Abstract
Several registries and quality improvement initiatives have focused on assessing and improving secondary prevention of CVD in India. While the Treatment and Outcomes of Acute Coronary Syndromes in India (CREATE), Indian Heart Rhythm Society-Atrial Fibrillation (IHRS-AF), and Trivandrum Heart Failure (THF) registries are limited to collecting data, the Tamil Nadu–ST-Segment Elevation Myocardial Infarction (TN-STEMI) program was aimed at examining and improving access to revascularization after an ST-elevation myocardial infarction (STEMI). The Acute Coronary Syndromes: Quality Improvement in Kerala (ACS-QUIK) study recruited hospitals from the Kerala ACS registry to assess a quality improvement kit for patients with ACS while the Practice Innovation and Clinical Excellence India Quality Improvement Program (PIQIP) provides valuable data on outpatient CVD quality of care. Collaborative efforts between health professionals are needed to assess further gaps in knowledge and policy makers to utilize new and existing data to drive policy-making.
Keywords: Secondary prevention, Cardiovascular disease, Registries, Quality improvement, India
Abbreviations: ACEi, angiotensin-converting-enzyme-inhibitor; ACS, acute coronary syndrome; ACS QUIK, Acute Coronary Syndromes: Quality Improvement in Kerala; AF, atrial fibrillation; aOR, adjusted Odds Ratio; ARB, angiotensin receptor blocker; BB, beta-blockers; CABG, coronary artery bypass graft; CAD, coronary artery disease; CREATE, Treatment and outcomes of acute coronary syndromes in India; CVD, cardiovascular disease; HR, hazard Ratio; IHRS-AF, Indian Heart Rhythm Society-Atrial Fibrillation; NORIN STEMI, North Indian ST-Segment Elevation Myocardial Infarction; NSTEMI, Non-ST elevation myocardial myocardial infarction; PCI, percutaneous coronary intervention; PINNACLE PIQIP, Practice Innovation and Clinical Excellence India Quality Improvement Program; ROW, rest of the world; STEMI, ST-elevation myocardial infarction; THFR, Trivandrum Heart Failure Registry; TN-STEMI, Tamil Nadu–ST-Segment Elevation Myocardial Infarction
1. Introduction
The epidemic of cardiovascular diseases (CVD) has shifted from high income countries to less industrialized parts of the world. Over three quarters of cardiovascular disease deaths occur in low income countries.1 India is no different, where an estimated 3% of the rural population, and 7% of the urban population has coronary artery disease (CAD).2 Several initiatives have evaluated risk factors, presentation, and management of CVD in India with the aim of reducing morbidity and mortality associated with these diseases.3 Secondary prevention refers to initiatives undertaken with the aim of reducing the impact of CVD on patients who have already been diagnosed with these diseases.
Several studies have suggested that data derived from registries improves the quality of care provided through more detailed information and aggregate experience of other patients in the registry.4, 5, 6 Furthermore, these registries can serve as platforms to deliver and subsequently test initiatives directed toward improving outcomes.7 In this article, we provide a brief overview of some of these initiatives that have specifically focused on secondary prevention of CVDs (Table 1). This review is meant to provide an overview through examination of large, longitudinal registries and cohort studies published in the last 10 years.
Table 1.
A summary of findings from secondary cardiovascular disease prevention registries and epidemiological cohorts in India.
| Initiative Year of Publication | Patient Population; Population size | Key Findings | Limitations |
|---|---|---|---|
| PINNACLE – India Quality Improvement Program (PIQIP)8, 9, 10, 11, 12 2015 |
Patients with coronary artery disease, heart failure, and atrial fibrillation evaluated in the outpatient setting. n > 100,000 | <35% of HFrEF patients had documentation of guideline-directed therapies. Women had lower rates of guideline-directed therapies documented for both, CAD and HF. |
High rate of missing data. |
| Kerala Acute Coronary Syndrome registry13,14 2013 |
Patients presenting to the hospital with acute coronary syndrome (ACS). n = 25,748 | Observed in-hospital mortality for ACS patients was around 8%. <50% of STEMI patients and <30% of non-STEMI/unstable angina patients underwent reperfusion (primary PCI or thrombolytic therapy). |
Possible selection bias (ACS patients included only if survived to be admitted to a coronary care unit) Voluntary participation of hospitals. |
| Acute Coronary Syndromes: Quality Improvement in Kerala (ACS QUIK)15,16 2017 |
Patients presenting to the hospital with acute coronary syndrome (ACS). Control group: n = 10,066 Intervention group: n = 11,308 |
Care of patients with the help of a quality improvement tool kit did not improve all-cause death, reinfarction, stroke, or major bleeding compared with standard care. However, it increased the prescription of optimal in-patient and out-patient medications. | Short-term follow up. |
| CREATE registry17 2008 |
Acute myocardial infarction (STEMI or non-STEMI) or suspected myocardial infarction in patients with prior ischemic heart disease. n = 20,937 | Higher proportion of STEMI cases in India compared with other nations. 30-day mortality 9% for STEMI; 4% for non-STEMI. Mean age of patients with ACS around 10 years younger than the Western world. |
Observational registry. |
| The Tamil Nadu–ST-Segment Elevation Myocardial Infarction (TN-STEMI) Program18 2017 |
Regional system-of-care program for STEMI patients. n = 2420 | Tamil Nadu – STEMI program included a regional system of care intervention through a hub-and-spoke model. Post-intervention: increased rates of coronary angiography, PCI and reduction in 1-year mortality (14.2% vs. 17.6% pre-intervention). |
Heterogeneity between different regions of India may limit ability to scale the hub-and-spoke model to other states. |
| Detection and Management of Coronary Heart Disease (DEMAT) Registry19 2013 |
