Abstract
The COVID-19 pandemic has shocked health systems worldwide, with visible impacts on intensive care units and emergency departments. The concept of “surge capacity” should be analyzed within this context as this crisis could be seen as an opportunity to improve the knowledge base of intensive care units and emergency departments.
We reflected, based on our experience from work at the frontlines, on health service planning and with epidemiological data, about the importance of surging critical care capacity for COVID, now and as lessons for the future. We summarize and relate virus clinical characteristics, epidemiological patterns and critical care surge capacity as important factors to consider for effective health systems response. Some practical aspects are described, but also the role that mathematical models can play to improve intensive care units surge capacity by considering its importance as a predictor of needs according to epidemiological patterns. Also, in the transitional phase, we consider the importance of coexisting COVID-19 and non-covid-19 health care services, and the importance of a new surge capacity for postponed activities. In this new transitional phase, also emergency departments will have to adapt their surge capacity for a rebound effect due to delayed visits from non-COVID-19 health conditions during the pandemic.
Health systems and society must remain vigilant for potential resurgence of cases as measures are relaxed to restart the economy and a new normal. Emergency departments and intensive care units have to develop surge strategies to deal together with COVID-19 and non-COVID-19 flow of patients.
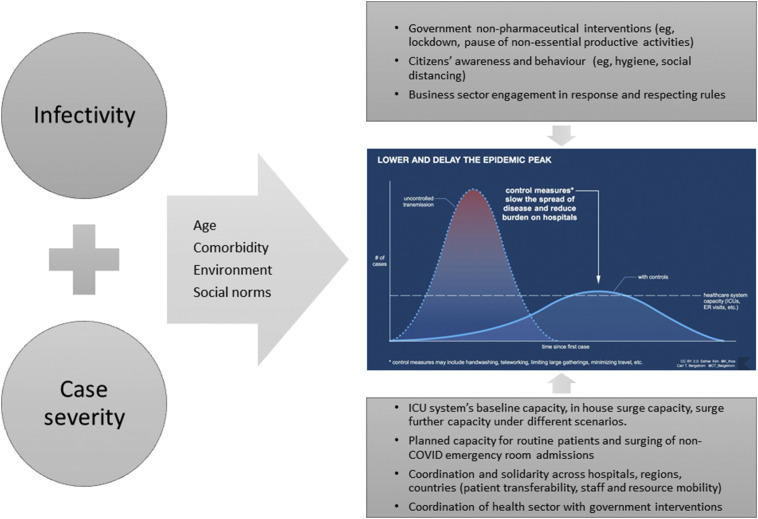
The pandemic spread of the novel SARS-CoV-2 coronavirus has unfolded into an unprecedent crisis upon its arrival to Europe and the US, unseen since the second World War and is now fast spreading into Africa and the rest of the Global South. We are learning fast about COVID-19 disease, [[1], [2]] but early experience from European countries where the epidemic hit first following China, and a growing body of research confirm that two points require cautious consideration for an effective health care response: infectiousness and case severity. (See Fig. 1.)
Fig. 1.
ICU surge capacity planning and coordination considerations for effective critical care utilization during COVID pandemic.
First, SARS-CoV-2, is a highly contagious virus, even in young healthy patients with mild symptoms. The novel coronavirus spike protein binds to human angiotensin-converting enzyme 2 (hACE2) receptor, and could do so more efficiently than SARS-CoV [2]. The peak of viral load is reached much earlier that in SARS-CoV, and is 1000 times more concentrated in the throat, where the virus replicates independently from the lungs [1]. Patients continue to be potentially infective at the time of seroconversion, and some time thereafter. Additional broad contributors to fast spread of SARS-CoV-2 were a large susceptible population in the absence of specific immunity for a novel virus [3], aided by dense international and domestic transportation networks [4] along with the initial undetected transit of people incubating the disease (5 days but up to 24 days [5]), asymptomatic [6], and symptomatic with no fever [7]. Altogether, the prospects of effective containment strategies implemented on early days of the pandemic were rigorously minimal.
