Abstract
Purpose
Most prostate cancer patients receiving enzalutamide or abiraterone develop resistance. Clinical evidence indicates that serum levels of dehydroepiandrosterone sulfate (DHEAS) and biologically active dehydroepiandrosterone (DHEA) remain in the high range despite anti-androgen treatment. The conversion of DHEAS into DHEA by steroid sulfatase (STS) may contribute to sustained intracrine androgen synthesis. Here, we determine the contribution of STS to treatment resistance and explore the potential of targeting STS to overcome resistance in prostate cancer.
Experimental Design
STS expression was examined in patients and cell lines. In vitro, STS activity and expression were modulated using STS specific siRNA or novel STS inhibitors (STSi). Cell growth, colony formation, androgen production, and gene expression were examined. RNAseq analysis was conducted on VCaP cells treated with STSi. Mice were treated with STSi with or without enzalutamide to determine their effects in vivo.
Results
STS is overexpressed in castration resistant prostate cancer (CRPC) patients and resistant cells. STS overexpression increases intracrine androgen synthesis, cell proliferation, and confers resistance to enzalutamide and abiraterone. Inhibition of STS using siRNA suppresses prostate cancer cell growth. Targeting STS activity using STSi inhibits STS activity, suppresses AR transcriptional activity, and reduces the growth of resistant C4–2B and VCaP prostate cancer cells. STSi significantly suppress resistant VCaP tumor growth, decrease serum PSA levels and enhance enzalutamide treatment in vitro and in vivo.
Conclusions
These studies suggest that STS drives intracrine androgen synthesis and prostate cancer proliferation. Targeting STS represents a therapeutic strategy to treat CRPC and improve second generation anti-androgen therapy.
Keywords: Prostate cancer, steroid sulfatase, resistance, intracrine androgen synthesis, adrenal androgens
Introduction
Targeting androgen signaling with androgen deprivation therapy (ADT) has been the mainstay of clinical interventions in PCa. While initially effective, most men experience only transient benefit from these interventions before developing CRPC, which is currently incurable. The second-generation anti-androgen drugs enzalutamide (Enza), abiraterone (Abi), and most recently apalutamide (Apal) and darolutamide (Daro), are approved for the treatment of CRPC (1–4). Even though these treatments are initially effective, resistance frequently occurs. This is the most common cause of treatment failure. Better understanding of the mechanisms that confer resistance is urgently needed in order to design more effective treatments to overcome resistance and improve therapies.
While AR mutations, amplifications, and overexpression of its variants, such as AR-V7, have been suggested to play important roles in promoting CRPC progression and induction of resistance to Enza and Abi therapy, the mechanisms associated with resistance to these treatments are still largely unknown. Intratumoral androgen biosynthesis is well characterized as a mechanism of CRPC (5–8). Many enzymes are involved in androgen synthesis, including steroid sulfatase (STS) (9,10). STS converts the abundantly circulated adrenal dehydroepiandrosterone sulfate (DHEAS) to biologically active dehydroepiandrosterone (DHEA) and its expression in CRPC could be contributing to increased androgen levels (11). DHEAS is present at plasma concentrations up to 500 times higher than testosterone and can potentially be transported into PCa cells via organic anion transporters (12–14). Once into the cells, DHEAS can be desulphated via endogenous STS into DHEA. DHEA can then be used as a precursor for the production of testosterone (T) through the activity of hydroxysteroid dehydrogenases and further into dihydrotestosterone (DHT) via 5α reductase, as previously discussed at Europeon Association of Urology Annual Congress EAU20 (15).
STS is present in most PCa specimens and its expression is increased in CRPC (11,16–18). Furthermore, DHEA is a major source of tumor androgens for prostate cancer and DHEAS is the most abundant adrenal steroid in male circulation. Therefore, conversion of circulated adrenal DHEAS to DHEA by STS is believed to be an alternative source of intracrine androgen which cannot be fully inhibited by Abi. While the nonspecific CYP17A1 inhibitor, ketoconazole, or the specific CYP17A1 inhibitor, Abi, greatly reduce circulating levels of DHEAS by up to 95%, significant circulating DHEAS concentrations are still present (~20 μg/dL, which is about 2000 times higher than castrate levels of testosterone) (14). This suggests that DHEAS could act as a depot for further downstream androgen formation via desulphatation. These clinical data highlight the importance for exploring STS inhibition to prevent DHEAS conversion to DHEA.
While the focus of prostate cancer treatment is often on reducing androgen signaling, the importance of adrenal androgens produced from DHEA is overlooked. DHEA is a major source of tumor androgens for prostate cancer and DHEAS is the most abundant steroid in male circulation. In fact, DHEAS is present 400- to 1000-fold higher than DHEA (DHEAS/DHEA: 2–10 μmol/L/10–25 nmol/L) (12–14).. Numerous STS inhibitors have been tested for potential activity both in animal and clinical studies in breast cancer (19–26). However, while STS has been widely investigated in breast cancer, there are limited studies in PCa.
In this study we demonstrated that STS is overexpressed in CRPC patients and cells. We found that STS controls CRPC cell growth through regulation of AR signaling and knockdown of STS suppresses cell growth and AR transcriptional activity in CRPC cells. Furthermore, we characterized two novel STS small molecule inhibitors that demonstrated efficacy in inhibition of prostate cancer cell proliferation, AR transcriptional activity and castration-resistant tumor growth. Additionally, we found that overexpression of STS conferred resistance to enzalutamide in C4–2B cells and combination of STSi with the leading anti-androgen enzalutamide had increased efficacy for inhibiting cell growth over either drug on its own in vitro and in vivo.
Materials and Methods
Reagents and Cell Culture
LNCaP and VCaP cells were obtained from the American Type Culture Collection (ATCC, Manassas, VA). All experiments with cell lines were performed within 6 months of receipt from ATCC or resuscitation from cryopreservation. C4–2B cells were kindly provided and authenticated by Dr. Leland Chung, Cedars-Sinai Medical Center, Los Angeles, CA. VCaP cells were maintained in DMEM supplemented with 10% fetal bovine serum (FBS), 100 units/ml penicillin and 0.1 mg/ml streptomycin. PZ-HPV7 cells were maintained in keratinocyte serum-free medium (K-SFM) with required supplements (Invitrogen). Other cell lines were maintained in RPMI 1640 supplemented with 10% FBS, 100 units/ml penicillin and 0.1 mg/ml streptomycin. All cells were maintained at 37°C in a humidified incubator with 5% carbon dioxide. All drugs were dissolved in DMSO and stored at −20°C.
Cell transfection and luciferase assay
STS siRNA (HSS100722) was purchased from Invitrogen. For luciferase assays, VCaP cells (1×105 cells per well of 12-well plate) were transfected with 0.5 μg of pGL3-PSA6.0-Luc reporter plasmid with or without 20 pmol STS siRNA. The luciferase activity was determined 72 hr after transfection using a dual-luciferase reporter assay system (Promega) as described previously (27).
For ovexpression of STS, STS expressing plasmids were obtained from GenScript (Piscataway, NJ) and transfected into C4–2B or LNCaP cells alongside vector control using Lipofectamine as previously described. STS overexpression was confirmed via western blot as described below.
Intracellular Steroid Analysis
C4–2B STS, C4–2B Neo, LNCaP STS and LNCaP Neo cells supplemented with 100 nM DHEAS in charcoal stripped FBS media were collected and whole cell pellets (10 × 106 cells/pellet) were flash frozen in liquid nitrogen. Mass Spectrometry for steroid metabolites was performed on the Thermo Fisher Vanquish / SciEx QTrap 6500 spectrometer.
