manage psychological issues. The concept of self-compassion, as defined by Neff, constitutes “being touched by and open to one's own suffering, not avoiding or disconnecting from it, generating the desire to alleviate one's suffering and to heal oneself with kindness [6]. Self-compassion thus involves offering nonjudgmental understanding to one's pain, inadequacies and failures, so that one's experience is understood as a part of the larger human experience” [6]. It involves the idea that individuals should treat themselves with the same care as they would treat their loved ones. The concept of self-compassion is further defined by three essential components, which include common humanity versus isolation, self-kindness versus self-judgment, and mindfulness versus over-identification [6].
Previous studies have demonstrated that self-compassion is linked to many factors of psychological well-being such as happiness, decreased anxiety, depression, stress, and a better quality of life [7-9]. A meta-analysis by MacBeth and Gumley revealed that individuals with high self-compassion reported having better mental health and quality of life compared to those with low self-compassion [10]. Furthermore, a study by Neff and McGehee demonstrated that self-compassion is correlated with resilience [11]. Another study by Neff, Kirkpatrick, and Rude demonstrated the protective role of self-compassion against anxiety [12].
To date, most of the research has directed its efforts toward the role of self-compassion in psychological well-being; however, there is evidence to suggest that self-compassion may well have a stronger contribution to make in the medical world as well. Although the research is limited to the role of self-compassion for health-related outcomes in medically ill patients, there are promising results to support the incorporation of self-compassion interventions to improve disease trajectory and management. This systematic review aimed to investigate the effects of self-compassion on psychosocial and clinical outcomes in medically ill patients.
Review
Methods
Data Sources and Search Strategies
A comprehensive search of several databases from their inception to August 10, 2020, was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [13]. The databases included Ovid MEDLINE(R) and Epub Ahead of Print, Ovid Embase, Ovid Cochrane Central Register of Controlled Trials, and Cumulative Index to Nursing and Allied Health Literature (CINAHL). The search strategy was designed and conducted by an experienced librarian. Controlled vocabulary supplemented with keywords was used to search for studies describing self-compassion and medical treatment. The actual strategy listing all search terms used and how they are combined is available in the Appendix section (Table 4).
Eligibility Criteria and Quality Assessment
Studies were deemed eligible if they met all of the following inclusion criteria: 1) investigate self-compassion; 2) involve patients aged more than 18 years with medical disorders, and 3) deal with psychosocial or clinical outcomes of self-compassion in medically ill patients. Case reports, conference abstracts and/or abstracts, and articles that were not in English were excluded from the study. The quality of each study was independently evaluated by two authors using the National Institutes of Health (NIH) Quality Assessment Tool [14]. Results of the quality assessment of all included studies are shown in the Appendix section (Table 5). All observational and cross-sectional studies were judged to be of good quality. The patients appeared to represent the whole experience of the investigator and the exposure and outcomes were adequately ascertained, and the length of follow-up was also deemed adequate.
Results
Study Selection and Characteristics
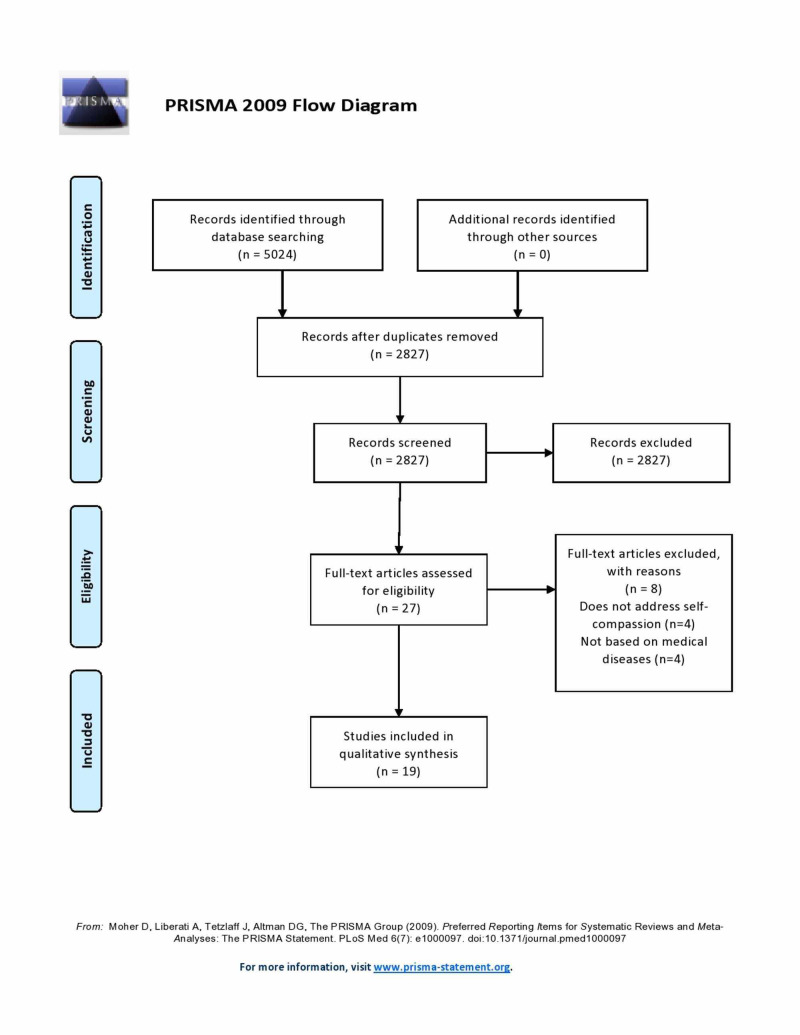
A total of 5,024 records were identified from the initial search of electronic databases. After the exclusion of duplicated articles, 2,827 articles underwent title and abstract review. Following the exclusion of articles that did not fulfill the eligibility criteria, 27 articles underwent a full-length review. Eight articles were further excluded, for reasons shown in the Appendix section (Figure 1). Finally, 19 articles (n=2,713 patients, of which 73.3% were females) met our eligibility criteria and were included in this systematic review [15-33]. The baseline characteristics of the included studies are comprehensively described in Table 1.
Table 1. Baseline characteristics of included studies.
