Abstract
Background
Acute poisoning is a common reason for visiting the emergency department (ED) worldwide. However, little is known about this issue in the western part of Ethiopia. This study was carried out to determine the prevalence, predictors, and treatment outcome of acute poisoning at the ED of western Ethiopia.
Patients and Methods
A hospital record-based retrospective study design was conducted on all patients admitted to the ED of the two hospitals between 01 January 2018 to 17 March 2019. Socio-demographic, clinical presentation, medication history, poisoning characteristics, time to hospital arrival, treatment given, and outcome of treatment were collected. All collected data were analyzed using SPSS Version 20. Backward multiple logistic regression analysis at p-value ≤0.05 tested the predictor for treatment outcome.
Results
The prevalence of acute poisoning was 134/7883 (1.7%) per ED admissions. The mean ±SD age of the study participants was 23.90±10.606 with female to male ratio of 1:1.06. The most vulnerable patients to poisoning were individuals in the age range of 18 to 29 years 68/134 (50.7%) for both genders. Moreover, the most common poisoning agent was organophosphate 72/134 (53.7%). Besides, intentional poisoning was the most common 103/134 (76.9%) manner of poisoning with family disharmony 37/103 (35.9%) as the common reason. The case fatality rate of acute poisoning in the two hospitals was 2/134 (1.5%). The mean ±SD length of hospital stay was 1.86 ±0.943. The independent predictors of poor treatment outcome of acute poisoning were age ≥35 years [p-value= 0.049], female gender [p-value= 0.027], and hospital stay of >48 hours [p-value= 0.035].
Conclusion
The prevalence of acute poisoning in western Ethiopia is higher than the ever-reported data in Ethiopia. Thus, stakeholders should have to pay more attention to prevention and control strategies and appropriate handling of agrochemical substances to minimize their negative effects on this productive age group.
Keywords: acute poisoning, mortality, treatment outcome, organophosphate, predictors, Ambo
Introduction
Poison is defined as any chemical that can change or impair the normal physiology of humans through general or local damage to cell or death by its chemical activity.1,2 Acute poisoning is exposure to poison for a short period (less than 24 hours) through any route, intentionally or unintentionally. It is the common cause of emergency admission, which may result in morbidity and mortality.1–3 One systematic review and Meta-analysis in Ethiopia reported that the mortality rate of acute poisoning was in the range of 0% to 14.8%.4
Acute poisoning is a significant global public health problem.5,6 Acute poisoning cases are increasing day by day due to changes in lifestyle, availability of chemicals, and social behavior.5,7 Especially, the problem is common and much worse in low- and middle-income countries (LMICs), because of the weak regulations and poor healthcare services.8 According to the World Health Organization (WHO) estimates, in 2004 and 2012 there were 193,460 to 346,000 deaths (3.5/100,000) worldwide from unintentional poisoning. Of these deaths, 84% to 91% occurred in LMICs. In 2004 and 2012, there is a loss of over 7.4 to 10.7 million years of healthy life (disability-adjusted life years) due to unintentional poisoning.5,6,9 Even though there was a decrease in the number of deaths, there was an increase in the disability-adjusted life years between the two reports (2004 versus 2012). Moreover, it is estimated that the intentional ingestion of pesticides causes 370,000 deaths each year. Data from WHO indicate that one person every 40 seconds dies due to suicide globally. Of this death, the most common cause of death is due to chemical agents. Globally, suicide is the most common cause of mortality in 15–29-year-olds populations. Indeed, 79% of suicides occurred in LMICs in 2016.10
This can be minimized by reducing the availability and access to highly toxic pesticides as well as by having a well-organized health care system.6 Thus, knowledge about the prevalence of poisoning, its characteristics or nature, and treatment outcome are important to the public, policymakers, emergency physicians and health practitioners,1,2 to take prompt and appropriate measures to save lives and reduce morbidity and mortality.7,11
The prevalence, nature, mortality, and morbidity of acute poisoning vary owing to differences in socioeconomic, cultural, and health care facility level of the country.5–9 Therefore, local data are paramount for planning and efficient use of resources for the prevention and management of acute poisoning. However, data about the nature, treatment outcome, its predictors, and hospital stay of patients with acute poisoning were limited. Besides, Ethiopia is among the countries that lack the poison center.4 The prevalence of acute poisoning at ED was reported as 134/30,154 to 106/8827 (0.77% to 1.2%) by a few studies in Africa.12–14 Even, that literature was failed to report the prevalence of acute poisoning in Ethiopia. Thus, the current study aimed to determine the prevalence, characteristics or nature, mortality, length of hospital stay, and their predictors at the two hospitals Ambo University Referral Hospital (AURH) and Ambo General Hospital (AGH) of western Ethiopia.
Methods and Participants
Study Area, Period, and Study Design
The study was conducted with a hospital register-based retrospective study design at EDs of AURH and AGH from March 27, 2019, to April 5, 2019 (data collection period). Both hospitals are located in Ambo city, west Shoa zone, western Ethiopia that is 126 km west of Addis Ababa. AGH is the oldest hospital in the Ambo town, while AURH is the only referral hospital for more than 1.3 million people from the West Shoa zone and surrounding catchment area that was founded in 2016 with 134 beds by Ambo University.
Study Population, Sample Size, and Selection Criteria
All patients with a diagnosis of acute poisoning and who have had visited ED of AURH and AGH with inclusion criteria were our study population. The inclusion criteria were all acutely poisoned patients and who have visited ED of ARUH and AGH from January 02/2018 to March 17/2019. The exclusion criteria were poisoning due to dog bite and snakebite or animal or insect bite (due to infrequent report), and cards with incomplete information. Thus, the sample size was all recorded data of acute poisoning at the ED of AURH, and AGH, over 15 months resulted in 134 study participants.