Patients presenting with ACS at 10 tertiary care centers across 9 cities in India. Data were prospectively collected to compare gender differences in ACS presentation, management, and outcomes. n = 1565 | Women presenting with ACS had comparable in-hospital management, discharge management, and 30-day outcomes compared with men who presented with ACS. | Small sample size, short duration of follow up, convenient sampling and limited clinical endpoints. |
| North Indian ST-Segment Elevation Myocardial Infarction (NORIN STEMI) Registry20 2019 |
All patients >18 years of age presenting with STEMI at two tertiary care hospitals in India .n~3500 (data collected on 558 patients thus far) | 45% of patients presented to the emergency department more than 1 h after symptom onset. More data to follow after further enrollment. |
Two hospitals in New Delhi, limiting generalizability. |
| Prospective observational longitudinal registry of patients with stable coronary artery disease (CLARIFY)21 2017 |
Patients with stable coronary artery disease. n = 1537 | Patients in India were significantly younger than rest of the world and had a higher prevalence of diabetes. Indian patients were also less likely to be on aspirin, statins, and beta-blockers. High LDL-C, low HDL-C was more common in Indian patients. |
Participants were selected from major cities, leading to urban bias. |
| Premature coronary artery disease in India: coronary artery disease in the young (CADY) registry22 2017 | Young patients (men age < 55 years and women age < 65 years) with CAD from 22 centers in India. n = 997 | Conventional risk factors (family history of CAD, hypertension, dyslipidemia, tobacco use, diabetes mellitus) were highly prevalent in these patients. Females were older and had higher burden of comorbidities. | Lack of data on genetic risk factors. |
| Indian Heart Rhythm Society – Atrial Fibrillation (IHRS-AF) registry23 2017 |
Patients with atrial fibrillation. n = 1537 | Mean onset of AF in Indian patients occurs 10 years earlier than in the West. | Possible selection bias (patients primarily recruited from tertiary centers). |
| Trivandrum Heart Failure registry25 2015 |
In-hospital heart failure admissions. n = 1205 | Most common cause of heart failure in this registry was ischemic heart disease accounting for > 70% of cases. 25% of HFrEF patients prescribed guideline-directed therapies at discharge. |
No drug-dosing data. |
ACS: acute coronary syndrome; AF: atrial fibrillation; HDL: high-density lipoprotein; HFrEF: heart failure with reduced ejection fraction; LDL: low-density lipoprotein; NSTEMI: non-ST-elevation myocardial infarction; PCI: percutaneous coronary intervention; STEMI: ST-elevation myocardial infarction.
1.1. PINNACLE (practice innovation and clinical excellence) India quality improvement program (PIQIP)
The PIQIP is India's first outpatient CVD quality improvement program that was initiated in 2011, after validation of the PIQIP tool in an earlier study.8,9 The tool was used to collect and report outpatient CVD performance metrics in patients with CAD, heart failure and AF. The PIQIP has provided data from more than 100,000 patient encounters, from 17 participating centers in 11 different cities (Adoni, Ahmedabad, Anand, Delhi, Hyderabad, Mumbai, Nagpur, Nashik, Patna, Pune, Talegaon).8
One of the earlier reports from the PQIP estimated the prevalence and risk factors of CVD (hypertension, diabetes, dyslipidemia, and current tobacco use) in 68,196 patients.8 The study found the prevalence of CAD, heart failure, and AF to be 14.8%, 4.0%, and 0.5% of patients, respectively. Hypertension, diabetes, current tobacco use, and dyslipidemia were prevalent in 29.7%, 14.9%, 7.6%, and 6.5% of the population, respectively. Self-reported use of medications in eligible CAD patients was 48.6% for aspirin, 37.1% for clopidogrel, and 50.6% for statins. Renin–angiotensin–aldosterone system (RAAS) antagonists and beta-blockers (BB) were used by 61.9% and 58.1% of patients with heart failure, respectively, while only 37.0% of patients with AF were on oral anticoagulation.
This study was followed by a report on the use of guideline-directed medical therapy in heart failure patients.10 The report included 15,870 patients from the PIQIP registry who had an ejection fraction (EF) less than 40%. The authors analyzed documented use of angiotensin converting-enzyme inhibitors (ACEi)/angiotensin receptor blockers (ARBs), BBs or both among outpatients with heart failure and depressed EF. They found that ACEi/ARB, BB, or both were documented in 33.5%, 34.9%, and 29.6% of patients, respectively. The study also noted that the documented use of these medications increased progressively during the course of the study.
Another study from PIQIP evaluated sex disparities in care and access to healthcare in India.11 The study included 31,796 women that were compared with 66,245 men. The study found that women, despite being younger, had a higher co-morbidity burden compared with men with regard to hypertension (62.0% in women vs. 45.6% in men, P ≤ 0.01), diabetes (39.4% vs. 35%, P ≤ 0.01), and hyperlipidemia (3.7% vs. 3.1%, P = 0.19). Women participants on average had fewer encounters (mean = 2.59) compared with men (2.82; P ≤ 0.001) during the study period. Most notably, there was a difference in guideline-directed medication prescriptions. Women with CAD had lower documented rates of aspirin (38% in women vs. 50.4% in men, P ≤ 0.001), aspirin or thienopyridine combination (46.9% vs. 57.2%, P ≤ 0.001), and BB (36.8% vs. 47.8%, P ≤ 0.001) prescriptions compared with men. Women with heart failure with low EF (EF ≤ 40%) also had lower prescription rates of guideline-directed medical therapy compared with men: BB (30.8% vs. 37.0%, P ≤ 0.001), ACEi or ARBs (29.3% vs. 34.9%, P ≤ 0.001), and both (24.6% vs. 31.0%, P ≤ 0.001). Among women with AF and CHADS2 score ≥2, however, more women were on oral anticoagulation compared with men (19.6% vs. 14.6%, P = 0.34), although the use of oral anticoagulants was low for both groups. It is worth noting that the sample size for AF patients was low in this study.
