Abstract
Objective
Given the lack of studies examining the associations between daily weather and air pollution with nightly objective sleep over multiple weeks, we quantified these associations in a prospective cohort of healthy participants with episodic migraine.
Methods
Ninety-eight participants completed daily electronic diaries and wore an actigraph for an average of 45 days, and a total 4,406 nights of data were collected. Nightly sleep characteristics including duration, wake after sleep onset (WASO), and efficiency were assessed using wrist actigraphy. Daily weather parameters and air pollution levels were collected from local weather station and ground-level air quality monitors. We used linear fixed effects models adjusting for participant, day of the week, and day of the year (for weather analysis), and additionally adjusted for temperature and relative humidity (for air pollution analysis).
Results
The participants were 35±12 years old and 86 were women. A 10°F higher daily average temperature was associated with 0.88 (95% CI: 0.06, 1.70) minutes longer WASO and 0.14% (95% CI: −0.01%, 0.30%) lower sleep efficiency on that night. A 14 parts per billion (ppb)(interquartile range) higher daily maximum 8-hour ozone was associated with 7.51 (95% CI: 3.23, 11.79) minutes longer sleep duration on that night. Associations did not differ between cold (October-March) and warm (April-September) seasons.
Conclusions
Higher daily ozone was associated with longer sleep duration and modest associations were observed between higher temperature and lower WASO and lower efficiency.
Keywords: cohort study, actigraphy, sleep, weather, air pollution
1. Introduction
Numerous prospective studies demonstrate that inadequate sleep duration and quality are risk factors for incident major depressive episodes [1–3], obesity [4–6], diabetes [7], cardiovascular disease [8–10], and mortality [11–13], posing a substantial economic, medical, and social burden [14–17]. Yet, over 30% of adults sleep <7 hours per night, below the recommend duration for optimal sleep [18,19]. Thus, it is important to identify modifiable factors that negatively impact sleep duration and continuity to inform the development of novel interventions that target sleep and thereby mitigate these burdens.
Despite several large-scale epidemiological studies examining the associations of daily ambient weather parameters and air pollution on sleep-disordered breathing, there is limited data on the relationship between environmental exposures and nightly sleep characteristics beyond the scope of sleep disorders [20–23]. Much of the evidence is derived from highly-controlled laboratory environments. Higher room temperature (usually >30 °C) has been linked to shorter sleep duration, higher wakefulness, and lower efficiency [24–30]. Despite these observations, only one previous epidemiological study in 669 adolescents examined the association between daily meteorological factors and objective sleep in the naturalistic setting [31]. Using data from 7–10 days of actigraphy monitoring per participant, the authors reported that 10°F higher daily temperature was associated with 3.3 (95% CI: 1.7, 5.0) minutes shorter daily sleep duration.
Ambient air pollution may also be an environmental factor that impacts sleep continuity. A previous cross-sectional study found that higher short-term exposure to PM10 (particulate matter <10 μm in diameter) was associated with lower single-night polysomnography (PSG)-based sleep efficiency in summer [20]. The finding is supported by plausible underlying biological mechanisms, including air pollution-induced respiratory dysfunction and neuroinflammation.
Despite the high prevalence of inadequate sleep and the potential for environmental exposure to influence it at the population level, there has been no study that investigated whether daily ambient weather parameters and air pollution are associated with nightly sleep measured over multiple weeks in adults in the naturalistic settings. To elucidate the associations between daily environmental exposures (i.e. weather and air pollution) and nightly objective sleep, we analyzed data from a prospective cohort study that collected 4,406 nights of detailed sleep data using wrist actigraphy and electronic daily sleep diaries from 98 participants with episodic migraine followed over 6 weeks. These data represent a novel opportunity to investigate the associations of daily weather parameters (ambient temperature, relative humidity, barometric pressure) and ambient air pollution (particulate matter <2.5 μm in diameter [PM2.5], ozone [O3], nitrogen dioxide [NO2], sulfur dioxide [SO2], and carbon monoxide [CO]) with detailed nightly actigraphy and self-reported sleep characteristics among individuals with average levels of sleep disturbance.
2. Material and methods
2.1. Study sample
The details of our study have been described elsewhere [32–34]. Briefly, we conducted the study from March 2016 to October 2017. Potential participants were identified by: 1) accessing the patient and research repositories at Beth Israel Deaconess Medical Center (BIDMC) and the clinical research registries at the Massachusetts General Hospital and the Brigham and Women’s Hospital; 2) posting flyers in public areas and in the neurology and primary care clinics at BIDMC; and 3) physician’s referral. All eligible participants spoke English, were 18 years and older, had a diagnosis of episodic migraine, and reported at least 2 migraines/month over the past 3 months. We screened potential participants using the validated Berlin questionnaire [35] at the time of enrollment, all potential participants underwent a standard clinical evaluation by a board-certified sleep physician, and those who had undergone previous clinical diagnostic sleep testing had their study reports reviewed by the sleep physician. We excluded participants if they reported chronic pain or current opioid use; were at high risk for obstructive sleep apnea or had untreated moderate-severe sleep apnea (defined as ≥15 events/hour on previous clinical sleep testing); had a history of hypersomnia; reported ≤15 headache days/month in the past 3 months; were pregnant; or failed to complete diaries for 4 of the 7-day run-in period during the pre-baseline visit.