Western blot analysis
Cellular protein extracts were resolved on SDS-PAGE and proteins were transferred to nitrocellulose membranes. After blocking for 1 hour at room temperature in 5% milk in PBS/0.1% Tween-20, membranes were incubated overnight at 4°C with the indicated primary antibodies: STS (Catalog number: 17870–1-AP, Proteintech); Tubulin (T5168, Sigma-Aldrich, St. Louis, MO). Tubulin was used as loading control. Following secondary antibody incubation, immunoreactive proteins were visualized with an enhanced chemiluminescence detection system (Millipore, Billerica, MA).
Sulfatase activity assays
VCaP cells were seeded on 12-well plates at a density of 2×105 cells/well in media containing 10% FBS and treated with various concentrations of SI’s for 24 hours. Cell lysates were harvested and subjected to STS activity assay by mixing with 0.5 mM of 4-Methylumbelliferyl sulfate in a 96-well plate. While 4-Methylumbelliferyl sulfate is also a substrate for arylsulfatases A and B, these enzymes are inactive at pH 7.5 wherein STS has optimal activity which makes this assay specific to STS under normal cell culture conditions (28). The plate was read in a fluorescence microtiter plate reader at excitation and emission wavelengths of 355 and 460 nm, respectively.
PZ-HPV7, LNCaP, C4–2B, VCaP, C4–2B Neo, C4–2B STS, LNCaP Neo, or LNCaP STS cells were seeded at a density of 1×105 cells/well or 2×105 cells/well (VCaP cells only) in 6-well plates and STS activity in was determined using the Sulfatase Activity Assay Kit (BioVision, Milpitas, CA) according to the manufacturer’s instructions. Sulfatase activity was normalized to total protein. A drawback of this method over the 4-Methylumbelliferyl sulfate assay is that it is not as specific to STS. However, due to the fact that endogenous expression levels of STS correlate to increased overall sulfatase activity when comparing the PZ-HPV7, LNCaP, C4–2B, and VCaP cells, and that the only difference between the C4–2B Neo and C4–2B STS or LNCaP Neo and LNCaP STS cells is STS overexpression, we are confident that this assay is reflective of STS activity in these cells.
Cell growth assay
C4–2B and VCaP cells were seeded on 12-well plates at a density of 0.5×105 cells/well and 1×105 respectively in media containing 10% FBS and transiently transfected with STS siRNA or control siRNA. Total cell numbers were counted after 3 and 5 days. C4–2B and VCaP cells were treated with different concentrations of STS inhibitors and total cell numbers were counted on day 3 and 5. VCaP cells were seeded on 12-well plates at a density of 1×105 cells/well in DMEM media containing 10% FBS and treated with DMSO, 20 μM enzalutamide, STS inhibitors or their combination for 3 days. Total cell numbers were counted and the cell survival rate (%) was calculated. Cell survival rate (%) = (Treatment group cell number / Control group cell number) ×100.
C4–2B cells were plated on 12-well plates at a density of 0.5×105 cells/well and transiently transfected with STS overexpressing plasmids or vector control. The following day, cells were treated with 20 μM Enza, 10 μM Abi, or DMSO for 3 days. Cell number was determined using Cell Counting Kit 8 (Dojindo Laboratories, Rockville, MD) per the manufacturer’s instructions.
Stably transfected C4–2B Neo, C4–2B STS, LNCaP Neo, and LNCaP STS cells were plated on 12-well plates at a density of 0.5×105 cells/well and treated with 20 μM enzalutamide or DMSO for 3 days. Cell number was determined using Cell Counting Kit 8 per the manufacturer’s instructions.
Clonogenic Assay
C4–2B or VCaP cells were treated with DMSO or different concentrations of STS inhibitors in media containing 10% FBS. Cells were plated at equal density (2000 cells/dish for C4–2B and 20000 cells for VCaP) in 100 mm dishes for 2–4 weeks. Colonies were rinsed with PBS before staining with 0.5% crystal violet/4% formaldehyde for 30 min and the number of colonies was counted.
Real-Time quantitative RT-PCR
Total RNAs were extracted using TriZOL reagent (Invitrogen). cDNAs were prepared after digestion with RNase-free RQ1 DNase (Promega). The cDNAs were subjected to real-time reverse transcription-PCR (RT-PCR) using Sso Fast Eva Green Supermix (Bio-Rad) according to the manufacturer’s instructions and as described previously (29). Each reaction was normalized by co-amplification of actin. Samples were run in triplicate on default settings of a Bio-Rad CFX-96 real-time cycler. Primers used for Real-time PCR are: KLK3, 5’-ccctgcccgaaagg-3′(forward) and 5’-gatccacttccggtaatgca-3′ (reverse); NKX3.1, 5’-ccgagacgctggcagagacc-3′(forward) and 5′-gcttaggggtttggggaag-3′(reverse); FKBP5, 5’-gggaagatagtgtcctggttag-3’ (forward) and 5’-gcagtcttgcagccttattc-3’ (reverse) and Actin, 5′-agaactggcccttcttggagg-3′(forward) and 5′-gtttttatgttcctctatggg-3′ (reverse).
Measurement of Testosterone
For determination of intratumoral testosterone, sections of tumors from the VCaP model mice were homogenized in a buffer consisting of 20 mM EDTA, 20 mM Tris, and 20 mM NaCL for 30 seconds. The homogenized tumor was extracted 2X using ethyl acetate and dessicated using a vacuum centrifuge. The resulting dessicate was reconstituted in 300 μL of calibrator diluent provided in the assay. From there, testosterone was measured using the Parameter Testosterone Assay (R&D Systems, Inc. Minneapolis, MN) according to the manufacturer’s directions using 100 μL of reconstituted tumor extract per well.
Measurement of PSA
Blood was collected from the VCaP tumor model mice and the serum was isolated. The PSA level was measured using a PSA ELISA Kit (KA0208, Abnova, Inc., Walnut, CA) according to the manufacturer’s instructions as described previously (30).
In vivo tumorigenesis assays
VCaP cells (4×106) were mixed with matrigel (1:1) and injected subcutaneously into the flanks of 6–7 week old male SCID mice. After PSA levels were detectable (5–10 ng/mL), mice were castrated and the tumor volume was monitored, once the tumors grew back to 50–100 mm3, tumor-bearing mice were randomized into three groups (5 mice in each group) for the first animal study: : (1) vehicle control (5% Tween 80 and 5% ethanol in PBS, i.p.), (2) SI-1 (25 mg/kg, i.p.), (3) SI-2 (25 mg/kg, i.p.). Tumors were measured using calipers twice a week and tumor volumes were calculated using length × width2/2. Tumor tissues were harvested after 3 weeks of treatment.
For the second animal experiment, VCaP cells (4×106) were mixed with matrigel (1:1) and injected subcutaneously into the flanks of 6–7 week old male SCID mice. After PSA levels were detectable (5–10 ng/mL), mice were castrated and the tumor volume was monitored, once the tumors grew back to 50–100 mm3, tumor-bearing mice were randomized into four groups (5 mice in each group) and treated as follows: (1) vehicle control (5% Tween 80 and 5% ethanol in PBS, i.p.), (2) Enzalutamide (20 mg/Kg p.o.), (3) SI-1 (25 mg/kg, i.p.), (4) Enzalutamide (20 mg/Kg p.o.) + SI-1 (25 mg/kg, i.p.). Tumors were measured using calipers twice a week and tumor volumes were calculated using length × width2/2. Tumor tissues were harvested after 3 weeks of treatment.
