ABSTRACT
Coronavirus disease 19 (COVID-19) is caused by SARS-Cov-2 and the manifestations of this infection range from an absence of symptoms all the way up to severe disease leading to death. To estimate the prevalence of past infection in a population, the most readily available method is the detection of antibodies against the virus. This study has investigated the prevalence of anti-SARS-CoV-2 antibodies in outpatients of the Hospital das Clinicas, in Sao Paulo city (Brazil), which is a large university hospital belonging to the public health system that cares for patients with complex diseases who need tertiary or quaternary medical care. Our serological inquiry was carried out for 6 weeks, with once-a-week blood sampling and included 439 patients from several outpatient services. Overall, 61 patients tested positive for anti-SARS-CoV-2 IgG (13.9%); 56.1 % of the patients live in Sao Paulo city, with the remaining living in other towns of the metropolitan area; 32.8% of the patients testing positive for IgG antibodies to SARS-CoV-2 were asymptomatic, 55.7% developed mild or moderate disease and 11.5% had to be hospitalized. The prevalence of SARS-CoV-2 positive serology was lower among patients who had received the seasonal influenza vaccine compared to the ones who did not. These findings may indicate that those individuals care more about health issues, and/or that they have a better access to health care and/or a better quality of health care service. The large proportion of patients who were unaware of having had contact with SARS-CoV-2 deserves attention, reflecting the scarcity of tests performed in the population.
KEYWORDS: COVID-19, Anti-SARS-CoV-2 antibodies, Serological inquiry
INTRODUCTION
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is the causative agent of the ongoing outbreak of coronavirus disease 2019 (COVID-19), that started in Wuhan, China at the end of 2019, and had already killed about 917,000 people worldwide 1 . SARS-CoV-2 are enveloped non-segmented positive-sense RNA viruses belonging to the Coronaviridae family 2 , 3 . Clinical manifestations include a variety of respiratorysymptoms, varying from mild to severe, which are associated with high mortality 4 , 5 .
In Brazil, up to September 12th 2020, more than 4 million cases had been registered, including more than 130 thousand deaths 6 . The community transmission of SARS-CoV-2 is widespread in Brazil, with the city of Sao Paulo as the first epicenter of the disease. The city is surrounded by several neighboring towns, making up the Metropolitan Area of Sao Paulo, with a population estimated at 21.5 million people, where about 500 thousand COVID-19 cases, including 22 thousand deaths, had been registered up to September 2020 7 . In the last household inquiry to monitor the seroprevalence of infection by SARS-CoV-2 virus in adults in the city of Sao Paulo, a seroprevalence of 17.9% was estimated, meaning that more than 1.5 million people had already antibodies to SARS-CoV-2 in the city at that time 8 .
Serological tests to detect IgG antibodies against SARS-CoV-2 play an important role in estimating the true prevalence of the virus in the population, and to identify individuals who are potentially immune to reinfection 9 , especially in countries where testing is scarce, as in Brazil. Furthermore, these are extremely relevant data for planning the resumption of activities in the city.
Additionally, there is also a portion of the population that remains asymptomatic or has only subclinical infection, representing a blind spot for intervention measures to control contagion and track individuals who have already had contact with the virus. Studies have found proportions of asymptomatic people ranging from 4-80% across different populations and exposure rates 10 .
The Hospital das Clinicas of the University of Sao Paulo Medical School is the largest hospital complex in Brazil, receiving thousands of patients every day, both from the city of Sao Paulo and from surrounding areas. We investigated the prevalence of antibodies to SARS-CoV-2 among patients who came for routine tests blood sampling. Data on the patients' age, gender, place of residence and influenza vaccination status were also obtained.
MATERIALS AND METHODS
Patient population and samples collection
We collected blood samples from 439 adult patients followed-up at various outpatient services of the hospital. Patients came to the clinical laboratory to collect samples for routine tests requested by their physicians. We obtained an informed and signed consent to perform the SARS-CoV-2 serological test, in addition to their other exams. Samples were collected on a weekly basis for six consecutive weeks, from June 30th to August 4th, 2020.