F: female; M: male; GCSE: general certificate of secondary education; NA: not applicable; T1DM: type 1 diabetes mellitus; T2DM: type 2 diabetes mellitus; TAFE: technical and further education; HIV: human immunodeficiency virus
| Study | Year | Country | Sample size | Gender | Age (in years) | Education | Medical condition | Treatment of disease | Time from diagnosis | Study design |
| Abdollahi, Taheri, and Allen [15] | 2020 | Iran | 210 | All females | 43.2 ± 7.4 | Diploma (n=54); bachelor's degree (n=86); master's degree (n=28) | Breast cancer | Chemotherapy (n=155); radiation (n=147); hormone (n=164); reconstructive (n=73) | ≤1 year (n=70); 1-2 years (n=61); 2-5 years (n=52); >5 years (n=27) | Cross-sectional study |
| Ambridge, Fleming, and Henshall [16] | 2020 | UK | 66 | 32F, 34M | NA | GCSE (n=37); A-level (n=14); degree (n=10); doctoral degree (n=4) | Brain injury | NA | ≤1 year (n=16); 1-2 years (n=15); 2-3 years (n=4); 3-4 years (n=4); 4-5 years (n=4); >5 years (n=21) | Mixed methods |
| Arambasic, Sherman, and Elder [17] | 2019 | Australia | 82 | All females | 58.46 ± 8.77 | Grade 12 or less (n=26); vocational (n=16); bachelor's degree (n=27); master's degree (n=13) | Breast cancer | Chemotherapy (n=53); radiation (n=59); hormone (n=55); targeted (n=15); reconstructive (n=21) | 82.14 ± 19.34 months | Cross-sectional study |
| Brown et al. [18] | 2019 | UK | 184 | All females | 51.54 ± 9.42 | Degree and above (n=109); non-degree (n=71) | Breast cancer | Chemotherapy (n=116); radiation (n=135); hormone (n=139); targeted (n=30); mastectomy (n=57) | NA | Cross-sectional study |
| Dowd and Jung [19] | 2017 | Canada | 220 | 202F, 17M, 1 preferred not to say | 44.01 ± 13.33 | NA | Celiac disease | NA | 7.85 ± 7.85 years | Prospective study |
| Edwards et al. [20] | 2019 | USA | 339 | 236F, 96M | 51.66 ± 14.58 | NA | Chronic pain | NA | NA | Cross-sectional study |
| Friis et al. [21] | 2015 | New Zealand | 110 | 72F, 38M | 47.6 ± 15.2 | NA | T1DM (n=67); T2DM (n=20); type 2 insulin (n=23) | NA | 16.7 ± 12.3 years | Cross-sectional study |
| Friis et al. [22] | 2016 | New Zealand | 63 | 20M, 43F | 44.37 ± 15.62 | NA | T1DM (n=46); T2DM (n=9); type 2 insulin (n=8) | NA | 16.84 ± 12.32 years | RCT |
| Hayter and Dorstyn [23] | 2013 | Australia | 97 | 64F, 33M | 40.1 ± 11.8 | High school certificate (n=32); some high school (n=31); degree (n=15); postgraduate (n=6); apprenticeship (n=6) | Spina bifida | NA | NA | Cross-sectional study |
| Karami et al. [24] | 2018 | Iran | 20 | NA | Control: 43.57 ± 2.59; experimental: 44.38 ± 2.35 | NA | T2DM | NA | NA | Quasi-experimental study |
| Klein et al. [25] | 2020 | USA | 86 | 33F, 53M | 29.7 ± 14.4 | NA | Bleeding disorders | NA | NA | Cross-sectional study |
| Morrison et al. [26] | 2019 | UK | 176 | 120M, 56F | 64 ± 8 | NA | T2DM | NA | 12 ± 8 years | Cross-sectional study |
| Ferrari, Dal Cin, and Steele [27] | 2017 | Australia | 310 | 58M, 252F | 37.6 ± 15.1 | High school (n=58); TAFE (n=81); university undergraduate (n=109); university graduate (n=35) | T1DM (n=203); T2DM (n=73) | Insulin injections (n=98); diet and exercise (n=97); insulin pump (n=76) | NA | Cross-sectional study |
| Hurwit, Yun, and Ebbeck [28] | 2018 | USA | 259 | 41M, 218F | NA | NA | Multiple sclerosis | NA | NA | Cross-sectional study |
| Baillargeon et al. [29] | 2018 | Canada | 48 | All females | 26.83 ± 5.98 | NA | Vulvodynia | NA | NA | Cross-sectional study |
| Skelton et al. [30] | 2020 | USA | 34 | 17F, 17M | 47.79 ± 12.67 | Grade 1-8 (n=2); some high school (n=7); diploma (n=11); some college (n=8); associates (n=4); college degree (n=2) | HIV | NA | 18.77 ± 11.26 years | Cross-sectional study |
| Vasigh et al. [31] | 2019 | Iran | 168 | 91M, 77F | 43.13 ± 8.76 | Literacy reading and writing (n=13); diploma (n=89); academic (n=66) | Migraine | NA | NA | Cross-sectional study |
| Wren et al. [32] | 2012 | USA | 88 | 71.6%F | 53.93 ± 9.65 | Some high school or less (n=7); high school graduate (n=15); some college (n=35); college graduate or higher (n=31) | Musculoskeletal pain | NA | 11.79 ± 10.23 years | Cross-sectional study |
| Zhu et al. [33] | 2018 | China | 153 | 52M, 100F, 1 unknown | 50.78 ± 11.61 | Low (n=16); middle (n=103); high (n=30); missing (n=3) | Cancer | Chemotherapy (n=64); radiation (n=23); operation (n=22); Chinese medicine (n=12) | NA | Longitudinal study |
Baseline Characteristics
As shown in Table 1, 19 studies were included of which four studies were from the UK, five studies from the USA, four studies from Australia, two studies from New Zealand, three studies from Iran, and one study from China; 2,713 patients were included of which 1,989 were female, with an age range of 26-64 years. Common medical conditions included were diabetes (n=5), breast cancer (n=3), multiple sclerosis (n=1), spina bifida (n=1), celiac disease (n=1), HIV (n=1), brain injury (n=1), migraine (n=1), musculoskeletal pain (n=1), and vulvodynia (n=1). Studies were mostly cross-sectional (n=14), followed by randomized controlled trials (n=2), mixed methods (n=1), longitudinal study (n=1), and quasi-experimental (n=1). Time from diagnosis ranged between 6-18 years for different medical conditions. Treatment options were included for breast cancer and diabetes. Breast cancer treatment options in different studies were similar and included chemotherapy, radiation, surgery, and hormone therapy. Treatment for diabetes included insulin pumps, insulin injections, and lifestyle modifications (diet and exercise).
