Abstract
Psychosis is common among individuals with neurocognitive disorders, is difficult to manage, and causes considerable burden and stress to patients and caregivers. Developing effective treatments is a substantial unmet medical need but research has been slowed by the need for updated consensus diagnostic criteria. To address this need, the International Psychogeriatrics Association (IPA) initiated a process to develop criteria for clinical use, research, and treatment development efforts. The process included clinical, regulatory, and industry stakeholders as well as input from a global network of experts in geriatric psychiatry responding to two surveys (N=336). Results from the consensus process confirmed that clinicians wanted elaboration of aspects of the definition proposed by Jeste and Finkel in 2000 to ensure that the criteria are applied appropriately. Based on discussions, the survey, and emerging research, criteria were revised to apply to psychosis occurring with all major and mild neurocognitive disorders. Other important changes include providing examples of hallucinations and delusions and clarifying time course, impact, and exclusionary criteria. This definition of psychosis in major and mild neurocognitive disorders can be used to advance many types of research including development of much needed pharmacologic and nonpharmacologic interventions for psychosis in patients with neurocognitive disorders.
Keywords: Alzheimer’s disease, psychosis, major neurocognitive disorder, mild neurocognitive disorder, hallucinations, delusions, diagnoses, therapy development, clinical trials
Introduction
Psychosis and other psychiatric and behavioral syndromes are common in neurocognitive disorders (NCD) and are difficult to treat and manage, compromising patient quality of life and causing caregiver stress and frustration. In addition to the behavioral disturbances themselves, neuropsychiatric symptoms are associated with increased healthcare utilization, institutionalization, and mortality(1). The prevalence of psychosis in NCD varies depending on the underlying disease, with an overall prevalence of approximately 30% in Alzheimer’s disease (AD), 75% in dementia with Lewy bodies (DLB), 50% in Parkinson’s disease (PD), 15% in vascular dementia (VaD), and 10% in frontotemporal dementia (FTD)(2).
Developing effective pharmacologic and nonpharmacologic interventions for psychosis in NCD is a major unmet medical need; and the absence of contemporary consensus criteria for defining, identifying, and classifying psychotic symptoms has impeded progress in clinical management and drug development. We saw a role for the International Psychogeriatric Association (IPA) as a neutral body in addressing revisions of the widely used Jeste and Finkel criteria of 2000(3) with the goal of providing updated criteria for clinical use, epidemiologic studies, and interventional research. Drs. Jeste and Finkel (members of the IPA) concurred that after 20 years of use, a reconsideration of the specifics of the criteria was warranted. The process consisted of forming a small work group of international leaders to create a survey with questions about how the current criteria could be improved and sending the survey to IPA members and affiliate members. After completion and analysis of the survey, a larger international multi-stakeholder work group was formed and met in person. A review of the literature, definition-related talks by advisory board attendees, review of the survey results, and discussion of proposed changes in the definition comprised the elements of the meeting. Following the meeting, draft criteria were developed, circulated, and adjusted in a reiterative process. The draft criteria were circulated to IPA members and affiliate members with a survey to assess views of the proposed revised criteria. All elements of the process were synthesized into a manuscript that was circulated among the work group members to reach consensus on the manuscript through a reiterative process.
IPA has a long history of defining and evaluating behavioral and psychological symptoms of dementia (BPSD), also referred to as neuropsychiatric symptoms (NPS), in recognition that they occur in many neurodegenerative diseases. For example, in 2015, the IPA published a provisional consensus clinical and research definition of agitation in cognitive disorders(4). These criteria have been influential in advancing the development of both pharmacological and nonpharmacological treatments. The process followed in reaching consensus on a definition of agitation in cognitive disorders was used as a model for the development of a consensus definition of psychosis in NCD.
The rising prevalence of AD(5), limited progress in developing curative or preventive interventions, increasing public concern about the impact of the disease on public health and economies worldwide, and the need to stimulate research into neuropsychiatric disorders in the elderly, motivated the IPA to address the challenge of defining psychosis in NCD. Other motivating factors included advances in understanding the pathophysiology of psychosis in NCD, the development of biomarkers of AD and other NCDs, continued research on the pharmacological and psychosocial management of psychopathology, and emerging technologies that may expedite detection, identification, and classification of NPS. Alignment with revisions of major classification systems under consideration (e.g., Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5®)(6) and the International Classification of Disease, 11th edition (ICD 11)(7) is improved if consensus is reached on a definition of psychosis in NCDs.
Multiple sets of diagnostic criteria have been proposed to define psychosis in AD and other NCDs. Those introduced by Jeste and Finkel in 2000 (Table 1)(3) have been widely used in the field but lack specificity regarding severity and duration of symptoms and also exclude patients who exhibit psychotic symptoms prior to a dementia diagnosis(8–11). Lyketsos and colleagues proposed criteria in 2001 based on empirical evidence from the Cache County study of memory and aging(12). They proposed grouping AD patients into three clusters based on different patterns of NPS: 1) minimally affected persons with only one NPS, 2) persons with multiple but predominantly affective NPS, and 3) those with multiple but predominantly psychotic NPS. A recent review of the criteria for psychosis in NCD concluded that greater differentiation of hallucinations and delusions, better description of associated syndromes (e.g., agitation), facilitating earlier diagnosis in prodromal states, and promoting development of relevant biomarkers were priorities for the field(13).
Table 1 –
Diagnostic criteria for psychosis of AD, 2000.
| A. Characteristic Symptoms |
| Presence of one (or more) of the following symptoms: |
| 1. Visual or auditory hallucinations |
| 2. Delusions |
| B. Primary Diagnosis |
| All the criteria for dementia of the Alzheimer type are met |
| C. Chronology of the onset of symptoms of psychosis vs. onset of symptoms of dementia |
| There is evidence from the history that the symptoms in Criterion A have not been present continuously since prior to the onset of the symptoms of dementia |
| D. Duration and Severity |
| The symptom(s) in Criterion A have been present, at least intermittently, for 1 month or longer. Symptoms are severe enough to cause some disruption in patients’ and/or others’ functioning. |
| E. Exclusion of schizophrenia and related psychotic disorders |
| Criteria for Schizophrenia, Schizoaffective Disorder, Delusional Disorder, or Mood Disorder with Psychotic Features have never been met |
| F. Relationship to delirium |
| The disturbance does not occur exclusively during the course of a delirium |
| G. Exclusion of other causes of psychotic symptoms |
| The disturbance is not better accounted for by another general-medical condition or direct physiological effects of a substance (e.g., a drug of abuse, a medication) |
| Associated features: (Specify if associated) |
| With Agitation: when there is evidence, from history or examination, of prominent agitation with or without physical or verbal aggression |
| With Negative Symptoms: when prominent negative symptoms, such as apathy, affective flattening, avolition, or motor retardation, are present |
| With Depression: when prominent depressive symptoms, such as depressed mood, insomnia or hypersomnia, feelings of worthlessness or excessive or inappropriate guilt, or recurrent thoughts of death, are present |
Note: For other dementias, such as vascular dementia, Criterion B will need to be modified appropriately.