In a recent report, the authors of the PIQIP analyzed the influence of electronic health records (EHR) on the quality of care patients received.12 The study compared documentation of CVD comorbidity burden (hypertension, diabetes mellitus, and hyperlipidemia) in CAD patients between practices with (n = 2 practices) and without (n = 15 practices) integrated and operational EHRs. Documentation of guideline-directed medical therapy for CAD, AF, and heart failure was also compared between these practices. The study found that comorbidity burden in patients with CAD was documented less frequently among practices with EHR — hypertension (49.8% at practices with EHR vs. 52.1% at practices without EHR; P = 0.003), diabetes (34.9% vs. 38.3%; P < 0.001), and hyperlipidemia (0.2 vs. 3.9%; P < 0.001). On the contrary, guideline-directed medical therapy was prescribed more frequently at practices with EHR. In patients with CAD, aspirin (63.2% in practices with EHR vs.17.8% in practices without EHR; P < 0.001), clopidogrel (41.7% vs. 27.4%; P < 0.001), BB (61.4% vs. 9.8%; P < 0.001), and ACEi or ARBs (53.9% vs.16.4%; P < 0.001) were all prescribed more frequently at practices with EHR. Similarly, patients with heart failure received BB (43.8% vs. 10.7%; P < 0.001) and ACEi or ARBs (40.8% vs. 16.1%; P < 0.001) more frequently at practices with EHR. Documentation of warfarin prescription was higher in patients with AF receiving care at practices with EHR (42.5% vs. 26.1%; P < 0.001).
In conclusion, the PIQIP registry demonstrated the feasibility of conducting quality improvement programs in an outpatient cardiovascular setting in India. In addition, it highlighted the suboptimal rates of GDMT, especially in females. It is limited by mostly enrolling sites from urban locations, which makes these results less generalizable to a large part of India. In addition, the study design is only feasible for patients who return to the practices where they were initially evaluated. This results in a significant number of patients being lost to follow-up. In addition, due to the time constraints in a resource-limited setting, data on medication contraindications are not recorded. The generalizability of data is limited by participation of highly-motivated centers. Finally, high cost of medications may have influenced prescription rates of guideline-directed medical therapy. Future directions for the PIQIP registry include inclusion of semi-urban and rural practices and enhanced data capture (e.g., socioeconomic status, data on biomarkers, and contraindication to medications, etc.).
2. Secondary prevention after myocardial infarction
2.1. Kerala acute coronary syndrome (ACS) registry
The Kerala ACS Registry is a prospective registry developed specifically to study trends in presentation, management, and outcomes of patients with ACS in Kerala.13 Data were collected from 25,748 patients with age greater than 18 years who presented with ACS at 125 different hospitals between May 2007 and May 2009.
In its initial report, the registry found that ST-elevation myocardial infarction (STEMI) was the most common presentation (37%), followed by non-ST elevation myocardial infarction (NSTEMI) (31%) and unstable angina (32%; P < 0.001 for difference between the groups).14 A higher proportion of patients with unstable angina had a history of prior diabetes compared with patients who presented with STEMI and non-STEMI (40.7% in unstable angina vs. 37.9% in NSTEMI vs. 34.6% in STEMI), stroke (3.2% vs. 2.2% vs. 2.2%), and percutaneous coronary intervention or coronary artery bypass graft surgery (PCI or CABG) (0.7% vs. 0.1% vs. 0.1%; P < 0.001 for all). On the other hand, history of prior hypertension (40.4% in unstable angina vs. 48.2% in NSTEMI vs. 55.5% in STEMI) and smoking (30.2% vs. 37.9% vs. 35.3%; P < 0.001 for all) was more prevalent among STEMI and non-STEMI patients. Thrombolytics were administered in 41% of patients with STEMI. Approximately 19% of NSTEMI, and 11% of unstable angina admissions inappropriately received thrombolytic therapy. These were more common at low-volume, and non-teaching hospitals. In-hospital antiplatelet use was greater than 90%. Percutaneous coronary intervention rates were marginally higher in STEMI admissions (12.9% in STEMI vs. 11.7% in NSTEMI vs. 10.9% in unstable angina; P < 0.001). Discharge medication rates were variable and generally suboptimal with 76.4% patients discharged on aspirin, 79.4% on clopidogrel, 62.7% on beta-blockers (BB), 70.1% on statins, and 25.5% on ACEi/ARBs.
In another report, differences in presentation, diagnosis and management were compared between men (n = 19,923) and women (n = 5825).13 The study found that women (mean age = 64.4 years) were older than men (mean age = 59.3 years, P < 0.001). A higher proportion of women had a history of prior MI (16% vs. 14%, P < 0.001) but a lower prevalence of hypertension (50% vs. 52%, P = 0.02). There were no major numerical differences in the presentation in terms of chest pain (85% in women vs. 86% in men; P = 0.06), dyspnea (12% vs. 11%; P = 0.006), or left bundle branch block (2% vs. 3%; P = 0.03). Women were more likely, however, to have positive cardiac biomarkers (60% vs. 57%), and to undergo coronary angiography (13% vs. 11%; P < 0.001 for all) compared with men.