The sample size was calculated based on previous results obtained by the hospital clinical pathology laboratory during the validation of the serological tests. The 5% prevalence found in the validation led us to assume a 6% prevalence in our study, with a 95% confidence interval ranging from 3-8% in a study with test power of 80%. As the daily number of patients coming to the laboratory for routine blood drawing was around 300 at that time, and we planned a once-a-week blood samplings, we estimated the sample size at 346, based on the assumptions described above (approximately 70 samples per week, during five consecutive weeks, instead of the six weeks previously planned). Later on, a sixth week was included in the study, resulting in a total of 439 enrolled patients. Blood sampling was carried out always on the same day of the week (on Tuesdays) and the research team was specifically trained to employ a convenient approach to invite the patients to participate in the study. We obtained written informed consent from all pateints, according to the protocol of the Hospital das Clinicas Ethical Committee, following the guidelines of resolution 466/2012 from the National Commission for Ethics in Research with human beings.
Serological tests
Five milliliters of venous blood were drawn from the patients' arms. Then, samples were centrifuged to obtain serum samples that were analyzed by an automated quantitative chemiluminescence assay to determine IgG antibodies titers raised to proteins S1 and S2 of SARS-CoV-2 by using LIAISON® SARS-CoV-2 S1/S2 IgG (DiaSorin S.p.A., Saluggia, Italy). This assay was validated by testing 162 samples, reaching a sensitivity of 97.8% and specificity of 99.1% 14 days after symptoms onset. Samples with inconclusive results and antibody titles between 12 and 15 UA/mL were retested by another electrochemiluminescence immunoassay for the detection of total Ig antibodies (IgM and IgG) directed to the NC protein of SARS-CoV-2, using the Elecsys Anti-SARSCoV-2 Cobas® assay (Roche Diagnostics GmbH, Mannheim, Germany). For this assay, the sensitivity was 90% and specificity about 100% 14 days after symptoms onset.
Statistical analysis
We performed the statistical analysis and graphical representation using the GraphPad Prism (version 8.0.1, GraphPad Software, La Jolla, CA, USA). We used the Student's t test, one-way analysis of variance (ANOVA) and nonparametric Kruskal-Wallis tests for comparison of means and the chi-square test for comparing proportions. The statistical significance was set at p<0.05. We used coordinated geographic data for data mapping, with the aid of the geographic mapping software QGIS (version 3.14.1, Free Software Foundation, Inc., Boston, MA, USA).