The DSM-5®(6) uses “specifiers”, e.g., “major neurocognitive disorder due to Alzheimer’s disease with a behavioral disturbance (psychosis)”. The DSM approach distinguishes between major and mild NCDs and thus recognizes that psychosis may occur in mild cognitive impairment (MCI)(14) and in the predementia stage of neurocognitive disorders. However, it does not make a distinction between delusions and hallucinations and pays limited attention to the temporal relationship between onset of psychosis and course of the cognitive decline.
The International Society to Advance Alzheimer’s Research and Treatment (ISTAART) NPS Professional Interest Area (PIA) of the Alzheimer’s Association, collaborating with the IPA Psychosis Work Group (PWG), reviewed the literature concerning psychosis in NCDs (summarized below) and concluded that published criteria are limited by a lack of symptom specificity; unclear definitions of terms such as hallucinations and delusions; insufficient emphasis on the temporal development of psychotic symptoms; absence of biomarkers supportive of diagnostic criteria; and exclusion of means to identify psychosis in predementia states of NCDs(13). These observations contributed to the decision to reconsider the criteria for psychosis in NCD.
Methods: Consensus building process
INITIAL REVIEW OF THE LITERATURE
Preliminary studies suggest that delusions can be divided into two main types, persecutory and misidentification. Using cross-sectional data, Cook et al(15) found two principal subtypes of psychosis in AD: 1) those with auditory and visual hallucinations combined with misidentification of people and 2) those with persecutory delusions. Persecutory delusions typically revolve around predictable themes, including the delusions of theft, phantom boarders, abandonment, and infidelity; misidentification delusions include the imposter or replacement delusion of familiar persons, objects or self. Studies with diverse demographic populations are needed to confirm this grouping across the continuum of NCDs. Diverse types of hallucinations and delusions must be anticipated in a revised definition.
Psychosis in non-AD NCDs such as DLB, PD, FTD, and VaD show different patterns of psychotic symptoms but with substantial overlap (Figure 1). In AD, psychosis occurs mostly in the mid-stages of disease, delusions are typically paranoid (e.g., believing that things have been stolen or that unwelcome guests are present in the home), and visual hallucinations are more common than auditory. In DLB, delusions are often paranoid, can be very elaborate, and are often related to misidentification. In DLB, visual hallucinations, auditory hallucinations, and delusional misidentification increase as cognitive impairment worsens(16). Psychosis criteria applicable across NCDs must accommodate these differing phenotypes.
Figure 1.
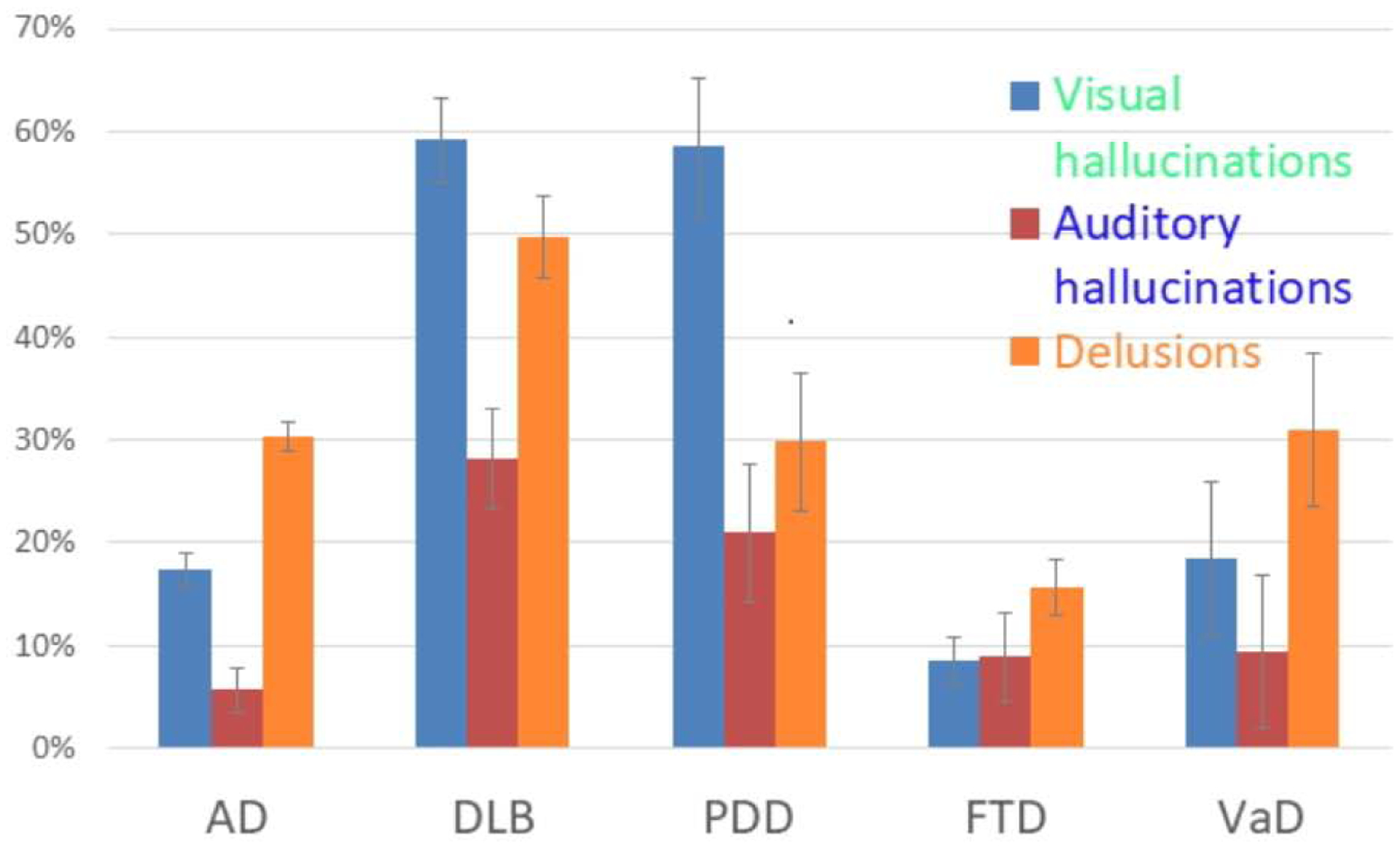
Prevalence of hallucinations and delusions in major types of dementia (contributed by Dr. Debby Tsuang and Andrew Shutes-David).
