Structured Abstract
Objective
The aim of this systematic review and meta-analysis was to assess the risk of early mortality in hip fracture patients with COVID-19 infection who undergo surgical intervention.
Data sources
MEDLINE (PubMed) and CINAHL (Cumulative Index to Nursing and Allied Health Literature) databases.
Study selection
Studies were included in the systematic review if they reported postoperative mortality in patients with COVID-19 infection who underwent operative intervention for hip fracture. From this selection of studies, only investigations that reported postoperative mortality in a COVID-positive and a non-COVID group were included in the meta-analysis.
Data extraction
Data regarding patient demographics, age, and sex were recorded. Additional data that was extracted included study location, data collection period, length of follow-up, COVID testing methodology, COVID testing results, and number of patients who underwent operative versus nonoperative management. The primary outcome of interest was postoperative mortality.
Data synthesis
Random effects meta-analyses were performed to assess the pooled relative risk of postoperative mortality according to COVID status. Odds ratios and 95% confidence intervals (CI) were calculated.
Conclusions
The overall pooled mortality rate in the early postoperative period for hip fracture patients with concomitant COVID-19 infection was 32.6%. The relative risk for postoperative mortality in COVID-positive patients compared to non-COVID patients was 5.66 (95% CI 4.01–7.98; p < 0.001). The currently available literature demonstrates that COVID-19 infection represents a substantial risk factor for early postoperative mortality in the already susceptible hip fracture population. Further investigations will be needed to assess longer-term morbidity and mortality in this patient population.
Level of evidence
Therapeutic Level IV.
Keywords: Coronavirus, COVID-19, Pandemic, Hip fracture, Mortality
1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) - also known as 2019 novel coronavirus or COVID-19 - first emerged on December 31, 2019 in China, and has since rapidly spread to become a world-wide pandemic. The impact of this pandemic has been widespread, but healthcare systems have been uniquely affected. In the field of orthopaedic surgery, there has been a significant decline in the volume of surgical cases.1 In some instances, hospitals have become overwhelmed with COVID-19 patients and cancelled elective procedures to stem the spread of COVID-19 and conserve healthcare resources. Overall, there has also been a decrease in patients seeking elective or non-emergent medical care due to anxiety and fears evoked by the ongoing pandemic.2,3
Orthopaedic trauma services, however, have maintained a significant portion of their previous volume throughout the pandemic. Specifically, hip fractures in the elderly population have continued to present to hospitals at levels comparable to before the pandemic, even in regions that were the hardest hit by COVID-19 outbreaks.4, 5, 6 These patients require prompt evaluation and treatment, as mortality rates from hip fractures without appropriate surgical intervention are extremely high.7, 8, 9, 10 Urgent and emergent surgical cases – which include hip fractures – have been proceeding at the majority of medical centers worldwide,2 and while many protocols for operating room procedures during the pandemic have been instituted,11 reports on the impact of COVID-19 infection on postoperative outcomes are just beginning to emerge.
The impact of COVID-19 infection on hip fracture patients is important to understand because of the overlap in characteristics between patients at high risk for poor outcomes from COVID-19 infection and those at high risk for poor outcomes from sustaining a hip fracture.12, 13, 14 Because of its significant potential to adversely affect outcomes, COVID-19 status is an important variable to consider in developing treatment algorithms for hip fracture patients in the setting of the ongoing pandemic.15 The objective of this study was to perform a systematic review and meta-analysis of the current literature reporting on the early outcomes of hip fracture patients with COVID-19 infection who underwent surgical intervention. The meta-analysis aimed to assess the risk of mortality in this patient population compared to non-COVID hip fracture patients. We hypothesized that there would be a significantly elevated rate of early mortality in COVID-positive (COVID+) patients who underwent hip fracture surgery.
2. Materials and methods
Literature Search. A systematic review of publicly available literature regarding the outcomes of hip fracture patients during the COVID-19 pandemic was conducted on September 10, 2020 adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.16 The databases queried were MEDLINE (PubMed) and CINAHL (Cumulative Index to Nursing and Allied Health Literature). The MEDLINE (PubMed) search strategy was as follows:
-
●
Search 1: “fracture” [MeSH Terms] OR “fracture” [All Fields]
-
●
Search 2: “coronavirus” [MeSH Terms] OR “coronavirus” [All Fields] “COVID” [MeSH Terms] OR “COVID” [All Fields]
-
●
Search 3: search 1 AND search 2
Only results with a publication year of 2020 were included in the search. These parameters were repeated in the CINAHL database.
All studies were initially screened by title and abstract, followed by full text review. The exclusion criteria included non-English-language studies, letters to the editor, and studies without any COVID+ patients. Level I, II, III, or IV evidence was acceptable (as per the Oxford Centre for Evidence-Based Medicine guidelines).17 In the event of disagreement on study inclusion, discussion and group consensus determined the final decision.
Patient demographics, age, and sex were extracted from the included studies. Additional data that was extracted included patient selection criteria, data collection period, length of follow-up, COVID testing methodology, COVID testing results, and number of patients who underwent nonoperative management. The primary outcome of interest was postoperative mortality.