RESULTS
Samples collection and gender characteristics of the patients
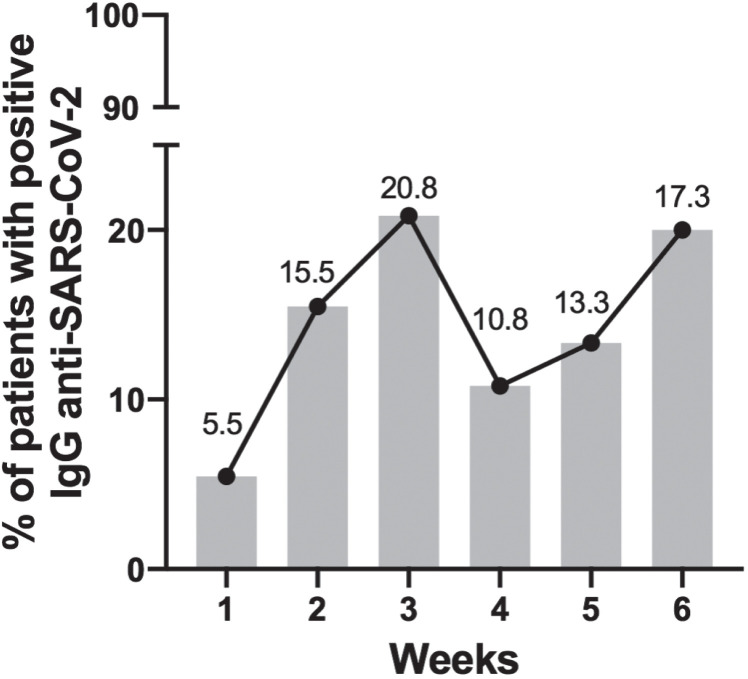
We included 439 outpatients who came for routine laboratory tests, from June 30th to August 4th, 2020, and blood sampling was performed once a week for six consecutive weeks. Serum samples were tested for the presence of anti-SARS-CoV-2 IgG antibodies. Samples with inconclusive results from five patients (1.1%) were retested with a different serological kit, this time for detecting total antibody titles raised to SARS-CoV-2. Four of them proved to be non-reactive and one turned out to be reactive. For convenience, henceforth, we refer to all positive samples as anti-SARS-CoV-2 positive IgG. We found aweekly increase of seroprevalence in the first 3 weeks, an upward trend that did not last for the next three weeks ( Figure 1 ). Overall, 61 patients (13.9%) tested positive for antibodies anti-SARS-CoV-2; 64.5% of our sample was composed of female patients, but this gender proportion was lower among those testing positive to anti-SARS-CoV-2 IgG antibodies that was 57.4 % ( Table 1 ).
Figure 1. Weekly seropositivity for SARS-CoV-2. Percentage of positive patients for IgG anti-SARS-CoV-2, according to each week of the survey.
Table 1. Distribution of the studied patients according to the gender.
| Positive | Negative | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| anti-SARS-CoV-2 IgG | anti-SARS-CoV-2 IgG | |||||||
| 61 (13.9) | 378 (86.1) | 439 | ||||||
| Male | Female | Male | Female | Male | Female | |||
| 26 (42.6) | 35 (57.4) | 130 (34.4) | 248 (65.6) | 156 (35.5) | 283 (64.5) | |||
Distribution of cases by age group
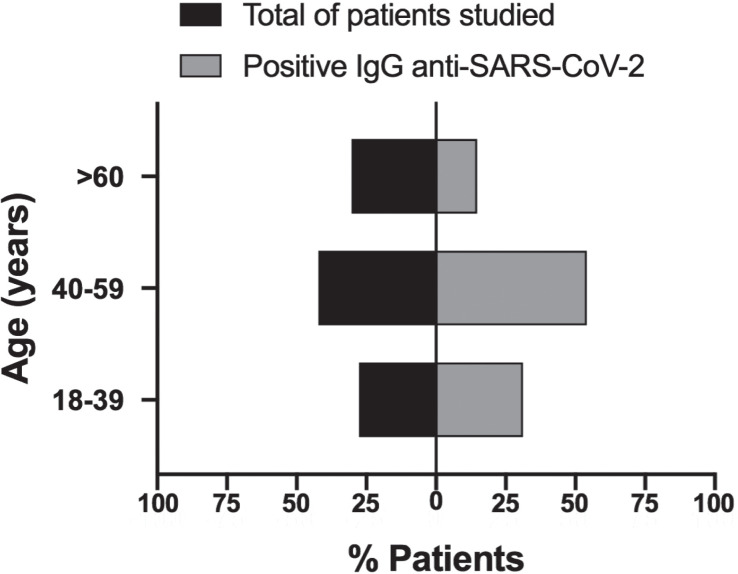
All adulthood age groups were represented in our sample, with the following distribution: 27.6% in the age group 18-39 years old; 42.1% in the group 40-59 years and 30.3% in those ≥ 60 years old. The age group profile of positive anti-SARSCoV-2 IgG patients, in turn, was slightly higher in the group 18-39 years (31.2%), and 54.1% in the 40-59 group. Patients aged 60 years and over represented only 14.8% of the anti-SARS-CoV-2 positive IgG patients, showing a decrease of 50% in the proportional participation of this age group as compared with that of the whole sample ( Figure 2 ).