The temporal sequence of symptoms varies in different types of NCDs. In DLB, nonamnestic cognitive and neuropsychiatric symptoms emerge before motor symptoms(17). DLB is characteristically associated with fluctuating cognition and psychiatric and autonomic symptoms. In PD, psychotic symptoms change as the disease progresses; patients in early stages typically have minor illusions; these progress to hallucinations with insight, followed by hallucinations without insight, and finally to delusions. Variable persistence of symptoms, visual hallucinations, and misidentification are phenomenological features that may distinguish neurodegenerative causes of psychosis from non-neurodegenerative causes, although further research is required.
There are several subtypes of frontotemporal lobar degeneration including behavioral variant FTD (bvFTD), primary progressive aphasia, progressive supranuclear palsy (PSP), and corticobasal degeneration (CBD). Psychosis with fixed and bizarre delusions may lead to a misdiagnosis of schizophrenia in younger patients. The criteria should accommodate psychosis in all types of NCD.
In VaD, depression and apathy are the most common NPS in VaD; psychotic symptoms may occur, especially in the early stages. Hallucinations occur with a similar frequency as is seen in AD, while delusions are less common in VaD than in AD(18, 19). VaD rarely occurs in a pure form and the pathology of AD is often present at autopsy in patients diagnosed clinically with VaD. Criteria must accommodate the heterogeneity of psychosis across NCD.
Age differences (e.g., in young-onset versus late-onset NCD) may influence psychotic symptoms and sex differences may influence the type of psychotic symptoms reported. Criteria must apply across these dimensions.
Psychosis in NCDs can be triggered by multiple factors including medical conditions, pain, physical discomfort, urinary tract infection, constipation, delirium, polypharmacy, environmental factors that result in overstimulation or social isolation, premorbid personality, and maladaptive coping mechanisms. These factors must be accomodated in a definition of psychosis in NCD.
The expression of psychotic symptoms in NCDs and the management of patients is further complicated by differences in residential setting, with many advanced patients residing in long-term care institutions with mental or physical co-morbidities. Not only do these patients often display different patterns of hallucinations and delusions in combination with other NPS such as agitation, aggression, or apathy, but the environment may contribute to their distress.
Hallucinations can occur in non-psychotic neurological disorders such as eye disease, migraine, and post-stroke syndromes; this must be distiguished in the criteria.
Despite the heterogeneity in the diagnostic setting and manifestations of psychosis in NCDs, there are unifying principles that suggest that a single definition is appropriate for psychosis in NCDs and is applicable across diagnostic groups. There are four converging themes of research that suggest that a unified transdiagnostic approach to NCD-related psychosis is warranted.
Phenotypic definition: The original definition of psychosis in AD developed by Jeste and Finkel(3), states that the definition can be applied to other dementia syndromes. Psychosis is identified by delusions and hallucinations regardless of the neurological context in which it is found. The definition of psychosis demands delusions and/or hallucinations in every type of dementia, and this provides a common terminology and common phenotypic description across all types of dementia. Survey 1 (below) shows that most survey respondents endorsed the concept of one definition applicable across a broad range of NCDs.
Use of antipsychotics across dementia diagnoses: The same psychopharmacologic interventions are used for all disorders with the psychosis phenotype(20). Quetiapine and risperidone are widely used in AD, FTD, and VaD. Clozapine and quetiapine are more often chosen in patients with PD and DLB with psychosis given the sensitivity to antipsychotic interventions conferred by these disorders(21). Although efficacy is not as well studied as is desirable, available practice standards suggest that these agents are helpful across diagnoses.
Diagnostic overlap: There have been great efforts in recent years to differentiate among etiologies of dementia, for example, distinguishing AD with biomarker-based precision from FTD, DLB, VaD, and PD with dementia (PDD). This effort has been successful in demonstrating predominant etiologies of different dementia syndromes. These investigations have revealed the marked pathologic overlap among dementias and the rarity of pure disorders. Autopsy series show that among patients with a diagnosis of AD in life, only 30% have AD as the only pathology at the time of autopsy. Seventy percent have mixtures of vascular lesions, TAR DNA-binding protein-43 (TDP-43), and alpha-synuclein with the pathological changes of AD(22–24). This overlap of pathologies may contribute to shared pathogenesis of clinical syndromes among NCDs including psychosis.
Shared biology: Recent studies show that psychosis has similar magnetic resonance imaging and biomarker changes across neuropsychiatric disorders(25, 26). Genetic studies of AD and schizophrenia indicate that psychosis in AD—particularly delusions—may share genetic liability supporting a transdiagnostic view of psychotic symptoms(27). Investigations of misidentification delusions show the syndrome can be associated with lesions in multiple brain locations; all lesions sites are linked to circuits mediating expectation and familiarity(28). These preliminary studies suggest that transdiagnostic endophenotypes reflect a shared underlying biology.
SURVEY 1
The PWG created a survey to gather input from members on currently used criteria for psychosis in NCD. The intent of the survey was to determine if the survey participants consistently indicated necessary changes to the Jeste and Finkel criteria to enhance their utility. Members of IPA and affiliate organizations around the world that share the mission of advancing clinical practice, research, and education to improve the mental health of the elderly were invited by email to complete the survey. The survey was promoted on IPA social media channels and shared with other relevant professional networks. The email included a link to the online survey platform, SurveyMonkey®, which hosted the survey. Emails were sent three times over 90 days.
The survey was designed using the Jeste and Finkel diagnostic criteria for psychosis in AD (Table 1) (3) as a framework. Survey questions evaluated each major element of the criteria: characteristic symptoms of psychosis in AD, criteria for a primary diagnosis of NCD (AD, VaD, DLB, etc.), chronology of the onset of symptoms of psychosis as related to onset of symptoms of cognitive decline, duration and severity of symptoms, exclusionary criteria, the relationship of psychosis to delirium, and associated features that should be specified (e.g., agitation, apathy, depression.)
The survey was opened by 2,279 individuals; 428 individuals (18.8%) responded to some of the questions and 175 (7.7% of those who opened the email survey; 41% of those who chose to engage the survey) provided complete responses (data on responses are provided in Table 2). The data below reflect the answers of those who responded.
Table 2.
