Abstract
When observing diffuse ground‐glass opacities in both lungs, physicians should consider several diseases, including heart failure, interstitial lung diseases, and pulmonary infections. However, brain diseases rarely cause lung infiltration. We present an instructive case of neurologic pulmonary edema showing a pathological link between the brain and the lung.
Keywords: crazy‐paving appearance, dyspnea, meningioma, neurogenic pulmonary edema, seizure
When observing diffuse ground‐glass opacities in both lungs, physicians should consider several diseases, including heart failure, interstitial lung diseases, and pulmonary infections. However, brain diseases rarely cause lung infiltration. We present an instructive case of neurologic pulmonary edema showing a pathological link between the brain and the lung.
1. CASE PRESENTATION
A 56‐year‐old previously healthy woman was transferred to our hospital for seizure of the right upper limb followed by acute‐onset dyspnea. During the 2 days prior to her admission, she experienced a preceded symptom, which was temporary twitching of the right hand lasting for several minutes. On admission, she was conscious and had the following symptoms: blood pressure, 135/70 mm Hg; temperature, 35.9°C; respiratory rate, 48/min; oxygen saturation, 77%; white blood cell count, 7600 cells/μL; C‐reactive protein, 0.21 mg/dL; N‐terminal pro‐brain natriuretic peptide, 74.1 pg/mL (normal range, <125); and KL‐6, 233 U/mL (normal range, <500). Chest computed tomography (CT) revealed diffuse ground‐glass opacities in both lungs (Figure 1A). Autoantibodies including antinuclear antibody (ANA), antineutrophil cytoplasmic antibody (ANCA), rheumatoid factor, anti‐Jo‐1 antibody, and SS‐A/B were all negative. Echocardiography revealed no left heart failure (EF, 65%). The examinations for infection, such as blood/sputum culture, rapid antigen test for influenza virus (nasal swab), Streptococcus pneumoniae (urine), and Legionella pneumophila (urine) were negative. Brain magnetic resonance imaging revealed a left parietal lobe mass (Figure 2); later, pathological examination revealed meningioma. After admission, the patient was treated with positive pressure ventilation and osmotic diuretics. Additionally, her respiratory condition was normalized on the next day, while the abnormal shadows on chest X‐ray disappeared within 2 days. Chest CT performed 5 days after admission confirmed complete disappearance (Figure 1B). She was finally diagnosed as having neurogenic pulmonary edema (NPE) caused by meningioma because other differential diagnoses including heart failure, interstitial lung diseases, pulmonary infections, and collagen diseases were all ruled out by the aforementioned laboratory findings.
FIGURE 1.
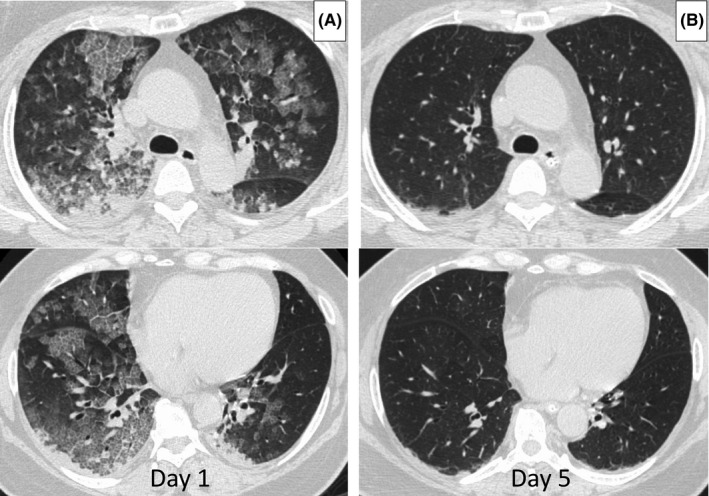
Chest computed tomography. Diffuse ground‐glass opacities with thickening of the interlobular septa, so‐called crazy‐paving appearance, were observed on day 1 (A); however, these abnormal shadows completely disappeared on day 5 (B)
FIGURE 2.
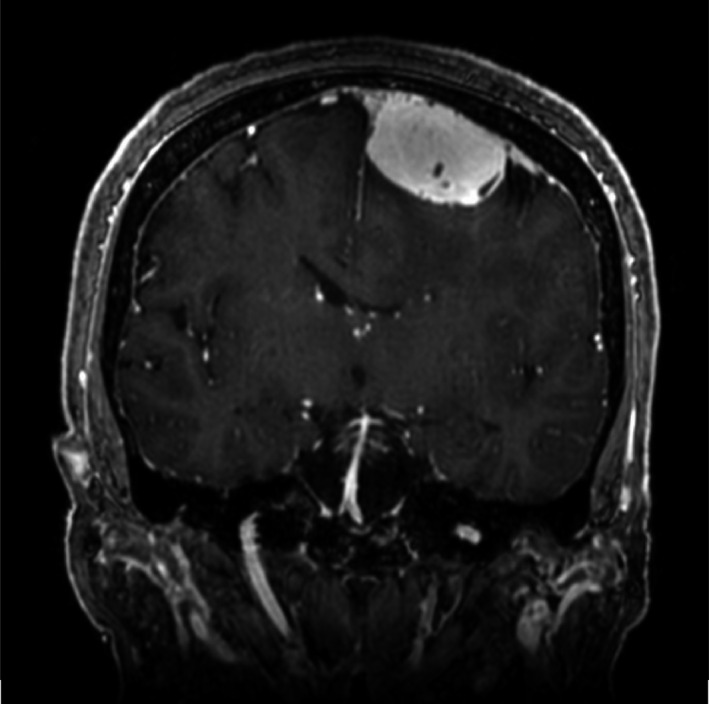
Brain magnetic resonance imaging.Brain magnetic resonance imaging revealed a dural‐based mass of 3 cm in diameter in the left parietal lobe. This mass was removed by surgery and a diagnosis of meningioma was made on the basis of pathological examination findings
Neurogenic pulmonary edema is defined as acute respiratory distress triggered by various events in the brain. Such stress increases catecholamine release and/or the levels of inflammatory mediators and then causes NPE through increased permeability of the lung capillary vessels. 1 Meningioma is a rare cause of NPE, and only one case report has been published previously. 1 , 2 When observing pulmonary edema in patients without a causative lung and heart disorder, the possibility of NPE should be considered.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
WA, TK, HN, and JF: writing of the draft and approval of the manuscript for submission.
ETHICAL APPROVAL
Written informed consent was obtained from the patient for the publication of this clinical image.
ACKNOWLEDGMENTS
We thank Editage (www.editage.com) for English language editing.
Arakaki W, Kinjo T, Nakamura H, Fujita J. Seizure followed by lung edema: An intriguing link between the brain and the lung. Clin Case Rep. 2020;8:2291–2292. 10.1002/ccr3.3139
REFERENCES
- 1. Finsterer J. Neurological perspectives of neurogenic pulmonary edema. Eur Neurol. 2019;81(1‐2):94‐102. [DOI] [PubMed] [Google Scholar]
- 2. Goyal A, Bharadwaj S. Neurogenic pulmonary edema and stunned myocardium in a patient with meningioma: a heart‐brain cross talk. J Neurosurg Anesthesiol. 2019;31(2):264‐265. [DOI] [PubMed] [Google Scholar]