Figure 2. Distribution of patients according to age groups (years). Patients were analyzed according to the different age groups. On the left is the total number of studied patients; on the right, are the postive patients for IgG anti-SARS-CoV-2.
Patients' residence profile
The Hospital das Clinicas complex is a tertiary/ quaternary medical facility that serves patients in the public health system. All medical specialties and subspecialties are present in the complex. Its patients come from all areas of the city of Sao Paulo (divided into sectors), and from its five surrounding subregions that together make up the Metropolitan Area of Sao Paulo.
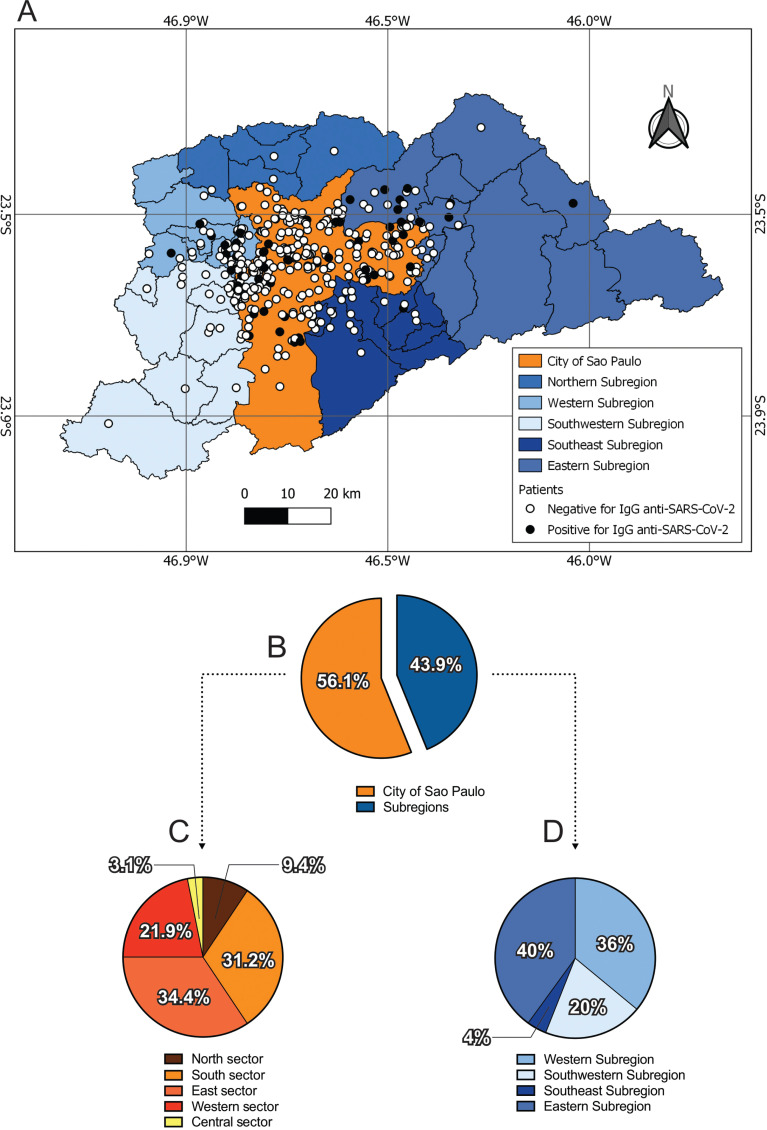
According to Figure 3, among the 439 investigated patients, 56.1% reside in the city of Sao Paulo, while 43.9% live in one of its subregions ( Figures 3A and 3B ). Considering only the patients who live in the city of Sao Paulo, 32/252 or 12.7% presented with positive tests to anti-SARS-CoV-2 IgG antibodies, while among the 152 patients who live in the subregions, 29/152 or 19.1% presented with anti-SARS-CoV-2 IgG antibodies.