IPA Psychosis Survey 1.
| Question | Yes | No | Total | ||
|---|---|---|---|---|---|
| Q1 Characteristic symptoms are noted to be visual or auditory hallucinations or delusions. Would it be helpful to provide definitions of these symptoms (e.g., delusions are fixed false beliefs that the patient believes to be true)? | 230 | 68.45% | 106 | 31.55% | 336 |
| Q2 Would it be helpful to provide examples of these phenomena (e.g., silent individuals standing in the room; believing that one is not who one claims to be [Capgras syndrome], etc.)? | 262 | 77.98% | 74 | 22.02% | 336 |
| Q3 The primary diagnosis is noted to be dementia of the Alzheimer type. Should this be broadened to be any cognitive impairment syndrome (e.g., mild cognitive impairment, dementia with Lewy bodies, frontotemporal dementia, vascular dementia, etc.)? | 283 | 83.98% | 54 | 16.02% | 337 |
| Q4 Which cognitive impairment syndromes should be specifically identified: | |||||
| Mild cognitive impairment | 169 | 74.78% | 57 | 25.22% | 226 |
| Frontotemporal Dementia | 241 | 93.05% | 18 | 6.95% | 259 |
| Dementia with Lewy Bodies | 256 | 96.24% | 10 | 3.76% | 266 |
| Parkinson’s disease dementia | 245 | 94.96% | 13 | 5.04% | 258 |
| Vascular dementia | 248 | 96.12% | 10 | 3.88% | 258 |
| Progressive supranuclear palsy | 159 | 75.00% | 53 | 25.00% | 212 |
| Corticobasal degeneration | 157 | 73.02% | 58 | 26.98% | 215 |
| Traumatic brain injury | 159 | 73.27% | 58 | 26.73% | 217 |
| Others (comments listed at end) | 62 | 48.44% | 66 | 51.56% | 128 |
| Q5 If the criteria are broadened would it be better to use major and minor neurocognitive disorder as the major diagnostic designations? | 182 | 68.42% | 84 | 31.58% | 266 |
| Q6 If the criteria are broadened would it be better to use major and minor neurocognitive disorder as the major diagnostic designations followed by the specific diagnoses listed above? | 202 | 75.94% | 64 | 24.06% | 266 |
| Q7 The criteria note that the hallucinations and delusions cannot have been present before the onset of the dementia. Do you support this ordering with the presence of the dementia syndrome first followed by the onset of the symptoms of psychosis? | 154 | 57.46% | 114 | 42.54% | 268 |
| Q8 The criteria require that the symptoms of psychosis have been present at least intermittently for 1 month prior to diagnosis. What do you think is the appropriate interval of symptom duration prior to diagnosis? | . | 267 | |||
| 6 months | 33 | 12.36% | |||
| 2 months | 29 | 10.86% | |||
| 1 month | 95 | 35% | |||
| 2 weeks | 35 | 13.11% | |||
| 1 week | 8 | 3.00% | |||
| No specified duration | 67 | 25.09% | |||
| Q9 The criteria require that symptoms are severe enough to cause some disruption in patients’ and/or others’ functioning. Should “disruption” be defined such as interfering with the patient’s ability to accomplish activities of daily living or interact as usual socially. | 201 | 75.00% | 67 | 25.00% | 268 |
| Q10 The criteria include “duration and severity?” Should this section be divided into two, one section addressing duration and one section addressing severity? | 202 | 75.66% | 65 | 24.34% | 267 |
| Q11 Do you agree with the “patients’ or others’” functioning? | 180 | 67.42% | 87 | 32.58% | 267 |
| Q12 Should “others’ functioning” be changed or defined (e.g, interfering with the ability of others to care for or interact with the patient or causing distress to the partner). | 214 | 80.45% | 52 | 19.55% | 266 |
| Yes | No | Total | |||
| Q13 Would you add a reference to “posing a threat to the safety of self or others”? | 155 | 58.49% | 110 | 41.51% | 265 |
| Q14 Would you prefer that it pertains only to the patients’ functioning? | 87 | 32.71% | 179 | 67.29% | 266 |
| Q15 Should functioning be defined (e.g., being able to interact with family members and others, not being preoccupied with the hallucinations, etc)? | 194 | 73.21% | 71 | 26.79% | 265 |
| Q16 The definition requires that criteria for Schizophrenia, Schizoaffective Disorder, Delusional Disorder, or Mood Disorder with Psychotic Features have never been met. Do you agree with this criterion? | 168 | 63.16% | 98 | 36.84% | 266 |
| Q17 The criteria require that the disturbance does not occur exclusively during the course of a delirium. Could delirium be included as one of the cognitive impairment syndromes to which the new definition applies (e.g., “psychosis in delirium” as a diagnosis)? | 94 | 35.215 | 173 | 64.79% | 267 |
| Q18 Would you prefer to keep delirium as an exclusion for the diagnosis of psychosis in cognitive impairment? | 221 | 83.40% | 44 | 16.6% | 265 |
| Q19 The criteria require that the disturbance is not better accounted for by another general-medical condition or direct physiological effects of a substance (e.g., a drug of abuse, a medication).Could a general medical condition or effects of a substance be included as one of the cognitive impairment syndromes to which the new definition applies (e.g., “psychosis with hyperthyroidism” or other medical condition)? | 103 | 39.16% | 160 | 60.84% | 263 |
| Q20 Would you prefer to keep general medical conditions as an exclusion for the diagnosis of psychosis in cognitive impairment? | 212 | 80.30% | 52 | 19.70% | 264 |
| Q21 Would you prefer to keep effects of substances as exclusions for the diagnosis of psychosis in cognitive impairment? | 229 | 87.07% | 34 | 12.93% | 263 |
| Q22 Should we add that the psychosis is not “solely” attributable to another general-medical condition or direct physiological effects of a substance (e.g., a drug of abuse, a medication)? | 231 | 88.17% | 31 | 11.83% | 262 |
| Q23 The criteria specify that the psychotic symptoms are present with any of the following: agitation, negative symptoms, depression. Should “agitation” be continued as a notable accompanying syndrome in a new definition? | 203 | 76.32% | 63 | 23.68% | 266 |
| Q24 Should “aggression” be added a notable accompanying syndrome in the new definition? | 188 | 70.94% | 77 | 29.06% | 265 |
| Q25 Should “negative symptoms” be continued as a notable syndrome in a new definition? | 119 | 44.74% | 147 | 55.26% | 266 |
| Q26 Should “negative symptoms” replaced by “apathy” in a new definition? | 156 | 58.65% | 110 | 41.35% | 266 |
| Q27 Should “depression” be continued as a notable accompanying syndrome in a new definition? | 159 | 60.23% | 105 | 39.77% | 264 |
| Q28 Should depression with psychotic features be identified as a separate disorder to be excluded from the definition? | 189 | 71.05% | 77 | 28.95% | 266 |
| Q29 The symptoms are culturally appropriate (e.g., ancestor hallucinations in some cultures)? | 187 | 70.30% | 79 | 29.70% | 266 |
| Q30 Visual hallucinations are associated with blindness or other ocular diseases? | 197 | 74.06% | 69 | 25.94% | 266 |
| Q31 Auditory hallucinations are associated with hearing impairment? | 189 | 71.86% | 74 | 28.14% | 263 |
| Q32 Should distress of the patient be included as a criterion for psychosis in cognitive impairment? | 137 | 51.50% | 129 | 48.50% | 266 |
| Q33 Has distress of the patient as a criterion been adequately addressed in the previous questions on disturbance and functioning? | 155 | 58.49% | 110 | 41.51% | 265 |
Among respondents, 68.4% supported providing definitions such as “delusions are fixed false beliefs that the patient believes to be true”; and 78.0% supported providing examples such as “reporting there are silent individuals standing in the room” or of Capgras syndrome as the belief “that one is not who one claims to be.”