Meta-Analysis. All included studies that reported postoperative mortality for a COVID+ and non-COVID group were included in the meta-analysis. These were assessed for quality using the Office of Health Assessment and Translation (OHAT) risk of bias tool. Data from each study was reviewed to remove outcomes from patients who underwent nonoperative treatment. In cases where mortality data for the COVID+ and non-COVID groups were unclear from the published manuscript, the corresponding author for the respective publication was contacted for clarification. The initial analysis stratified between COVID+ patients and non-COVID patients (patients with a negative COVID test result and patients who were not tested for COVID). Patients without COVID testing results were then excluded in a subsequent analysis. Separate analyses were conducted for studies with 30-day follow-up versus less than 30-day follow-up. For studies that reported on patients with fractures that were not hip fractures, all non-hip fractures were excluded from the meta-analysis. Case series and studies without COVID+ patients who underwent operative intervention were excluded from the meta-analysis.
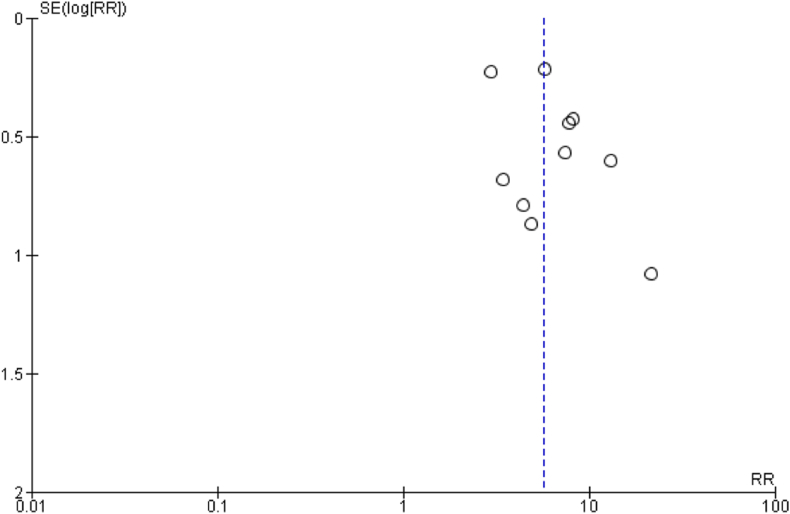
Publication Bias. Publication bias was determined to be unlikely on this topic given the potential high impact of a study demonstrating zero or negative effects of COVID-19 infection on postoperative mortality. Nonetheless, the results of each included study were displayed in funnel plots, which were qualitatively evaluated to assess for asymmetry. No quantitative analyses were conducted.
Heterogeneity. Heterogeneity between studies was assessed quantitatively with the Cochrane Q test and the I2 test.18
Pooled Effect. Included studies in which hip fracture mortality was the primary reported outcome were analyzed to determine the pooled relative risk. Because of varying testing protocols, the groups in the primary analysis were defined as COVID+ (positive COVID-19 swab test result) versus non-COVID (negative COVID-19 test result or did not meet criteria to warrant a COVID-19 test). The relative risk of mortality was initially calculated for these two groups. However, there were varying testing protocols utilized during the height of the pandemic. As such, a secondary analysis was conducted excluding patients who did not undergo COVID-19 testing. The relative risk for postoperative hip fracture mortality was then determined based on COVID-19 test status (positive versus negative). Further sub-analyses of these groups were performed to evaluate the relative risk of mortality based on studies with 30-day follow-up or less than 30-day follow-up. For pooled estimation, a random-effects model was chosen based on the significant variability between included studies from variables such as the type of medical management, treating institution, and patient population. Data analysis was performed using Review Manager (RevMan) version 5.4 (The Cochrane Collaboration). A p-value <0.05 was considered to be statistically significant.
3. Results
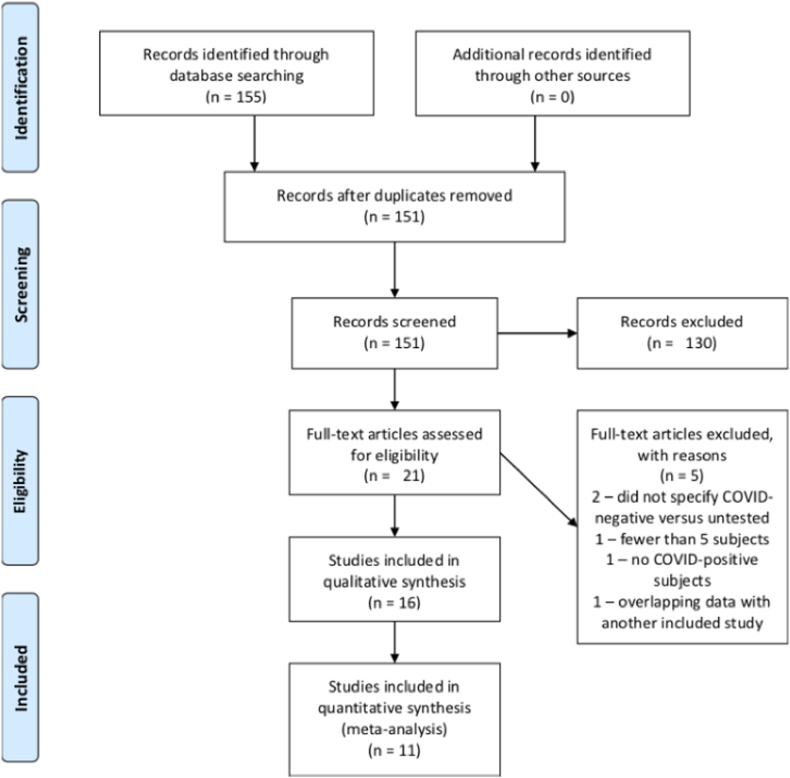
Literature Search. The initial literature search identified 155 studies. After removal of duplicates, 151 unique studies were identified and 43 potentially relevant titles were selected for abstract review. One was excluded because it was a Letter to the Editor. Twenty-one studies were eliminated after abstract screening. After full text review of the remaining 21 studies, a total of 16 studies were included for analysis (Fig. 1).4,5,19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32 No additional potentially relevant titles were identified from screening the reference lists of the included studies. There were 5 case series, 8 retrospective cohort studies, and 3 prospective cohort studies (Table 1). There were 2 studies from Asia (1 from China and 1 from Iran), 3 studies from the United States (all from New York City), and 11 studies from Europe (7 from the United Kingdom, 2 from Spain, and 2 from Italy).