Data Collection Instruments and Process
The data collection checklist was developed from the previous publication with slight modification.1,5,11,14 Then, pre-test was done to check consistency and completeness of the checklist relative to the current objectives. Two trained 5th-year pharmacy students collected the data. The data were collected from the patient card using a pre-tested and pre-prepared data collection checklist after recording the card number of acute poisoning cases from the ED patient’s registration logs. Then using this card number, the data collectors filtered the patient’s chart from the medical record room. The checklist was filled by searching for appropriate information from the patients’ charts. This information includes age, sex, residence, educational level, diagnosis, co-morbidity, route, and reason of poisoning, manner of poisoning, the dosage form of poisoning, the season of poisoning, time of hospital admission since exposure, type of poisoning agent, cause of poisoning, given medication, consciousness at admission which was categorized into two conscious and unconscious (stupor or total unconscious patient), time of arrival, treatment outcome and hospital stay.
Data Quality Assurance, Data Processing, and Analysis
Completeness, accuracy, clarity, and consistency of the data were checked before data entry and analysis. All collected data were analyzed using SPSS Version 20 and presented in the form of median, means, and standard deviations (SD) for continuous variables depending on the data distribution. Categorical variables were presented by frequency and percentages. The independent predictors were tested using backward multiple logistic regression models. Significance was set at p-value ≤0.05.
Ethical Consideration
An official ethical clearance letter was received from Ambo University College of Medicine and Health Sciences research and ethics committee (Phar/136/2011) and was sent to AURH and AGH for permission. As the data were collected from the patient’s chart and no unique identification that was going to be reported in this research, consent from patients was not applicable and it was waived by the committee. This study was conducted according to the Declaration of Helsinki principles.
Operational Definition
Disability: Disability was to mean either a physical disability or physiological disability leading to new morbidity, dialysis, or respiratory or another organ failure following acute poisoning which was confirmed by laboratory investigation or suspected by clinicians, based on the clinical complaints of patients. Intentional poisoning is the result of a person taking or giving a substance to cause harm. Unintentional poisoning is if a person taking or giving a substance did not mean to cause harm. The outcome of acute poisoning: In this study, the outcome of acute poisoning could be death, survival with a disability, or without a disability. Poor treatment outcome: Cure with disability or death. Good treatment outcome: Cure without a disability. Prevalence of acute poisoning: in this study was defined as the proportion of a population who were poisoned from the total number of people attending the EDs of the two hospitals.
Results
Characteristics of the Study Participants
The fifteen-month prevalence of acute poisoning in the two hospitals was 134/7883 (1.7%) per emergency admissions. The mean ±SD age of the study participants was 23.90±10.606 with 69/134 (51.5%) males that equate to female-to-male ratio of 1:1.06. The most vulnerable patients to acute poisoning were individuals in the age range of 18 to 29 years 68/134 (50.7%). Most of the study participants were adults (≥18 years) 32/134 (77.8%), from urban area 93/134 (69.4%), and unconscious at admission 94/134 (70.1%). The most common place where the poisoning occurred was at home 119/134 (88.8%), while summer and spring were the commonest reasons for the occurrence of poisoning in 58/134 (43.3%) and 41/134 (30.6%), respectively (Table 1).
Table 1.
Patients’ Socio-Demographic Characteristics of the Study Participants
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Age in year | <5 | 5 | 3.7 |
| 5 to 11 | 6 | 4.5 | |
| 12 to 17 | 21 | 15.7 | |
| 18 to 29 | 68 | 50.7 | |
| 30 to 39 | 23 | 17.2 | |
| 40 to 49 | 8 | 6.0 | |
| ≥50 | 3 | 2.2 | |
| Mean ±SD | 23.90±10.606 | ||
| Residence | Rural | 41 | 30.6 |
| Urban | 93 | 69.4 | |
| Sex | Male | 69 | 51.5 |
| Female | 65 | 48.5 | |
| Education level | N/A* | 5 | 3.7 |
| Cannot read and write | 28 | 20.9 | |
| Primary(1 to 8) | 35 | 26.1 | |
| Secondary(9 to 12) | 31 | 23.1 | |
| Certificate/Diploma and above | 35 | 26.1 | |
| Patient status at admission | Conscious | 40 | 29.9 |
| Unconscious | 94 | 70.1 | |
| Source/place poisoning | Home | 119 | 88.8 |
| Hotel | 9 | 6.7 | |
| Workplace | 3 | 2.2 | |
| Forest | 3 | 2.2 | |
| Season of poisoning | Summer | 58 | 43.3 |
| Spring | 41 | 30.6 | |
| Autumn | 14 | 10.4 | |
| Winter | 21 | 15.7 | |
Note: *Too young to start education.
Nature of Poisoning Agent, Manner, and Reason for Poisoning
Of the 134 poisoned cases, the oral route is the most common route of exposure 122/134 (91.0%). Moreover, 129/134 clients had a record of known poisoning agents, of which organophosphate was the most common poisoning agent 72/134 (53.7%). Intentional poisoning was the most common 103/134 (76.9%) manner of poisoning, of which 68/103 (66.2%) of cases had a known reason for poisoning. Thus, the most common cues for self-harm were family disharmony, followed by financial problems in 38/103 (36.9%) and 7/103 (6.8%), respectively, among intentional poisoning (Table 2).
Table 2.