Immunohistochemistry
Tumors were fixed by formalin. Paraffin embedded tissue blocks were dewaxed, rehydrated, and blocked for endogenous peroxidase activity. Antigen retrieval was performed in sodium citrate buffer (0.01 mol/L, pH 6.0) in a microwave oven at 1,000 W for 3 min and then at 100 W for 20 min. Nonspecific antibody binding was blocked by incubating with 10% fetal bovine serum in PBS for 30 min at room temperature. Slides were then incubated with anti-Ki-67 (at 1:500; NeoMarker) at 4°C overnight. Slides were then washed and incubated with biotin-conjugated secondary antibodies for 30 min, followed by incubation with avidin DH-biotinylated horseradish peroxidase complex for 30 min (Vectastain ABC Elite Kit, Vector Laboratories). The sections were developed with the diaminobenzidine substrate kit (Vector Laboratories) and counterstained with hematoxylin. Nuclear staining of cells was scored and counted in 5 different vision fields. Images were taken on an Olympus BX51 microscope equipped with a DP72 camera.
Statistical Analysis
Data are presented as means ± standard deviation of the mean (SD). Statistical analyses were performed with Microsoft Excel analysis tools or JMP. Differences between individual groups were analyzed by one-way analysis of variance (ANOVA) followed by the Scheffé procedure for comparison of means. P < 0.05 was considered statistically significant.
Results
STS regulates intracrine androgen synthesis and controls cell growth
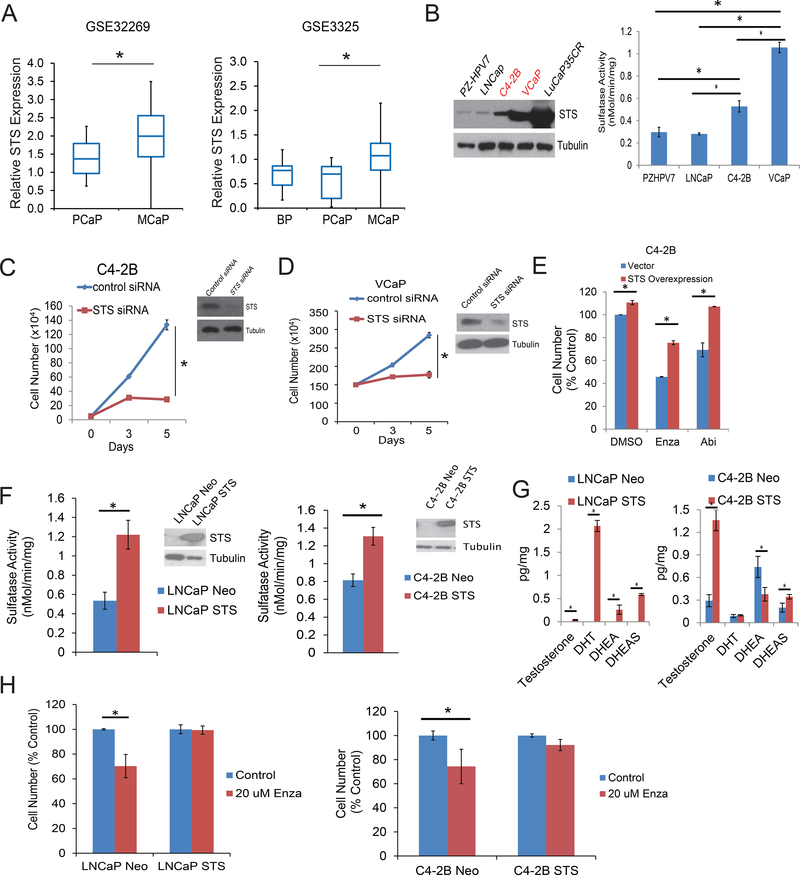
Adrenal-derived steroids such as DHEAS act as precursors for the production of more potent androgens in peripheral tissues including prostate. DHEA synthesized from cholesterol can be sulfonated by DHEA sulfotransferase into DHEAS. The conversion of DHEAS back to biologically active DHEA is mediated by STS. To determine the role of STS in prostate cancer, we first interrogated two independent GEO data bases and examined STS expression in primary prostate cancer (PCa) and mCRPC patients. As shown in Fig. 1A, STS expression is significantly elevated in mCRPC compared with primary prostate cancer tissues in two independent data bases. We next determined the expression levels of STS in benign prostate epithelial cells and cancer cells. As shown in Fig. 1B, STS expression is relatively low in PZ-HPV7 benign epithelial cells, and moderate in LNCaP and C4–2B cells. The level of STS is substantially up-regulated in VCaP cells and LuCaP 35CR tumors. STS expression correlated to increased overall sulfatase activity (Fig. 1B) as well as STS activity (Supplemental Fig.1A). We next determined if STS affects cell proliferation in CRPC cells, as shown in Fig. 1C left, knockdown of STS significantly inhibited C4–2B cell growth in a time dependent manner. These results were also confirmed in VCaP cells where knockdown of STS also significantly reduced cell number (Fig. 1D). Furthermore, transient overexpression of STS in C4–2B cells promotes resistance to treatment with Enza and Abi (Fig. 1E).
Figure 1.
STS is highly expressed in CRPC tumors and regulates the AR pathway. A. STS gene expression analysis using the GEO database in two datasets comparing benign, primary or metastatic prostate cancer. GSE32269: primary prostate cancer, n = 22; and metastatic prostate cancer, n = 29. GSE3325: Benign, n = 4; primary prostate cancer, n = 5; and metastatic prostate cancer, n = 4; Data were extracted and analyzed by Subio platform. B. PZHPV7, LNCaP, C4–2B, VCaP, LuCaP 35CR xenograft tumors were harvested and whole cell lysates were subjected to Western blotting. Sulfatase activity was assessed. C. C4–2B cells were transiently transfected with control siRNA or STS siRNA and the cell numbers were determined on different days. Whole cell lysates were collected at 3 days and subjected to Western blotting. D. VCaP cells were transiently transfected with control siRNA or STS siRNA and cell numbers were determined on different days. Whole cell lysates were collected on day 3 day and subjected to Western blotting. E. C4–2B cells were transiently transfected with STS containing plasmids or vector control and then treated with DMSO, 20μM Enza, or 10 μM Abi for 3 days. Cell number was determined on day 3 day. F. STS activity was assessed using a STS Activity Kit in C4–2B and LNCaP cells stably overexpressing STS. Inset: Western blot of STS expression. G. Testosterone, DHT, DHEA, and DHEAS levels in C4–2B and LNCaP cells stably overexpressing STS treated with 100 nM DHEAS. H. C4–2B and LNCaP cells stably overexpressing STS were treated with DMSO or 20 μM Enza for 3 days and cell number was assessed. * p<0.05
In LNCaP and C4–2B cells stably overexpressing STS, we found that overexpression of STS resulted in increased sulfatase activity (Fig. 1F) and STS activity (Supplemental Fig.1B). Intracellular levels of androgens where increased in the STS overexpressing cells when the cells were supplemented with DHEAS (Fig 1.G). Unexpectedly, DHEA-S was increased in the C4–2B STS overespressing cells compared to the C4–2B Neo cells. This observation is currenty under further investigation and one possible explanation could be incomplete rinsing of these samples prior to Mass-spec analysis to cleanse them of the supplemental DHEA-S in the media. In addition, we found that the stable STS overexpressing clones have a marked resistance to treatment with enzalutamide compared to vector expressing controls (Fig. 1H). Collectively, these results suggest that STS is overexpressed in CRPC and overexpression of STS increases intracrine androgens and regulates cell growth.