Fig. 1.
PRISMA flow diagram outlining the search strategy.
Table 1.
Study characteristics and patient demographics.
| Study | Study Design | Study Location | Mean Age (Range) | COVID-19 Test Method | Overall Female (%) | COVID + Female (%) | Non-COVID Female (%) | Data Collection Period | Follow-up |
|---|---|---|---|---|---|---|---|---|---|
| LeBrun et al. | Retrospective cohort | NYC | 85 (65–100) | PCR | 44 (74.6%) | 6 (66.7%) | 38 (76%) | 3/20/2020–4/25/2020 | Inpatient |
| Munoz Vives et al. | Retrospective case-control | Spain | 85.3 (65–101) | PCR | 102 (75%) | Not reported | Not reported | 3/14/2020–April 4, 2020 | 14 days |
| Cheung & Forsh | Case series | NYC | 79.7 (67–90) | PCR | 8 (80%) | 8 (80%) | N/A | 3/1/2020–5/22/2020 | Inpatient |
| Maniscalco et al. | Retrospective cohort | Italy | 81.6 (41–99) | CT scan with confirmatory PCR or PCR-alone | 89 (73.6%) | Not reported | Not reported | 2/22/2020–4/18/2020 | 21 days |
| Egol et al. | Retrospective cohort | NYC | 83.0 (Not reported) | PCR | 88 (63.8%) | 5 (29.4%) | 73 (68.2%) | January 2, 2020–4/15/2020 | Inpatient & 30 days |
| Catellani et al. | Case series | Italy | 85 (74–90) | PCR | 6 (37.5%) | 6 (37.5%) | N/A | 2/2020–4/2020 | Inpatient |
| Mi et al. | Case series | China | 75.6 (50–85) | PCR/CT scan | 4 (66.6%) | 4 (66.6%) | N/A | January 1, 2020–2/27/2020 | Inpatient |
| Hall et al. | Retrospective cohort | UK | 80.7 (50–101) | PCR | 211 (66.6%) | 13 (48.1%) | 198 (86.3%) | 3/1/2020–4/15/2020 | 30-day minimum |
| Kayani et al. | Retrospective cohort | UK | 72.5 (Not reported) | PCR | 255 (60.4%) | 51 (62.2%) | 204 (60%) | 2/1/2020–4/20/2020 | 30 days |
| Thakrar et al. | Prospective cohort | UK | 81.6 (Not reported) | PCR | 20 (46.5%) | Not reported | Not reported | 3/15/2020–4/14/2020 | 30 days |
| Segarra et al. | Prospective cohort | Spain | 82.4 (not reported) | PCR | 47 (69.1%) | 2 (100%) | 45 (69.2%) | January 2, 2020–4/15/2020 | 69.7 days |
| Sobti et al. | Retrospective cohort | UK | 83.5 (Not reported) | Not specified | Not reported | Not reported | Not reported | 3/1/2020–5/31/2020 | Not reported |
| Malik-Tabassum et al. | Retrospective cohort | UK | 84.3 (Not reported) | Not specified | 43 (63.2%) | 0 (0%) | 43 (64.2%) | 3/23/2020–5/11/2020 | 30 days |
| Rabie et al. | Case series | Iran | 81 (72–91) | PCR | 3 (75%) | 3 (75%) | N/A | Not reported | Not reported |
| Narang et al. | Prospective cohort | UK | 84 (Not reported) | PCR | 477 (70.4%) | 53 (62.4%) | 424 (71.5%) | January 3, 2020–4/30/2020 | 30 days |
| Dupley et al. | Case series | UK | 83 (Not reported) | PCR | 35 (54.7%) | 35 (54.7%) | N/A | January 3, 2020–4/26/2020 | 30 days |
Demographics. Table 1 outlines the patient demographics from the 16 included studies. There were a total of 2248 hip fracture patients, including 397 patients who were COVID+ and 1851 patients who were not COVID+. Of the non-COVID patients, 1011 were COVID-negative (COVID-) and 840 had unknown COVID-19 status.
Mortality. The primary outcome of interest was inpatient or early mortality. All 16 included studies reported mortality rates (Table 2). The overall early postoperative mortality rate in COVID+ hip fracture patients across all of the included studies was 32.6% (119/365).
Table 2.