Distribution of Type of Poisoning Agent, Manner, and Reason for Poisoning
| Variables | Category | Frequency | Percentage (%) |
|---|---|---|---|
| Type of poison (N=134) | Organophosphate | 72 | 53.7 |
| Prescription drug | 10 | 7.5 | |
| Food poisoning | 10 | 7.5 | |
| Other | 10 | 7.5 | |
| Alcohol | 10 | 7.5 | |
| Herbal medication | 7 | 5.2 | |
| Hydrogen peroxide | 2 | 1.5 | |
| Kerosene | 1 | 0.7 | |
| Benzene | 3 | 2.2 | |
| Carbon monoxide | 4 | 3.0 | |
| Unknown chemical | 5 | 3.7 | |
| Manner of poisoning (N= 134) | Intentional | 103 | 76.9 |
| Unintentional | 31 | 23.1 | |
| Reason of clients for intentional poisoning (N= 103) | Family disharmony | 38 | 36.9 |
| Unknown | 35 | 34.0 | |
| Exam failure or University dismissal | 4 | 3.9 | |
| Un-planed pregnancy | 6 | 5.8 | |
| Marital disharmony | 3 | 2.9 | |
| Financial problem/loss of money | 7 | 6.8 | |
| Unemployment | 4 | 3.9 | |
| Conflict on a work area | 4 | 3.9 | |
| Mental disorder | 1 | 1.0 | |
| Being RVI | 1 | 1.0 | |
| Dosage form/Route of exposure (N= 134) | Solid or liquid/Oral | 122 | 91.0 |
| Gas/Inhalation | 9 | 6.7 | |
| Eye drop/topical | 3 | 2.2 |
Note: Other, aluminum phosphate, aluminum phosphatide, bleaching agent, hydrocarbon.
Abbreviation: RVI, retroviral infection.
Nature of Acute Poisoning by Age and Gender
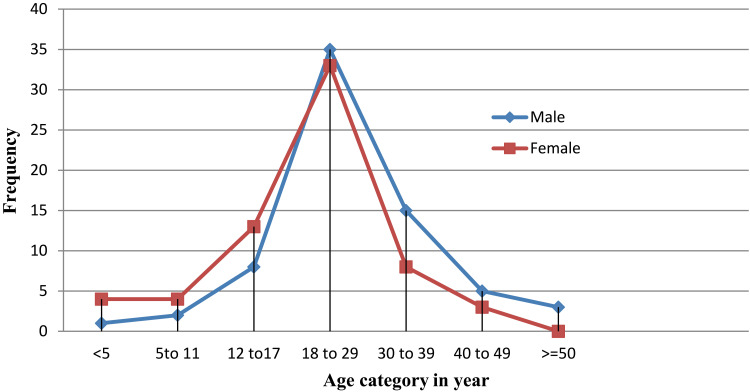
It was noted that acute poisoning was common in females before the age of 18 to 29 years and start to decline after this age for females unlike that of the male gender. The peak age for poisoning in both genders was noted in the age range of 18 to 29 (Figure 1).
Figure 1.
Overall distribution of poisoning cases by gender and age.
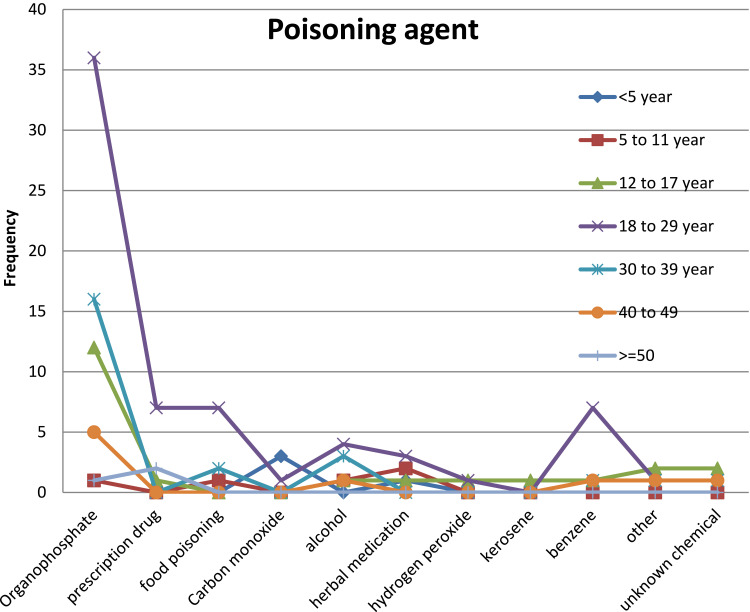
Distribution of Poisoning Agent and Manner of Poisoning by Age and Gender
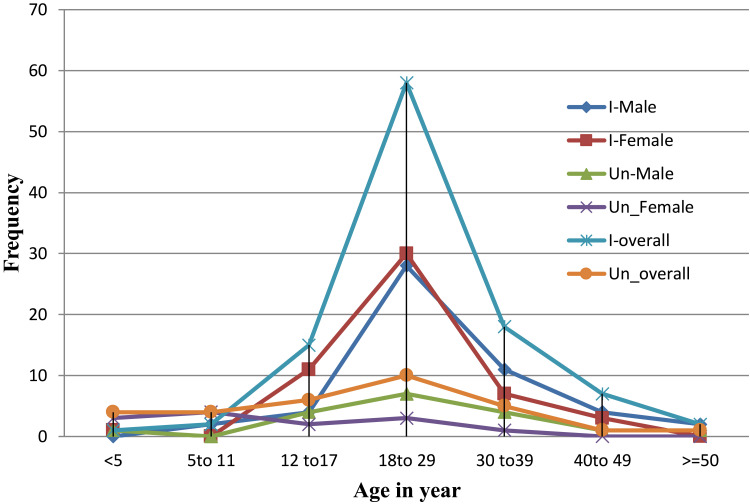
Organophosphate was noted as the most common poisoning agent in the age group of 18 to 29, 30 to 39 followed by 12 to 17 years in the descending order. Moreover, prescription drug and carbon monoxide were the most common poisoning agent in the age range of ≥50 and <5 years, respectively. Almost organophosphate was the most commonly implicated agent in acute poisoning (Figure 2). Of the total poisoned clients, intentional poisoning was the most prevalent with a peak in the age range of 18 to 29 years. The pattern of both intentional and unintentional poisoning was similar throughout all age range for both genders; with low prevalence at the two extremities. However, there was slightly higher overall unintentional poisoning at the earlier age of life (≤11 years) than that of the older age of life (≥40 years) (Figure 3).