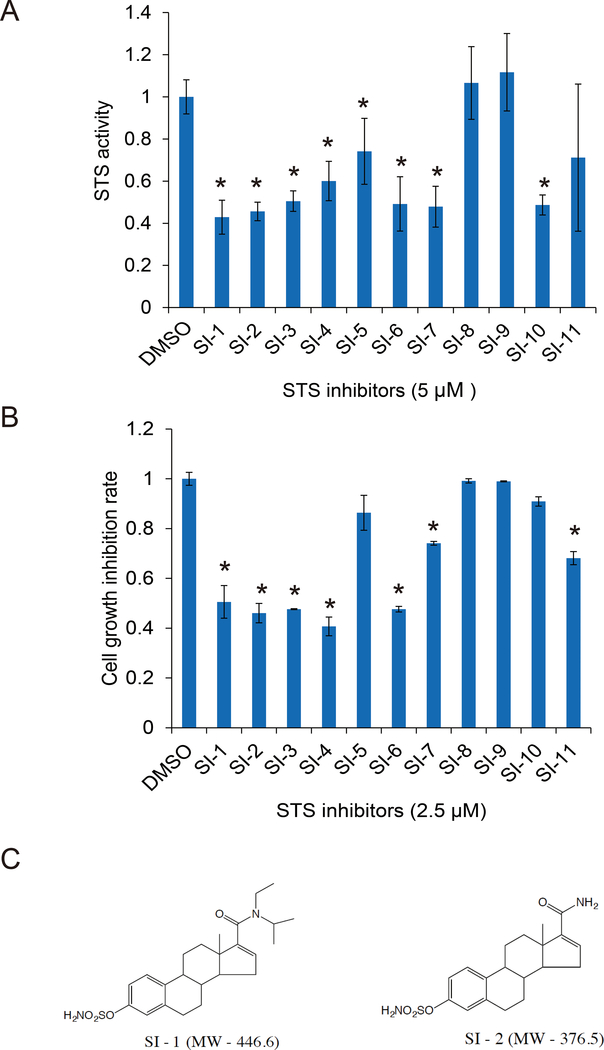
Potent STS inhibitors suppress STS activity and inhibit prostate cancer cell growth
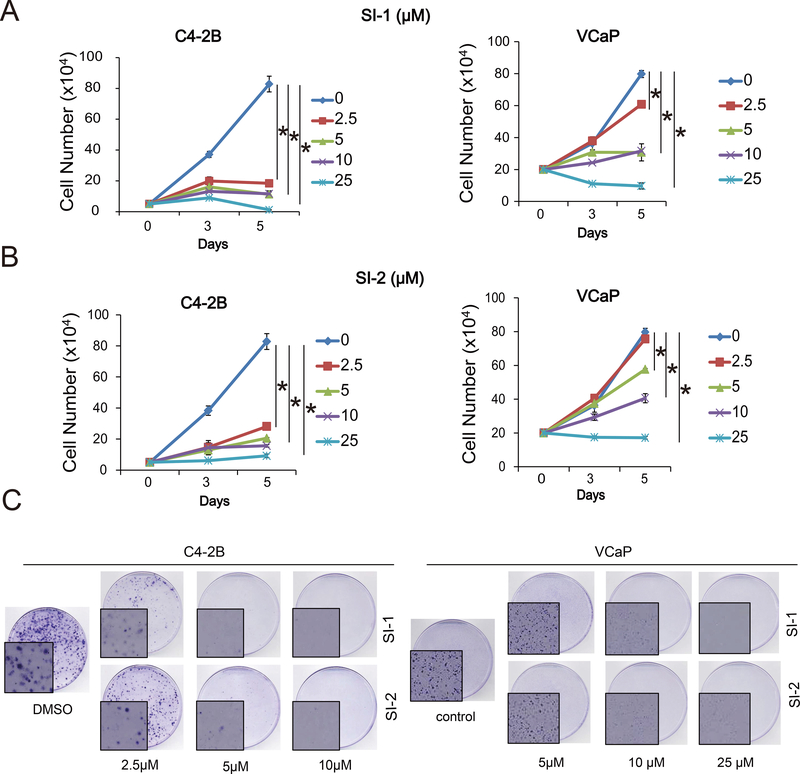
Having demonstrated that inhibition of STS expression using specific siRNA suppressed prostate cancer cell growth, we next designed and synthesized eleven small molecular STS inhibitors (SI-1 to SI-11) with molecular weights ranging from 300 to 460 kDa. These STS inhibitors were assessed for their efficacy on preventing sulfatase activity. As shown in Fig. 2A, eight novel inhibitors were able to inhibit STS activity. Among them, SI-1, SI-2, SI-3, SI-6, SI-7 and SI-10 inhibited STS activity by 50%−60%, SI-4 and SI-5 suppressed 30%−40% STS activity. We also determined if these inhibitors suppressed prostate cancer cell growth. As shown in Fig. 1B, SI-1, SI-2, SI-3, SI-4, SI-6, SI-7 and SI-11 impeded VCaP cell growth. In general, the extent of cell growth inhibition by these inhibitors is correlated with their ability to decrease STS activity (Fig 2A and 2B). We then selected SI-1 and SI-2, which had slightly improved overall ability to both inhibit STS activity and reduce cell number, to further characterize in subsequent studies (Fig. 2C). As shown in Fig. 3A–B, both SI-1 and SI-2 significantly suppressed cell growth in a time-dependent manner. These results were further confirmed by clonogenic assays; both STS inhibitors significantly suppressed colony formation in a dose-dependent manner in C4–2B and VCaP cells (Fig. 3C). Collectively, these results suggest that inhibition of STS activity using selective STS inhibitors suppresses cell growth.
Figure 2.
STS inhibitor design and selection. A. VCaP cells were treated with 5 μM STS inhibitors overnight and STS activity was determined by STS fluorometric assay. B. C4–2B cells were treated with 2.5 μM of STS inhibitors for 3 days. Total cell numbers were determined. C. SI-1 and SI-2 chemical structures and molecular weight. * p<0.05.
Figure 3.
SI-1 and SI-2 suppress prostate cancer cell proliferation. A. C4–2B or VCaP cells were treated with different concentrations of SI-1 and cell numbers were determined on different days. B. C4–2B or VCaP cells were treated with different concentrations of SI-2, cell numbers were determined on different days. C. C4–2B or VCaP cells were treated with different concentrations of SI-1 or SI-2 and clonogenic assays were performed. Pictures of colonies were taken on a microscope. * p<0.05.