Of the 101 participants enrolled, we further excluded three participants because they contributed <21 days of diary data. In the end, we analyzed data from 98 participants. On average, we observed each participant for 45 days.
At baseline, each participant completed questionnaires that collected data on demographics, medication use, sleep symptoms, lifestyle factors, and psychological factors. Participants then completed an online diary each morning and evening and wore a wrist actigraph for the subsequent 6 weeks. The electronic data were collected by the Research Data Capture (REDCap) tools hosted by BIDMC [36]. All participants provided written informed consent and the study protocol was approved by the Committee on Clinical Investigations at BIDMC.
2.2. Daily weather and air pollution exposure
All participants lived in the Greater Boston Area. We obtained daily averages of ambient temperature, relative humidity, and barometric pressure from the Boston Logan Airport Weather Station (https://www.ncdc.noaa.gov/cdo-web/datasets/LCD/stations/WBAN:14739/detail). Daily levels of air pollutants were measured by local U.S. Environment Protection Agency (EPA) Air Quality System including daily mean PM2.5 (Roxbury, North End, and Von Hillern sites), daily maximum 1-hour SO2 (Kenmore and Roxbury sites), daily maximum 1-hour NO2 (Kenmore, Roxbury, and Von Hillern sites), daily maximum 8-hour O3 (Roxbury site), and daily maximum 8-hour CO (Roxbury and Von Hillern sites). All the monitoring sites are located within the Greater Boston Area. In our study region, ambient air pollutants are from both regional and local sources, including road traffic, power plants, and residential heating [37]. PM2.5 is a mixture of small solid particles and liquid droplets from both local and regional sources. Gaseous pollutants including O3, NO2, and CO are viewed as correlates of local traffic, and SO2 is primarily from regional sources such as fossil-fuel burning power plants. The data are publicly available and can be downloaded at: https://www.epa.gov/outdoor-air-quality-data/download-daily-data.
2.3. Nightly sleep outcomes
Wrist actigraphy has been established as a valid and objective method of estimating sleep-wake parameters in naturalistic settings [38–40]. Participants were asked to wear a wrist actigraph (Actiwatch Spectrum; Philips Respironics, Murrysville, PA) on their non-dominant wrist for 24 hours a day for at least 6 weeks. It collected data on movement and environmental light in 30-sec intervals and indicated any “off wrist” time. Our trained research coordinators provided the participants with instructions on operating the actigraph. After the devices were returned, we downloaded the data and transmitted to the Brigham and Women's Hospital Sleep Reading Center for scoring [40,41].
A trained technician who was blinded to participants’ questionnaire responses scored actigraphy data and manually identified the start and stop of the rest period using a hierarchical approach [42]. After designating the rest interval, sleep/wake status was determined using the Actiware 6.0 algorithm for each 30-sec epoch. The algorithm weights the activity counts in relationship to activity levels in the surrounding 2-min periods, and uses a wake threshold activity count of 40. Sleep onset was defined as 5 minutes of immobile time and sleep offset as the last epoch in the rest interval. We calculated total sleep duration, WASO (minutes), and efficiency (proportion of total sleep duration/duration of rest period, %).
We collected data on sleep latency and sleep quality from daily electronic diaries [43]. Each morning, participants were asked the question “How long did it take you to fall asleep last night?” and “How would you rate the quality of your sleep?”. Sleep quality was rated from “very poor, poor, fair, good, to very good”.
2.4. Statistical analysis
We calculated the average levels of temperature, relative humidity, barometric pressure, and air pollutants on the day of sleep onset. If the participant fell asleep after midnight, we assigned the exposure data on the day before to that sleep. We used multivariable linear fixed effects models that account for within person repeated measures to examine the associations of the daily average of each exposure with actigraphy-estimated sleep duration, wake after sleep onset (WASO), efficiency, and self-reported sleep latency.
In models of weather conditions and sleep outcomes, we adjusted for a participant identifier, day of week (categorical, 1–7), and day of year (continuous, 1–366). For analyses of air pollutants and sleep outcomes, we additionally included linear terms of temperature and relative humidity because we considered temperature and relative humidity as potential upstream common causes of both air pollution and sleep.