Figure 2.
Overall distribution of chemicals contributed to poisoning by age.
Figure 3.
Distribution of manner or intension of poisoning by age and gender.
Notes: I_Female is intentional poisoning in females; Un_female is unintentional poisoning in females and vice versa.
Arrive Time at the Hospital Since Poisoning and Outcome at Discharge
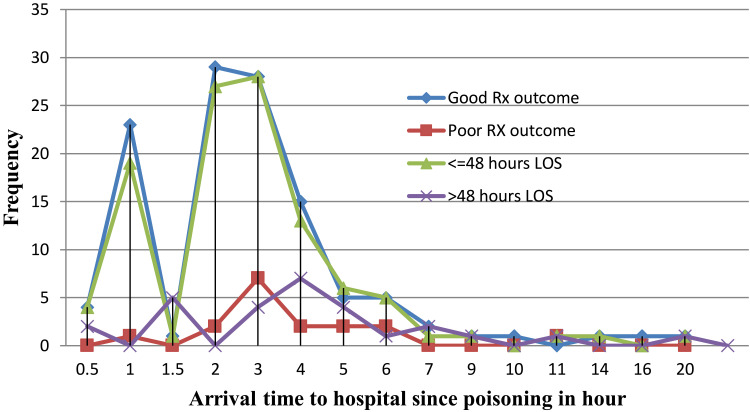
Arrive at the hospital since poisoning was within 5 hours for most of the clients with a peak at 2 to 3.5 hours with the mean ±SD of 3.235±2.76 hours. The current study showed that individuals who were arrived at the hospital within 5 hours had good treatment outcomes and stayed for a short duration (≤48 hours) in the hospital (Figure 4 and Table 3).
Figure 4.
Time of arrival to the hospital since poisoning versus treatment outcome and length of hospital stay.
Abbreviations: Rx, treatment; LOS, length of hospital stay.
Table 3.
Acute Poisoning Management Practice and Its Outcome
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Time of arrival to the hospital since the poisoning | ≤1 hour | 28 | 20.9 |
| >1 to ≤5 hours | 91 | 67.9 | |
| >5 hours | 15 | 11.2 | |
| Mean ± SD | 3.235±2.76 | ||
| Non-pharmacologic treatment | Gastric lavage | 18 | 13.4 |
| Not given | 114 | 85.1 | |
| Oxygen therapy | 4 | 3.0 | |
| Time arrival and gastric lavage (N= 18) | ≤1 hour | 4 | 22.2 |
| >1 to ≤5 hours | 9 | 50.0 | |
| >5 hours | 5 | 27.8 | |
| Pharmacologic treatment* | Antacid | 54 | 40.3 |
| Cimetidine/ranitidine | 45 | 33.6 | |
| Atropine | 23 | 17.2 | |
| Analgesics | 12 | 9.0 | |
| 40% dextrose | 9 | 6.7 | |
| Maintenance fluid | 8 | 6.0 | |
| Omeprazole/pantoprazole | 7 | 5.2 | |
| Metoclopramide or plasil | 6 | 4.5 | |
| Antibiotics | 8 | 6.0 | |
| Diazepam or haloperidol or phenobarbitone | 5 | 3.7 | |
| Other | 4 | 3.0 | |
| Length of hospital stay (days) | 1 | 56 | 41.8 |
| 2 | 52 | 38.8 | |
| 3 | 18 | 13.4 | |
| 4 | 5 | 3.7 | |
| ≥5 | 3 | 2.2 | |
| Mean ±SD | 1.86± 0.943 | ||
| Treatment outcome | Cure without disability | 117 | 87.3 |
| Cure with disability | 15 | 11.2 | |
| Death | 2 | 1.5 | |
Notes: Other, antidote, tetracycline eye ointment, zoxan eye drop; *There is a multiple response.
Management Practice of Acute Poisoning and Treatment Outcome
For acute poisoning based on the patient’s case, both pharmacological and non-pharmacological care was provided to the client. It was noted that gastric lavage was administered in 18/134 (13.4%) of cases, as non-pharmacologic care, to prevent the absorption of toxic agents. However, for most of the patients 9/18 (50.0%) it was done for patients who were arrived at the hospital within 1 to 5 hours of poisoning. Moreover, the most commonly used pharmacological treatment was antacid 54/134 (40.3%) (cimetidine/ranitidine) 45/134 (33.6%), followed by atropine injection 23/134 (17.2%). Regarding the outcome of poisoning, almost 117/134 (87.3%) of the cases were cured without a disability. The case fatality rate of acute poisoning in the two hospitals was 2/134 (1.5%). Most of the clients stayed in the hospital (ED) for 1 day 56/134 (41.8%) with the mean ±SD of 1.86 ±0.943 (Table 3).