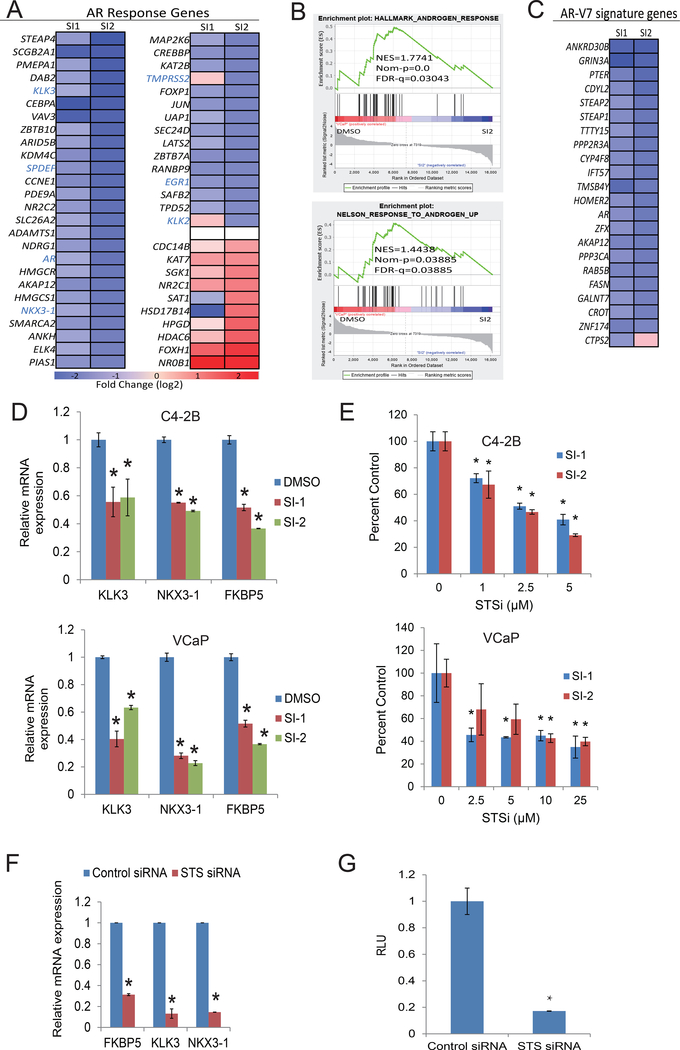
Inhibition of STS regulates AR-target gene expression
Knowing that STS overexpression results in increased androgen levels, we next wanted to determine the effects of STS on AR signaling. We analyzed RNA-seq transcriptomes of VCaP cells treated with STS inhibitors to identify gene programs affected by STS inhibition (GEO accession number: GSE153245). Genes that are characterized as AR targets or androgen-induced genes were significantly inhibited by both inhibitors (Fig. 4A). Conversely, androgen-repressed genes were strongly induced by the inhibitors (Fig. 4A). Further examination by gene set enrichment analysis (GSEA) using the AR activity signature revealed a highly robust disruption of AR gene programs by STS inhibition (Fig. 4B). Significantly, the STS inhibitors also strongly inhibited the expression of genes preferentially up-regulated by AR-V7 (Fig. 4C). qRT-PCR verified that well-characterized AR targets including FKBP5, KLK3, and NKX3–1 were strongly inhibited by STS inhibitors in C4–2B and VCaP cells (Fig. 4D). The effects of STS inhibitors on AR signaling in C4–2B and VCaP cells was further analyzed by assessing PSA-luciferase activity in C4–2B and VCaP cells treated with SI-1 and SI-2. PSA luciferase activity was significantly inhibited in a dose-dependent manner in both cell lines (Fig. 4E). Similarly, knockdown STS expression using STS specific siRNA suppressed the expression of AR target genes and inhibited PSA-luciferase activity and (Fig 4F & 4G). These results suggest that the selected STS inhibitors can down regulate AR signaling in CRPC cells.
Figure 4.
STS regulates AR signaling. VCaP cells were treated with SI-1 or SI-2. RNA was collected and sent for RNAseq. A. Heatmap depicting alterations in AR responsive genes. B. GSEA analysis of AR pathway. C. Heatmap depicting the effects of SI-1 or SI-2 on genes kown to be upregulated by ARv7. D. C4–2B or VCaP cells were treated with SI-1 or SI-2 for 3 days, total RNA was extracted and KLK3, NKX3–1 or FKBP5 mRNA levels were analyzed by qRT-PCR. E. C4–2B or VCaP cells were transiently transfected with PSA luciferase plasmid and then treated with different concentrations of SI-1 or SI-2 overnight. PSA luciferase activity was determined. F. VCaP cells were transiently transfected with STS siRNA, total RNA was extracted and KLK3, NKX3–1 and FKBP5 mRNA levels were analyzed by qRT-PCR.G. VCaP cells were transiently transfected with STS siRNA. PSA luciferase activity was determined. * p<0.05.
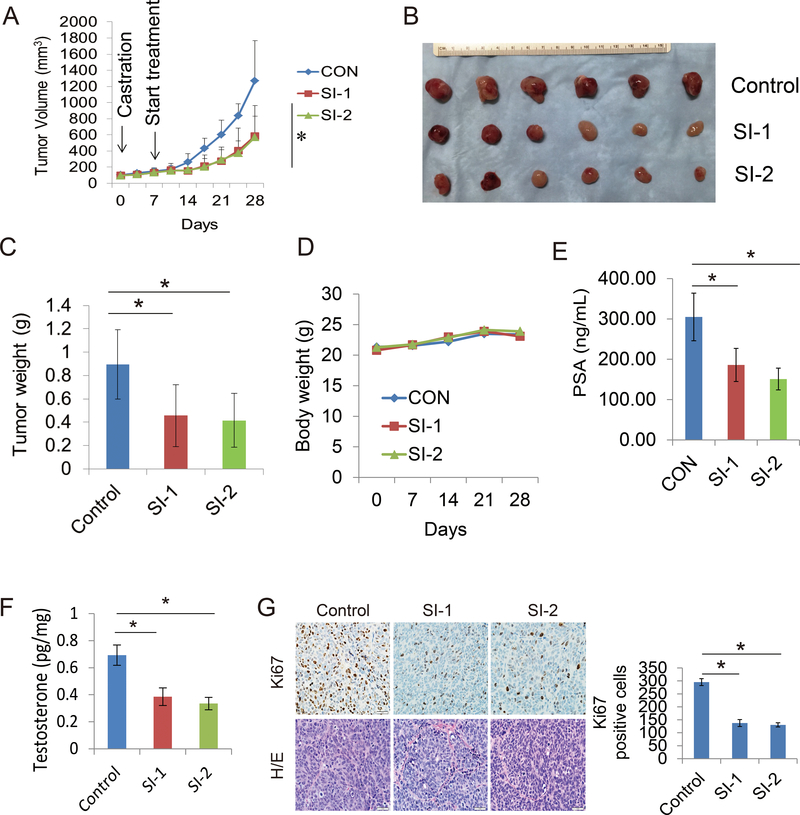
SI-1 and SI-2 inhibit growth of the relapsed VCaP tumors
We next examined the effects of STS inhibition on tumor growth in vivo. The VCaP tumor model was selected because it expresses higher levels of endogenous STS. VCaP tumors were allowed to develop in intact SCID mice and the animals were castrated after PSA levels reached around 5–10 ng/mL. One to two weeks later, when the tumors grew back to 80–100 mm3 (indicating relapse), mice were treated with SI-1 or SI-2 (25 mg/kg, i.p.) for 3 weeks. Both SI-1 and SI-2 significantly inhibited tumor growth compared to the untreated controls (p=0.00155 and p=0.00061 respectively) (Fig. 5A–5C). Mouse body weights were not affected by either treatment compared with the control group (Fig. 5D). Serum PSA level was significantly decreased after 3 weeks of drug treatment. As shown in Fig. 5E, the control group expressed 300 ng/mL PSA at 3 weeks of treatment time point, SI-1 decreased PSA by about 50% (p<0.01) and SI-2 by about 55% (p<0.01). Furthermore, intratumoral testosterone levels were also decreased by SI-1 and SI-2 treatment (Fig. 5F). Tumor proliferation was appraised by IHC. As shown in Fig. 5G, both SI-1 and SI-2 treatments had less Ki67 staining in tumors. Taken together, these results further demonstrate that inhibition of STS by SI-1 or SI-2 has great anti-tumor efficacy in vivo.
Figure 5.
SI-1 and SI-2 suppress replased VCaP tumor growth. A-D. Mice bearing VCaP xenografts were castrated and replased tumors were treated with vehicle control, SI-1 (25 mg/Kg i.p) or SI-2 (25mg/Kg i.p) for 3 weeks. Tumor volumes were measured twice weekly and the tumors were collected and weighed after 3 weeks of treatment. Mouse body weights were monitored twice weekly. E. Mouse blood was collected after 3 weeeks of treatment and the serum was extracted. PSA level of each group was determined by PSA ELISA kit. F. Intratumoral testosterone was assessed by ELISA on extracts from tumors. G. IHC staining of Ki67 and H/E staining in each group was performed and quantified as described in methods. * p<0.05.