By a large majority (84.0%), survey respondents indicated that the primary diagnosis should be broadened from “dementia of the Alzheimer type” to any NCD. More than 90% supported specific identification of DLB, VaD, PDD, and FTD. Between 70 and 90% also favored specific identification of PSP, MCI, traumatic brain injury, and CBD.
Survey respondents further indicated that if the criteria are broadened, it would be better to use major and mild NCD as the primary diagnostic designation (supported by 68.4%), followed by the specific diagnosis (supported by 75.9%).
The current criteria note that hallucinations and delusions must have been present for at least 1 months to support a diagnosis of psychosis in dementia. Most respondents (57.5%) supported this approach; there was some lack of agreement on the appropriate interval of psychosis symptom duration prior to diagnosis of psychosis, ranging from having no specified duration (25.1%) to a high of 6 months (supported by 12.4% of respondents). An interval of one month received the most support (35.6%). 75.7% of respondents agreed that duration and severity should be addressed separately.
The Jeste and Finkel criteria (Table 1) require that symptoms are severe enough to cause some disruption in patients’ and/or others’ functioning. Three quarters (75.0%) of respondents favored defining “disruption” as: “e.g., interfering with the patient’s ability to accomplish activities of daily living or interact as usual socially.” Similarly, 73.2% favored defining “functioning” as: “e.g., being able to interact with family members and others”; 67.4% agreed that both patients’ and others’ functioning should be included; 32.7% preferred considering only the patient’s functioning. 80.4% agreed that ‘others’ functioning should be defined, for example, as “interfering with the ability of others to care for or interact with the patient or causing distress to the partner.” 58.5% supported adding a reference to “posing a threat to the safety of self or others.”
Survey respondents were split on the question of whether distress of the patient should be included as a criterion for psychosis in NCD, with 51.5% supporting this addition. A larger percentage (58.5%) felt that distress of the patient is adequately addressed by questions on disturbance of functioning.
Most (70.3%) survey respondents agreed that the symptoms that are culturally appropriate (e.g., ancestor hallucinations in some cultures) should be excluded from the diagnosis of psychosis. Similarly, there was slightly more agreement among respondents that visual hallucinations associated with blindness or other ocular diseases (74.1%) or auditory hallucinations associated with hearing impairment (71.9%) should be excluded from the diagnosis of psychosis.
The current criteria require excluding a diagnosis of psychosis of AD in patients who have ever met the criteria for schizophrenia, schizoaffective disorder, delusional disorder, or mood disorder with psychotic features; and those in whom the disturbance occurs exclusively during the course of delirium or when the disturbance is better accounted for by another general medical condition or the effects of substances such as medications or drugs of abuse. Respondents supported retaining these exclusions. 88% agreed that the criteria should indicate that psychosis is not ‘solely’ attributable to another general medical condition or direct physiological effects of a substance.
The Jeste and Finkel criteria require specifying when prominent agitation, negative symptoms, or depressive symptoms co-occur with psychotic symptoms. More than three quarters of survey respondents (76.3%) agreed that agitation should continue to be listed as a notable accompanying syndrome; 60.2% agreed that depression should continue to be listed as a notable accompanying syndrome. A greater percentage (71.0%) supported identifying “depression with psychotic features” as a separate disorder to be excluded from the definition of psychosis in NCD. 58.6% supported replacing the term “negative symptoms” with “apathy”; 44.7% supported listing this as a notable accompanying syndrome.
INTERNATIONAL EXPERT CONSENSUS MEETING ON DRAFT DEFINITION
Following completion and analysis of the survey, an international expert consensus meeting was held in Lisbon, Portugal to reexamine the criteria for psychosis in AD and develop revised criteria for based on new knowledge and understanding of the condition, information derived from the survey, and the experience and perspective of those in attendance. Participants in the consensus meeting included IPA members, international attendees, biopharma industry representatives, psychosis experts, advocates, medical directors of residential facilities, regulatory experts, and members of the ISTAART NPS PIA representing a range of disciplines and backgrounds (participants are listed as authors of this paper). Support for this meeting was provided by unrestricted grants from pharmaceutical companies; the selection of the working group, intellectual content development, and creation of this report were independent of this funding. Supporting companies did not have approval or alteration authority.
The meeting began with a discussion of the existing definition and an overview of the prevalence and phenomenology of psychosis in NCD, including a review of other disorders with psychosis. Survey results were reviewed and discussed. In addition, PWG members discussed the effects of psychosis on caregivers and whether these effects should be incorporated into the criteria. Regulatory aspects related to the definition of psychosis were examined.
REPORT PREPARATION AND ITERATIVE REVIEW
The organizers of the meeting, working with a professional science and medical writer, prepared a report on the consensus definition that emerged from the meeting and the results of the survey. The draft report was circulated among participants of the meeting and was discussed through emails and conference calls to gain consensus on the criteria and edit the manuscript. The proposed criteria were then shared with survey respondents and others, who made recommendations in a second survey that were incorporated into the final manuscript.
PROPOSED CRITERIA
The criteria which represent modifications to the Jeste and Finkel criteria(3) are provided in Table 3.
Table 3.
Revised criteria for psychosis in major or mild neurocognitive disorder.