Psychosocial Outcomes
Eighteen included studies exhibited outcomes of self-compassion using the Self-Compassion Scale (SCS) questionnaire as shown in Table 2. Five studies provided the values of self-compassion based on the average of all subscales from 1-5. The range for the self-compassion values was between 2.8-3.46. Three studies looked at specific subscales with the SCS [16,18,30]. A study by Ambridge, Fleming, and Henshall looked at the Self-Compassion Scale-Short-Form (SCS-SF), which was 5.69 ± 1.15 [16]. A study by Brown et al. demonstrated self-kindness: 2.74 ± 0.94, common humanity: 3.11 ± 0.93, mindfulness: 3.18 ± 0.83, and reflection: 1.70 ± 0.61 [18]. Lastly, a study by Skelton et al. observed scores of 64.12 ± 19.48 for compassionate engagement and action [30]. The rest of the studies reported SCS as an average of the total score, which ranged from 18-80.
Table 2. Effect of self-compassion on psychosocial outcomes.
BC Major Depression Inventory: British Columbia Major Depression Inventory; PHQ: Patient Health Questionnaire; SCS: Self-Compassion Scale, DDS17: 17-item Diabetes Distress Scale; CD-RISC 10: 10-item Connor Davidson Resilience Scale; QoL: quality of life; MSC: mindful self-compassion
| Studies | Year | Questionnaires | Psychosocial outcomes | Correlations |
| Abdollahi, Taheri, and Allen [15] | 2020 | Self-Compassion Scale | Mean: 56.1 ± 9.25 | Self-compassion moderates the relationship between perceived stress and self-care behaviors. Stress and self-compassion were significant predictors of self-care behaviors |
| Perceived Stress Scale | Mean: 24.3 ± 5.23 | |||
| Self-care utilization questionnaire | Mean 43.2 ± 7.4 | |||
| Ambridge, Fleming, and Henshall [16] | 2020 | Self-Compassion Scale-Short-Form | 5.69 ± 1.15 (SCS-SF); 95.93 ± 6.01 (AQ) | A negative relationship at the .1 level (p = .055) was demonstrated between anxiety and self-compassion; participants who felt anxious were less likely to be self-compassionate. The results also illustrated a significant regression coefficient for self-compassion and shame (β = -1.615, SE = .515, t = -3.138, p = .003). This provides evidence that as the levels of self-compassion increased, shame decreased |
| Self-awareness perceived responsibility | 23.48 ± 32.89 | |||
| Shame and guilt scale | 11.51 ± 4.82 (shame) | |||
| Hospital Anxiety and Depression Scale | 9.29 ± 5.24 (anxiety); 7.67 ± 4.09 (depression) | |||
| Arambasic, Sherman, and Elder [17] | 2019 | General attachment style | Attachment avoidance: 3.12 ± 1.11; attachment anxiety: 2.51 ± 1.05 | Both attachment anxiety and attachment avoidance negatively correlated with self-compassion |
| Self-compassion | 3.46 ± 0.57 | |||
| Psychological adjustment (negative impact of cancer) | 2.76 ± 0.77 | |||
| Brown et al. [18] | 2019 | Self-Compassion Scale | Self-kindness: 2.74 ± 0.94 | Self-compassion subscales demonstrated a negative correlation with HADS, depression, and anxiety, although only smaller correlations were observed between common humanity than self‐kindness and mindfulness subscales. The final model included structural paths that showed that kindness and mindfulness scores, but not common humanity, uniquely predicted reduced brooding, depressive brooding, and worry |
| Common humanity: 3.11 ± 0.93 | ||||
| Mindfulness: 3.18 ± 0.83 | ||||
| Reflection: 1.70 ± 0.61 | ||||
| Hospital Anxiety and Depression Scale | HADS anxiety: 8.33 ± 4.59 | |||
| Ruminative Response Scale | HADS depression: 5.50 ± 4.01 | |||
| Penn State Worry Scale | Worry: 3.19 ± 0.90 | |||
| Dowd and Jung [19] | 2017 | Celiac Dietary Adherence Test | Baseline: 11.78 ± 3.22; after: 11.18 ± 2.68 | Both self-compassion and self-regulatory efficacy at time 1 had a direct relationship with the prediction of adherence to GFD at time 2. Self-compassion directly predicted celiac QoL |
| Self-Compassion Scale | Baseline: 3.34 ± 0.75, After: 3.38 ± 0.76 | |||
| Celiac QoL | After: 2.54 ± 0.80 | |||
| Self-Regulatory Efficacy Scale | Baseline: 95.30 ± 8.85; after: 95.90 ± 8.94 | |||
| Edwards et al. [20] | 2019 | Self-Compassion Scale | 75.90 ± 20.03 | Self‐compassion accounted for a significant and unique amount of variance in physical and psychosocial disability, depression, pain acceptance, success in valued activities, use of traditional pain coping strategies, use of flexible pain coping strategies, and pain anxiety |
| Sickness Impact Profile | 0.24 ± 0.21 (physical) | |||
| 0.25 ± 0.20 (psychosocial) | ||||
| BC Major Depression Inventory | 28.43 ± 16.33 | |||
| Chronic pain questionnaire | 47.40 ± 19.26 | |||
| Pain Anxiety Symptom Scale | 45.88 ± 22.22 | |||
| Friis et al. [21] | 2015 | PHQ-9 | 6.8 ± 5.6 | As self-compassion increased, depression and diabetes-distress scores decreased. A positive relationship between distress and HbA1c among persons with lower self-compassion |
| Diabetes Distress Scale | 6.3 ± 2.7 | |||
| Self-Compassion Scale | 80 ± 16.8 | |||
| Friis et al. [22] | 2016 | Self-Compassion Scale | Pre-control SCS: 2.88 ± 0.60 | Self-compassion increased in the MSC group between T1 and T2, with gains maintained at T3 |