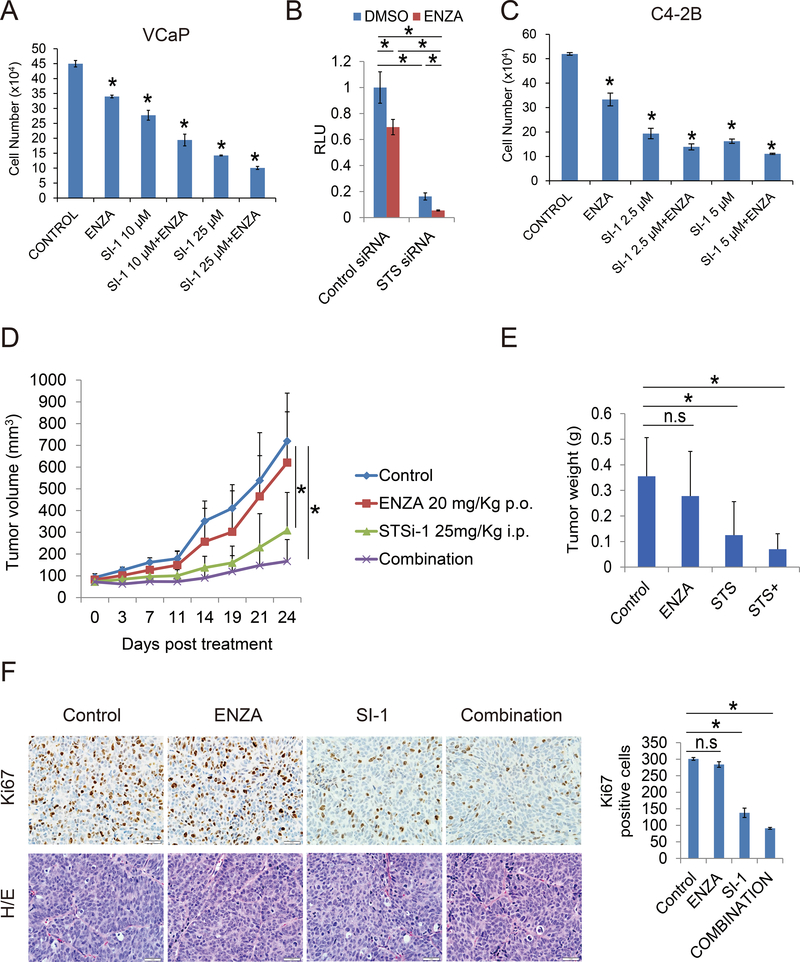
STS activity is involved in enzalutamide response in vitro and in vivo
Previous studies demonstrate that uncontrolled intraprostatic androgen synthesis likely plays an important role in enzalutamide and abiraterone resistance (29,31). To test if inhibition of STS improved enzalutamide treatment, SI-1 and SI-2 were used in combination with enzalutamide in VCaP cells. As shown in Fig. 6A, enzalutamide reduced VCaP cell growth in vitro, however SI-1 and SI-2 were more effective. Combination of SI-1 or SI-2 with enzalutamide further reduced VCaP cell growth in vitro. Additionally, siRNA specific to STS alone or in combination with enzalutamide significantly diminished AR transcriptional activity (Fig. 6B). We also confirmed the growth inhibition ability of the combination treatment in C4–2B cells (Fig. 6C).
Figure 6.
STS inhibitors improve enzalutamide treatment in vitro and in vivo. A. VCaP cells were treated with 10 μM or 25 μM SI-1 or SI-2 with or without 20 μM enzalutamide for 3 days, cell number was determined. B. VCaP cells were transiently transfected with control siRNA or STS siRNA with PSA luciferase plasmid for 3 days and thentreated with 10 μM enzalutamide for 24 hours. Luciferase activity was determined. C. C4–2B cells were treated with 2.5 μM or 5 μM SI-1 or SI-2 with or without 20 μM enzalutamide for 3 days and cell number was determined. D-E. Mice bearing VCaP xenografts were castrated and the replase tumors were treated with vehicle control, enzalutamide (25 mg/Kg p.o), SI-1 (25 mg/Kg i.p), or their combination for 3 weeks, tumor volumes were measured twice weekly and the tumors were collected and weighed after 3 weeks treatment. F. IHC staining of Ki67 and H/E staining in each group was performed and quantified as described in methods. * p<0.05.
To test the efficacy of the combination of SI inhibitors with enzalutamide in vivo, we next used the relapsed VCaP tumor model. As shown in Fig. 6D–E, enzalutamide treatment alone only marginally inhibited tumor growth and produced a tumor growth curve very similar to the vehicle control group. SI-1 treatment alone significantly suppressed tumor growth and combination of SI-1 with enzalutamide further suppressed tumor growth more than either compound alone. IHC staining confirmed that enzalutamide did not affect Ki67 expression in the relapsed VCaP tumors. SI-1 significantly decreased Ki67 expression while combination treatment further lowered Ki67 expression (Fig. 6F). These data demonstrate that inhibition of STS activity by SI-1 improved enzalutamide treatment in vivo, providing preclinical data to support further clinical development of combination therapy of STS inhibitors and enzalutamide to treat advanced prostate cancer.
Discussion
Steroid sulfatase (STS) catalyzes the conversion of dehydroepiandrosterone sulfate (DHEAS) into biologically active dehydroepiandrosterone (DHEA). Emerging clinical evidence shows that serum levels of steroids, particularly DHEAS and DHEA, remain in the high range and may serve as an ample pool of precusors for androgen synthesis, even when CYP17A1 mediated testosterone biosynthesis is inhibited with abiraterone in CRPC cells. STS is present in 85% of prostate cancer specimens (12) with increased expression in CRPC (12). Conversion of the abundantly circulated adrenal androgen DHEAS into DHEA by STS is believed to be an alternative source of androgens which can not be inhibited by Abi. In this study, we found that STS is overexpressed in CRPC patients and in resistant cells. Overexpression of STS stimulates incracrine androgen synthesis, increases cell growth and confers resistance to enzalutamide. Targeting STS activity using selected small molecule inhibitors of STS (STSi) inhibits STS activity, suppresses AR transcriptional activity, and reduces the growth of resistant C4–2B and VCaP prostate cancer cells in vitro and in vivo. Furthermore, STSi enhance enzalutamide treatment in vitro and in vivo.
Numerous STS inhibitors have been tested for potential activity both in animal and clinical settings in breast cancer (20,22,32). TZS-8478 has potent steroid sulfatase-inhibitory activity and exhibits no estrogenicity in vitro or in vivo (20). It can completely inhibit STS activity in tumor, uterus and liver, and also lowers the concentrations of estrone and estradiol in plasma (20). STX64 and STX 213 are new generation STS inhibitors that can suppress hormone-dependent human breast cancer growth (21,22). Noticeably, a phase II trial using the STS inhibitor Irosustat (STX-64) in combination with aromatase inhibitor for ER-positive breast cancer patients (IRIS Study) has been launched (26). Addition of Irosustat to aromatase inhibitor further suppressed estradiol levels in advanced breast cancer patients. KW-2581 can irreversibly inhibit STS activity in breast cancer cells and cause tumor shrinkage in a mouse xenograft model (33,34). Additionally, SR 16157 is a dual STS and ER alpha modulators inhibitor. It not only suppresses STS activity but also inhibits ER alpha binding affinity and has anti-estrogenic effects in breast cancer (35). Although STS inhibitors have been widely investigated in breast cancer, there are limited reports in prostate cancer. In the present study, we report that STS is more abundant in CRPC cell lines, such as C4–2B and VCaP cells, compared to benign prostate cells. We also identified several potent inhibitors of STS, and demonstrsted that inhibition of STS activity using the selected novel inhibitors suppresses androgen signaling, reduces cell growth in vitro and tumor growth in vivo, suggesting STS could be a valuble therapeutic target for CRPC treatment.