In the Acute Coronary Syndromes: Quality Improvement in Kerala (ACS QUIK) study, 63 of the 125 hospitals in the Kerala ACS registry (in addition to 12 government hospitals not in the Kerala ACS registry) were cluster randomized into intervention and usual care groups.15 Hospitals in the intervention group provided care to patients with ACS with the help of a quality improvement tool kit that consisted of audit and feedback, checklists, patient education materials, and linkage to emergency cardiovascular care and quality improvement training. The study showed no difference in the primary outcome (composite of all-cause death, reinfarction, stroke, or major bleeding) between the two groups (5.3% in the intervention group vs. 6.4% in the control group; adjusted Odds Ratio [aOR]: 0.98, 95% CI: 0.80–1.21). There were also no statistically significant differences observed in tobacco cessation advice (96.0% vs. 94.7%; aOR: 1.06, 95% CI: 0.67–1.67); however, optimal in-patient medications (aspirin, adenosine diphosphate receptor antagonist, anticoagulant, and BB) (31.7% vs. 35.8%; aOR: 1.45; 95% CI: 1.28–1.64), and optimal discharge medications (aspirin, adenosine diphosphate receptor antagonist, statin, and BB) (61.8% vs. 64.0%; aOR: 1.61, 95% CI: 1.42–1.82) were higher in the intervention group.
In one study, 27 ACS providers (cardiologists, emergency room physicians, emergency room nurses, coronary care unit nurses, cardiac catheterization laboratory technicians, ambulance paramedics, a hospital administrator, and a state government health policy official) who were part of the ACS QUIK study were interviewed to better understand the facilitators and barriers to prehospital ACS care, and to understand contextual barriers.16 Based on their responses, the study concluded that, (1) patients with ACS often attribute their symptoms to non-cardiac causes; (2) emergency medical services are infrequently utilized in pre-hospital management; (3) the pre-hospital healthcare infrastructure in Kerala is insufficient and leads to pre-hospital delay (4) multiple stops are made (e.g., at a primary health center, a peripheral hospital); before arriving at a facility that can provide definitive diagnosis and treatment, and (5) high cost of healthcare limits health care delivery. The study also noted the potential of mobile health technologies in accelerating the diagnosis and initiation of treatment processes.
The Kerala ACS registry is the largest ACS registry in India to date, and it provides valuable data that is assisting in setting up programs that improve the quality of ACS management in India. The heterogeneity of the Indian population and systemic differences between different geographical regions in India, however, make results from the Kerala ACS registry difficult to generalize to other parts of the nation. Participation in the Kerala ACS registry was voluntary; therefore, the data may not be representative of all inpatient practices in Kerala. Moreover, some of the event rates may be falsely low as data were only limited to patients hospitalized in coronary care units and could not be collected from emergency departments or other inpatient units due to resource constraints.
2.2. Treatment and outcomes of acute coronary syndromes in India (CREATE)
The CREATE registry recruited participants who presented with ACS at 89 hospitals in 50 different Indian cities for a 4-year period ending in 2005.17 Data were prospectively collected on these patients at the time of enrollment and at 30 days. Data collected included baseline clinical characteristics, demographics, medical history, time to reach the hospital, time until thrombolysis, treatments in hospital, outcomes in hospital and at 30 days, and socioeconomic indicators. Mean age of the participants was 57.5 years with 76.4% (n = 15,644) participants being male. Of the 20,468 patients recruited and analyzed, 12,405 patients had STEMI (60.4%), and the median time of presentation was 6 h after symptom onset. Patients who presented with STEMI were more likely to be smokers (34.1% vs. 18.5%) but less likely to have a history of diabetes (26.9% vs. 35.8%), hypertension (31.4% vs. 47.5%), myocardial infarction (11.5% vs. 26.6%), and heart failure (0.8% vs. 1.6%; P < 0.001 for all) compared with patients who did not present with STEMI. Around 97.9% patients received antiplatelet agents on presentation, while 23.2% (21.8% with STEMI and 25.7% with NSTEMI) underwent coronary angiography. Thrombolysis was administered in 58.5% (n = 7261) of STEMI patients. BB, lipid-lowering drugs, and ACEi or ARBs were administered to 59.3%, 52.0%, and 56.8% patients while in the hospital, respectively. At 30 days, death occurred in 8.6% STEMI, and 3.8% in NSTEMI patients. In terms of socioeconomic status, patients classified as “rich” had the highest proportion of known diabetes (40.9%) and hypertension (22.3%), and the lowest proportion of tobacco smoking (32.7%; P < 0.001 for trend for all). They also had the lowest proportion of STEMI (47.3%), but were most likely to undergo coronary angiography (40.9%) and receive PCI (15.3%). Mortality was lowest in the “rich” group (5.5%), and highest in the “poor” group (8.2%). This difference did not correct after adjusting for risk factors and location of infarct.
The strength of the study lies in the inclusion of 50 different cities in India. The study is limited by its observational design. Other indicators such as physical exercise and education may have been confounders that were not evaluated. The study also did not collect data such as medications at discharge and medication adherence at follow-up.
2.3. The Tamil Nadu–ST-Segment Elevation Myocardial Infarction (TN-STEMI) program
The TN-STEMI program is a multicenter, prospective study initiated with the aim of examining and improving access to perfusion and PCI during STEMI.18 The study linked 4 PCI-capable facilities to 35 non-PCI-capable health centers, and a non-profit ambulance service that was capable of acquiring and transmitting electrocardiograms (ECGs) and transporting patients between hospitals. Patients with STEMI were enrolled prior to (n = 898) and after implementation (n = 1522) of the program, and the two groups were compared. Data collected included demographics, medical history, data relating to processes of care (mode of transportation and intervals of onset of chest pain, time of arrival at the hospital, time taken to perform ECG, and time when coronary angiography and/or PCI [if performed]), in-hospital management, and in-hospital outcomes. The study found a significant increase in the proportion of patients that were transferred from non-PCI healthcare centers to PCI-capable health centers after the implementation of the program (3.7% prior to implementation vs. 33.5% after implementation; P < 0 0.001). Time from first medical contact to ECG (7 min vs. 5 min; P = 0.02), and time from ECG to PCI (39.2 min vs. 17.3min; P = 0.003) decreased after the implementation of the program. The implantation also resulted in a greater proportion of STEMI patients undergoing coronary angiography (3.5% vs. 31.3%) and PCI (3.1% vs. 20.6%). In-hospital mortality at non-PCI centers decreased from 7.6% to 6.1% after implementation of the program. The program also resulted in higher rates of antiplatelet agents (59.2% vs. 82.3% for aspirin, 57.6% vs. 64.1% for clopidogrel, 3.7% vs. 15.5% for prasugrel, and 3.2% vs. 11.8% for ticagrelor) and statins (62.6% vs. 76.5%; P < 0.001 for all) being prescribed at discharge.