| Post-control SCS: 3.12 ± 0.64 | ||||
| Pre-experiment SCS: 2.52 ±0.57 | ||||
| Post-experiment SCS: 3.10 ± 0.50 | ||||
| PHQ-9 | Pre-control PHQ-9: 9.74 ± 6.06 | The intervention reduced depression scores in the MSC group between T1 and T2, with results maintained at T3 | ||
| Post-control PHQ-9: 7.30 ± 5.02 | ||||
| Pre-experiment PHQ-9: 14.01 ± 4.52 | ||||
| Post-experiment PHQ-9: 9.16 ± 6.50 | ||||
| DDS17 | Pre-control DDS17: 2.35 ± 0.63 | |||
| Post-control DDS17: 2.29 ± 0.85 | ||||
| Pre-experiment DDS17: 3.16 ± 0.88 | ||||
| Post-experiment DDS17: 2.33 ± 0.86 | ||||
| Hayter and Dorstyn [23] | 2013 | CD-RISC 10 scale | 25.65 ± 8.07 | Increased self-compassion was associated with lower levels of depression, anxiety, and stress |
| Self-Compassion Scale | 18.04 ± 3.90 | |||
| Self-esteem | 18 ± 5.43 | |||
| Depression | 11.92 ± 11.59 | |||
| Anxiety | 9.36 ± 9.39 | |||
| Stress | 13.90 ± 10.18 | |||
| Karami et al. [24] | 2018 | NA | NA | NA |
| Klein et al. [25] | 2020 | Self-Compassion Scale | 3.45 ± 0.72 | Hope and self-compassion together predicted physical and psychosocial QOL. Hope stood as the primary significant predictor of all three QOL scores |
| Adult Hope Scale | 53.3 ± 7.00 | |||
| QoL | 75.92 ± 16.62 | |||
| Morrison et al. [26] | 2019 | Self-Compassion Scale | 3.29 ± 0.69 | A negative correlation was found between levels of SCS and both depressive symptoms (PHQ-9) and diabetes distress (DDS-17) |
| PHQ-9 | 5.4 ± 6.5 | |||
| DDS-17 | 1.84 ± 0.90 | |||
| Ferrari, Dal Cin, and Steele [27] | 2017 | Self-Compassion Scale-Short-Form | NA | Self-compassion was correlated with higher well-being, lower HbA1c, higher self-management behaviors, and adherence to diet and exercise |
| Diabetes Self-Management Questionnaire | ||||
| Well-being questionnaire | ||||
| Hurwit, Yun, and Ebbeck [28] | 2018 | Resilience | 3.60 ± 0.64 | Self-compassion had a significant positive relationship with HRQoL and resilience. A similar relationship was found between resilience and HRQoL |
| Self-Compassion Scale | 3.32 ± 0.76 | |||
| Health-related QoL | 4.89 ± 1.24 | |||
| Baillargeon et al. [29] | 2018 | Self-Compassion Scale | 2.81 ± 0.61 | Women’s higher self-compassion was associated with their own lower anxiety and depression. Self-compassion was not associated with their own sexual distress |
| Spielberger Trait Anxiety Scale | 43.92 ± 9.60 | |||
| Beck Depression Inventory-II | 10.69 ± 6.25 | |||
| Female Sexual Distress Scale | 33.48 ± 9.83 | |||
| Skelton et al. [30] | 2020 | Self-Compassion Scale | 64.12 ± 19.48 (compassionate engagement and action) | Self-compassion was not associated with adherence behavior, shame, or quality of life |
| Experience of Shame Scale | 49.71 ± 20.68 | |||
| Adherence to Medication and Refill Scale | 17.87 ± 5.67 | |||
| QoL-HIV | 40.30 ± 22.63 | |||
| Vasigh et al. [31] | 2019 | Mindfulness questionnaire | 53.33 ± 4.69 | There was no relationship between self-compassion and pain |
| Self-Compassion Scale | 71.48 ± 4.85 | |||
| Numeric rating scale | 3.33 ± 1.75 | |||
| Wren et al. [32] | 2012 | Self-Compassion Scale | 19.37 ± 4.12 | There was a correlation between self-compassion and pain self-efficacy, pain disability, negative, and positive affect |
| Pain intensity | 65.95 ± 26.16 | |||
| Positive and Negative Affect scale | Positive: 2.79 ± 0.89 | |||
| Negative: 1.75 ± 0.85 | ||||
| Pain Disability Index | 35.89 ± 11.41 | |||
| Pain Self-Efficacy Questionnaire | 43.17 ± 16.42 | |||
| Zhu et al. [33] | 2018 | Self-Compassion Scale | 39.7 ± 6.49 | Self‐compassion total score at T1 was negatively associated with symptoms of depression, anxiety, and fatigue at T2 |
| PHQ-9 | Baseline: 7.27 ± 5.74 | |||
| After: 8.11 ± 6.47 | ||||
| Checklist Individual Strength | Baseline: 78.57 ± 23.88 | |||
| After: 79.12 ± 20.81 | ||||
| State-Trait Anxiety Inventory | Baseline: 14.44 ± 4.14 | |||
| After: 14.49 ± 3.89 |
Important Correlations
All included studies evaluated the correlation of self-compassion with other important psychosocial outcomes such as depression, anxiety, stress, resilience, shame, quality of life, and other outcomes as shown in Table 2. Nine studies evaluated the correlation between self-compassion and depression [16,18,20-23,26,29,33]. All studies found that a higher self-compassion was correlated with lower levels of depression in individuals with a medical illness. Four of these studies looked specifically at self-compassion scores in relation to the Patient Health Questionnaire-9 (PHQ-9) scores, which found that increased SCS scores were associated with decreased levels of PHQ-9 scores [21,22,26,33]. Moreover, two studies looked at self-compassion in relation to the Hospital Anxiety and Depression Scale (HADS) questionnaire and demonstrated similar results [16,18]. Five studies looked at the correlation between self-compassion and anxiety, two of which were previously discussed using the HADS questionnaire. The rest of the three studies used different types of questionnaires but revealed that self-compassion scores were negatively correlated with anxiety [23,29,33].