| A. Characteristic Symptoms |
| Presence of one (or more) of the following symptoms: |
| 1. Visual or auditory hallucinations (e.g., seeing silent individuals standing in the room, seeing children in the yard, or seeing animals in the house) |
| 2. Delusions (fixed false beliefs that the patient believes to be true, e.g. that the spouse is unfaithful, that possessions are being stolen, or that one is not who one claims to be) |
| B. Primary Diagnosis |
| All the criteria for any major and mild neurocognitive disorder are met, with the etiologic diagnoses specified (e.g., major neurocognitive disorder (Alzheimer’s disease)). Specific diagnoses include Alzheimer’s disease, dementia with Lewy bodies, vascular dementia, Parkinson disease dementia, frontotemporal dementia, progressive supranuclear palsy, mild cognitive impairment, traumatic brain injury, and corticobasal degeneration. Other rarer causes of major and mild neurocognitive disorder are also appropriate when diagnosed as a cause of psychosis. |
| C. Chronology of the onset of symptoms of psychosis vs. onset of symptoms of |
| cognitive impairment |
| There is evidence from the history that the symptoms in Criterion A have not been present continuously since prior to the onset of the symptoms of dementia |
| D. Duration |
| The symptom(s) in Criterion A have been present, at least intermittently, for 1 month or longer. |
| E. Severity |
| Symptoms are severe enough to cause some disruption in patients’ and/or others’ functioning or pose a threat to the safety of self or others. “Disruption” is defined as interfering with the |
| patient’s or others’ ability to accomplish activities of daily living or interact as usual socially; “patient’s functioning” is defined as being able to interact with family members and others, not being preoccupied with hallucinations, etc.; “other’s functioning” is defined as interfering with the ability of others to care for or interact with the patient or causing distress to the partner. |
| F. Exclusionary Criteria |
| A diagnosis of psychosis in major or mild neurocognitive disorder should be excluded in the following patients: |
| 1. Patients who have met the criteria for Schizophrenia, Schizoaffective Disorder, Delusional Disorder, Mood Disorder with Psychotic Features, or Depression with Psychotic Features. |
| 2. When the psychosis occurs exclusively during the course of a delirium. |
| 3. When the psychosis is solely attributable to another general-medical condition (e.g., hypothyroidism) or direct physiological effects of a substance (e.g., a drug of abuse, a medication). |
| 4. When the symptoms are culturally appropriate (e.g., ancestor hallucinations in some cultures). |
| 5. When the hallucinations are more readily attributable to conditions known to cause hallucinations such as epilepsy, migraine, disease of the sensory organs, or stroke. |
| G. Associated features: (Specify if associated) |
| With Agitation: when there is evidence, from history or examination, of prominent agitation with or without physical or verbal aggression. |
| With Depression: when prominent depressive symptoms, such as depressed mood, insomnia or hypersomnia, feelings of worthlessness or excessive or inappropriate guilt, or recurrent thoughts of death are present (note that Mood Disorder with Psychotic Features is an exclusion for the diagnosis of psychosis with major or mild neurocognitive disorders (see F.1 above) |
SURVEY 2
Following construction of the proposed revised criteria for psychosis in major and mild NCDs, a follow-up survey was sent to the IPA and affiliate members to assess their views of the criteria (complete response data to the survey are provided in supplemental material). One hundred thirty-nine respondents participated in the survey. The survey was opened by 2,351 individuals; 239 individuals (10.2%) responded to some of the questions and 179 (7.6% of those who opened the email; 75% of those who engaged the survey) provided complete responses. More than 85% of respondents found the expansion of the definitions (e.g., descriptions and examples of delusion and hallucinations) to be helpful. There was good agreement (78.7%) that the revised definition assists in distinguishing long-standing psychotic features from those beginning after the onset of the NCD. Similarly, there was agreement (72.2%) that a 1-month period was “reasonable” in terms of the requirement for duration of symptoms prior to diagnosis. Among respondents, 86.5% agreed with qualifying psychosis by noting the presence or absence of agitation, and 82.9% agreed with qualifying psychosis by noting the presence or absence of depression. Other informative outcomes included: 87.9% found it useful to include a definition of severity; 94.9% concurred with including the impact of the psychosis on others as part of the severity definition; 95.9% agreed with excluding delirium from the definition; 89.1% agreed with excluding the application of the definition if the symptoms appeared to be part of a shared cultural belief system. Overall, 88.5% found that the definition captures the phenomenology of the psychosis occurring with major and mild NCDs, and 90.0% found the definition to be an improvement over previous definitions of psychosis with NCDs. Thoughtful text responses were captured in the survey, resulting in minor adjustments to the criteria and others providing a basis for possible future revisions and assessing the utility of the current consensus definition.
Discussion
Here we convey the discussion of individual components of the revised definition.
Limitation to syndromes with cognitive impairment
The DSM-5(6) replaced the word “dementia” with the term “major neurocognitive disorder,” and added “mild neurocognitive disorder” to allow for the inclusion of prodromal stages of disease. It added specifiers to indicate the underlying condition (AD, FTD, LBD, VaD, PD, etc.). The PWG endorsed a broad application of psychosis in NCD and included in the definition AD, DLB, FTD, PD, VaD, PSP, CBD, Huntington’s disease, TBI, and mixed dementias. Other causes of major and mild NCD are appropriate when considered to be related to the psychosis.
Characteristic symptoms
Hallucinations are defined as the perception of an object or event in the absence of an external stimulus, for example, seeing, hearing, smelling, or feeling things that are not there. Delusions are fixed false beliefs that the patient believes to be true, for example, believing that someone is not who they claim to be (misidentification delusion) or that someone is trying to harm them (persecutory delusion). These descriptions are now included in the consensus definition.
Duration, severity, and excess disability
Symptoms of psychosis must be present for at least one month prior to diagnosis of major or mild NCD to meet the requirements of the revised criteria. Delusions and hallucinations may fluctuate, recur, or persist. The decision to require a minimum of one month of symptoms balances specificity with inclusivity.
Psychotic symptoms typically remit and recur intermittently but persist over time. Patterns appear to differ according to the type of NCD, e.g., individuals with DLB tend to have more persistent visual hallucinations(29). Psychotic symptoms may vary in severity. For definitional purposes, symptoms should be severe enough to cause a disruption in patients’ or others’ functioning or to pose a threat to the safety of self or others. Disruptions include interfering with the patient’s ability to accomplish activities of daily living or interact as usual as well as limiting the ability of others to interact with the patient. Duration and severity are now included in the consensus definition.
Notable accompanying syndromes
Psychosis in major or mild NCD is frequently accompanied by other NPS including agitation and depressive symptoms. These are now included as qualifying features of the revised consensus definition. Major depression with psychotic features is excluded from the diagnosis of psychosis in NCD.
Necessary exclusions
In the consensus definition, a diagnosis of psychosis with major or mild NCD will be excluded if the disturbance is better accounted for by effects of substances, including medications or drugs of abuse or by another medical condition, if the disturbance occurs exclusively during the course of delirium, or the criteria for schizophrenia, schizoaffective disorder, delusional disorder, or mood disorder with psychotic features are met and account for the symptoms.
Rating scales and checklists
Rating scales and checklists have been used to define behavior and assess the presence of psychotic symptoms. They may assist in detecting and characterizing behavioral changes in patients with NCD. Cohen-Mansfield and Golander compared several different scales that have been used to assess NPS in the residential setting: the Behavioral Pathology in Alzheimer’s Disease Rating Scale (BEHAVE-AD), the Neuropsychiatric Inventory-Nursing Homes (NPI-NH), the Consortium to Establish a Registry for Alzheimer’s Disease Behavior Rating Scale for Dementia (CERAD-BRSD), and the Columbia University Scale for Psychopathology in Alzheimer’s Disease (CUSPAD)(30). They found that the different scales result in variable prevalence rates for delusions and hallucinations although the BEHAVE-AD and NPI-NH yielded similar rates and showed high convergent validity.
A challenge in approaching psychosis in major and mild NCD is how best to describe behavior, recognizing that the terminology used affects how it is detected, characterized, and treated. Gerritsen and colleagues reviewed different approaches to conceptualizing the relationship between challenging behavior and NCD(31). They noted the importance of understanding why behavior is experienced as challenging. In assessing and interpreting delusions versus hallucinations, Gerritsen and coworkers suggested that it may be more important to focus on behavior rather than the delusions and hallucinations per se. It is also important to assess whether the delusions are amendable (less severe) or not amendable (more severe) to psychosocial interventions.