The findings of the study suggest that a referral model, such as the one proposed in this study, may be the key in a higher proportion of patients with ACS receiving standard of care. The model, however, requires strong partnerships between the primary, secondary, and tertiary care hospitals. The heterogeneity of the healthcare setup in India may limit the applicability of this model.
2.4. Detection and management of coronary heart disease (DEMAT) registry
The DEMAT registry recruited patients who presented with ACS at 10 tertiary care centers across 9 cities in India.19 Data was prospectively collected during the hospitalization, upon discharge, and at 30-day follow-up. A total of 1565 patients suspected to have ACS were enrolled, 334 (21.3%) of whom were women. The study found that women presenting with ACS were older than men (mean age 60.8 years vs. 57.2 years; P < 0.001), and less likely to present with STEMI (38% vs. 55%; P < 0.001) compared with men. Hypertension (62% vs. 42%; P < 0.001) and diabetes (46% vs. 38%; P = 0.01) were more prevalent in women while tobacco use (2% vs. 33%; P < 0.001) was higher in men. Hyperlipidemia (15.6% vs. 15.0%; P = 0.81) and stroke (0.9% vs. 1.5%; P = 0.37) were similar in both groups. In-hospital management was not significantly different between the two groups, with comparable rates of PCI (49.4% vs. 49.0%; P = 0.90) and CABG (5.8% vs. 6.6%; P = 0.61), as well as prescription of aspirin (93.7% vs. 96.1%; P = 0.06), clopidogrel (92.5% vs. 93.7%; P = 0.42), BB (76.4% vs. 79.2%; P = 0.26), and unfractionated or low-molecular weight heparin (52.1% vs. 51.5%; P = 0.85) between the two groups. Thrombolytic therapy was administered less frequently in women than men (16.2% vs. 25.4%; P < 0.01). Management at discharge was found to be similar between both groups with comparable prescription rates of aspirin (94.4% vs. 93.9%; P = 0.74), BB (77.3% vs. 80.0%; P = 0.28), and statins (86.2% vs. 88.5%; P = 0.26) between the two groups. Clopidogrel prescription at discharge was higher in males compared with females (87.2% vs. 91.8%; P = 0.01). At 30 days, death (3.0% vs. 1.8%; aOR: 1.40, 95% CI: 0.62–3.16) and combined outcome of death, rehospitalization, or cardiac arrest at 30 days (13.5% vs. 12.5%; aOR: 1.00, 95% CI: 0.67–1.48) were similar in both groups.
The DEMAT registry was one of the earlier studies that compared outcomes between men and women presenting with ACS. The study, however, is limited by its relatively small sample size and short duration of follow-up.
2.5. North Indian ST-Segment Elevation Myocardial Infarction (NORIN STEMI) registry
The NORIN STEMI registry is a prospective cohort study based in two large, largely cost-free tertiary medical centers in New Delhi, India.20 These institutions are government-funded and allow the inclusion of an underserved population. The goal of the study is to study risk factors (such as hypertension, hyperlipidemia, kidney disease, diabetes mellitus), practice patterns (such as duration from onset of symptoms to presentation and PCI), and prognosis of patients presenting with STEMI at these tertiary care hospitals. The study started enrolling in January 2019 with the goal of enrolling 3500 patients. Data collected from 558 patients were presented in a recent report that showed the median age of the patients to be 55 years, with 34% of patients younger than 50 years of age. Prevalence of hypertension, diabetes mellitus, hyperlipidemia, and current smoking was 29%, 23%, 5%, and 60%, respectively. Of note, 45% of patients presented to the emergency department more than 1 h after symptom onset. The study stands out for providing contemporary data, as well as for describing presentation and practice patterns in two large tertiary care hospitals. While findings from this registry after complete enrollment are awaited, initial findings indicate concerning trends.
3. Prevention of atherothrombosis in stable coronary artery disease
3.1. Prospective observational longitudinal registry of patients with stable coronary artery disease (CLARIFY)
The CLARIFY registry was conducted across 45 geographical regions of the world with the objective to gain information on their demographic characteristics, clinical presentation, and management of CAD.21 Patients in the registry had stable CAD, with at least one of the following: coronary stenosis >50% on coronary angiography; documented myocardial infarction (MI > 3 months ago); chest pain with myocardial ischemia proven using stress electrocardiogram, stress echocardiography, or myocardial imaging; history of CABG or PCI (performed > 3 months ago). One report from this registry compared clinical characteristics, prevalence, and control of risk factors for coronary artery disease between participants in India and the rest of the world (ROW). The study found that patients in India were significantly younger than the ROW (59.6 ± 10.9 years vs. 64.3 ± 10.4 years). Patients from India had a higher prevalence of diabetes (42.9% vs. 28.8%) compared with ROW, but a lower prevalence of family history of premature CAD (21.3% vs. 28.7%), dyslipidemia (63% vs. 75.2%), peripheral artery disease (4.8% vs. 10%), abdominal aortic aneurysm (0.1% vs. 1.6%), and carotid disease (1.8% vs 7.7%). At the time of enrollment, Indian patients were also less likely to be on aspirin (85.6% vs. 87.8%; P = 0.0443), statins (77.9% vs. 90%, P < 0.001), and BB (69.4% vs. 75.4%; P < 0.001). High LDL cholesterol (LDL cholesterol ≥70 mg/dL) (41.6% vs. 31.2%) and low HDL cholesterol (41.6% vs. 31.2%) were more common in Indian patients, while they were also less likely to be obese (27.2% vs. 48.4%) compared with the ROW.