Two studies looked at the relationship between self-compassion and shame [16,30]. One study showed that as self-compassion levels increased, shame decreased, while the other study showed no correlation between self-compassion and shame. Four studies looked at the correlation between self-compassion and quality of life [19,21,28,30]. Two studies showed that increased self-compassion improved quality of life, while two studies showed that higher levels of self-compassion correlate with any improvement [19,21,28,30]. Four studies investigated correlations between self-compassion and levels of stress [21-23,26]. Three of the four studies looked at self-compassion and Diabetes Distress Scores (DDS-17) and demonstrated that as self-compassion increased, DDS decreased [21,22,26]. The other study demonstrated that higher self-compassion levels correlated with lower stress levels [23]. One study by Hurwit, Yun, and Ebbeck demonstrated that higher self-compassion is associated with higher resilience [28]. Furthermore, the self-compassion interventions are likely to be more effective with women, as they have previously been reported to have lower self-compassion levels than men [6]. Lastly, two studies investigated the link between self-compassion and adherence behavior [19,30]. Skelton et al. demonstrated that self-compassion was not associated with increased adherence behavior in HIV patients [30]. On the other hand, Dowd and Jung exhibited that self-compassion at baseline was able to predict adherence to a gluten-free diet in celiac patients [19].
Clinical Outcomes
Only two studies investigated the effect of self-compassion on clinical outcomes specifically for diabetes with HbA1c and blood glucose levels, as shown in Table 3 [22,24]. Karami et al. demonstrated an improvement in blood glucose levels in patients who were in the intervention group (self-compassion program) compared to the control group at baseline and after the completion of the intervention [24]. The control group had a glucose level of 271 ± 35.88 at baseline compared to 272.75 ± 21.96 for the experimental group [24]. Post-intervention (after eight weeks), the control group had glucose levels of 267 ± 28.98 compared to 205.25 ± 12.55 for the experimental group [24]. Similarly, the other study by Friis et al. aimed to compare HbA1c levels between the control group and the experimental group [22]. They demonstrated that HbA1c levels improved after the intervention and at the three-month follow-up significantly in the experimental group (baseline: 74.25 ± 15.11; post-intervention: 71.44 ± 18.34; follow-up: 64.03 ± 16.25) compared to the control group (baseline: 64.04 ± 13.32; post-intervention: 66.03 ± 14.20; follow-up: 62.32 ± 12.41) [22].
Table 3. Effect of self-compassion on clinical outcomes.
| Studies | Year | Parameter | Clinical outcomes |
| Karami et al. [24] | 2018 | Blood glucose levels | Pre-control: 271 ± 35.88 |
| Post-control: 267 ± 28.98 | |||
| Pre-experimental: 272.75 ± 21.96 | |||
| Post-experimental: 205.25 ± 12.55 | |||
| Friis et al. [22] | 2016 | HbA1c (mmol/mol) | Pre-control: 64.04 ± 13.32 |
| Post-control: 66.03 ± 14.20 | |||
| Follow-up: 62.32 ± 12.41 | |||
| Pre-experimental: 74.25 ± 15.11 | |||
| Post-experimental: 71.44 ± 18.34 | |||
| Follow-up: 64.03 ± 16.25 |
Discussion
This systematic review included 19 studies involving 2,713 patients suffering from a variety of medical illnesses. The psychosocial outcomes of self-compassion scores were low and correlated with other parameters such as depression, anxiety, stress, shame, resilience, and quality of life. Moreover, two studies demonstrated the positive impact of incorporating a self-compassion-based intervention in disease management.
In previous studies, higher levels of self-compassion have been linked to lower levels of stress, depression, and anxiety [34,35]. For example, a group of healthy females was subjected to a high-stress task, and those who were trained in self-compassion were found to have lower sympathetic nervous system response compared to the placebo group [36]. Similarly, in another study that investigated the relationship between self-compassion and depression in a German cohort of 2,404 healthy individuals, Korner and colleagues used the PHQ-9 questionnaire to determine depression symptoms and demonstrated that increased depression correlated with lower SCS total scores and subscores [37]. After a logistic regression was performed and variables were adjusted, the model showed that 23% of the variance in depression symptoms was explained by SCS [37]. Therefore, self-compassion was shown to be a protective factor against depression [37]. Self-compassion has been demonstrated to have great implications on psychological well-being in chronic diseases given the contribution of psychological parameters in the exacerbation of diseases.
Another important role of self-compassion in medical disease management is related to the increase in health-promoting behaviors. Self-management behaviors have long been a central component of symptom management and improving disease trajectory and outcomes in chronic conditions [38]. The recent 2019 novel coronavirus pandemic has affected all spheres of health. Mental health has been no exception and resultant cognitive distress, anxiety, and fear of being out in public have been reported [39]. Self-compassion may prove to be quite an effective tool in managing these.
Previous studies have also demonstrated an association between self-compassion and self-management behaviors [3,4]. A meta-analysis by Sirois pooled 3,252 individuals across 15 studies and found that higher self-compassion was positively correlated to better engagement in health-promoting behaviors for chronic diseases [40]. These behaviors included better stress management, adherence to medication, lifestyle modifications, and improved sleep quality. This was consistent with data in our review, which demonstrated that in one of the two studies, self-management behaviors increased with increasing self-compassion.
Self-compassion-based training and interventions have been linked to better clinical outcomes in individuals experiencing medical illnesses. These interventions include compassion-focused therapy (CFT) and compassionate mind training (CMT) [41]. Previous studies have demonstrated success in these targeted interventions in providing acceptance and care for oneself by practicing health-promoting behaviors [42]. A review by Leaviss and Uttley, which included 14 studies, demonstrated that CFT is an effective intervention particularly in individuals prone to high self-criticism [43]. Although limited data exist in the role of self-compassion in improving clinical outcomes, there have been promising outcomes in the effect of self-compassion therapy in the improvement of treatment of medical conditions [44,45]. As shown by two studies in this review, self-compassion intervention compared to placebo can truly affect clinical outcomes in diabetes parameters such as HbA1c and blood glucose levels [22,24].