Weather, air pollution, hours of sun light, and sleep are likely affected by season. Therefore, we considered day of the year as an important confounder for the current analysis. Moreover, the associations of weather, air pollution, and sleep with time of a year may not be linear. To better account for the underlying seasonal patterns, we modeled day of the year as a restricted cubic spline term (mkspline2 in Stata) with boundary knots placed at March 1st and February 28th, and 3 inner knots placed at May 31st, August 31st, and November 31st. The inner knots were selected to reflect local seasonality patterns, and allows for different patterns in different seasons.
We then examined associations of weather and air pollution with binary indicators of high WASO, low sleep efficiency, and poor sleep quality. High WASO was defined as having actigraphy-estimated WASO above the 75th percentile (53 minutes), low sleep efficiency as having actigraphy-estimated sleep efficiency no greater than the 25th percentile (88%), and poor sleep quality as participants reported their nightly sleep quality as poor or very poor (14% of 4,088 responses). We applied multivariable logistic regression models, adjusting for the same covariates as in the corresponding linear regression models.
Because weather and air pollution may have cumulative effects on sleep, we also examined the associations using 2-day moving averages, defined as the average levels of exposure on the day of and the day prior to sleep onset. We further explored non-linear associations by modeling each exposure as a restricted cubic spline term with 3 knots placed at 10%, 50%, and 90% of the distribution, and we found no evidence of deviations from linearity. We also performed sensitivity analyses: 1) including both NO2 and O3 in the same model; 2) additionally adjusting for temperature in the models for relative humidity and barometric pressure; and 3) additionally adjusting for PM2.5 in the models for other air pollutants. Moreover, because the distribution of daily average SO2 were right-skewed, we excluded days with daily average SO2 above 2.1 parts per billion (ppb) (95th percentile) or with daily CO above 600 ppb (95th percentile), and re-analyzed the data. We also examined whether the associations differed between the warm season (April to September) and the cold season (October to March) using an interaction term.
To facilitate interpretation of the results, we scaled the parameter estimates for temperature by 10°F (5.6°C). We also scaled the parameter estimates for PM2.5 by 3.6 μg/m3, NO2 by 11.7 ppb, SO2 by 0.55 ppb, O3 by 14 ppb, CO by 150 ppb, relative humidity by 26.5%, and barometric pressure by 0.28 inHg. These factors approximate the interquartile range of the daily average levels. We reported differences in sleep duration, WASO, efficiency, and self-reported sleep latency, and odds ratios (ORs) for having high WASO, low sleep efficiency, and poor sleep quality, with 95% confidence intervals (CIs). Analyses were performed using mkspline2 and glm functions in Stata 13 (StataCorp. College Station, TX).
3. Results
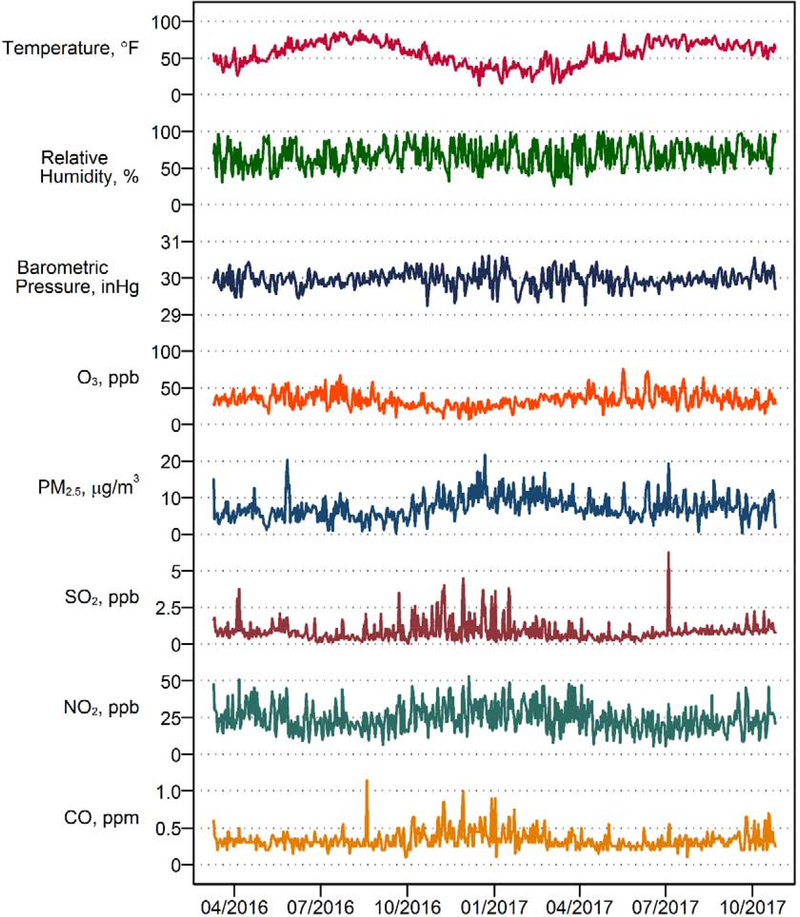
The mean age of the 98 study participants was 35.1 ± 12.1 years old, the majority were non-Hispanic whites (72%), and 86 (88%) were women, including 68 who were premenopausal (Table 1). At baseline, the average Pittsburgh Sleep Quality Index was 4.7 ± 3.0. During the follow-up, the average sleep duration was 7.3 ± 1.2 hours, WASO was 44.8 ± 17.0 minutes, and efficiency was 89.5% ± 3.3%. The daily average temperature during the study period was 56.9°F ± 16.0°F (13.8°C ± 8.9°C), and the daily average PM2.5 was 7.3 ± 3.2 μg/m3. Detailed distributions of temperature, relative humidity, barometric pressure, and air pollutants are included in Table S1. Figure 1 shows the daily levels of each weather parameter and air pollutant during the study period, which reflects typical weather and air pollution patterns in the Greater Boston area. The highest peak of SO2 in 2017 corresponds to the Independence Day (July 4th), potentially because of the increased traffic and fireworks. Moreover, July 4th, 2017 had slightly lower temperature, higher relative humidity, and lower wind speed compared to July 4th, 2016.