Predictors for Treatment Outcome of Acute Poisoning
The result of backward multivariate logistic regression analysis showed that, the independent predictors of poor treatment outcome of acute poisoning were age ≥35 years [AOR=6.6 at 95% C.I 1.006–43.693; p-value= 0.049], female gender [AOR= 0.282 at 95% C.I 0.087–0.92; p-value= 0.027], and hospital stay of >48 hours [AOR= 3.584 at 95% C.I 1.094–11.724; p-value= 0.035] (Table 4).
Table 4.
Independent Predictors for Treatment Outcome of Acute Poisoning
| Variables | Category | Treatment Outcome, N=134 | AOR | 95% CI | P-value* | |
|---|---|---|---|---|---|---|
| Good (%) | Poor (%) | |||||
| Age | <19 | 37(94.9) | 2(5.1) | 1 | ||
| 19 to34 | 64(87.7) | 9(12.3) | 2.515 | 0.441–14.358 | 0.299 | |
| ≥35 | 16(72.7) | 6(27.3) | 6.63 | 1.006–43.693 | 0.049 | |
| Sex | Male | 56(81.2) | 13(18.8) | 1 | 0.027 | |
| Female | 61(93.8) | 4(6.2) | 0.282 | 0.087–0.92 | ||
| Residence | Rural | 38(92.7) | 3(7.3) | 0.215 | ||
| Urban | 79(84.9) | 14(15.1) | 2.245 | 0.608–8.3 | ||
| Patient status | Conscious | 35(87.5) | 5(12.5) | 1 | 0.97 | |
| Unconscious | 82(87.2) | 12(12.8) | 1.024 | 0.336–3.126 | ||
| Manner of poisoning | Intentional | 91(88.3) | 12(11.7) | 0.542 | ||
| Unintentional | 26(83.9) | 5(16.1) | 1.5 | 0.471–4.52 | ||
| Time of arrival since exposure (hours) | ≤1 | 27(96.4) | 1(3.6) | 1 | ||
| >1 to ≤5 | 78(85.7) | 13(14.3) | 5.170 | 0.586–45.594 | 0.139 | |
| >5 | 12(80.0) | 3(20.0) | 4.317 | 0.355–52.554 | 0.251 | |
| Hospital stay | ≤48 | 97(89.8) | 11(10.2) | 1 | 0.035 | |
| >48 | 20(76.9) | 6(23.1) | 3.584 | 1.094–11.724 | ||
Note: *Multivariate analysis result.
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval.
Discussion
This was a hospital registry-based retrospective study done at AURH and AGH over 15 months had found a high rate of acute poisoning and good treatment outcome. To our best knowledge, this study was the first to report predictors of acute poisoning treatment outcomes in Ethiopia.
In the current study, the prevalence of acute poisoning was higher than the ever-reported data from Ethiopia and some African countries. Yet the true prevalence might be more than this, due to uncommon practice of health-seeking practice of poisoned patients,15 and the poor recording.4 Even though data regarding the prevalence of acute poisoning are rare in Ethiopia,4 it was reported to be as high as 0.67% to 1.1% of ED admission at Gondar, Northwest Ethiopia which is lower than the current data,14,16 and in Tanzania 1.2%.12 This is evidence that there is an increase in the rate of acute poisoning from time to time due to an increase in the availability of poisoning agents and social behavior as well as poor knowledge amongst users,17,18 and weak controlling systems of agrochemicals, especially in LMICs.5,8,18 However, this result is lower as compared to the study done in Iran-Tabriz (5.4%).19
In the current study, the most common poisoning was due to organophosphate, which is the common chemical that has been in use as pesticides by Ethiopian farmers.17 The contributing chemicals for acute poisoning are different based on the geographical area and availability of the chemicals;7 for instance, in Birjand and Tehran, Iran, the most common cause of poisoning were pharmaceutical chemicals.20,21
In our study, the most vulnerable patients to poisoning were young adults (18 to 29 years). This result was comparable with the studies done in Ethiopia,4 Kenya,22 Iran,19 and China.15 The reason for the high rate of poisoning in young adults was partially explained by their vulnerability to stressful life situations and immaturity to cope up with the situation; thus, they would be easily emotional to decide suicide. Besides, in this age group, there was a high prevalence of adjustment disorder that might predispose them to commit suicide.21 Moreover, people in this age group probably face failure or frustration in love or job or exams, inability to fulfill the parents’ expectations.15,19,21
However, this result was different as compared to a study conducted in Taiwan, which reported the age of 65 years or older to have the highest rate for acute poisoning.23 This may be related to the fact that this population has a lower literacy rate, resulting in a lack of knowledge and skills related to handling poisoning agents safely. Besides, the existence of multiple illnesses, multiple medications, and poor physical conditions may also increase the risk of poisoning.
The gender distribution of acute poisoning in the current study revealed that male preponderance. This finding appears to be concordant with other studies conducted in the southern part of India (81.2%),24 Iran-Teheran (51%),25 Zambia (52%),26 Birjand, Iran,20 and Nakuru-Kenya (58.33%).22 This may be related to more exposure of males to occupational hazards and stress. However, other studies have indicated a higher incidence of acute poisonings in females, in Iran-Teheran (55.7%),19 Turkey (60%),27 and Gondar-Ethiopia (63.5%).16 The higher proportion of females being acutely poisoned in other studies might be because some situations such as family disharmony could be frustrating for them and they might commit suicide. Besides, when there are economic challenges in a family, they might feel guilty and might attempt for self-poisoning.