In this review, the studies examined the effect of self-compassion on clinical diabetic outcomes in the short-term, for a period of three months. There is a growing body of evidence that self-compassion interventions need to be provided through multiple sessions for at least 12 weeks to yield any differences in both psychosocial and clinical outcomes [46]. A study by Philips and Hine underlined the importance of a multi-session self-compassion intervention to impact self-management behaviors, improve psychological outcomes, and enhance physical health [46]. Thus, combining a self-compassion intervention with multiple sessions for a duration of more than six months can enhance the magnitude of self-compassion in its influence on disease management of individuals with medical illnesses.
The introduction of self-compassionate intervention is only the start in this realm; however, the practice of self-compassion by healthcare workers is necessary to maximize the impact of such an intervention. Studies have demonstrated that workers in the healthcare industry can affect the behaviors of patients [47]. Therefore, it is crucial to foster a compassionate setting to promote better communication, understanding, and disease management in patients [48,49]. This ongoing training and support will cultivate an environment that will enhance the patients' sense of self-efficacy and compassion toward themselves and thus improve their attitude towards engaging in health-promoting behaviors [50].
This study has several limitations. Firstly, the study only included publications in the English language. Secondly, there was significant variability in data presentation between studies. For example, the questionnaires used for each study varied. Moreover, even though the same self-compassion questionnaire was used, each study had calculated the scores differently by removing various items from the questionnaire. As such, this hindered our ability to conduct a meta-analysis and grasp the extent of the effects of self-compassion on psychosocial and clinical outcomes. Finally, only two of the included studies reported the role of self-compassion intervention on clinical outcomes, thus limiting our ability to identify whether using a self-compassion program can affect clinical outcomes and disease trajectory in medically ill individuals.
Conclusions
In conclusion, this systematic review highlights the role of self-compassion with respect to its correlation and effect on psychosocial outcomes. Moreover, albeit the small sample size, this study showed the significance of the integration of a self-compassion program in the management of medical illnesses. Therefore, there is a dire need for the use of self-compassion as a tool to tackle the treatment of diseases. Further studies are needed to evaluate long-term outcomes of a self-compassion-based intervention to highlight its importance in the role of disease management.
Appendices
Table 4. Search strategy used.
CINAHL: Cumulative Index to Nursing and Allied Health Literature
| Search strategy employed in our review | ||||
| S5 | S3 NOT (S4 OR TI child* OR TI youth OR TI adolesc* OR TI teen*) | Expanders - apply equivalent subjects; search modes - boolean/phrase | Interface - EBSCOhost Research Databases; search screen - basic; search database - CINAHL with Full Text | 472 |
| S4 | (MH "Child+") NOT (MH "Adult+") | Expanders - apply equivalent subjects; search modes - boolean/phrase | Interface - EBSCOhost Research Databases Search Screen - Basic Search Database - CINAHL with Full Text | 503,536 |
| S3 | S1 AND S2 AND (TI(regulat* OR self-compassion*) OR AB(regulat* OR self-compassion*)) AND (therap* OR treat* OR heal OR healing OR health OR recover* OR restor* OR recuperat*) | Limiters - English Language; publication type - journal article; expanders - apply equivalent subjects; search modes - boolean/phrase | Interface - EBSCOhost Research Databases Search Screen - Basic Search Database - CINAHL with Full Text | 570 |
| S2 | (MH "Disease Management+" OR MH "Disease+" OR MH "Psychosocial Aspects of Illness+" OR MH "Severity of Illness" OR MH "Attitude to Illness+" OR disease* OR illness* OR chronic* OR disorder* OR patient OR patients OR condition OR conditions OR MH "Sexually Transmitted Diseases+" OR MH "Immunologic Diseases+" OR MH "Endocrine Diseases+" OR (MH "Nutritional and Metabolic Diseases+" OR MH "Skin and Connective Tissue Diseases+" OR MH "Congenital, Hereditary, and Neonatal Diseases and Abnormalities+" OR MH "Hemic and Lymphatic Diseases+" OR MH "Cardiovascular Diseases+" OR MH "Female Urogenital Diseases and Pregnancy Complications+" OR MH "Male Urogenital Diseases+" OR MH "Eye Diseases+" OR MH "Nervous System Diseases+" OR MH "Otorhinolaryngologic Diseases+" OR MH "Respiratory Tract Diseases+" OR MH "Stomatognathic Diseases+" OR MH "Digestive System Diseases+" OR MH "Musculoskeletal Diseases+" OR MH "Neoplasms+" OR MH "Virus Diseases+" OR MH "Parasitic Diseases+" OR MH "Bacterial and Fungal Diseases+" OR MH "Symptoms and General Pathology+") | Expanders - apply equivalent subjects; search modes - boolean/phrase | Interface - EBSCOhost Research Databases Search Screen - Basic Search Database - CINAHL with Full Text | 4,324,677 |
| S1 | (MH "Self Regulation+" or self-compassion*) | Expanders - apply equivalent subjects; search modes - boolean/phrase | Interface - EBSCOhost Research Databases Search Screen - Basic Search Database - CINAHL with Full Text | 6,852 |
Table 5. NIH Quality Assessment Tool.
NIH: National Institutes of Health; NA: not applicable
| Criterion | Abdollahi, Taheri, and Allen | Ambridge, Fleming, and Henshall | Arambasic, Sherman, and Elder | Brown et al. | Dowd and Jung | Edwards et al. | Friis et al. | Friis et al. | Hayter and Dorstyn | Karami et al. | Klein et al. | Morrison et al. | Ferrari, Dal Cin, Steele | Hurwit, Yun, and Ebbeck | Baillargeon et al. | Skelton et al. | Vasigh et al. | Wren et al. | Zhu et al. |
| 1. Was the research question or objective in this paper clearly stated? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2. Was the study population clearly specified and defined? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 3. Was the participation rate of eligible persons at least 50%? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 5. Was a sample size justification, power description, or variance and effect estimates provided? | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No |
| 6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)? | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No |
| 9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 10. Was the exposure(s) assessed more than once over time? | No | No | No | No | Yes | No | No | Yes | No | Yes | No | No | No | No | No | No | No | No | Yes |
| 11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 12. Were the outcome assessors blinded to the exposure status of participants? | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 13. Was loss to follow-up after baseline 20% or less? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Figure 1. PRISMA 2009 Flow Diagram.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
Footnotes
The authors have declared that no competing interests exist.