Table 1.
Sample characteristics at baseline and sleep characteristics during the study, among 98 patients of episodic migraine.
| Characteristics | Mean ± SD or N (%) |
|---|---|
| Age | 35.1 ± 12.1 |
| Women | 86 (88%) |
| Premenopausal | 68 (79%) |
| Non-Hispanic White | 71 (72%) |
| Pittsburgh Sleep Quality Index | 4.7 ± 3.0 |
| Actigraphy-based sleep duration, hour | 7.3 ± 1.2 |
| Actigraphy-based wake after sleep onset, minutes | 44.8 ± 17.0 |
| Actigraphy-based sleep efficiency, % | 89.5 ± 3.3 |
| Self-reported sleep latency, minutes | 27.7 ± 30.0 |
Figure 1.
Daily levels of temperature, relative humidity, barometric pressure, ozone (O3), fine particulate matter (PM2.5), sulfur dioxide (SO2), nitrogen dioxide (NO2), and carbon monoxide (CO) in the Greater Boston area, Massachusetts, 2016–2017.
3.1. Weather and sleep characteristics
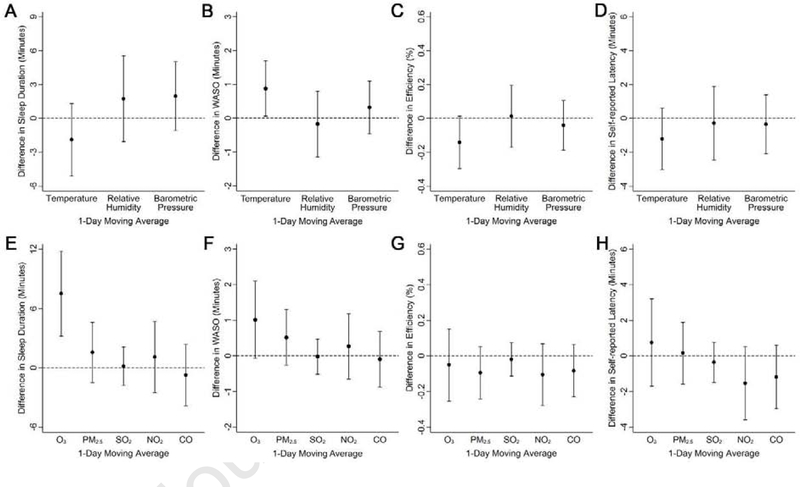
Higher temperature was associated with modestly higher WASO (Figure 2B) and lower sleep efficiency (Figure 2C). For example, a 10°F higher daily average temperature was associated with 0.88 minutes (95% CI: 0.06, 1.70) longer WASO and 0.14% (95% CI: −0.01%, 0.30%) lower sleep efficiency on that night. There were no consistent associations between meteorology and sleep duration, self-reported latency, binary indicators of WASO, efficiency, and sleep quality (Figures 2 and S1).
Figure 2.
Associations of weather and air pollution with continuous measures of sleep among participants with migraine in the Greater Boston area, Massachusetts, 2016–2017. Models were adjusted for day of week, a restricted cubic spline term of day of year, and a participant identifier. Models for air pollution were additionally adjusted for temperature and relative humidity. Results were scaled to 10°F for temperature, 26.5% for relative humidity, 0.28 inHg for barometric pressure, 3.6 μg/m3 for fine particulate matter (PM2.5), 11.7 ppb for nitrogen dioxide (NO2), 0.55 ppb for sulfur dioxide (SO2), 14 ppb for ozone O3, and 150 ppb for carbon monoxide (CO). Error bars indicate the 95% confidence intervals.