Figure 3. Mapping of the origin of patients living in the Metropolitan Area of Sao Paulo. (A) The Metropolitan Area was divided into the city of Sao Paulo and subregions. Negative and positive patients for IgG anti-SARS-CoV-2 were represented by dots. (B, C and D). The percentage of positive patients for IgG anti-SARS-CoV-2 in the city of Sao Paulo and subregions (B); subregions of the Metropolitan Area of Sao Paulo (C); and sectors of the city of Sao Paulo (D).
Concerning the patients who live in the city of Sao Paulo ( Figure 3C ), specific anti-SARS-CoV-2 IgG was found in individuals from all five regions, 34.4% coming from the South sector, 31.2% from the East and 21.9% from the Western sector, whereas the North contributed with 9.4% and the Central sector with 3.1%.
Patients living in the metropolitan area outside the city of Sao Paulo who had positive anti-SARS-CoV-2 antibodies came most from the Eastern subregion (40%), followed by 36% from the Western subregion, whereas 20% and 4% of them live in the Southwestern and Southeastern subregions, respectively. None of the patients from the Northern subregion had antibodies anti-SARS-CoV-2 ( Figure 3D ).
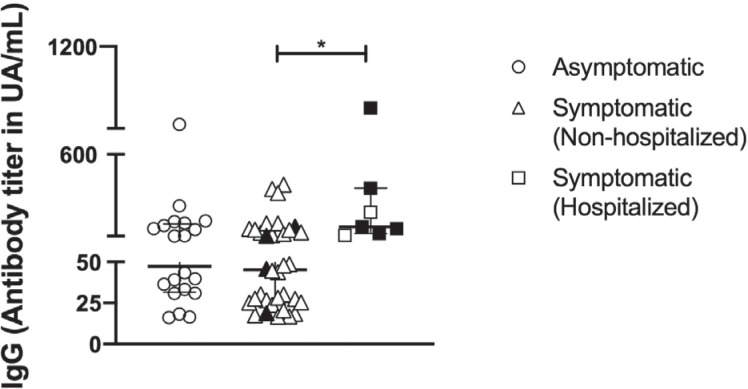
Patients IgG anti-SARS-CoV-2 antibody titers
Sixty-one patients (13.9%), from the total sample of 439 individuals, had positive IgG anti-SARS-CoV-2, and only 2% (9/439) had a previous diagnosis of COVID-19 ( Figure 4, black symbols). Among those presenting with antibodies anti-SARS-CoV-2, 32.8% (20/61) did not report symptoms, 55.7% (34/61) had symptoms of COVID-19 and 11.5% (7/61) were admitted to hospitals. Non-hospitalized patients experienced a variety of symptoms of COVID-19, such as fever or chills, cough, shortness of breathe or respiratory distress, fatigue, muscle or body aches, headache, loss of taste or smell, sore throat, congestion or runny nose, nausea and diarrhea. Hospitalized people related cough, shortness of breath or difficulty breathing, fatigue, muscle or body aches, loss of taste or smell, sore throat, stuffy or runny nose and diarrhea. None of them needed respiratory y support. According to Figure 4 IgG titers among hospitalized patients were significantly higher than those of non-hospitalized ones (p=0.02).
Figure 4. IgG anti-SARS-CoV-2 titers. Patients were divided according to the presence of symptoms into asymptomatic (n: 20) and symptomatic (non-hospitalized n: 34) and hospitalized (n: 7) patients who have already had a previous diagnosis for COVID-19 are shown in black. One-way ANOVA and the non-parametric Kruskal-Wallis test were used for the comparison of groups. *p=0.02.