3.2. Premature coronary artery disease in India: coronary artery disease in the young (CADY) registry
The CADY registry is a multi-centric, prospective, observational study that was designed to determine risk factors of premature CAD (men age < 55 years and women age < 65 years) in the Indian population.22 CAD was defined by a positive stress test or a definite imaging technique, or history of prior PCI or CABG. The study was conducted across 22 centers in India and enrolled 997 patients that had a mean age of 49.1 ± 8 years (46.7 ± 7 years in men and 55.1 ± 7 years in women). Around 680 (68%) patients presented with ACS (51% STEMI, 49% NSTEMI). Family history of CAD, hypertension, dyslipidemia, tobacco use, diabetes mellitus, and BMI≥23 were present in 49.4%, 11.4%, 38.6%, 44.2%, and 56.4% of the population, respectively. Diabetes mellitus (62.2% vs. 37.1%) and hypertension (72.1% vs. 40.3%; P < 0.0001 for all) were more prevalent in females with premature CAD compared with males, while tobacco use (52.7% vs. 3.2%; P < 0.001) was more common in males. The study also found that compared with patients without ACS, BB (54.6% vs. 38.7%) and statins (80.8% vs. 63.5%) were more frequently prescribed in patients with ACS. Antiplatelet agents (80.5% vs. 91.8%) and ACEi/ARBs (35.9% vs. 53.3%) were less frequently prescribed in patients with ACS compared with patients without ACS.
The CADY registry was an important initiative that identified risk factors for premature CAD in the Indian population. The study also identified a greater potential for prevention in females given a higher rate of comorbidities. The study was limited by a lack of information on genetic risk factors, that are major contributors to CAD in this specific population.
4. Improving outcomes in patients with heart failure and atrial fibrillation)
4.1. Indian Heart Rhythm Society-Atrial Fibrillation (IHRS-AF) registry
The IHRS-AF was created with the aim of capturing epidemiological data on atrial fibrillation (AF) in India.23 The study prospectively enrolled 1537 patients with AF from 24 inpatient or outpatient settings across 12 cities in India. Data collected included patient demographics, their presentation, associated comorbidities, treatment practices, and 1-year follow-up outcomes. Mean age of the participants was 54.7 ± 15.9 years, 51.5% of whom were female. This was much lower than the age of AF patients in the United States, where median age was 75 years.24 In addition, 47.6% of the participants had rheumatic heart disease. Hypertension, heart failure, and coronary artery disease were present in 31.4%, 18.7%, and 16.2% patients, respectively. At baseline visit, 20.4% patients were diagnosed with paroxysmal AF while 33.0% and 35.1% had persistent and permanent AF, respectively. At one-year follow-up, 45.6% patients were in permanent AF, while only 10.5% and 20.3% continued to have paroxysmal and persistent AF, respectively. Approximately 22.6% patients had no AF at 1 year. Rate control strategy was the mainstay of treatment for 75.3% of patients at baseline visit, and the proportion increased to 79% at 1 year. Approximately 66% patients were successfully rate controlled (heart rate < 90 beats per minute) at 1 year. At 1 year, 1.03% (n = 16) patients had stroke, of which 8 were ischemic (mean INR = 1.85 in these patients), 4 were hemorrhagic, and 2 were undetermined. Of the 100 patients who died at 1 year, the most common cause of death was heart failure (35%), followed by myocardial infarction (14%), sudden cardiac death (12%), and stroke (4%).
The IHRS-AF brings to light that patients with AF in India are younger compared with the West. It also showed a high prevalence of rheumatic heart disease in this population. A major limitation of this study was the selection bias, as a result of patient recruitment from tertiary care centers only. Thus, this may not be a true reflection of the actual incidence and etiology of AF in the community.
4.2. Trivandrum Heart Failure Registry (THFR)
The THFR was designed to evaluate the presentation, clinical management, and outcomes of patients with heart failure in Trivandrum, an urban district in Kerala, India.25 All 18 hospitals in the district were enrolled. Data were collected on patients admitted with heart failure at these hospitals through questionnaires, and these patients were followed at 90 days either through outpatient visits or phone. Of the 1209 patients who were enrolled in the registry, 834 (69%) were male. Most common etiology of heart failure was ischemic heart disease (72%), followed by dilated cardiomyopathy (13%) and rheumatic heart disease (8%). Mean duration of hospital stay was 6 days (IQR 4–9 days), and nearly all patients (94%) received diuretics. BB, ACEi/ARBs and aldosterone antagonists were prescribed to 54%, 46%, and 44% patients, respectively. Only 19% patients with left ventricular systolic dysfunction (defined by investigators as EF<45%) were on guideline-directed medical therapy (combination of BB, ACEi or ARB, and aldosterone receptor blockers) during hospital stay, while 25% were prescribed guideline-directed medical therapy at discharge. At 30 and 90 days, mortality was 12.5% and 18.1%, respectively. Compared with patients who did not receive guideline-directed medical therapy, patients who received guideline-directed medical therapy had lower mortality rates (HR:0.28, 95% CI: 0.14–0.53; P < 0.001). Older age (age>55) (hazard ratio [HR]: 1.50, 95% CI: 1.05–2.15), New York Heart Association Class IV symptoms (HR: 1.60, 95% CI: 1.18–2.16), less than primary education (HR: 1.82; 95% CI: 1.04–3.17), and decreased renal function (HR: 1.22, 95% CI: 0.82–1.52; P < 0.05 for all) were associated with higher mortality rates at 90 days.