3.2. Air pollution and sleep characteristics
Higher levels of daily maximum 8-hour O3 was associated with longer sleep duration (Figure 2E): a 14 ppb (interquartile range) higher daily maximum 8-hour O3 was associated with 7.51 minutes (95% CI: 3.23, 11.79) longer sleep duration. We also found modest positive associations between O3 and WASO (Figure 2F). However, lower SO2 and CO were associated with having high WASO (Figure S1D). There were no other consistent associations between air pollution and sleep characteristics.
3.3. Sensitivity analyses
Using 2-day moving averages led to similar findings, except that a 11.7 ppb higher 2-day moving average of NO2 was associated with a 0.26% (95% CI: 0.04%, 0.48%) lower sleep efficiency. The associations did not differ between the cold and warm season (Figures S2 and S3). Adjusting for NO2 and O3 in the same model; adjusting for temperature in weather analysis; and adjusting for PM2.5 in air pollution analysis did not alter our results materially. Last, after excluding days with higher levels of SO2 or CO, the negative associations of SO2 and CO with presence of high WASO were attenuated.
4. Discussion
In this prospective cohort study, we found that higher daily O3 was associated with longer nightly sleep duration, and higher daily average temperature was associated with modestly higher WASO and lower efficiency. To our knowledge, this is the first study to examine the associations of daily weather and air pollution with repeated objective assessments of nightly sleep among adults over a period of several weeks.
Numerous animal and human studies have examined the health effects of ozone [44]. Two major pathways have been suggested: (1) ozone may induce oxidative stress and inflammation in the respiratory system, and respiratory tract injury, and (2) ozone may react with the sensory nerves in the lung, modulate autonomic nervous system and activate sympathetic nervous system, triggering neuroendocrine stress responses. Both pathways can cause systemic oxidative stress and inflammation [44]. Additionally, circulating inflammatory cytokines and reactive oxygen species may reach the brain through bloodstream, causing neuroinflammation [44]. Therefore, exposure to ozone may contribute to sleep problems through decreased pulmonary function, increased respiratory symptoms, and neuroinflammation. Particulate matter and other gaseous pollutants may share the same biological pathways as ozone. Moreover, inhaled particle pollutants may be directly transmitted into the brain via the cribriform plate and detected by the olfactory bulb, or induce local and systemic inflammation that lead to production of inflammatory biomarkers capable of reaching the brain [45–47].
In the current study, the associations for O3 were small, which may be due to relatively low levels of O3 in our study region (average 33.6 ± 10.4 ppb during our study) compared to the U.S EPA national standard of 8-hour O3 (70 ppb). Limited previous studies have examined the associations between daily air pollution and objectively assessed sleep duration or WASO. One study examining the associations between monthly average BC and self-reported sleep duration reported generally null associations. Two studies that examined the associations between air pollution and sleep efficiency had inconsistent findings: in the Sleep Heart Health Study, short-term exposure to higher PM10 was associated with lower single-night PSG-based sleep efficiency across individuals only in summer [20], and in the Multi-Ethnic Study of Atherosclerosis study, average single-day PM2.5 level at baseline was not associated with sleep efficiency averaged over the subsequent 7 days of actigraphy recording [48]. We found that O3 was associated with longer sleep duration, which is opposite to our hypothesis. Therefore, O3 may not contribute to insufficient sleep on a population level. Unlike previous studies, we did not observe associations between other pollutants with sleep characteristics. This may be due to the generally low levels of air pollution in the region and the overall good sleep quality of our participants.
In addition, several studies conducted in highly controlled experimental settings, found that higher room temperature were associated with shorter sleep duration, higher wakefulness, and/or lower efficiency on polysomnography [24–30]. These studies generally had small sample sizes (≤40) and measured sleep characteristics in single night, except for one study lasting for 5 days [26]. Our study extends these data by evaluating daily fluctuations in temperature with objective sleep assessments over multiple weeks in the naturalistic setting. Moreover, our findings are generally consistent with one previous study that prospectively collected daily weather and objective nightly sleep data over 7 days among adolescents in the same region [31], which found that a 10°F higher daily temperature was associated with 3.3 (95% CI: 1.7, 5.0) minutes shorter daily sleep duration, 0.9 (95% CI: 0.0, 1.8) minute higher daily WASO, and 0.2% (95% CI: 0.1%, 0.3%) lower daily efficiency. In the current study, with at least 6 weeks of follow-up, we observed associations of daily ambient temperature with longer WASO and lower sleep efficiency, of similar magnitudes. However, we did not observe any association between weather and nightly sleep duration, which may be because we conducted the analyses in adults who may have shorter sleep duration than adolescents [49]. We also had a much longer observation period.
Evidence from previous studies also indicated that the associations of daily weather and air pollution with sleep may differ by season [20–23]. This may be due to higher levels of ambient O3 in the warm season and higher PM2.5 or PM10 in the cold season. Additionally, region-specific climate patterns may influence weather and air pollution levels, and compositions of ambient air pollutants likely differ by region. However, our findings did not differ by season.