As expected, the androgen signaling pathway is one of the main targets for STS inhibition in our study. Both siRNA knockdown of STS and pharmacological inhibition of STS activity decrease AR transcriptional activity. Inhibition of STS expression and activity reduces AR transactivation indicated by both the luciferase assay and RT-PCR detection of downstream molecules such as FKBP5, KLK3 and NKX3–1. Adrenal androgens in circulation, such as DHEA, contribute to CRPC tumor growth by promoting androgen synthesis. Data from our study demonstrate that overexpression of STS in both LNCaP cells and C4–2B cells results in a significant increase in intracellular testosterone. This is likely the result of upregulated STS activity producing increased amounts of DHEA from DHEAS which is then further converted to testosterone by other enzymes. A retrospective cohort study showed that rise of serum levels of androsterone, DHEA, estrone, and estradiol correlated with shorter time to development of CRPC in men receiving ADT (36). Both DHEA and estrone are the products of STS activity and therefore inhibition of STS activity could reduce the levels of active DHEA and thus suppress growth and tumor progression. Additionally, STS has been implicated in epithelial mesenchymal transition (37). Overexpression of STS up-regulates β-catenin and its nuclear translocation. Inhbition of STS activity suppresses cyclin D1, c-Myc and MMP-7 and expression of the mesenchymal markers vimentin, N-cadherin and twist (37). In addition to the predicted effects of the novel STSi achieved through blocking DHEAS desulfatation, there is the potential for off target effects. Due to the fact that SI-1 and SI-2 have minimal effects in vitro in charcoal stripped media in the absence of ligand (data not shown), we feel that any off target activities are likely minor. Ongoing studies in our laboratories continue to investigate SI-1 and SI-2 to identify alternative effects these compounds may have, and for further clinical development to treat advanced prostate cancer.
In summary, we found that STS is overexpressed in CRPC cells. Overexpression of STS increases intracrine androgen synthesis and promotes cell proliferation and confers resistance to enzalutamide. Targeting STS activity using selected small molecule inhibitors of STS (STSi) inhibits STS activity, suppresses AR transcriptional activity, and reduces the growth of resistant C4–2B and VCaP prostate cancer cells in vitro and in vivo. Furthermore, STSi enhance enzalutamide treatment in vitro and in vivo. These studies suggest that STS plays a critical role in prostate cancer proliferation and targeting this enzyme represents a therapeutic strategy to treat CRPC and improve 2nd generation anti-androgen therapy.
Supplementary Material
Translational Relevance.
Most prostate cancer patients who receive anti-androgen treatment such as enzalutamide or abiraterone eventually develop resistance. We observed that an enzyme called steroid sulfatase (STS), which catalyzes the dehydroepiandrosterone sulfate (DHEAS) to the biologically active dehydroepiandrosterone (DHEA), contributes to anti-androgen resistance. We demonstrate that overexpression of STS increases intracrine androgen synthesis and confers resistance to enzalutamide and abiraterone. Inhibition of STS expression using specific siRNA or novel chemical inhibitors suppresses AR transcriptional activity, reduces cell growth, and enhances enzalutamide treatment in resistant prostate cancer cells in vitro and in vivo. Our studies indicate that STS drives sustained intracrine androgen synthesis and targeting this enzyme with novel inhibitors represents a therapeutic strategy to treat advanced prostate cancer and improve anti-androgen therapy in prostate cancer patients.
Acknowledgements
This work was supported in part by grants CA179970 (A.C. G), CA 225836 (A.C.G), DOD PC150229 (A.C. G), and the U.S. Department of Veterans Affairs, Office of Research & Development BL&D grant number I01BX0002653 (A.C. G), a Research Career Scientist Award (A.C. G). A.C.G is also a Research Career Scientist at VA Northern California Health Care System, Mather, California.
Footnotes
Conflict of interest: PKL and ACG are co-inventors of a patent application of the selected small molecule inhibitors of steroid sulfatase.
References
- 1.Fizazi K, Shore N, Tammela TL, Ulys A, Vjaters E, Polyakov S, et al. Darolutamide in Nonmetastatic, Castration-Resistant Prostate Cancer. N Engl J Med 2019;380(13):1235–46 doi 10.1056/NEJMoa1815671. [DOI] [PubMed] [Google Scholar]
- 2.Smith MR, Saad F, Chowdhury S, Oudard S, Hadaschik BA, Graff JN, et al. Apalutamide Treatment and Metastasis-free Survival in Prostate Cancer. N Engl J Med 2018;378(15):1408–18 doi 10.1056/NEJMoa1715546. [DOI] [PubMed] [Google Scholar]
- 3.de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, et al. Abiraterone and Increased Survival in Metastatic Prostate Cancer. New England Journal of Medicine 2011;364(21):1995–2005 doi doi: 10.1056/NEJMoa1014618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scher HI, Fizazi K, Saad F, Taplin M-E, Sternberg CN, Miller K, et al. Increased Survival with Enzalutamide in Prostate Cancer after Chemotherapy. New England Journal of Medicine 2012;367(13):1187–97 doi doi: 10.1056/NEJMoa1207506. [DOI] [PubMed] [Google Scholar]
- 5.Mohler JL, Gregory CW, Ford OH 3rd, Kim D, Weaver CM, Petrusz P, et al. The androgen axis in recurrent prostate cancer. Clin Cancer Res 2004;10(2):440–8. [DOI] [PubMed] [Google Scholar]
- 6.Montgomery RB, Mostaghel EA, Vessella R, Hess DL, Kalhorn TF, Higano CS, et al. Maintenance of intratumoral androgens in metastatic prostate cancer: a mechanism for castration-resistant tumor growth. Cancer Res 2008;68(11):4447–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mostaghel EA, Marck BT, Plymate SR, Vessella RL, Balk S, Matsumoto AM, et al. Resistance to CYP17A1 inhibition with abiraterone in castration-resistant prostate cancer: induction of steroidogenesis and androgen receptor splice variants. Clin Cancer Res 2011;17(18):5913–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mostaghel EA, Page ST, Lin DW, Fazli L, Coleman IM, True LD, et al. Intraprostatic androgens and androgen-regulated gene expression persist after testosterone suppression: therapeutic implications for castration-resistant prostate cancer. Cancer Res 2007;67(10):5033–41 doi 67/10/5033 [pii] 10.1158/0008-5472.CAN-06-3332. [DOI] [PubMed] [Google Scholar]
- 9.de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med 2011;364(21):1995–2005 doi 10.1056/NEJMoa1014618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ryan CJ, Smith MR, de Bono JS, Molina A, Logothetis CJ, de Souza P, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med 2013;368(2):138–48 doi 10.1056/NEJMoa1209096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Purohit A, Foster PA. Steroid sulfatase inhibitors for estrogen- and androgen-dependent cancers. The Journal of endocrinology 2012;212(2):99–110 doi 10.1530/JOE-11-0266. [DOI] [PubMed] [Google Scholar]
- 12.Nakamura Y, Suzuki T, Fukuda T, Ito A, Endo M, Moriya T, et al. Steroid sulfatase and estrogen sulfotransferase in human prostate cancer. Prostate 2006;66(9):1005–12 doi 10.1002/pros.20426. [DOI] [PubMed] [Google Scholar]
- 13.Mueller JW, Gilligan LC, Idkowiak J, Arlt W, Foster PA. The Regulation of Steroid Action by Sulfation and Desulfation. Endocrine reviews 2015;36(5):526–63 doi 10.1210/er.2015-1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tamae D, Mostaghel E, Montgomery B, Nelson PS, Balk SP, Kantoff PW, et al. The DHEA-sulfate depot following P450c17 inhibition supports the case for AKR1C3 inhibition in high risk localized and advanced castration resistant prostate cancer. Chemico-biological interactions 2015;234:332–8 doi 10.1016/j.cbi.2014.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gao AC. Best Abstract: Targeting STS to overcome resistance in PCa cells https://eaucongressuroweborg/best-abstract-targeting-sts-to-overcome-resistance-in-pca-cells Europeon Association of Urology Annual Congress EAU20, 2020.