The study highlights low prescription rates of guideline-directed medical therapy in this population. The study also identified younger age, male sex, and ischemic heart disease to be associated with heart failure. It is, however, limited by a lack of information on medication dosages, and the inability to infer causality due to the observational nature of the study. Moreover, as this was a hospital-based study, many cases who did not present in an inpatient setting, would have been excluded.
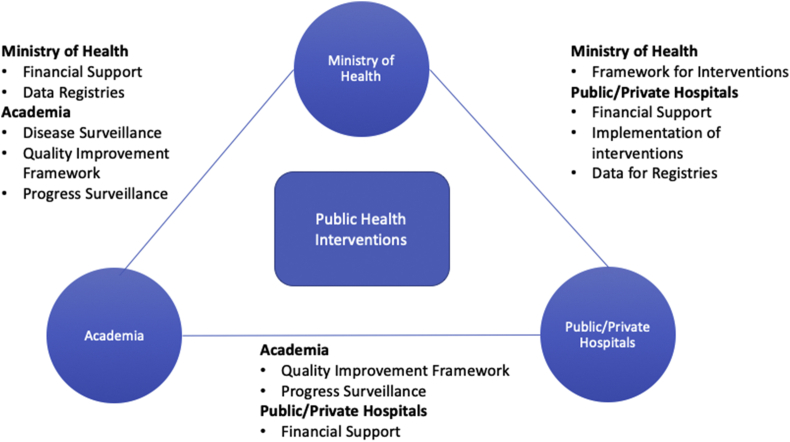
In summary, data suggest that patients presenting with CVD in India are younger, and have a higher burden of CVD risk factors. In addition, there is a suboptimal rate of guideline recommended management. Recommendations from local health professional societies should emphasize on a greater push for primary prevention, perhaps at younger ages, given the higher risk of premature CAD. Efforts also need to be made to identify deficiencies in practices and to drive system-level interventions to provide better patient care. These objectives require collaborative efforts between health professionals in government, private and academic settings that use these data to drive policy-making. We propose one such model in Fig. 1 where we assign the Health Ministry to provide a framework for interventions to public/private hospitals, which in return are responsible for implementation of these initiatives as well providing financial support for these interventions. Similarly, academia is responsible for providing quality improvement frameworks, and monitoring progress of health interventions in exchange for data and financial support from hospitals and the Health Ministry.
Fig. 1.
Potential framework for collaboration between academia, ministry of health and public/private hospitals.
5. Conclusion
The CVD epidemic in India requires urgent attention. Review of data suggests that patients presenting for secondary prevention in India are younger and have a higher burden of CVD risk factors. There is a need for collaborative efforts between health professionals in government, private and academic settings to assess gaps in knowledge and use these data to drive policy-making.
Declaration of competing interest
Dr. Deepak L. Bhatt discloses the following relationships - Advisory Board: Cardax, CellProthera, Cereno Scientific, Elsevier Practice Update Cardiology, Level Ex, Medscape Cardiology, PhaseBio, PLx Pharma, Regado Biosciences; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care, TobeSoft; Chair: American Heart Association Quality Oversight Committee; Data Monitoring Committees: Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Cleveland Clinic (including for the ExCEED trial, funded by Edwards), Contego Medical (Chair, PERFORMANCE 2), Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi Sankyo), Population Health Research Institute; Honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Vice-Chair, ACC Accreditation Committee), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim; AEGIS-II executive committee funded by CSL Behring), Belvoir Publications (Editor in Chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees, including for the PRONOUNCE trial, funded by Ferring Pharmaceuticals), HMP Global (Editor in Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), K2P (Co-Chair, interdisciplinary curriculum), Level Ex, Medtelligence/ReachMD (CME steering committees), MJH Life Sciences, Population Health Research Institute (for the COMPASS operations committee, publications committee, steering committee, and USA national co-leader, funded by Bayer), Slack Publications (Chief Medical Editor, Cardiology Today’s Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), WebMD (CME steering committees); Other: Clinical Cardiology (Deputy Editor), NCDR-ACTION Registry Steering Committee (Chair), VA CART Research and Publications Committee (Chair); Research Funding: Abbott, Afimmune, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Cardax, Chiesi, CSL Behring, Eisai, Ethicon, Ferring Pharmaceuticals, Forest Laboratories, Fractyl, Idorsia, Ironwood, Ischemix, Lexicon, Lilly, Medtronic, Pfizer, PhaseBio, PLx Pharma, Regeneron, Roche, Sanofi Aventis, Synaptic, The Medicines Company; Royalties: Elsevier (Editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease); Site Co-Investigator: Biotronik, Boston Scientific, CSI, St. Jude Medical (now Abbott), Svelte; Trustee: American College of Cardiology; Unfunded Research: FlowCo, Merck, Novo Nordisk, Takeda.
Dr. Salim S. Virani is supported by grant support from the American Heart Association, the American Diabetes Association, Baylor Global Initiatives, and the Department of Veterans Affairs. Honorarium: American College of Cardiology (Associate Editor for Innovations, ACC.org).