Patients profile according to influenza vaccination status
We have also investigated whether influenza vaccination status was associated with the serological status for SARS-CoV-2. We did not retrieve information on the vaccination status of four patients, so that, for this analysis, we included a total of 435 patients. We observed that 69% (300/435) of the patients were vaccinated, while 31% (135/435) were not immunized against influenza. Among the vaccinated patients, 11.3% (34/300) were positive for anti-SARS-CoV-2 IgG antibodies, whereas among non-vaccinated patients 20% (27/135) were positive (p=0.016) ( Table 2 ).
Table 2. Association between influenza immunization status and anti-SARS-CoV-2 IgG serological status.
| Positive | Negative | Total | |
|---|---|---|---|
| anti-SARS-CoV-2 IgG | anti-SARS-CoV-2 IgG | ||
| Anti-Influenza vaccinated | 34 (11.3) | 266 (88.7) | 300 |
| Anti-Influenza non-vaccinated | 27 (20.0) | 108 (80.0) | 135 |
| Total | 61 (14.0) | 374 (86.0) | 435 |
Qui-square test=5.8; p=0.016; Odds ratio=0.5121; 95% CI=0.2944 to 0.8737
DISCUSSION
Knowledge on the prevalence of COVID-19 in a population is essential for the adoption of public health actions and reopening decisions, constituting a great challenge in regions where diagnostic tests are scarce, such as in Brazil.
Considering the different symptoms severity scales among infected individuals, ranging from absence of symptoms all the way up to severe manifestations that can lead to death, it is not surprising that a considerable part of the population does not know whether or not they have had contact with the virus. In this context, we proposed to determine the anti-SARS-CoV-2 serological profile of outpatients of the Hospital das Clinicas, a tertiary/ quaternary hospital that serves the population of the Metropolitan Area of Sao Paulo, a location that was the first and the most affected by COVID-19 in Brazil.
We found a prevalence of 16.6%of positive serology to SARS-CoV-2 in men and 12.4 % in women, results that are similar to those found in a study developed in the Northeastern Ceara State (Brazil), that has a also found higher prevalence in men in comparison with women 11 .
During the first three weeks of our study, we found weekly increases on the frequency of positive anti-SARS-CoV-2 IgG antibodies, followed by a decrease and subsequent increment in these frequencies in the last week. In the phase zero of a serological survey in the city of Sao Paulo, samples were collected in the second half of June, and the mean prevalence of antibodies anti-SARS-CoV-2 in the population of the city was 9.5% 12 . At the same time, during the first week of blood sampling in the present study, only 5.5% of our patients were positive, the frequency incresed to 15.5% in the second week and to 20.8% in the third week. Close to this date, results of phase 2 of the serological survey in the city were released, showing a prevalence of 11.1% 12 . In general, our survey in outpatients of the Hospital das Clinicas found a prevalence of 13.9%, while the estimate for the city of Sao Paulo was 10.9% on the same time point of the last week of our study. It is worth noting that our patients were distributed in all groups of adulthood and they came from different regions of the city of Sao Paulo as well as from several neighboring towns surrounding the city.
We found that patients aged 60 years old and over corresponded to 30% of the sample, but only about 15% of them had positive SARS-CoV-2 serology. Considering that patients in that age group are at higher risk for a more severe course of COVID-19, we hypothesize that they were more adherent to the measures to minimize the risk of contagion, such as social distance, use of masks and more rigid hand hygiene.
Focusing on the city of Sao Paulo, we found that the Eastside sector had the highest proportion of positive patients, with 34.4%, followed by the South sector with 31.2% and the Westside one with 21.9%. The Northern and Central sectors had lower prevalences, of only 9.4% and 3.1%. Results of the phase 3 of a serological survey in the city of Sao Paulo 12 showed that, like our findings, the South and East sectors seem to be the most affected ones. It is important to note that in that survey, the distribution of residences was representative of all areas of the city, whereas in our hospital-based survey, the distribution was not fully representative of the whole population of the city.