- 16.James MR, Skaar TC, Lee RY, MacPherson A, Zwiebel JA, Ahluwalia BS, et al. Constitutive expression of the steroid sulfatase gene supports the growth of MCF-7 human breast cancer cells in vitro and in vivo. Endocrinology 2001;142(4):1497–505 doi 10.1210/endo.142.4.8091. [DOI] [PubMed] [Google Scholar]
- 17.Utsumi T, Yoshimura N, Takeuchi S, Ando J, Maruta M, Maeda K, et al. Steroid sulfatase expression is an independent predictor of recurrence in human breast cancer. Cancer Res 1999;59(2):377–81. [PubMed] [Google Scholar]
- 18.Foster PA, Woo LW, Potter BV, Reed MJ, Purohit A. The use of steroid sulfatase inhibitors as a novel therapeutic strategy against hormone-dependent endometrial cancer. Endocrinology 2008;149(8):4035–42 doi 10.1210/en.2008-0223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sadozai H Steroid sulfatase inhibitors: promising new therapy for breast cancer. JPMA The Journal of the Pakistan Medical Association 2013;63(4):509–15. [PubMed] [Google Scholar]
- 20.Saito T, Kinoshita S, Fujii T, Bandoh K, Fuse S, Yamauchi Y, et al. Development of novel steroid sulfatase inhibitors; II. TZS-8478 potently inhibits the growth of breast tumors in postmenopausal breast cancer model rats. The Journal of steroid biochemistry and molecular biology 2004;88(2):167–73 doi 10.1016/j.jsbmb.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 21.Foster PA, Newman SP, Chander SK, Stengel C, Jhalli R, Woo LL, et al. In vivo efficacy of STX213, a second-generation steroid sulfatase inhibitor, for hormone-dependent breast cancer therapy. Clin Cancer Res 2006;12(18):5543–9 doi 10.1158/1078-0432.CCR-06-0632. [DOI] [PubMed] [Google Scholar]
- 22.Stanway SJ, Delavault P, Purohit A, Woo LW, Thurieau C, Potter BV, et al. Steroid sulfatase: a new target for the endocrine therapy of breast cancer. Oncologist 2007;12(4):370–4 doi 10.1634/theoncologist.12-4-370. [DOI] [PubMed] [Google Scholar]
- 23.Palmieri C, Januszewski A, Stanway S, Coombes RC. Irosustat: a first-generation steroid sulfatase inhibitor in breast cancer. Expert review of anticancer therapy 2011;11(2):179–83 doi 10.1586/era.10.201. [DOI] [PubMed] [Google Scholar]
- 24.Sang X, Han H, Poirier D, Lin SX. Steroid sulfatase inhibition success and limitation in breast cancer clinical assays: An underlying mechanism. The Journal of steroid biochemistry and molecular biology 2018;183:80–93 doi 10.1016/j.jsbmb.2018.05.009. [DOI] [PubMed] [Google Scholar]
- 25.Coombes RC, Cardoso F, Isambert N, Lesimple T, Soulie P, Peraire C, et al. A phase I dose escalation study to determine the optimal biological dose of irosustat, an oral steroid sulfatase inhibitor, in postmenopausal women with estrogen receptor-positive breast cancer. Breast cancer research and treatment 2013;140(1):73–82 doi 10.1007/s10549-013-2597-8. [DOI] [PubMed] [Google Scholar]
- 26.Palmieri C, Stein RC, Liu X, Hudson E, Nicholas H, Sasano H, et al. IRIS study: a phase II study of the steroid sulfatase inhibitor Irosustat when added to an aromatase inhibitor in ER-positive breast cancer patients. Breast cancer research and treatment 2017;165(2):343–53 doi 10.1007/s10549-017-4328-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu C, Lou W, Zhu Y, Nadiminty N, Schwartz CT, Evans CP, et al. Niclosamide Inhibits Androgen Receptor Variants Expression and Overcomes Enzalutamide Resistance in Castration-Resistant Prostate Cancer. Clinical Cancer Research 2014;20(12):3198–210 doi 10.1158/1078-0432.ccr-13-3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolff B, Billich A, Brunowsky W, Herzig G, Lindley I, Nussbaumer P, et al. Microtiter plate cellular assay for human steroid sulfatase with fluorescence readout. Anal Biochem 2003;318(2):276–84. [DOI] [PubMed] [Google Scholar]
- 29.Liu C, Lou W, Zhu Y, Yang JC, Natiminty N, Gaikwad N, et al. Intracrine androgens and AKR1C3 activation confer resistance to enzalutamide in prostate cancer. Cancer Res 2015;75(7) doi 10.1158/0008-5472.CAN-14-3080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu C, Lou W, Yang JC, Liu L, Armstrong CM, Lombard AP, et al. Proteostasis by STUB1/HSP70 complex controls sensitivity to androgen receptor targeted therapy in advanced prostate cancer. Nat Commun 2018;9(1):4700 doi 10.1038/s41467-018-07178-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu C, Armstrong CM, Lou W, Lombard A, Evans CP, Gao AC. Inhibition of AKR1C3 Activation Overcomes Resistance to Abiraterone in Advanced Prostate Cancer. Mol Cancer Ther 2017;16(1):35–44 doi 10.1158/1535-7163.MCT-16-0186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stanway SJ, Purohit A, Woo LW, Sufi S, Vigushin D, Ward R, et al. Phase I study of STX 64 (667 Coumate) in breast cancer patients: the first study of a steroid sulfatase inhibitor. Clin Cancer Res 2006;12(5):1585–92 doi 10.1158/1078-0432.CCR-05-1996. [DOI] [PubMed] [Google Scholar]
- 33.Ishida H, Nakata T, Suzuki M, Shiotsu Y, Tanaka H, Sato N, et al. A novel steroidal selective steroid sulfatase inhibitor KW-2581 inhibits sulfated-estrogen dependent growth of breast cancer cells in vitro and in animal models. Breast cancer research and treatment 2007;106(2):215–27 doi 10.1007/s10549-007-9495-x. [DOI] [PubMed] [Google Scholar]
- 34.Ishida H, Nakata T, Sato N, Li PK, Kuwabara T, Akinaga S. Inhibition of steroid sulfatase activity and cell proliferation in ZR-75–1 and BT-474 human breast cancer cells by KW-2581 in vitro and in vivo. Breast cancer research and treatment 2007;104(2):211–9 doi 10.1007/s10549-006-9404-8. [DOI] [PubMed] [Google Scholar]
- 35.Rasmussen LM, Zaveri NT, Stenvang J, Peters RH, Lykkesfeldt AE. A novel dual-target steroid sulfatase inhibitor and antiestrogen: SR 16157, a promising agent for the therapy of breast cancer. Breast cancer research and treatment 2007;106(2):191–203 doi 10.1007/s10549-007-9494-y. [DOI] [PubMed] [Google Scholar]
- 36.Toren P, Hoffman A, Ding K, Joncas FH, Turcotte V, Caron P, et al. Serum Sex Steroids as Prognostic Biomarkers in Patients Receiving Androgen Deprivation Therapy for Recurrent Prostate Cancer: A Post Hoc Analysis of the PR.7 Trial. Clin Cancer Res 2018;24(21):5305–12 doi 10.1158/1078-0432.CCR-18-1187. [DOI] [PubMed] [Google Scholar]
- 37.Shin S, Im HJ, Kwon YJ, Ye DJ, Baek HS, Kim D, et al. Human steroid sulfatase induces Wnt/beta-catenin signaling and epithelial-mesenchymal transition by upregulating Twist1 and HIF-1alpha in human prostate and cervical cancer cells. Oncotarget 2017;8(37):61604–17 doi 10.18632/oncotarget.18645. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.