COVID-19 status and postoperative mortality.
| Study | Total Number of Hip Fracture Patients | COVID-19 Test Status |
Number of Nonoperative COVID + Patients | Overall Postoperative Mortality | COVID + Postoperative Mortality | ||
|---|---|---|---|---|---|---|---|
| COVID+ | COVID- | Untested/Undefined COVID-19 Status | |||||
| LeBrun et al. | 59 | 9 | 40 | 10 | 2 | 4 | 3/7 (42.9%) |
| Munoz Vives et al. | 136 | 23 | 39 | 74 | 8 | 5 | 2/15 (13.3%) |
| Cheung & Forsh | 10 | 10 | 0 | 0 | 0 | 1 | 1/10 (10.0%) |
| Maniscalco et al. | 121 | 32 | 32 | 57 | 0 | 17 | 14/32 (43.8) |
| Egol et al. | 138 | 17 | 107 | 14 | 4 | 15 | 7/13 (53.8%) |
| Catellani et al. | 16 | 16 | 0 | 0 | 3 | 4 | 4/13 (30.8%) |
| Mi et al. | 6 | 6 | 0 | 0 | 3 | 1 | 1/3 (33.3%) |
| Hall et al. | 317 | 27 | 290 | 0 | 2 | 17 | 7/25 (28%) |
| Kayani et al. | 422 | 82 | 340 | 0 | 0 | 60 | 25/82 (30.5%) |
| Thakrar et al.a | 43 | 12 | 6 | 25 | 0 | 7 | 4/12 (33.3%) |
| Segarra et al. | 68 | 2 | 59 | 7 | 0 | 8 | 1/2 (50.0%) |
| Sobti et al. | 94 | 6 | 47 | 41 | 0 | 9 | 3/6 (50.0%) |
| Malik-Tabassum et al. | 68 | 1 | 51 | 16 | 1 | 6 | 0/0 |
| Rabie et al. | 4 | 4 | 0 | 0 | 3 | 0 | 0/1 |
| Narang et al. | 682 | 86 | 0 | 596 | 0 | 66 | 30/86 (34.9%) |
| Dupley et al. | 64 | 64 | 0 | 0 | 6 | 17 | 17/58 (29.3%) |
| 2248 | 397 | 1011 | 840 | 32 | 237 | 119/365 (32.6%) | |
Data obtained from authors.
Meta-analysis. Of the included studies, 10 reported mortality for a COVID+ and non-COVID cohort, and were included in the meta-analysis. One of these studies did not provide clear differentiation between COVID- and untested patients, and was excluded from the COVID+ versus COVID- sub-analysis.24 Five studies reported 30-day follow-up,24, 25, 26, 27,31 and 4 studies reported less than 30-day follow-up.5,19, 20, 21,28 One study reported on both inpatient and 30-day mortality, and the 30-day data was utilized in the meta-analysis.4
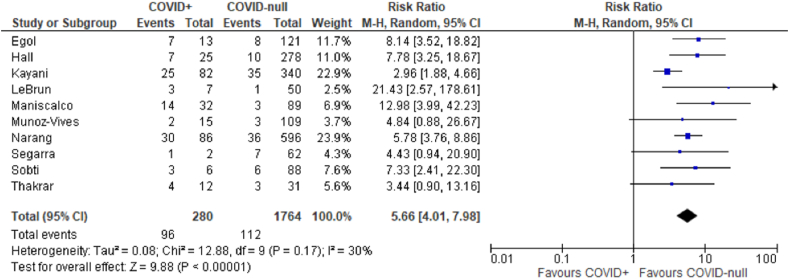
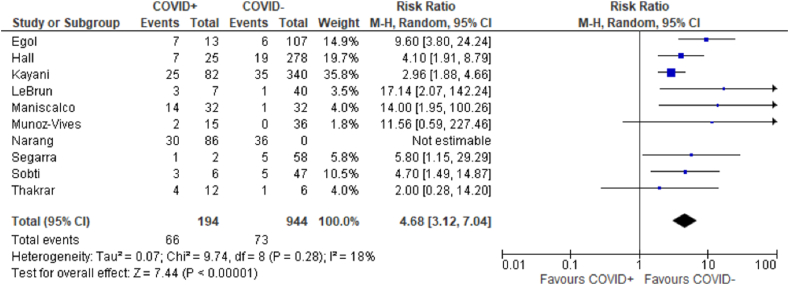
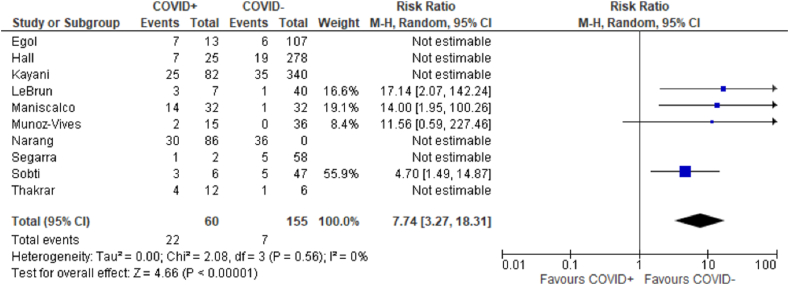
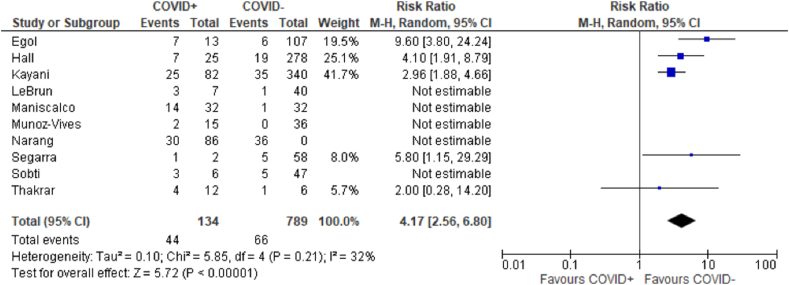
Pooled Effect. The relative risk for mortality for COVID+ compared to non-COVID patients was 5.66 (95% CI 4.01–7.98; p < 0.001) (Fig. 2). After excluding patients without COVID-19 test results from the non-COVID cohort, the relative risk for mortality for COVID+ patients was 4.68 (95% CI 3.12–7.04; p < 0.001) (Fig. 3). There was a greater effect of COVID-19 infection on mortality in studies with less than 30-day follow-up (RR 7.74; 95% CI 3.27–18.31; p < 0.001) compared to those studies with a minimum 30-day follow-up (RR 4.17; 95% CI 2.56–6.80; p < 0.001) (Fig. 4, Fig. 5).