The level of economic development and socio-culture of the community determines the pattern of poisoning agents.7 Thus, for LMICs agrochemical agents were the most common agent contributing to poisoning as it has been in use for farming purposes.5,6,8,9 In the current study, it was noted that poisoning due to organophosphate was the most prevalent, which coincide with summer and spring as the most common season of poisoning. It is the time when organophosphate/pesticides were highly available or accessible for farming purposes in Ethiopia. This study result was in line with different studies from LMICs.2,11,26,28–30 This can be minimized by reducing the availability and access to highly toxic pesticides as well as by increasing knowledge of the farmers or users of this chemical about its health risk, storage, and necessary risk reduction measures during spray of the chemical.6,17
The intentional manner of poisoning type was the most common in this study. Similarly, other studies have confirmed the situation in a different part of the world; Kathmandu–India, Addis Ababa–Ethiopia, and China.2,5,15,30,31 The high prevalence of intentional poisoning might be partially explained by low job opportunity and economic achievement, which contributes to loss of hope among young adults.15,21 Thus, the government and stakeholders should increase job opportunities and training for young adults on how to cope up with a difficult situation like family disharmony. Unintentional poisoning was common in the age range of <11years, where carbon monoxide was the most common poisoning agent for under 5year, which could be easily prevented by appropriate handling of this chemical.
Treatment outcome of acute poisoning is determined by early recognition of the case, appropriate supportive care, patient and poisoning agent-related factors. Thus, provision of appropriate assessment and diagnosis (ABC of life), gastric decontamination (lavage and activated charcoal) based on the patients’ time of arrival, and nature of poisoning agent, and provision of specific antidotes were paramount in reducing morbidity and mortality.4,32–38 However, the studied hospitals lack standard guidelines for the management of acute poisoning or specific poison center during the study period.14 Thus, there was no consistent practice among clinicians.
Nevertheless, based on the patients’ case, both pharmacological and non-pharmacological care was provided. For instance, gastric lavage was done as a non-pharmacologic treatment. However, for most of the patients it was done almost irrespective of the time of arrival; within 1 to 5 hours of poisoning or more. Indeed, the best time for gastric lavage was within 1 hour of toxin ingestion and/or for very large or dangerous chemical ingestion, where an antidote is unavailable.14,38 Thus, delayed gastric lavage lacks any scientific support, as it lacks a beneficial effect for the patients.38 The most commonly used pharmacological treatment was antacid and/or cimetidine/ranitidine, followed by atropine; the antidote for organophosphate poisoning.15,38 Besides, supportive care like fluid and antiemetic was provided to alleviate the clinical presentation or complication of poisoning agents. This indicates that most of the treatments are supportive or symptomatic treatment. This may be due to a lack of standardized diagnostic laboratory tests to identify the exact chemical agent so that the clinician can administer a specific antidote.32
Regarding the outcome of poisoning, most of the cases were cured without a disability with short (less than 1 day) hospital stay in most cases. The case fatality rate of acute poisoning in the two hospitals was 1.5%, which is similar to the other studies’ reports from China, Botswana, and Ethiopia.4,5,15,29,39 Even though the outcome of treatment was promising, the truthiness of the result may be doubted by that, not all cases of poisoning are brought to an ED of these hospitals, and poor recording of immediate death upon arrival or before arrival at the hospital may have led to an underestimation of mortality rate and prevalence of acute poisoning.14,15 Thus, the interpretation of this data should give due emphasis to such drawbacks. However, this result was different as compared to the studies conducted in India, the case fatality rate of 13.2%,40 and Iran 4.8% to 19.5%.20,21 This variation may be explained by a lack of early diagnosis and treatment as well as the difference in the chemical agent and dose ingested or severity of poisoning cases.
The independent predictors of poor treatment outcomes of acute poisoning were age ≥35 years and are more like to contribute to a poor treatment outcome by around 7 times than age <19 years.41,42 Moreover, the female gender is less likely to have poor treatment outcome by around 72% relative to male, while hospital stay of >48 hours increase the likelihood of poor treatment outcome by around 4 times than ≤48 hours of hospital stay. Patients with longer hospital stay might have more severe cases, which might contribute to poor treatment outcomes.
As a limitation, there might be an underestimation of the overall prevalence of poisoning and mortality rate due to poor registration or not all poisoned patients seek health care at these hospitals. Second the retrospective nature of the study design, which prohibited us from collecting detail clinical and laboratory data to determine the severity of the cases as a determinant of treatment outcome,43 we hope the future research will solve this issue through prospective study design. However, it is the first study to report the predictors of acute poisoning treatment outcomes in Ethiopia.
Conclusion
It was noted that the prevalence of acute poisoning in western Ethiopia was higher than the every reported data in Ethiopia. This issue should urge the stakeholder to pay more attention to the area in planning prevention and control strategies of poisoning. Control and appropriate handling of agrochemical substances to minimize their negative effects on this productive age group are warranted. Most of the patients were discharged with good treatment outcomes. The independent predictors for poor treatment outcomes were older age, female gender, and longer hospital stay. The authors recommend that prospective research has to be done to predict the factors contributing to poor treatment outcome with the incorporation of clinical, laboratory, and treatment-related factors.
Acknowledgments
Our heartfelt gratitude goes to the staff of AURH and AGH for their co-operation in providing relevant information.
Funding Statement
The authors have no source of funding for this study.
Abbreviations
AGH, Ambo General Hospital; ARUH, Ambo University Referral Hospital; AOR, adjusted odds ratio; CI, confidence interval; ED, emergency department; LMICs, low- and middle-income countries; SD, standard deviation; WHO, World Health Organization.