Including information on the causes and consequences of behaviors is important as a means of rating the severity of behavior. To capture these complex relationships, different rating scales may be needed for home versus institutional settings. Different scales may be needed for clinical practice versus clinical trials. Clinicians might benefit from a checklist or brief scales. These need to be designed and should capture most symptoms, include a severity component, and be sensitive to change (both in frequency and severity). Capturing all variables in a single rating scale may not be practical in clinical research, clinical trials, or practice. IPA PWG members concluded that appropriate scales and checklists based on the revised criteria are needed to improve detection and management of psychosis in NCD.
Psychosis may be amendable to nonpharmacological and pharmacological interventions and trials assessing both types of interventions are needed. Assessment of severity, persistence, and recurrence of symptoms as well as recognition of high rates of improvement in patients in placebo groups are required. Since criteria include “persistence” and “disruption,” it is important to acknowledge that intervention is likely needed, but what type of intervention will vary with the circumstances and the resources available. Delivery of treatment and management with both pharmacological and nonpharmacological approaches are not well defined and require further research to maximize implementation.
Regulatory issues
Clinical meaningfulness and clinical relevance of criteria are important issues for regulators. Definitions should help busy clinicians, inform clinical decision-making, and assist adherence to labeling of any approved treatments.
Regulatory acceptance of psychosis in major and mild NCD as an indication will require a specific definition, valid assessment tools, understanding of clinical meaningfulness, and the use of appropriate clinical trial designs with a well-defined target population and adequate safety endpoints. The proposed definition for psychosis in major and mild NCD will help advance these goals.
Conclusion and Next Steps
Comments on the survey clearly showed that clinicians endorse elaboration of aspects of the original definition of Jeste and Finkel(3) including more examples and definitions to ensure that the criteria are being applied appropriately. Providing clinicians with better tools for diagnosing and managing patients with psychosis in NCDs should facilitate efforts to deliver effective and safe treatments and provide much needed assistance to patients and their families. These consensus criteria represent an important step in advancing a research agenda to better understand the neurobiology of psychosis in NCD and develop novel, targeted therapeutics.
This process of developing a consensus definition has identified several gaps that need to be addressed to improve identification of individuals with NCD-related psychosis for inclusion in clinical research and clinical trials and for application in clinical care. These include the need to develop a checklist as a companion document to the definition, a care path algorithm, and descriptions with clinical vignettes on how to most effectively use these tools. Also needed is a framework for clinical meaningfulness, linked to this definition and to instruments developed to implement the definition.
Prospective validation of this consensus definition is required to establish its utility for research and clinical management. Diagnostic criteria typically begin as expert consensus initiatives followed by a reiterative process of implementation, evaluation, and adjustment. This process will be required for these criteria for psychosis in NCD.
There are several symptom types included in the psychosis in NCD criteria – delusions with different features, hallucinations of different types - and these may respond differentially to pharmacologic and nonpharmacologic interventions(32). Exploring the response profile will be an important aspect of the prospective implementation of these criteria.
Currently there are no approved treatments for the broad indication of psychosis in NCD; there is a high rate of misdiagnosis; high levels of psychosis-related distress; and enormous costs to the healthcare system associated with care of patients with this condition. This IPA.STAART definition provides a foundation for educating clinicians about psychosis in NCD as well as facilitating pharmacologic and nonpharmacologic research.
Highlights.
What is the primary question addressed by this study?
Criteria for psychosis in dementia have not been reviewed and revised for twenty years; new knowledge informed a process led by the International Psychogeriatric Association (IPA) to update these criteria.
What is the main finding of this study?
On the basis of 2 surveys of members, an international multi-stakeholder conference, and a reiterative consensus-building process, the original Jeste and Finkle criteria were updated with definitions of delusions and hallucinations, description of time frames, and notation of severity and accompanying features. The terminology of “psychosis in major and mild neurocognitive disorders” was adopted, expanding the definition into predementia phases of neurocognitive disorders.
What is the meaning of the finding?
The updated definition will assist in advancing clinical research and clinical trials leading to improved understanding, detection, recognition, and treatment of psychosis in major and mild neurocognitive disorders.
Acknowledgements
J. Cummings is supported by Keep Memory Alive (KMA); NIGMS grant P20GM109025; NINDS grant U01NS093334; and NIA grant R01AG053798. Z. Ismail has received funding for research and consultancy from Janssen, Otsuka and Lundbeck. K. Lanctot has received funding for research and advising from AbbVie Canada, ICG Pharma, Otsuka and Kondor Pharma. D. Tsuang has received research grants from NIH.
Conflicts of Interest and Sources of Funding
J. Cummings has received funding for research, consultancy and advising from Acadia, Actinogen, AgeneBio, Alkahest, Alzheon, Annovis, Avanir, Axsome, Biogen, BioXcel, Cassava, Cerecin, Cerevel, Cognoptix, Cortexyme, EIP Pharma, Eisai, Foresight, Gemvax, Green Valley, Grifols, Hisun, Idorsia, Karuna, Nutricia, Orion, Otsuka, Probiodrug, ReMYND, Resverlogix, Roche, Samumed, Samus Therapeutics, Third Rock, Signant Health, Sunovion, Suven, and United Neuroscience pharmaceutical and assessment companies. J Cummings has received consultancy fees from Alzheimer Drug Discovery Foundation; stock ownership in ADAMAS, BioAsis, MedAvante, QR Pharma, and United Neuroscience; and royalty fees for copyright ownership of Neuropsychiatric Inventory. J. Cummings is supported by Keep Memory Alive (KMA); NIGMS grant P20GM109025; NINDS grant U01NS093334; and NIA grant R01AG053798. G. Grossberg has received funding for consultancy from Acadia, Avanir, BioXcel and Otsuka. TJ Huang has received speaking honorariums from Janssen Pharmaceutical, Eisai Taiwan and Otsuka. Z. Ismail has received funding for research and consultancy from Janssen, Otsuka and Lundbeck. K. Lanctot has received funding for research and advising from AbbVie Canada, ICG Pharma, Otsuka and Kondor Pharma. C. Sampaio has received honorariums from vTv Therapeutics, Kyowa, Pfizer/ Lilly and Green Valley. D. Tsuang has received research grants from NIH. H. Wang has received honorariums from Eisai and Lundbeck and consulting fees from Eisai, Biogen, vTv and F. Hoffman LaRoche. K. Zhong, L. Cortez Pinto, M. Cruz, C. Fischer, D. Gerritsen, R. Koopmans, D. Jeste, R. Mateos, S. Peschin, and L.J. Bain have no disclosures to report.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lanctot KL, Amatniek J, Ancoli-Israel S, et al. : Neuropsychiatric signs and symptoms of Alzheimer’s disease: new treatment paradigms. Alzheimers Dement (N Y) 2017; 3:440–449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cummings J, Ballard C, Tariot P, et al. : Pimavanserin: potential treatment for dementia-related psychosis. J Prev Alzheimers Dis 2018; 5:253–258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeste DV,Finkel SI: Psychosis of Alzheimer’s disease and related dementias. Diagnostic criteria for a distinct syndrome. Am J Geriatr Psychiatry 2000; 8:29–34 [DOI] [PubMed] [Google Scholar]