Fig. 2.
Forest plot of postoperative mortality in COVID+ versus non-COVID hip fracture patients.
Fig. 3.
Forest plot of postoperative mortality in hip fracture patients with COVID+ testing versus COVID- testing.
Fig. 4.
Forest plot of postoperative mortality with less than 30-day follow-up in hip fracture patients with COVID+ testing versus COVID- testing.
Fig. 5.
Forest plot of postoperative mortality with a minimum 30-day follow-up in hip fracture patients with COVID+ testing versus COVID- testing.
Publication Bias. The funnel plot for the included studies showed no apparent publication bias on qualitative evaluation as demonstrated in Fig. 6.
Fig. 6.
Funnel plot of included studies demonstrating no apparent publication bias.
Heterogeneity. There were multiple potential sources of heterogeneity among the included studies. COVID-19 testing criteria varied among studies, with some studies reporting testing of all included patients and others reporting limited testing based on symptomatology. Additionally, testing algorithms were noted to have evolved even within individual studies due to the rapidly changing nature of the pandemic. The included studies also represented heterogeneous patient populations from different geographic locations. Despite these potential sources of heterogeneity, the I2 index in our primary analysis was 30% (p = 0.17), which did not demonstrate a statistically significant amount of heterogeneity between reported risks of mortality.
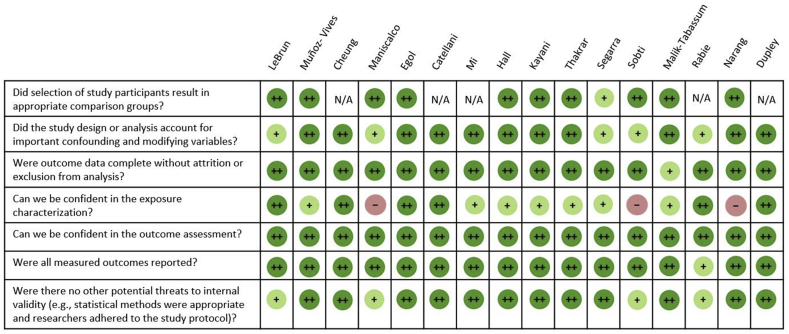
Risk of Bias. The risk of bias in each of the included studies as determined using the OHATS criteria is outlined in Fig. 7.
Fig. 7.
Risk of bias in the included studies according to the OHATS criteria.
4. Discussion
In this systematic review and meta-analysis, COVID+ patients with hip fractures who underwent surgical intervention had more than 5 times higher risk of early mortality compared to hip fracture patients without COVID-19 infection. The overall mortality rate of COVID+ hip fracture patients in the early postoperative period was 32.6%. This exceeded the mortality rate previously reported in patients with a hip fracture or COVID-19 infection in isolation, suggesting that there may be an effect modification of COVID-19 infection on mortality in hip fracture patients who undergo surgical treatment.33
Elderly patients who become infected with COVID-19 have a reported mortality rate between 15% and 30%, with mortality risk being correlated with increasing age.33,34 A recent meta-analysis demonstrated less than 1% mortality in patients aged <50 years, compared to an exponential increase in mortality after age 50.35 Patients aged 80 years had the highest mortality rate at nearly 30%, which was 6-fold higher than the mortality rate of patients aged <80 years.35
Independent of COVID-19 infection, hip fracture patients have significant morbidity and mortality, with 1-year mortality rates estimated between 8.5% and 36%.36,37 Many medical comorbidities have been identified as risk factors for adverse outcomes after hip fracture surgery, including obesity, hypertension, heart failure, active smoking, and chronic obstructive pulmonary disease.37 Preoperative disease burden plays a significant role in hip fracture outcomes, and COVID-19 infection likely represents an additional risk factor that further contributes to the pre-existing comorbidity burden in this patient population. A recent study using a modification to the Score for Trauma Triage in the Geriatric and Middle-Aged tool to evaluate the significance of COVID-19 infection as an independent factor for predicting mortality supports this assertion.15
Overall, the majority of included studies in this meta-analysis consistently reported high early postoperative mortality rates >30% for COVID+ hip fracture patients. However, one case series reported a lower mortality rate of 10% in 10 patients.21 The authors noted that nearly all of the COVID+ hip fracture patients in their series were asymptomatic or had only mild COVID-19 symptoms on admission. This was in contrast to other studies in which patients presented with clear evidence of symptomatic COVID-19 infection.22 The relatively low mortality rate observed in this case series was therefore attributed to the lack of severe COVID-19 symptomatology on presentation.21 Consistent with this, another study reported a mortality rate of 30% and 12.5% in symptomatic and asymptomatic COVID+ hip fracture patients, respectively.15 Symptomatology and severity of COVID-19 infection are therefore important factors to consider in managing and treating COVID+ hip fracture patients.