Our study has a few limitations. First, the air pollution levels in our study region were relatively low during the follow-up, which may influence our ability to assess the relatively small variation in measured sleep characteristics that can be attributed to daily ambient air pollution. Second, the study participants were patients with episodic migraine and predominantly women with European ancestry. Although the participants generally reported good sleep quality during the follow-up, our findings may still have limited generalizability to other populations. Third, there is a possibility that some of the participants had undiagnosed obstructive sleep apnea. However, 69% of our final study sample was comprised of young premenopausal women. Therefore, we presumed that the prevalence of obstructive sleep apnea among our sample was low. Fourth, weather conditions were measured at one fixed station and air pollution levels were measured at several local fixed stations, which may induce non-differential measurement errors that may have attenuated the statistical power. Additionally, we did not assess indoor thermal conditions or levels of air pollution. Previous studies showed moderate to high correlations between indoor and outdoor sulfate over the year, whereas the correlations for indoor and outdoor PM2.5 was moderate to high in summer but lower in winter. The correlations for other gaseous pollutants were generally low [50–52]. It is possible that indoor thermal conditions and air pollution are more relevant, and future studies are needed to examined these associations. Last, although we collected 4,406 nights of sleep data from 98 participants, we may have inadequate statistical power to examine season-specific associations of weather and air pollution with objective measures of sleep.
There are also some strengths. First, we objectively estimated nightly sleep among study participants for at least 6 weeks using standardized protocols. To our knowledge, this is one of the first studies to examine associations of daily weather and air pollution with repeated measures of sleep over several weeks in adults. Second, we used fixed effect models that accounted for participants’ time-invariant conditions during the relatively short follow-up period, such as age, sex, and socioeconomic position. Our study design and within-person analysis accounted for each individual’s sleep pattern, and may better capture the impact of daily weather and air pollution on their nightly sleep. Third, we conducted several sensitivity analyses and found our results to be robust. Fourth, the weather conditions and air pollution levels were measured by National Oceanic and Atmospheric Administration and U.S. EPA, independent of assessment of sleep.
5. Conclusions
Among the 98 patients with episodic migraine who were otherwise in good health and without known sleep-related disorders, we found that daily maximum 8-hour O3 was associated with longer sleep duration, and higher ambient temperature was associated with modestly higher WASO and lower efficiency. Future larger-scale studies with longer follow-up time are warranted in other regions with differing meteorology and air pollution patterns.
Supplementary Material
Highlights.
Weather and air pollution have been associated with sleep-disordered breathing
The impact of daily weather and air pollution on sleep remains unclear
We collected 4,406 nights of sleep data from 98 participants
Higher daily ozone is related to longer nightly sleep duration
Higher daily temperature is modestly related to higher sleep fragmentation
Acknowledgements
Funding: This work was supported by American Sleep Medicine Foundation, the National Institute of Health grant 1R21NS091627-01A1, and Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR002541) and financial contributions from Harvard University and its affiliated academic healthcare centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or the National Institutes of Health.
Financial disclosure: Dr. Bertisch reports research support from Lockheed Martin and ApniMed, and personal fees from Verily, Eisai Inc, and Merck. All other authors declare no financial conflict of interest.
Abbreviations
- BIDMC
Beth Israel Deaconess Medical Center
- CO
carbon monoxide
- CI
confidence interval
- EPA
Environment Protection Agency
- NO2
nitrogen dioxide
- O3
ozone
- OR
odds ratio
- ppb
parts per billion
- PSG
polysomnography ()
- PM2.5
particulate matter <2.5 μm in diameter
- PM10
particulate matter <10 μm in diameter
- REDCap
Research Data Capture
- SO2
sulfur dioxide
- WASO
wake after sleep onset
Footnotes
Non-financial disclosure: none.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Roth T, Roehrs T. Insomnia: epidemiology, characteristics, and consequences. Clin Cornerstone. 2003; 5 (3): 5–15. [DOI] [PubMed] [Google Scholar]
- 2.Salo P, Sivertsen B, Oksanen T, et al. Insomnia symptoms as a predictor of incident treatment for depression: prospective cohort study of 40,791 men and women. Sleep Med. 2012; 13 (3): 278–284. [DOI] [PubMed] [Google Scholar]