References
- 1.Self-regulation and chronic pain: the role of emotion. Hamilton NA, Karoly P, Kitzman H. Cognit Ther Res. 2004;28:559–576. [Google Scholar]
- 2.Perceived stress as a risk factor for changes in health behaviour and cardiac risk profile: a longitudinal study. Rod NH, Grønbaek M, Schnohr P, Prescott E, Kristensen TS. J Intern Med. 2009;266:467–475. doi: 10.1111/j.1365-2796.2009.02124.x. [DOI] [PubMed] [Google Scholar]
- 3.Self-compassion, stress, and coping in the context of chronic illness. Sirois FM, Molnar DS, Hirsch JK. Self Identity. 2014;14:334–347. [Google Scholar]
- 4.A systematic review of the efficacy of interventions that aim to increase self-compassion on nutrition habits, eating behaviours, body weight and body image. Rahimi-Ardabili H, Reynolds R, Vartanian LR, McLeod LV, Zwar N. Mindfulness. 2017;9:1–13. [Google Scholar]
- 5.Baumeister RF, Zell AL, Tice DM. Handbook of Emotion Regulation. Vol. 1. New York, NY: The Guilford Press; 2007. How emotions facilitate and impair self regulation; pp. 408–426. [Google Scholar]
- 6.The development and validation of a scale to measure self-compassion. Neff KD. Self Identity. 2003;2:223–250. [Google Scholar]
- 7.The role of self-compassion in development: a healthier way to relate to oneself. Neff KD. Hum Dev. 2009;52:211–214. doi: 10.1159/000215071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Self-compassion versus global self-esteem: two different ways of relating to oneself. Neff KD, Vonk R. J Pers. 2009;77:23–50. doi: 10.1111/j.1467-6494.2008.00537.x. [DOI] [PubMed] [Google Scholar]
- 9.Neff KD. Self compassion. London, UK: Hodder & Stoughton; 2013. Self Compassion. [Google Scholar]
- 10.Exploring compassion: a meta-analysis of the association between self-compassion and psychopathology. MacBeth A, Gumley A. Clin Psychol Rev. 2012;32:545–552. doi: 10.1016/j.cpr.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 11.Self-compassion and psychological resilience among adolescents and young adults. Neff KD, McGehee P. Self Identity. 2010;9:225–240. [Google Scholar]
- 12.Self-compassion and adaptive psychological functioning. Neff KD, Kirkpatrick KL, Rude SS. J Res Pers. 2007;41:139–154. [Google Scholar]
- 13.Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [Aug;2020 ];http://www.prisma-statement.org 2020
- 14.NIH quality assessment tool for observational cohort and cross-sectional studies. [Aug;2020 ];https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools 2020
- 15.Self‐compassion moderates the perceived stress and self‐care behaviors link in women with breast cancer. Abdollahi A, Taheri A, Allen KA. Psychooncology. 2020;29:927–933. doi: 10.1002/pon.5369. [DOI] [PubMed] [Google Scholar]
- 16.The influence of self-compassion on perceived responsibility and shame following acquired brain injury. Ambridge J, Fleming P, Henshall L. Brain Inj. 2020;34:945–957. doi: 10.1080/02699052.2020.1763466. [DOI] [PubMed] [Google Scholar]
- 17.Attachment styles, self-compassion, and psychological adjustment in long-term breast cancer survivors. Arambasic J, Sherman KA, Elder E; Breast Cancer Network Australia. Psychooncology. 2019;28:1134–1141. doi: 10.1002/pon.5068. [DOI] [PubMed] [Google Scholar]
- 18.Could worry and rumination mediate relationships between self-compassion and psychological distress in breast cancer survivors? Brown SL, Hughes M, Campbell S, Cherry MG. Clin Psychol Psychother. 2020;27:1–10. doi: 10.1002/cpp.2399. [DOI] [PubMed] [Google Scholar]
- 19.Self-compassion directly and indirectly predicts dietary adherence and quality of life among adults with celiac disease. Dowd AJ, Jung ME. Appetite. 2017;113:293–300. doi: 10.1016/j.appet.2017.02.023. [DOI] [PubMed] [Google Scholar]
- 20.The relation of self-compassion to functioning among adults with chronic pain. Edwards KA, Pielech M, Hickman J, Ashworth J, Sowden G, Vowles KE. Eur J Pain. 2019;23:1538–1547. doi: 10.1002/ejp.1429. [DOI] [PubMed] [Google Scholar]
- 21.Does kindness matter? Self-compassion buffers the negative impact of diabetes-distress on HbA1c. Friis AM, Johnson MH, Cutfield RG, Consedine NS. Diabet Med. 2015;32:1634–1640. doi: 10.1111/dme.12774. [DOI] [PubMed] [Google Scholar]
- 22.Kindness matters: a randomized controlled trial of a mindful self-compassion intervention improves depression, distress, and HbA1c among patients with diabetes. Friis AM, Johnson MH, Cutfield RG, Consedine NS. Diabetes Care. 2016;39:1963–1971. doi: 10.2337/dc16-0416. [DOI] [PubMed] [Google Scholar]
- 23.Resilience, self-esteem and self-compassion in adults with spina bifida. Hayter MR, Dorstyn DS. Spinal Cord. 2014;52:167–171. doi: 10.1038/sc.2013.152. [DOI] [PubMed] [Google Scholar]
- 24.Effectiveness of self-compassion intervention training on glycemic control in patients with diabetes. Karami J, Rezaei M, Karimi P, Rafiee Z. J Kermanshah Univ Med Sci. 2018;22:1. [Google Scholar]
- 25.The relationship of self‐compassion and hope with quality of life for individuals with bleeding disorders. Klein DE, Winterowd CL, Ehrhardt MD, Carter JC, Khan O, Mayes S. Haemophilia. 2020;26:4–6. doi: 10.1111/hae.13959. [DOI] [PubMed] [Google Scholar]
- 26.Self-compassion, metabolic control and health status in individuals with type 2 diabetes: a UK observational study (Epub ahead of print) Morrison AE, Zaccardi F, Chatterjee S, et al. Exp Clin Endocrinol Diabetes. 2019 doi: 10.1055/a-0897-3772. [DOI] [PubMed] [Google Scholar]
- 27.Self-compassion is associated with optimum self-care behaviour, medical outcomes and psychological well-being in a cross-sectional sample of adults with diabetes. Ferrari M, Dal Cin M, Steele M. Diabet Med. 2017;34:1546–1553. doi: 10.1111/dme.13451. [DOI] [PubMed] [Google Scholar]