The body's response to trauma is often thought of in terms of a two-hit model, where trauma itself is regarded as the “first hit”. Inflammatory or hypercoagulable states may then further amplify this “first hit”. Current reports about the immunologic response to COVID-19 infection indicate that there is an inflammatory response with elevations of proinflammatory cytokines, including interleukin-2 (IL-2), IL-6, and tumor necrosis factor (TNF-).38 Systemic inflammation from COVID-19 infection is thought to cause endothelial dysfunction, which then predisposes to microangiopathy and microthrombi.39 Clinically, this can place patients at risk for thromboembolic events such as pulmonary embolism, and thereby further exacerbate hypoxemia secondary to COVID-related acute respiratory distress syndrome (ARDS). In addition to microvascular disease, COVID-19 infection has also been associated with a prothrombotic state characterized by elevated D-dimer levels, increased fibrinogen and fibrin degradation product levels, decreased international normalized ratio (INR) and prothrombin time, and disseminated intravascular coagulation (DIC).40 The hyperinflammatory and hypercoagulable state induced by COVID-19 infection may therefore amplify the initial inflammatory response to low-energy trauma such as a hip fracture (i.e., “first hit”), and thereby predispose this high risk patient population to a catastrophic “second hit”.41
Based on a modified risk stratification tool to predict inpatient mortality in geriatric and middle-aged trauma patients (modified Score for Trauma Triage in the Geriatric and Middle-Aged-COVID inpatient mortality risk scores or STTGMACOVID), Konda et al. triaged 100% of COVID-19 patients with low-energy geriatric hip fractures to the highest risk quartile.15 COVID+ or COVID-suspected hip fracture patients during the pandemic in their New York City cohort were found to have 32 times increased risk of inpatient mortality and 5.2 times increased risk of 30-day mortality, compared with COVID- patients. Furthermore, patients with higher scores on the modified risk stratification tool had longer LOS, greater need for ICU-level care, and longer ICU LOS. COVID-19 infection therefore places hip fracture patients at extremely high risk for morbidity and mortality, and the authors proposed that surgical treatment should be deferred until COVID-19 symptoms have improved or resolved, with downgrading of their inpatient mortality risk on the STTGMACOVID risk stratification tool. Inflammatory markers (such as erythrocyte sedimentation rate and C-reactive protein) are important potential adjuncts to this algorithm, which have not yet been well-reported in the current literature. These reports of a significantly higher risk of inpatient mortality associated with COVID-19 infection are consistent with the findings from our meta-analysis of the current literature, which demonstrated 7.7 times increased risk of mortality in studies with <30-day follow-up and 4.2 times increased risk of mortality in studies with a minimum 30-day follow-up.
While this meta-analysis focused on operative outcomes, it should be noted that during the pandemic, there has been a higher than usual rate of nonoperative treatment of hip fractures in COVID+ or COVID-suspected patients. Konda et al. reported a 16.1% rate of nonoperative treatment (compared to 1.4% prior to the pandemic), which was directly attributable to COVID-19 symptoms on admission.15 Geriatric hip fracture patients who undergo nonoperative treatment are known to have significantly higher mortality than patients who undergo operative treatment.8 In a cohort of 77 hip fracture patients who underwent nonoperative treatment, mortality rates during inpatient stay, at 30-days, and at 1-year were reported to be 28.6%, 63.6%, and 84.4%, respectively.8 This was dramatically higher than mortality rates in a matched cohort of hip fracture patients who underwent operative treatment (3.9%, 11.0%, and 36.4%, respectively). At this time, there remains limited data on outcomes for hip fracture patients with concomitant COVID-19 infection who were treated nonoperatively. However, early data from limited sample sizes suggests an even higher early mortality rate in these patients compared to those without COVID-19 infection who undergo nonoperative treatment. For example, Mi et al. reported a 67% inpatient mortality rate (2/3), while Konda et al. reported a 40% inpatient mortality rate (2/5) in hip fracture patients who were deemed too sick and not appropriate for operative intervention during the COVID-19 pandemic.15,23
There are several limitations to our systematic review and meta-analysis of early postoperative mortality in patients with concomitant hip fracture and COVID-19 infection. Given the relatively recent outbreak of the COVID-19 pandemic, studies selected for inclusion were largely retrospective cohort studies or case series with small sample sizes. No randomized controlled studies have been performed yet. The inter-study heterogeneity regarding patient inclusion criteria, fracture characteristics, and medical management presents another limitation to this meta-analysis. Clinical criteria for COVID testing and diagnostic criteria for COVID-19 infection also differed among studies. Furthermore, studies categorized patients according to COVID-19 status (i.e., COVID+, COVID-suspected, or COVID-), but patients were not further subcategorized according to symptomatology such as oxygen requirement. Therefore, asymptomatic COVID+ patients were not differentiated from symptomatic COVID+ patients. Future investigations on postoperative mortality in COVID+ hip fracture patients should account for symptomatology and inflammatory markers, which could provide important prognostic markers to help guide management decisions and determine the appropriate timing of operative intervention in surgical candidates.