- 3.Sivertsen B, Lallukka T, Salo P, et al. Insomnia as a risk factor for ill health: results from the large population-based prospective HUNT Study in Norway. J Sleep Res. 2014; 23 (2): 124–132. [DOI] [PubMed] [Google Scholar]
- 4.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity(Silver Spring). 2008; 16 (3): 643–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. Am J Epidemiol. 2006; 164 (10): 947–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008; 31 (5): 619–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ayas NT, White DP, Al-Delaimy WK, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003; 26 (2): 380–384. [DOI] [PubMed] [Google Scholar]
- 8.Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011; 32 (12): 1484–1492. [DOI] [PubMed] [Google Scholar]
- 9.Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003; 163 (2): 205–209. [DOI] [PubMed] [Google Scholar]
- 10.Bertisch SM, Pollock BD, Mittleman MA, et al. Insomnia with objective short sleep duration and risk of incident cardiovascular disease and all-cause mortality: Sleep Heart Health Study. Sleep. 2018; 41 (6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel SR, Ayas NT, Malhotra MR, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004; 27 (3): 440–444. [DOI] [PubMed] [Google Scholar]
- 12.Sivertsen B, Pallesen S, Glozier N, et al. Midlife insomnia and subsequent mortality: the Hordaland health study. BMC Public Health. 2014; 14: 720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wallace ML, Stone K, Smagula SF, et al. Which Sleep Health Characteristics Predict All-Cause Mortality in Older Men? An Application of Flexible Multivariable Approaches. Sleep. 2018; 41 (1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.St-Onge MP, Grandner MA, Brown D, et al. Sleep Duration and Quality: Impact on Lifestyle Behaviors and Cardiometabolic Health: A Scientific Statement From the American Heart Association. Circulation. 2016; 134 (18): e367–e386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Itani O, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. 2017; 32: 246–256. [DOI] [PubMed] [Google Scholar]
- 16.Jike M, Itani O, Watanabe N, Buysse DJ, Kaneita Y. Long sleep duration and health outcomes: A systematic review, meta-analysis and meta-regression. Sleep Med Rev. 2018; 39: 25–36. [DOI] [PubMed] [Google Scholar]
- 17.Grandner MA, Alfonso-Miller P, Fernandez-Mendoza J, Shetty S, Shenoy S, Combs D. Sleep: important considerations for the prevention of cardiovascular disease. Curr Opin Cardiol. 2016; 31 (5): 551–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of Healthy Sleep Duration among Adults--United States, 2014. MMWR Morb Mortal Wkly Rep. 2016; 65 (6): 137–141. [DOI] [PubMed] [Google Scholar]
- 19.Mukherjee S, Patel SR, Kales SN, et al. An Official American Thoracic Society Statement: The Importance of Healthy Sleep. Recommendations and Future Priorities. Am J Respir Crit Care Med. 2015; 191 (12): 1450–1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zanobetti A, Redline S, Schwartz J, et al. Associations of PM10 with sleep and sleep-disordered breathing in adults from seven U.S. urban areas. Am J Respir Crit Care Med. 2010; 182 (6): 819–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weinreich G, Wessendorf TE, Pundt N, et al. Association of short-term ozone and temperature with sleep disordered breathing. Eur Respir J. 2015; 46 (5): 1361–1369. [DOI] [PubMed] [Google Scholar]
- 22.Cassol CM, Martinez D, da Silva F, Fisher MK, Lenz M, Bos AJG. Is sleep apnea a winter disease?: meteorologic and sleep laboratory evidence collected over 1 decade. Chest. 2012; 142 (6): 1499–1507. [DOI] [PubMed] [Google Scholar]
- 23.Shen YL, Li WT, Lee KY, Chuang HC, Chen HW, Chuang KJ. Association of PM2.5 with sleep-disordered breathing from a population-based study in Northern Taiwan urban areas. Environ Pollut. 2018; 233: 109–113. [DOI] [PubMed] [Google Scholar]
- 24.Haskell EH, Palca JW, Walker JM, Berger RJ, Heller HC. The effects of high and low ambient temperatures on human sleep stages. Electroencephalogr Clin Neurophysiol. 1981; 51 (5): 494–501. [DOI] [PubMed] [Google Scholar]
- 25.Muzet A, Libert JP, Candas V. Ambient temperature and human sleep. Experientia. 1984; 40 (5): 425–429. [DOI] [PubMed] [Google Scholar]
- 26.Libert JP, Di Nisi J, Fukuda H, Muzet A, Ehrhart J, Amoros C. Effect of continuous heat exposure on sleep stages in humans. Sleep. 1988; 11 (2): 195–209. [DOI] [PubMed] [Google Scholar]
- 27.Libert JP, Bach V, Johnson LC, Ehrhart J, Wittersheim G, Keller D. Relative and combined effects of heat and noise exposure on sleep in humans. Sleep. 1991; 14 (1): 24–31. [DOI] [PubMed] [Google Scholar]
- 28.Okamoto-Mizuno K, Tsuzuki K, Mizuno K. Effects of mild heat exposure on sleep stages and body temperature in older men. Int J Biometeorol. 2004; 49 (1): 32–36. [DOI] [PubMed] [Google Scholar]
- 29.Okamoto-Mizuno K, Tsuzuki K, Mizuno K, Iwaki T. Effects of partial humid heat exposure during different segments of sleep on human sleep stages and body temperature. Physiol Behav. 2005; 83 (5): 759–765. [DOI] [PubMed] [Google Scholar]