Second, COVID-19 present with varying degrees of severity, ranging from asymptomatic to very severe, where severe pneumonia and acute respiratory distress syndrome (ARDS), aggravated by concomitant disease and age [8,9], can commonly occur and be fatal [7]. Given the aging populations in a majority of European countries and the US relative to China, this should translate into a larger number of cases requiring admission to hospital facilities and important pressure on intensive care units (ICU) [10].
The combination of infectivity and disease severity, in absence of other effective measures, have the potential to generate a perfect storm scenario for health systems in general and ICUs in particular due to the spatial clustering and temporal spike in cases. Patient inflows follow then an epidemic curve, with manageable growth in number of cases in early days followed by exponential growth later, which are more difficult to manage as ICU systems approach full capacity [10]. Additionally, ICU length of stay is typically long for these patients, [[8], [9]] putting additional pressure on admission capacity [11].
This situation calls immediately for surge capacity preparedness for critical care utilization, prone to be under stress first. Surge capacity points to health care and ICU systems ability to manage a sudden influx of patients relying on operational and effective crisis management systems, resource allocation of space, staff, equipment and supplies and special protection of health workers and patients (the use of personal protection equipment and compartment of hospitals and ICUs to treat these patients) [12]. All the above highlights the urgent need for a coordinated and rapid upgrade of health systems in Europe, US and elsewhere to cope with this protracted crisis [10]. Moreover, we consider three key concepts that may prove helpful to delineate our course of action and improve health systems' response: coordination, anticipation and solidarity.
Anticipate the epidemic progression and the required critical care capacity are both attainable objectives. On one hand, regions and nations must assess their inhouse potential to expand available critical care capacities. For example, the Australian and New Zealand Intensive Care Society conducted a rapid assessment on surge capacity in Australia and found feasible to increase by 189% ICU beds from baseline [13]. Intensive care and ventilator capacity vary strongly across countries and regions [14], therefore context-relevant planning is essential. In Australia, this exercise proved useful as ventilators were found to be a scarcer resource (expandable by 120%), allowing for early and progressive stockpiling to correct for this mismatch. Importantly, commensurate staff resources can be derived from numbers of ICU beds, saving precious time for administration procedures and staffing [13].
Another important point is to estimate exceedance beyond this extended capacity due to the exponential presentation of cases. Estimating this requires a combination of clinical-epidemiological measures (eg, ICU rates) and mathematical modelling. The latter to predict the maximum number of active cases, with particular relevance at epidemic peak; the former to know how many of those patients typically require hospitalization, an ICU bed, or a ventilator; in good operational conditions that ensure adequate care [10].
There are different approaches proposed to estimate these numbers, some model these quantities jointly [15] and some separately [10]. We advise to give priority to national surveillance data [10]. Irrespectively of the methods chosen, we recommend pragmatism in the measures: clinically meaningful, robust and locally relevant and available in each context. Equally important, the epidemic curves should consider government measures to be realistic enough and applicable. Creating a large number of scenarios could be counterproductive and the numbers mistrusted [10].
Coordination is key for this crisis and deserves special attention for two reasons. On one side, the epidemic is widespread but show intense clustering in regions and cities. While local and regional health services may be overwhelmed, certain nations, regions and hospitals may be operating below maximum capacity. This capacity needs to be urgently loaded into the system. Agile coordination and removal or softening of bureaucratic and administrative burdens should be temporarily permitted. These transferability needs (of patients but also of staff, equipment and supplies), again, requires anticipation and planning, and well-understood solidarity in resource use. Patient transferability should be thought of beyond political boundaries.
On the other side, in an emergency phase, we should prioritize surge capacity estimation in coordination with health sector and government measures to protect health systems, and ICU systems in particular. Our ability to implement the above heavily relies on publicly available data of sufficient quality and adhering to international standards. Hospitalization, ICU and ventilator use rates are key, highly contextual, and prone to vary as the situation evolves and learning accumulates. Research and early experience from China and Europe suggest that an organized surge capacity and planned response should be effective in dealing with this unprecedent pandemic emergency [[3], [8], [10], [11]].