In summary, the overall mortality rate in the early postoperative period for hip fracture patients with concomitant COVID-19 infection who underwent operative treatment was 32.6%. COVID+ hip fracture patients had greater than 5 times increased risk of early mortality compared to non-COVID patients. This elevated mortality risk was more pronounced in the immediate 30-day postoperative period. The currently available literature demonstrates that COVID-19 infection represents a substantial risk factor for early postoperative mortality in the already susceptible hip fracture population. Further investigations will be needed to assess longer-term morbidity and mortality in this patient population.
5. Institutional review board approval
IRB approval was not required for the submitted work at our institution.
Declaration of competing interest
Dr. Forsh has financial relationships with Stryker (paid consultant). None of the other authors have any financial interests or affiliations with institutions, organizations, or companies relevant to the manuscript. None of the authors received payment or funding support in kind for any aspect of the submitted work.
References
- 1.Wong J.S.H., Cheung K.M.C. Impact of COVID-19 on orthopaedic and trauma service: an epidemiological study. J Bone Joint Surg Am. 2020;102(14):e80. doi: 10.2106/JBJS.20.00775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Randelli P.S., Compagnoni R. Management of orthopaedic and traumatology patients during the Coronavirus disease (COVID-19) pandemic in northern Italy. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1683–1689. doi: 10.1007/s00167-020-06023-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Emanuel E.J., Persad G., Upshur R. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382(21):2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 4.Egol K.A., Konda S.R., Bird M.L., NYU COVID Hip Fracture Research Group Increased mortality and major complications in hip fracture care during the COVID-19 pandemic: a New York City perspective. J Orthop Trauma. 2020;34(8):395–402. doi: 10.1097/BOT.0000000000001845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maniscalco P., Poggiali E., Quattrini F. Proximal femur fractures in COVID-19 emergency: the experience of two Orthopedics and Traumatology Departments in the first eight weeks of the Italian epidemic. Acta Biomed. 2020;91(2):89–96. doi: 10.23750/abm.v91i2.9636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nunez J.H., Sallent A., Lakhani K. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury. 2020;51(7):1414–1418. doi: 10.1016/j.injury.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moja L., Piatti A., Pecoraro V. Timing matters in hip fracture surgery: patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PloS One. 2012;7(10) doi: 10.1371/journal.pone.0046175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chlebeck J.D., Birch C.E., Blankstein M., Kristiansen T., Bartlett C.S., Schottel P.C. Nonoperative geriatric hip fracture treatment is associated with increased mortality: a matched cohort study. J Orthop Trauma. 2019;33(7):346–350. doi: 10.1097/BOT.0000000000001460. [DOI] [PubMed] [Google Scholar]
- 9.Frenkel Rutenberg T., Assaly A., Vitenberg M. Outcome of non-surgical treatment of proximal femur fractures in the fragile elderly population. Injury. 2019;50(7):1347–1352. doi: 10.1016/j.injury.2019.05.022. [DOI] [PubMed] [Google Scholar]
- 10.van de Ree C.L.P., De Jongh M.A., Peeters C.M.M., de Munter L., Roukema J.A., Gosens T. Hip fractures in elderly people: surgery or no surgery? A systematic review and meta-analysis. Geriatr Orthop Surg Rehabil. 2017;8(3):173–180. doi: 10.1177/2151458517713821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Awad M.E., Rumley J.C.L., Vazquez J.A., Devine J.G. Perioperative considerations in urgent surgical care of suspected and confirmed COVID-19 orthopaedic patients: operating room protocols and recommendations in the current COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28(11):451–463. doi: 10.5435/JAAOS-D-20-00227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Du R.H., Liang L.R., Yang C.Q. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020;55(5):2000524. doi: 10.1183/13993003.00524-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shahid Z., Kalayanamitra R., McClafferty B. COVID-19 and older adults: what we know. J Am Geriatr Soc. 2020;68(5):926–929. doi: 10.1111/jgs.16472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Konda S.R., Ranson R.A., Solasz S.J., NYU COVID Hip Fracture Research Group Modification of a validated risk stratification tool to characterize geriatric hip fracture outcomes and optimize care in a post-COVID-19 world. J Orthop Trauma. 2020;34(9):e317–e324. doi: 10.1097/BOT.0000000000001895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moher D., Shamseer L., Clarke M., PRISMA-P Group Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Obremskey W.T., Pappas N., Attallah-Wasif E., Tornetta P., Bhandari M. Level of evidence in orthopaedic journals. J Bone Joint Surg Am. 2005;87(12):2632–2638. doi: 10.2106/JBJS.E.00370. [DOI] [PubMed] [Google Scholar]