- 28.Examining the roles of self-compassion and resilience on health-related quality of life for individuals with Multiple Sclerosis. Nery-Hurwit M, Yun J, Ebbeck V. Disabil Health J. 2018;11:256–261. doi: 10.1016/j.dhjo.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 29.Does self-compassion benefit couples coping with vulvodynia? Associations with psychological, sexual, and relationship adjustment. Santerre-Baillargeon M, Rosen NO, Steben M, Pâquet M, Macabena Perez R, Bergeron S. Clin J Pain. 2018;34:629–637. doi: 10.1097/AJP.0000000000000579. [DOI] [PubMed] [Google Scholar]
- 30.The role of self-compassion and shame in persons living with HIV/AIDS (Epub ahead of print) Skelton WM, Cardaciotto L, O'Hayer CV, Goldbacher E. AIDS Care. 2020 doi: 10.1080/09540121.2020.1769836. [DOI] [PubMed] [Google Scholar]
- 31.The relationship between mindfulness and self-compassion with perceived pain in migraine patients in Ilam, 2018. Vasigh A, Tarjoman A, Soltani B, Borji M. Arch Neurol. 2019;6:2–4. [Google Scholar]
- 32.Self-compassion in patients with persistent musculoskeletal pain: relationship of self-compassion to adjustment to persistent pain. Wren AA, Somers TJ, Wright MA, et al. J Pain Symptom Manage. 2012;43:759–770. doi: 10.1016/j.jpainsymman.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 33.The predictive role of self-compassion in cancer patients' symptoms of depression, anxiety, and fatigue: a longitudinal study. Zhu L, Yao J, Wang J, et al. Psychooncology. 2019;28:1918–1925. doi: 10.1002/pon.5174. [DOI] [PubMed] [Google Scholar]
- 34.Self-compassion in depression: associations with depressive symptoms, rumination, and avoidance in depressed outpatients. Krieger T, Altenstein D, Baettig I, Doerig N, Holtforth MG. Behav Ther. 2013;44:501–513. doi: 10.1016/j.beth.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 35.Self-compassion and physical health: exploring the roles of perceived stress and health-promoting behaviors. Homan KJ, Sirois FM. Health Psychol Open. 2017;4:2055102917729542. doi: 10.1177/2055102917729542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Arch JJ, Brown KW, Dean DJ, Landy LN, Brown KD, Laudenslager ML. Psychoneuroendocrinology. 2014;42:49–58. doi: 10.1016/j.psyneuen.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.The role of self-compassion in buffering symptoms of depression in the general population. Körner A, Coroiu A, Copeland L, Gomez-Garibello C, Albani C, Zenger M, Brähler E. PLoS One. 2015;10:0. doi: 10.1371/journal.pone.0136598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Self-management: a comprehensive approach to management of chronic conditions. Grady PA, Gough LL. Am J Public Health. 2014;104:0–31. doi: 10.2105/AJPH.2014.302041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Focus on mental health during the coronavirus (COVID-19) pandemic: applying learnings from the past outbreaks. Shah K, Kamrai D, Mekala H, Mann B, Desai K, Patel RS. Cureus. 2020;12:0. doi: 10.7759/cureus.7405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Procrastination and stress: exploring the role of self-compassion. Sirois FM. Self Identity. 2014;13:128–145. [Google Scholar]
- 41.Hoboken: Taylor and Francis. Vol. 1. Abingdon, UK: Routledge; 2014. Genes on the Couch: Explorations in Evolutionary Psychotherapy; p. 0. [Google Scholar]
- 42.Who benefits from training in self-compassionate self-regulation? A study of smoking reduction. Kelly AC, Zuroff DC, Foa CL, Gilbert P. J Soc Clin Psychol. 2010;29:727–755. [Google Scholar]
- 43.Psychotherapeutic benefits of compassion-focused therapy: an early systematic review. Leaviss J, Uttley L. Psychol Med. 2015;45:927–945. doi: 10.1017/S0033291714002141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.My changed body: breast cancer, body image, distress and self-compassion. Przezdziecki A, Sherman KA, Baillie A, Taylor A, Foley E, Stalgis-Bilinski K. Psychooncology. 2013;22:1872–1879. doi: 10.1002/pon.3230. [DOI] [PubMed] [Google Scholar]
- 45.The protective role of self-compassion in relation to psychopathology symptoms and quality of life in chronic and in cancer patients. Pinto-Gouveia J, Duarte C, Matos M, Fráguas S. Clin Psychol Psychother. 2014;21:311–323. doi: 10.1002/cpp.1838. [DOI] [PubMed] [Google Scholar]
- 46.Self-compassion, physical health, and health behaviour: a meta-analysis (Epub ahead of print) Phillips WJ, Hine DW. Health Psychol Rev. 2019:1–27. doi: 10.1080/17437199.2019.1705872. [DOI] [PubMed] [Google Scholar]
- 47.Developing compassionate leadership in health care: an integrative review. de Zulueta PC. J Healthc Leadersh. 2015;8:1–10. doi: 10.2147/JHL.S93724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Compassion in healthcare - lessons from a qualitative study of the end of life care of people with dementia. Crowther J, Wilson KC, Horton S, Lloyd-Williams M. J R Soc Med. 2013;106:492–497. doi: 10.1177/0141076813503593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Compassion as the foundation of patient-centered care: the importance of compassion in action. Frampton SB, Guastello S, Lepore M. J Comp Eff Res. 2013;2:443–455. doi: 10.2217/cer.13.54. [DOI] [PubMed] [Google Scholar]
- 50.Examining the role of patient experience surveys in measuring health care quality. Anhang Price R, Elliott MN, Zaslavsky AM, et al. Med Care Res Rev. 2014;71:522–554. doi: 10.1177/1077558714541480. [DOI] [PMC free article] [PubMed] [Google Scholar]