References
- 1.World Health Organization. Cardiovascular Diseases (CVDs): Key Facts [Internet]. http://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
- 2.Rao K.D., Bhatnagar A., Murphy A. Socio-economic Inequalities in the Financing of Cardiovascular & Diabetes Inpatient Treatment in India. Indian J Med Res. 2011;133:57–63. Internet. India: Medknow Publications. [PMC free article] [PubMed] [Google Scholar]
- 3.Kalra A., Bhatt D.L., Rajagopalan S. Overview of coronary heart disease risk initiatives in south asia. Curr Atherosclerosis Rep. 2017;19(6):25. doi: 10.1007/s11883-017-0662-1. [DOI] [PubMed] [Google Scholar]
- 4.Jacobson J.O., Neuss M.N., McNiff K.K. Improvement in oncology practice performance through voluntary participation in the Quality Oncology Practice Initiative. J Clin Oncol. 2008;26(11):1893–1898. doi: 10.1200/JCO.2007.14.2992. [DOI] [PubMed] [Google Scholar]
- 5.Schwamm L.H., Fonarow G.C., Reeves M.J. Get with the Guidelines-Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation. 2009;119(1):107–115. doi: 10.1161/CIRCULATIONAHA.108.783688. [DOI] [PubMed] [Google Scholar]
- 6.Raval M.V., Bentrem D.J., Eskandari M.K. The role of surgical champions in the American College of surgeons national surgical quality improvement program--a national survey. J Surg Res. 2011;166(1):e15–e25. doi: 10.1016/j.jss.2010.10.036. [DOI] [PubMed] [Google Scholar]
- 7.Gliklich R.E., Dreyer N.A., Leavy M.B., editors. Registries for Evaluating Patient Outcomes: A User's Guide [Internet] 3rd ed. Agency for Healthcare Research and Quality (US); Rockville (MD): 2014 Apr 22. Quality Improvement Registries. [PubMed] [Google Scholar]
- 8.Kalra A., Pokharel Y., Hira R.S. Cardiovascular disease performance measures in the outpatient setting in India: insights from the American College of cardiology's PINNACLE India quality improvement program (PIQIP) J Am Heart Assoc England. 2015;4 doi: 10.1161/JAHA.115.001910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kalra A., Glusenkamp N., Anderson K. American College of Cardiology (ACC)’s pinnacle India quality improvement program (PIQIP)-Inception, progress and future direction: a report from the PIQIP investigators. Indian Heart J India. 2016;68(Suppl 3):S1–S4. doi: 10.1016/j.ihj.2016.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pokharel Y., Wei J., Hira R.S. Guideline-directed medication use in patients with heart failure with reduced ejection fraction in India: American College of cardiology's PINNACLE India quality improvement program. Clin Cardiol United States. 2016;39:145–149. doi: 10.1002/clc.22519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalra A., Pokharel Y., Glusenkamp N. Gender disparities in cardiovascular care access and delivery in India: insights from the American College of cardiology's PINNACLE India quality improvement program (PIQIP) Int J Cardiol Netherlands. 2016;215:248–251. doi: 10.1016/j.ijcard.2016.04.058. [DOI] [PubMed] [Google Scholar]
- 12.Kalra A., Bhatt D.L., Wei J. Electronic Health Records and Outpatient Cardiovascular Disease Care Delivery: Insights from the American College of Cardiology's PINNACLE India Quality Improvement Program (PIQIP) Indian Heart J. 2018 doi: 10.1016/j.ihj.2018.03.002. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohanan P.P., Mathew R., Harikrishnan S. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J England. 2013;34:121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel A., Vishwanathan S., Nair T. Sex differences in the presentation, diagnosis, and management of acute coronary syndromes: findings from the Kerala-India ACS registry. Glob Heart England. 2015;10:273–280. doi: 10.1016/j.gheart.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huffman M.D., Mohanan P.P., Devarajan R. Effect of a quality improvement intervention on clinical outcomes in patients in India with acute myocardial infarction: the ACS QUIK randomized clinical trial. J Am Med Assoc. 2018;319(6):567–578. doi: 10.1001/jama.2017.21906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel A., Mohanan P.P., Prabhakaran D., Huffman M.D. Pre-hospital acute coronary syndrome care in Kerala, India: a qualitative analysis. Indian Heart J India. 2017;69:93–100. doi: 10.1016/j.ihj.2016.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xavier D., Pais P., Devereaux P.J. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. England. [DOI] [PubMed] [Google Scholar]
- 18.Alexander T., Mullasari A.S., Joseph G. A system of care for patients with ST-segment elevation myocardial infarction in India: the Tamil Nadu-ST-segment elevation myocardial infarction program. JAMA Cardiol United States. 2017;2:498–505. doi: 10.1001/jamacardio.2016.5977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pagidipati N.J., Huffman M.D., Jeemon P., Gupta R., Negi P. Association between gender, process of care measures, and outcomes in ACS in India: results from the detection and management of coronary heart disease (DEMAT) registry. PloS One. 2013;8(4) doi: 10.1371/journal.pone.0062061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arora S., Qamar A., Gupta P. Design and rationale of the North Indian ST-segment elevation myocardial infarction registry: a prospective cohort study. Clin Cardiol. 2019;42(12):1140–1146. doi: 10.1002/clc.23278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.KauL U., Natrajan S., Dalal J., Saran R.K. Prevalence and control of cardiovascular risk factors in stable coronary artery outpatients in India compared with the rest of the world: an analysis from international CLARIFY registry. Indian Heart J India. 2017;69:447–452. doi: 10.1016/j.ihj.2017.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iyengar S.S., Gupta R., Ravi S. Premature coronary artery disease in India: coronary artery disease in the young (CADY) registry. Indian Heart J. 2017;69(2):211–216. doi: 10.1016/j.ihj.2016.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vora A., Kapoor A., Nair M. Clinical presentation, management, and outcomes in the Indian heart Rhythm society-atrial fibrillation (IHRS-AF) registry. Indian Heart J India. 2017;69:43–47. doi: 10.1016/j.ihj.2016.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feinberg W.M., Blackshear J.L., Laupacis A., Kronmal R., Hart R.G. Prevalence, age distribution, and gender of patients with atrial fibrillation: analysis and implications. Arch Intern Med. 1995;155(5):469–473. doi: 10.1001/archinte.1995.00430050045005. [DOI] [PubMed] [Google Scholar]
- 25.Harikrishnan S., Sanjay G., Anees T. Clinical presentation, management, in-hospital and 90-day outcomes of heart failure patients in Trivandrum, Kerala, India: the Trivandrum Heart Failure Registry. Eur J Heart Fail England. 2015;17:794–800. doi: 10.1002/ejhf.283. [DOI] [PubMed] [Google Scholar]