- 18.Higgins J.P.T., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 19.LeBrun D.G., Konnaris M.A., Ghahramani G.C. Hip fracture outcomes during the COVID-19 pandemic: early results from New York. J Orthop Trauma. 2020;34(8):403–410. doi: 10.1097/BOT.0000000000001849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Munoz Vives J.M., Jornet-Gibert M., Camara-Cabrera J. Spanish HIP-COVID Investigation Group. Mortality rates of patients with proximal femoral fracture in a worldwide pandemic: preliminary results of the Spanish HIP-COVID Observational Study. J Bone Joint Surg Am. 2020;102(13):e69. doi: 10.2106/JBJS.20.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cheung Z.B., Forsh D.A. Early outcomes after hip fracture surgery in COVID-19 patients in New York City. J Orthop. 2020;21:291–296. doi: 10.1016/j.jor.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Catellani F., Coscione A., D'Ambrosi R., Usai L., Roscitano C., Fiorentino G. Treatment of proximal femoral fragility fractures in patients with COVID-19 during the SARS-CoV-2 outbreak in Northern Italy. J Bone Joint Surg Am. 2020;102(12):e58. doi: 10.2106/JBJS.20.00617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mi B., Chen L., Xiong Y., Xue H., Zhou W., Liu G. Characteristics and early prognosis of COVID-19 infection in fracture patients. J Bone Joint Surg Am. 2020;102(9):750–758. doi: 10.2106/JBJS.20.00390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hall A.J., Clement N.D., Farrow L., IMPACT-Scot Study Group IMPACT-Scot report on COVID-19 and hip fractures. Bone Joint Lett J. 2020;102-B(9):1219–1228. doi: 10.1302/0301-620X.102B9.BJJ-2020-1100.R1. [DOI] [PubMed] [Google Scholar]
- 25.Kayani B., Onochie E., Patil V. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Joint Lett J. 2020;102-B(9):1136–1145. doi: 10.1302/0301-620X.102B9.BJJ-2020-1127.R1. [DOI] [PubMed] [Google Scholar]
- 26.Thakrar A., Chui K., Kapoor A., Hambidge J. Thirty-day mortality rate of patients with hip fractures during the COVID-19 pandemic: a single centre prospective study in the United Kingdom. J Orthop Trauma. 2020;34(9):e325–e329. doi: 10.1097/BOT.0000000000001889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Segarra B., Ballesteros Heras N., Viadel Ortiz M., Ribes-Iborra, Martinez-Macias O., Cuesta-Peredo D. Are hospitals safe? A prospective study on SARS-CoV-2 prevalence and outcome on surgical fracture patients: a closer look at hip fracture patients. J Orthop Trauma. 2020;34(10):e371–e376. doi: 10.1097/BOT.0000000000001899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sobti A., Memon K., Bhaskar R.P.P., Unnithan A., Khaleel A. Outcome of trauma and orthopaedic surgery at a UK district general hospital during the Covid-19 pandemic. J Clin Orthop Trauma. 2020;11(Suppl 4):S442–S445. doi: 10.1016/j.jcot.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Malik-Tabassum K., Crooks M., Robertson A., To C., Maling L., Selmon G. Management of hip fractures during the COVID-19 pandemic at a high-volume hip fracture unit in the United Kingdom. J Orthop. 2020;20:332–337. doi: 10.1016/j.jor.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rabie H., Sharafi M.H., Oryadi Zanjani L., Nabian M.H. Novel coronavirus infection in orthopedic patients: report of seven cases. Arch Bone Jt Surg. 2020;8(Suppl 1):302–309. doi: 10.22038/abjs.2020.47805.2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Narang A., Chan G., Aframian A. Thirty-day mortality following surgical management of hip fractures during the COVID-19 pandemic: findings from a prospective multi-centre UK study. Int Orthop. 2020:1–9. doi: 10.1007/s00264-020-04739-y. (Online ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dupley L., Oputa T.J., Bourne J.T., North West COVID NOF Study Group 30-day mortality for fractured neck of femur patients with concurrent COVID-19 infection. Eur J Orthop Surg Traumatol. 2020:1–7. doi: 10.1007/s00590-020-02778-0. (Online ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Imam Z., Odish F., Gill I. Older age and comorbidity are independent mortality predictors in a large cohort of 1305 COVID-19 patients in Michigan, United States. J Intern Med. 2020;288(4):469–476. doi: 10.1111/joim.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shah P., Owens J., Franklin J. Demographics, comorbidities and outcomes in hospitalized Covid-19 patients in rural southwest Georgia. Ann Med. 2020;52(7):354–360. doi: 10.1080/07853890.2020.1791356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bonanad C., Garcia-Blas S., Tarazona-Santabalbina F. The effect of age on mortality in patients with COVID-19: a meta-analysis with 611,583 subjects. J Am Med Dir Assoc. 2020;21(7):915–918. doi: 10.1016/j.jamda.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hu F., Jiang C., Shen J., Tang P., Wang Y. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. 2012;43(6):676–685. doi: 10.1016/j.injury.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 37.Sathiyakumar V., Greenberg S.E., Molina C.S., Thakore R.V., Obremskey W.T., Sethi M.K. Hip fractures are risky business: an analysis of the NSQIP data. Injury. 2015;46(4):703–708. doi: 10.1016/j.injury.2014.10.051. [DOI] [PubMed] [Google Scholar]
- 38.Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J., HLH Across Specialty Collaboration, UK COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu P.P., Blet A., Smyth D., Li H. The science underlying COVID-19: implications for the cardiovascular system. Circulation. 2020;142(1):68–78. doi: 10.1161/CIRCULATIONAHA.120.047549. [DOI] [PubMed] [Google Scholar]
- 40.Ranucci M., Ballotta A., Di Dedda U. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J Thromb Haemostasis. 2020;18(7):1747–1751. doi: 10.1111/jth.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Puzzitiello R.N., Pagani N.R., Moverman M.A., Moon A.S., Menendez M.E., Ryan S.P. Inflammatory and coagulative considerations for the management of orthopaedic trauma patients with COVID-19: a review of the current evidence and our surgical experience. J Orthop Trauma. 2020;34(8):389–394. doi: 10.1097/BOT.0000000000001842. [DOI] [PMC free article] [PubMed] [Google Scholar]