Yet, significant uncertainties remain. Overall, it is unknown for how long the pandemic may last and where it will last longer. While temperature and humidity could play a role in disease dynamics, there is not yet a solid and generalizable answer to this question [[16], [17]]. Given the high infectivity of SARS-CoV-2 and the large susceptible population, even these effects may not be enough to control the disease. A vaccine may last months or years to come and today we do not have the capacity for vaccinating billions quickly [16]. As clinical management of the disease improves by more effective treatment and the early detection of patients at higher risk of ARDS or other complications, [[2], [16]] length of ICU stay and better disease prognosis will become tangible, and pressure on critical care utilization may gradually diminish.
A key point remains: dealing with regular patient flows. In the transitional phase, both COVID-19 and non-COVID-19 health care activities will have to coexist, but a new surge capacity will have to be developed for postponed activities during the pandemic [18]. In previous weeks, while preparing for COVID-19 and during the health response, many elective and semi-elective surgeries, consultations and diagnoses were postponed. Therefore, additional facilities like university residences, medicalized hotels or even the so called “field hospitals” built around the globe to support overwhelmed hospitals may be an important factor to recover normal health care system activities by admitting mild to moderate COVID-19 patients.
Emergency room workloads in particular may suffer from a rebound effect as a result of delayed visits from non-COVID-19 health conditions during the pandemic. Severe patients not properly followed up by their primary health care team, may be more likely to end in an emergency room as well as patients with mild to moderate chronic diseases who did not seek care during the epidemic rise may end up in more severe presentations [19].
Overall, the impact of the pandemic has been uneven in Europe and the US depending on various factors, with sufficient laboratory testing and ICU capacity, and timely and categorical government responses, or combinations of those factors, having a positive impact. The pandemic may now accelerate its course in countries from the South Hemisphere as they progress into winter, if indeed temperature and humidity play a role [17]. This offers an opportunity window to these countries to be prepared for surging critical care capacity while dealing with routine services.
The first wave is proving hard to be flatten and the field data is confirmatory of that trend. In Italy, at the time of writing after more than 40 days since the start of the first lockdown and above 30 days since the pause of all non-essential productive activities, surveillance is daily detecting around 2000 to 3000 new cases whereas over 6000 were detected at peak [20]. Our recommendations are certainly valid for countries presenting important epidemic peaks (e.g, Spain, Belgium) as well as for those that showed a slower increase during the first epidemic wave (e.g., Portugal, Greece).
The COVID-19 pandemic has unfolded a large diversity of complex responses from citizens, government and businesses and positive experiences exemplify important lessons to prevent overload of health care services in the future. Adequate resources for, the respect of social distancing and use of masks, adequate contact tracing services coupled to sufficient testing capacity and smart use of mobile technologies, as well as community support and solidarity, along with good governance and tempered and evidence base government communication are good examples of the complexity of effective response and resiliency to COVID-19 [ 21].
Conclusions
After overcoming pandemic peak, and while developing the transitional phase, governments and citizens, and particularly surveillance and health care systems should, thanks to the lessons learnt, remain vigilant and connected for potential resurgence of cases as measures are relaxed to restart the economy and a new normal. Emergency departments and intensive care units have to develop surge strategies to deal together with COVID-19 and non-COVID-19 flows of patients.
Availability of data and material
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Funding
Research activity at University of Padova was partly supported by MIUR (Italian Ministry of Education) under the initiative “Departments of Excellence” (Law 232/2016). The funders had no role in the conception, design, interpretation of data and in writing the manuscript.
Disclaimer
The views expressed in this article are those of the authors alone and do not represent the policies or views of the affiliated institutions.
CRediT authorship contribution statement
Jose M Rodriguez-Llanes: Conceptualization, Formal Analysis, Writing- Original draft, Writing- Reviewing and Editing, Visualization. Rafael Castro Delgado: Formal Analysis, Writing- Reviewing and Editing. Morten Gram Pedersen: Writing- Reviewing and Editing. Matteo Meneghini: Writing- Reviewing and Editing. Pedro Arcos Gonzalez: Formal Analysis, Supervision.
Declaration of Competing Interest
None declared.
Acknowledgements
The authors are grateful to Dr. Maryline Kolb for critical discussions on this piece.