- 30.Valham F, Sahlin C, Stenlund H, Franklin KA. Ambient temperature and obstructive sleep apnea: effects on sleep, sleep apnea, and morning alertness. Sleep. 2012; 35 (4): 513–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quante M, Wang R, Weng J, et al. Seasonal and weather variation of sleep and physical activity in 12–14-year-old children. Behav Sleep Med. 2019; 17 (4): 398–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mostofsky E, Mittleman MA, Buettner C, Li W, Bertisch SM. Prospective Cohort Stdy of Caffeinated Beverage Intake as a Potential Trigger of Headaches among Migraineurs. Am J Med. 2019; 132 (8): 984–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bertisch SM, Li W, Buettner C, et al. Nightly sleep duration, fragmentation, and quality an daily risk of migraine. Neurology. 2020; 94 (5): e489–e496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li W, Bertisch SM, Mostofsky E, Buettner C, Mittleman MA. Weather, ambient air pollution, and risk of migraine headache onset among patients with migraine. Environ Int. 2019; 132: 105100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Senaratna CV, Perret JL, Matheson MC, et al. Validity of the Berlin questionnaire in detecting obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med Rev. 2017; 36: 116–124. [DOI] [PubMed] [Google Scholar]
- 36.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data captre (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42 (2): 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Masri S, Kang CM, Koutrakis P. Composition and sources of fine and coarse particles collected during 2002–2010 in Boston, MA. J Air Waste Manag Assoc. 2015; 65 (3): 287–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marino M, Li Y, Rueschman MN, et al. Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. 2013; 36 (11): 1747–1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sadeh A. The role and validity of actigraphy in sleep medicine: an update. Sleep Med Rev. 2011; 15 (4): 259–267. [DOI] [PubMed] [Google Scholar]
- 40.Weiss AR, Johnson NL, Berger NA, Redlines S. Validity of activity-based devices to estimate sleep. J Clin Sleep Med. 2010; 6 (4): 336–342. [PMC free article] [PubMed] [Google Scholar]
- 41.Smith MT, McCrae CS, Cheung J, et al. Use of Actigraphy for the Evaluation of Sleep Disorders and Circadian Rhythm Sleep-Wake Disorders: An American Academy of Sleep Medicine Systematic Review, Meta-Analysis, and GRADE Assessment. J Clin Sleep Med. 2018; 14 (7): 1209–1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Patel SR, Weng J, Rueschman M, et al. Reproducibility of a Standardized Actigraphy Scoring Algorithm for Sleep in a US Hispanic/Latino Population. Sleep. 2015; 38 (9): 1497–1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carney CE, Buysse DJ, Ancoli-Israel S, et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep. 2012; 35 (2): 287–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.U.S. Environmental Protection Agency. Integrated Science Assessment(ISA)for Ozone and Related Photochemical Oxidants. In. April 2020 ed: U.S. Environmental Protection Agency; 2020. [Google Scholar]
- 45.Elder A, Gelein R, Silva V, et al. Translocation of inhaled ultrafine manganese oxide particles to the central nervous system. Environ Health Perspect. 2006; 114 (8): 1172–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Calderon-Garciduenas L, Leray E, Heydarpour P, Torres-Jardon R, Reis J. Air pollution, a rising environmental risk factor for cognition, neuroinflammation and neurodegeneration: The clinical impact on children and beyond. Rev Neurol (Paris). 2016; 172 (1): 69–80. [DOI] [PubMed] [Google Scholar]
- 47.Lucchini RG, Dorman DC, Elder A, Veronesi B. Neurological impacts from inhalation of pollutants and the nose-brain connection. Neurotoxicology. 2012; 33 (4): 838–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Billings ME, Gold D, Szpiro A, et al. The Association of Ambient Air Pollution with Sleep Apnea: The Multi-Ethnic Study of Atherosclerosis. Ann Am Thorac Soc. 2019; 16 (3): 363–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004; 27 (7): 1255–1273. [DOI] [PubMed] [Google Scholar]
- 50.Brown KW, Sarnat JA, Suh HH, Coull BA, Koutrakis P. Factors influencing relationships between personal and ambient concentrations of gaseous and particulate pollutants. Sci Total Environ. 2009; 407 (12): 3754–3765. [DOI] [PubMed] [Google Scholar]
- 51.Sarnat JA, Koutrakis P, Suh HH. Assessing the relationship between personal particulate and gaseous exposures of senior citizens living in Baltimore, MD. J Air Waste Manag Assoc. 2000; 50 (7): 1184–1198. [DOI] [PubMed] [Google Scholar]
- 52.Sarnat JA, Long CM, Koutrakis P, Coull BA, Schwartz J, Suh HH. Using Sulfur as a Tracer of Outdoor Fine Particulate Matter. Environmental Science & Technology. 2002; 36 (24): 5305–5314. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.