Data Sharing Statement
All data are presented within the article.
Ethics Approval and Consent to Participate
This study was conducted according to the Declaration of Helsinki principles and was approved by Ambo University, college of medicine and health sciences ethical review committee (phar/136/2011). Informed consent was waived due to the retrospective nature of the study and no effect on the study participants. However, the confidentiality of the data was secured.
Author Contributions
Both authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
- 1.Jesslin J, Adepu R, Churi S. Assessment of prevalence and mortality incidences due to poisoning in a South Indian tertiary care teaching hospital. Indian J Pharm Sci. 2010;72(5):587. doi: 10.4103/0250-474X.78525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maheswari E, Abraham L, Chacko CS, Saraswathy GR, Ramesh AC. Assessment of pattern, severity and outcome of poisoning in emergency care unit. J Appl Pharm Sci. 2016;6(12):178–183. doi: 10.7324/JAPS.2016.601225 [DOI] [Google Scholar]
- 3.Rutto J, Chepchirchir A, Odero T. Nurse’s knowledge, attitude and practice on the initial management of acute poisoning among adult casualties: study at Kenyatta National Hospital, Kenya. 2012.
- 4.Chelkeba L, Mulatu A, Feyissa D, et al. Patterns and epidemiology of acute poisoning in Ethiopia: systematic review of observational studies. Arch Public Health. 2018;76(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Desalew M, Aklilu A, Amanuel A, Addisu M, Ethiopia T. Pattern of acute adult poisoning at TikurAnbessa specialized teaching hospital, a retrospective study, Ethiopia. Hum Exp Toxicol. 2011;30(7):523–527. doi: 10.1177/0960327110377520 [DOI] [PubMed] [Google Scholar]
- 6.WHO. Poisoning prevention and management. Available from: https://www.who.int/ipcs/poisons/en/. Accessed August05, 2020.
- 7.Alinejad S, Zamani N, Abdollahi M, Mehrpour O. A narrative review of acute adult poisoning in Iran. Iran J Med Sci. 2017;42(4):327. [PMC free article] [PubMed] [Google Scholar]
- 8.Kaale E, Mori A, Risha P, Hasham S, Mwambete K. A retrospective study of poisoning at Muhimbili National Hospital in Dar-Es Salaam, Tanzania. J Public Health Front. 2013;2(1):21–26. doi: 10.5963/PHF0201003 [DOI] [Google Scholar]
- 9.Teklemariam E, Tesema S, Jemal A. Pattern of acute poisoning in Jimma University specialized hospital, south West Ethiopia. World J Emerg Med. 2016;7(4):290. doi: 10.5847/wjem.j.1920-8642.2016.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO. Mental health. Available from: https://www.who.int/mental_health/prevention/suicide/suicideprevent/en/. Accessed July30, 2020.
- 11.Hakim A, Khurshid R, Mufti S, Krishan K, Singh Y. Pattern, profile and outcome of poisoning cases: a study at a large teaching hospital in India. JK Pract. 2014;19(1–2):36–40. [Google Scholar]
- 12.Mbarouk GS, Sawe HR, Mfinanga JA, et al. Patients with acute poisoning presenting to an urban emergency department of a tertiary hospital in Tanzania. BMC Res Notes. 2017;10(1):482. doi: 10.1186/s13104-017-2807-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adinew GM, Asrie AB, Birru EM. Pattern of acute organophosphorus poisoning at university of gondar teaching hospital, Northwest Ethiopia. BMC Res Notes. 2017;10(1):1–6. doi: 10.1186/s13104-017-2464-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adinew GM, Woredekal AT, DeVos EL, Birru EM, Abdulwahib MB. Poisoning cases and their management in emergency centres of government hospitals in northwest Ethiopia. Afr J Emerg Med. 2017;7(2):74–78. doi: 10.1016/j.afjem.2017.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y, Yu B, Wang N, Li T. Acute poisoning in Shenyang, China: a retrospective and descriptive study from 2012 to 2016. BMJ Open. 2018;8(8):e021881. doi: 10.1136/bmjopen-2018-021881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adinew G. Pattern of acute poisoning in teaching hospital, Northwest Ethiopia. 2016 [DOI] [PMC free article] [PubMed]
- 17.Negatu B, Kromhout H, Mekonnen Y, Vermeulen R. Use of chemical pesticides in Ethiopia: a cross-sectional comparative study on knowledge, attitude and practice of farmers and farm workers in three farming systems. Ann Occup Hyg. 2016;60(5):551–566. doi: 10.1093/annhyg/mew004 [DOI] [PubMed] [Google Scholar]
- 18.Van Der Hoek W, Konradsen F, Athukorala K, Wanigadewa T. Pesticide poisoning: a major health problem in Sri Lanka. Soc Sci Med. 1998;46(4):495–504. doi: 10.1016/S0277-9536(97)00193-7 [DOI] [PubMed] [Google Scholar]
- 19.Islambulchilar M, Islambulchilar Z, Kargar-Maher M. Acute adult poisoning cases admitted to a university hospital in Tabriz, Iran. Hum Exp Toxicol. 2009;28(4):185–190. doi: 10.1177/0960327108099679 [DOI] [PubMed] [Google Scholar]