Another serial seroepidemiological survey on the prevalence of SARS-CoV-2 infection (SoroEpi MSP) 8 in the city of Sao Paulo included 1,470 blood samples collected from July 20th to 29th, and showed that 17.9% of the adult population had already been infected by SARS-CoV-2. Although laboratory test and commercial kits were different between studies and the fact that our data are restricted to samples from the Hospital das Clinicas outpatients, our 13.9%prevalence of seropositivity was not very far from the findings of that study.
We have also investigated a possible association between antibody IgG titers raised to SARS-CoV-2 and the severity of COVID-19 infection. According to our data, IgG titers were higher in hospitalized compared to non-hospitalized patients. Corroborating our findings, several studies have associated higher levels of anti-SARS-CoV-2 antibodies with severity of COVID-19 13 , 14 .
Previous reports have indicated that a substantial fraction of SARS-CoV-2-infected individuals are asymptomatic or present with only mild symptoms 15 – 17 . Data obtained in the present study showed that most studied patients (55.7%) had mild or moderate symptoms of COVID-19. In general, considering that only 2% of our sample had a previous diagnosis of COVID-19 and that almost half of those who presented with positive IgG antibodies anti-SARS-CoV-2 live in neighboring cities, our findings reinforce the notion that the spread of SARS-CoV-2 could be favored by undiagnosed infections.
We have also investigated the seasonal influenza immunization status among our patients. The prevalence of positive serology for SARS-CoV-2 was lower among those who took the vaccine compared to the ones who did not. This finding may indicate that there is a more careful health behavior among vaccinated patients, who cared enough to take the influenza vaccine and they probably pay more attention and avoid practices with a higher risk of SARS-CoV-2 transmission, consequently lowering the proportion of infection and of positive serology to SARS-CoV-2 in this group.
Serological surveys are very useful tools to estimate the proportion of people who may be, at least in part, protected against SARS-CoV-2. It also enables the knowledge on the profile of the most vulnerable individuals, in order to guide public policies aimed at fighting the infection. In our study, we focused on a differentiated population sample, composed of outpatients periodically monitored by the medical team. We observed that the profile of patients of Hospital das Clinicas that have already had contact with the virus is similar to that of the general population of the city of Sao Paulo in terms of the prevalence of seropositivity, gender and place of residence.
We have found a reasonable coverage of influenza immunization and a lower seropositivity among immunized patients as compared to those not vaccinated and also a lower prevalence of anti-SARS-CoV-2 antibodies in the elderly. Both findings indicate that vaccinated individuals care more about health issues, and/or that they have better access and better quality of health care. The large proportion of patients who were unaware of having had contact with the virus is due to the well-known fact that many infected people are asymptomatic and are not tested, with the consequent potential of a further spreading of the virus.
ACKNOWLEDGMENTS
We are grateful to Mrs. Laiza Carla Santos Silva, Mr. Silvio Saez de Oliveira and the entire team of the Collection Section of the Divisao de Laboratorio Central HCFMUSP for their support in interviewing the patients; Dr. Eliana Futata Taniguchi and Dr. Luciana Bento de Souza for their technical support.
Footnotes
FUNDING
This work was supported by Sao Paulo Foundation Research, FAPESP (grant N° 2016/25212-9). LMSO and LTS are recipients of fellowship from FAPESP (grants N° 2019/07976-0 and 2018/12460-0). BTT is recipient of a fellowship from CAPES (grant N° 88887.472042/2019-00). TMO is recipient of a fellowship from CNPq (grant N° 302945/2019-9).