References
- 1.Wölfel R., et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020 doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 2.Zhang H., Penninger J.M., Li Y., et al. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46:586–590. doi: 10.1007/s00134-020-05985-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Report of the WHO-China Joint Mission on Coronavirus Disease (COVID-19). 16–24 February 2020. 2019. https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf Accessed 1 April 2020.
- 4.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395(10225):689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.del Rio C., Malani P.N. COVID-19—new insights on a rapidly changing epidemic. JAMA. 2020 doi: 10.1001/jama.2020.3072. [DOI] [PubMed] [Google Scholar]
- 6.The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team (Feng Z), et al. The Epidemiological Characteristics of an Outbreak of 2019 Novel coronavirus diseases (COVID-19) — China, 2020. CCDC Weekly. 2020;2(8):113–122. [PMC free article] [PubMed] [Google Scholar]
- 7.W-j Guan, Z-y Ni, Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Instituto Superiore di Sanitá, ISS 2020. https://www.epicentro.iss.it/en/coronavirus/bollettino/Report-COVID2019_2_april_2020.pdf Accessed on 5 April 2020.
- 9.Zhou F., Yu T., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodriguez-Llanes J.M., Castro Delgado R., Pedersen M.G., Arcos González P., Meneghini M. Confronting COVID-19: Surging critical care capacity in Italy. [Submitted] Bull World Health Organ. 2020 doi: 10.2471/BLT.20.257766. E-pub: 6 April. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grasselli G., Pesenti A., Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020 doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 12.The American College of Emergency Physicians . October 2017. Policy Statement. Health Care System Surge Capacity Recognition, Preparedness, and Response. Accessed 5 April 2020. [Google Scholar]
- 13.Rhodes A., Ferdinande P., Flaatten H., Guidet B., Metnit P.G., Moreno R.P. The variability of critical care bed numbers in Europe. Intensive Care Med. 2012;38(10):1647–1653. doi: 10.1007/s00134-012-2627-8. [DOI] [PubMed] [Google Scholar]
- 14.Litton E., Bucci T., Chavan S., et al. Surge capacity of Australian intensive care units associated with COVID-19 admissions. Med J Aust. 2020;1 doi: 10.5694/mja2.50596. https://www.mja.com.au/journal/2020/212/10/surge-capacity-australian-intensive-care-units-associated-covid-19-admissions [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Wees J.D., Osinga S., van der Kuip M., Tanck M., Hanegraaf M., Pluymaekers M., et al. Forecasting hospitalization and ICU rates of the COVID-19 outbreak: an efficient SEIR model. Bull World Health Organ. 2020 doi: 10.2471/BLT.20.256743. [Submitted] E-pub: 30 March. [DOI] [Google Scholar]
- 16.Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T. D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lipsitch M. Seasonality of SARS-CoV-2: Will COVID-19 go away on its own in warmer weather? https://ccdd.hsph.harvard.edu/will-covid-19-go-away-on-its-own-in-warmer-weather/
- 18.WHO Strengthening the Health Systems Response to COVID-19 Technical working guidance #1: Maintaining the delivery of essential health care services freeing up resources for the COVID-19 response while mobilizing the health workforce for the COVID-19 response (18 April 2020) http://www.euro.who.int/__data/assets/pdf_file/0007/436354/strengthening-health-systems-response-COVID-19-technical-guidance-1.pdf?ua=1
- 19.Boston News As COVID-19 spreads, Massachusetts hospitals see decline in visits for other illnesses. 30 March 2020. https://www.boston.com/news/health/2020/03/30/massachusetts-coronavirus-emergency-rooms
- 20.Italian Civil Protection Data of COVID-19 Italy 2020. https://github.com/pcm-dpc/COVID-19 (Accessed from 14 March, everyday, up to 27 April 2020) [DOI] [PMC free article] [PubMed]
- 21.Shaw R., Kim Y.K., Hua J. Governance, technology and citizen behavior in pandemic: lessons from COVID-19 in East Asia. Progr Disast Sci. 2020;6:100090. doi: 10.1016/j.pdisas.2020.100090. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.