- 20.Mehrpour O, Akbari A, Jahani F, et al. Epidemiological and clinical profiles of acute poisoning in patients admitted to the intensive care unit in eastern Iran (2010 to 2017). BMC Emerg Med. 2018;18(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farzaneh E, Mehrpour O, Alfred S, Moghaddam HH, Behnoush B, Seghatoleslam T. Self-poisoning suicide attempts among students in Tehran, Iran. PsychiatriaDanubina. 2010;22(1):34–38. [PubMed] [Google Scholar]
- 22.Bundotich JK, Gichuhi M. Acute poisoning in the Rift Valley Provincial General Hospital, Nakuru, Kenya: January to June 2012. S Afr Fam Pract. 2015;57(3):214–218. doi: 10.1080/20786190.2014.975448 [DOI] [Google Scholar]
- 23.Chien W-C, Lin J-D, Lai C-H, Chung C-H, Hung Y-C. Trends in poisoning hospitalization and mortality in Taiwan, 1999–2008: a retrospective analysis. BMC Public Health. 2011;11(1):703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gargi J, Tejpal H, Chanana A, Rai G, Chaudhary R. A retrospective autopsy study of poisoning in the northern region of Punjab. J Punjab Acad Forensic Med Toxicol. 2008;8(2):17–19. [Google Scholar]
- 25.Shadnia S, Esmaily H, Sasanian G, Pajoumand A, Hassanian-Moghaddam H, Abdollahi M. Pattern of acute poisoning in Tehran-Iran in 2003. Hum Exp Toxicol. 2007;26(9):753–756. doi: 10.1177/0960327107083017 [DOI] [PubMed] [Google Scholar]
- 26.Z’gambo J, Siulapwa Y, Michelo C. Pattern of acute poisoning at two urban referral hospitals in Lusaka, Zambia. BMC Emerg Med. 2016;16(1):2. doi: 10.1186/s12873-016-0068-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kavalci C, Kavalci G, Durukan P. Poisoning cases in Trakya U Hospital, Turkey. J Toxicol. 2008;6(2):1–5. [Google Scholar]
- 28.Zöhre E, Ayrik C, Bozkurt S, et al. Retrospective analysis of poisoning cases admitted to the emergency medicine. Arch Iran Med. 2015;18(2):117. [PubMed] [Google Scholar]
- 29.Malangu N. Characteristics of acute poisoning at two referral hospitals in Francistown and Gaborone. S Afr Fam Pract. 2008;50(3):67–67c. [Google Scholar]
- 30.Abula T, Wondmikun Y. The pattern of acute poisoning in a teaching hospital, north-west Ethiopia. Ethiop Med J. 2006;44(2):183–189. [PubMed] [Google Scholar]
- 31.Marahatta S, Singh J, Shrestha R, Koju R. Poisoning cases attending emergency department in Dhulikhel hospital-Kathmandu university teaching hospital. Kathmandu Univ Med J. 2009;7(2):152–156. doi: 10.3126/kumj.v7i2.2711 [DOI] [PubMed] [Google Scholar]
- 32.Boyle JS, Bechtel LK, Holstege CP. Management of the critically poisoned patient. Scand J Trauma Resusc Emerg Med. 2009;17(1):1–11. doi: 10.1186/1757-7241-17-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brent J, Burkhart K, Dargan P, et al. Critical Care Toxicology: Diagnosis and Management of the Critically Poisoned Patient. Springer; 2017. [Google Scholar]
- 34.Hovda LR, Brutlag AG, Poppenga RH, Peterson KL. Emergency Management of the Poisoned Patient. Small Anim Toxicol. 2016:19. [Google Scholar]
- 35.McGlone MM, Teece SC. Management of the poisoned patient. Anaesth Intensive Care Med. 2016;17(10):506–509. doi: 10.1016/j.mpaic.2016.07.004 [DOI] [Google Scholar]
- 36.Morrison EE, Sandilands EA. Principles of management of the poisoned patient. Medicine. 2020;48(3):160–164. doi: 10.1016/j.mpmed.2019.12.003 [DOI] [Google Scholar]
- 37.Mudan A, Love JS, Greenwood JC, et al. The management of the poisoned patient using a novel emergency department-based resuscitation and critical care unit (ResCCU). Am J Emerg Med. 2020. doi: 10.1016/j.ajem.2020.06.068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schwarz E. Therapeutic approach to the critically poisoned patient In Critical Care Toxicology: Diagnosis and Management of the Critically Poisoned Patient. Springer International Publishing; 2017:43–78. [Google Scholar]
- 39.Malangu N, Ogunbanjo G. A profile of acute poisoning at selected hospitals in South Africa. South Afr J Epidemiol Infect. 2009;24(2):14–16. doi: 10.1080/10158782.2009.11441343 [DOI] [Google Scholar]
- 40.Raizada A, Kalra OP, Khaira A, Yadav A. Profile of hospital admissions following acute poisoning from a major teaching hospital in North India. Trop Doct. 2012;42(2):70–73. doi: 10.1258/td.2011.110398 [DOI] [PubMed] [Google Scholar]
- 41.Pap C, Zacher G, Kárteszi M. Prognosis in acute digitalis poisoning. Orvosihetilap. 2005;146(11):507–513. [PubMed] [Google Scholar]
- 42.Lee H-L, Lin H-J, Yeh ST-Y, Chi C-H, Guo H-R. Presentations of patients of poisoning and predictors of poisoning-related fatality: findings from a hospital-based prospective study. BMC Public Health. 2008;8(1):7. doi: 10.1186/1471-2458-8-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sam KG, Kondabolu K, Pati D, Kamath A, Kumar GP, Rao PG. Poisoning severity score, APACHE II and GCS: effective clinical indices for estimating severity and predicting outcome of acute organophosphorus and carbamate poisoning. J Forensic Leg Med. 2009;16(5):239–247. doi: 10.1016/j.jflm.2008.12.004 [DOI] [PubMed] [Google Scholar]