REFERENCES
- 1.World Health Organization WHO Coronavirus disease (COVID-19) dashboard. [cited 2020 Oct 14]. Available from: https://covid19.who.int/
- 2.Fehr AR, Perlman S. Coronaviruses: an overview of their replication and pathogenesis. Methods Mol Biol. 2015;1282:1–23. doi: 10.1007/978-1-4939-2438-7_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rabaan AA, Al-Ahmed SH, Haque S, Sah R, Tiwari R, Malik YS, et al. SARS-CoV-2, SARS-CoV, and MERS-COV: a comparative overview. Infez Med. 2020;28:174–184. [PubMed] [Google Scholar]
- 4.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20:355–362. doi: 10.1038/s41577-020-0331-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brasil. Ministério da Saúde COVID 19: painel Coronavírus. [cited 2020 Oct 14]. Available from: http://covid.saude.gov.br.
- 7.Brasil Ministério da Saúde. Covid-19 no Brasil. [cited 2020 Oct 14]. Available from: https://susanalitico.saude.gov.br/extensions/covid-19_html/covid-19_html.html.
- 8.SoroEpi MSP — Serial soroepidemiological survey to monitor the prevalence of SARS-CoV-2 infection in the Municipality of São Paulo, SP, Brazil Household survey to monitor the seroprevalence of SARS-CoV-2 infection in adults in the City of São Paulo, Brazil: cross-sectional study with probabilistic sampling conducted in the city of São Paulo, Brazil between July 20 and 29, 2020 (21 weeks after the city's first recorded case): phase 3 partial results. [cited 2020 Oct 14]. Available from: https://0dea032c-2432-4690-b1e5-636d3cbeb2bf.filesusr.com/ugd/6b3408_dfe18307a9ae4a99a59c23b1fbd8d8e2.pdf.
- 9.Theel ES, Slev P, Wheeler S, Couturier MR, Wong SJ, Kadkhoda K. The role of antibody testing for SARS-CoV-2: is there one? J Clin Microbiol. 2020;58:e00797-20. doi: 10.1128/JCM.00797-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nikolai LA, Meyer CG, Kremsner PG, Velavan TP. Asymptomatic SARS Coronavirus 2 infection: invisible yet invincible. Int J Infect Dis. 2020;100:112–116. doi: 10.1016/j.ijid.2020.08.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garces TS, Sousa GJ, Florêncio RS, Cestari VR, Pereira ML, Moreira TM. COVID-19 in a state of Brazilian Northeast: prevalence and associated factors in people with flu-like syndrome. J Clin Nurs. 2020 doi: 10.1111/jocn.15472. In Press. [DOI] [PubMed] [Google Scholar]
- 12.São Paulo. Núcleo de Comunicação do Comitê de Crise para o Enfrentamento ao COVID-19 Boletim diário COVID-19: edição 171, 13/09/2020. [cited 2020 Oct 14]. Available from: https://www.prefeitura.sp.gov.br/cidade/secretarias/upload/saude/20200913_boletim_covid19_diario.pdf.
- 13.Zhao J, Yuan Q, Wang H, Liu W, Liao X, Su Y, et al. Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa344. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Long QX, Tang XJ, Shi QL, Li Q, Deng HJ, Yuan J, et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med. 2020;26:1200–1204. doi: 10.1038/s41591-020-0965-6. [DOI] [PubMed] [Google Scholar]
- 15.Wang Y, Liu Y, Liu L, Wang X, Luo N, Li L. Clinical outcomes in 55 patients with severe acute respiratory syndrome Coronavirus 2 who were asymptomatic at hospital admission in Shenzhen, China. J Infect Dis. 2020;221:1770–1774. doi: 10.1093/infdis/jiaa119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kimball A, Hatfield KM, Arons M, James A, Taylor J, Spicer K, et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility - King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:377–381. doi: 10.15585/mmwr.mm6913e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pollán M, Pérez-Gómez B, Pastor-Barriuso R, Oteo J, Hernán MA, Pérez-Olmeda M, et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet. 2020;396:535–544. doi: 10.1016/S0140-6736(20)31483-5. [DOI] [PMC free article] [PubMed] [Google Scholar]