- 4.Cummings J, Mintzer J, Brodaty H, et al. : Agitation in cognitive disorders: International Psychogeriatric Association provisional consensus clinical and research definition. Int Psychogeriatr 2015; 27:7–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prince M, Wimo A, Guerchet M, et al. : World Alzheimer Report 2015: The Global Impact of Dementia, London, Alzheimer’s Disease International (ADI), 2015 [Google Scholar]
- 6.American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 5th ed (DSM-5), Washington, D.C., American Psychiatric Association, 2013 [Google Scholar]
- 7.World Health Organization: ICD-11 for Mortality and Morbidity Statistics (ICD-11 MMS) 2018 version, Geneva, Switzerland, World Health Organization, 2018 [Google Scholar]
- 8.Chan DC, Kasper JD, Black BS, et al. : Prevalence and correlates of behavioral and psychiatric symptoms in community-dwelling elders with dementia or mild cognitive impairment: the Memory and Medical Care Study. Int J Geriatr Psychiatry 2003; 18:174–182 [DOI] [PubMed] [Google Scholar]
- 9.Gallagher D, Fischer CE,Iaboni A: Neuropsychiatric symptoms in mild cognitive impairment. Can J Psychiatry 2017; 62:161–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lyketsos CG, Lopez O, Jones B, et al. : Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: results from the cardiovascular health study. JAMA 2002; 288:1475–1483 [DOI] [PubMed] [Google Scholar]
- 11.Van der Mussele S, Marien P, Saerens J, et al. : Psychosis associated behavioral and psychological signs and symptoms in mild cognitive impairment and Alzheimer’s dementia. Aging Ment Health 2015; 19:818–828 [DOI] [PubMed] [Google Scholar]
- 12.Lyketsos CG, Sheppard JM, Steinberg M, et al. : Neuropsychiatric disturbance in Alzheimer’s disease clusters into three groups: the Cache County Study. Int J Geriatr Psychiatry 2001; 16:1043–1053 [DOI] [PubMed] [Google Scholar]
- 13.Fischer CE, Ismail Z, Youakim JM, et al. : Revisiting criteria for psychosis in Alzheimer’s disease and related dementias: toward better phenotypic classification and biomarker research. J Alzheimers Dis 2020; 73:1143–1156 [DOI] [PubMed] [Google Scholar]
- 14.Sachs-Ericsson N,Blazer DG: The new DSM-5 diagnosis of mild neurocognitive disorder and its relation to research in mild cognitive impairment. Aging Ment Health 2015; 19:2–12 [DOI] [PubMed] [Google Scholar]
- 15.Cook SE, Miyahara S, Bacanu SA, et al. : Psychotic symptoms in Alzheimer disease: evidence for subtypes. Am J Geriatr Psychiatry 2003; 11:406–413 [PubMed] [Google Scholar]
- 16.Suarez-Gonzalez A, Serrano-Pozo A, Arroyo-Anllo EM, et al. : Utility of neuropsychiatric tools in the differential diagnosis of dementia with Lewy bodies and Alzheimer’s disease: quantitative and qualitative findings. Int Psychogeriatr 2014; 26:453–461 [DOI] [PubMed] [Google Scholar]
- 17.Ferman TJ, Smith GE, Kantarci K, et al. : Nonamnestic mild cognitive impairment progresses to dementia with Lewy bodies. Neurology 2013; 81:2032–2038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lyketsos CG, Steinberg M, Tschanz JT, et al. : Mental and behavioral disturbances in dementia: findings from the Cache County Study on Memory in Aging. Am J Psychiatry 2000; 157:708–714 [DOI] [PubMed] [Google Scholar]
- 19.Treiber KA, Lyketsos CG, Corcoran C, et al. : Vascular factors and risk for neuropsychiatric symptoms in Alzheimer’s disease: the Cache County Study. Int Psychogeriatr 2008; 20:538–553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirkham J, Sherman C, Velkers C, et al. : Antipsychotic use in dementia. Can J Psychiatry 2017; 62:170–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hershey LA,Coleman-Jackson R: Pharmacological management of dementia with Lewy bodies. Drugs Aging 2019; 36:309–319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brenowitz WD, Keene CD, Hawes SE, et al. : Alzheimer’s disease neuropathologic change, Lewy body disease, and vascular brain injury in clinic- and community-based samples. Neurobiol Aging 2017; 53:83–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.James BD, Wilson RS, Boyle PA, et al. : TDP-43 stage, mixed pathologies, and clinical Alzheimer’s-type dementia. Brain 2016; 139:2983–2993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pillai JA, Butler RS, Bonner-Jackson A, et al. : Impact of Alzheimer’s disease, Lewy body and vascular co-pathologies on clinical transition to dementia in a national autopsy cohort. Dement Geriatr Cogn Disord 2016; 42:106–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clementz BA, Sweeney JA, Hamm JP, et al. : Identification of distinct psychosis biotypes using brain-based biomarkers. Am J Psychiatry 2016; 173:373–384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gong Q, Scarpazza C, Dai J, et al. : A transdiagnostic neuroanatomical signature of psychiatric illness. Neuropsychopharmacology 2019; 44:869–875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Creese B, Vassos E, Bergh S, et al. : Examining the association between genetic liability for schizophrenia and psychotic symptoms in Alzheimer’s disease. Transl Psychiatry 2019; 9:273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Darby RR, Laganiere S, Pascual-Leone A, et al. : Finding the imposter: brain connectivity of lesions causing delusional misidentifications. Brain 2017; 140:497–507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ballard CG, O’Brien JT, Swann AG, et al. : The natural history of psychosis and depression in dementia with Lewy bodies and Alzheimer’s disease: persistence and new cases over 1 year of follow-up. J Clin Psychiatry 2001; 62:46–49 [DOI] [PubMed] [Google Scholar]
- 30.Cohen-Mansfield J,Golander H: The measurement of psychosis in dementia: a comparison of assessment tools. Alzheimer Dis Assoc Disord 2011; 25:101–108 [DOI] [PubMed] [Google Scholar]
- 31.Gerritsen DL, Smalbrugge M, Veldwijk-Rouwenhorst AE, et al. : The difficulty with studying challenging behavior. J Am Med Dir Assoc 2019; [DOI] [PubMed] [Google Scholar]
- 32.Rabinowitz J, Katz I, De Deyn PP, et al. : Treating behavioral and psychological symptoms in patients with psychosis of Alzheimer’s disease using risperidone. Int Psychogeriatr 2007; 19:227–240 [DOI] [PubMed] [Google Scholar]


