Abstract
This cohort study examines trends in the use of telemedicine and in-person outpatient visits in 2020 among a national sample of 16.7 million individuals with commercial or Medicare Advantage insurance.
The coronavirus disease 2019 (COVID-19) pandemic has dramatically altered patterns of health care delivery in the US. In the context of declining in-person outpatient visits, many clinicians began using telemedicine for the first time, spurred in part by regulatory changes that expanded public and private insurer reimbursement for a wider range of telemedicine services.1,2 To understand how telemedicine compensated for declining outpatient volume and geographic variation in changing patterns of outpatient care, we examined telemedicine and in-person outpatient visits in 2020 among a national sample of 16.7 million individuals with commercial or Medicare Advantage insurance.
Methods
We used insurance claims from the OptumLabs Data Warehouse3 to capture all outpatient visits over a 24-week period from January 1, 2020, to June 16, 2020. We included enrollees with 12 months of continuous enrollment (July 2019-June 2020). We assessed data completeness using weekly childbirth rates (eAppendix in the Supplement). We defined outpatient visits as Medicare’s list of Common Procedural Terminology (CPT) codes eligible for telemedicine4 and telemedicine visits via modifier codes GT, GQ, or 95 or CPT codes 99441-99443.
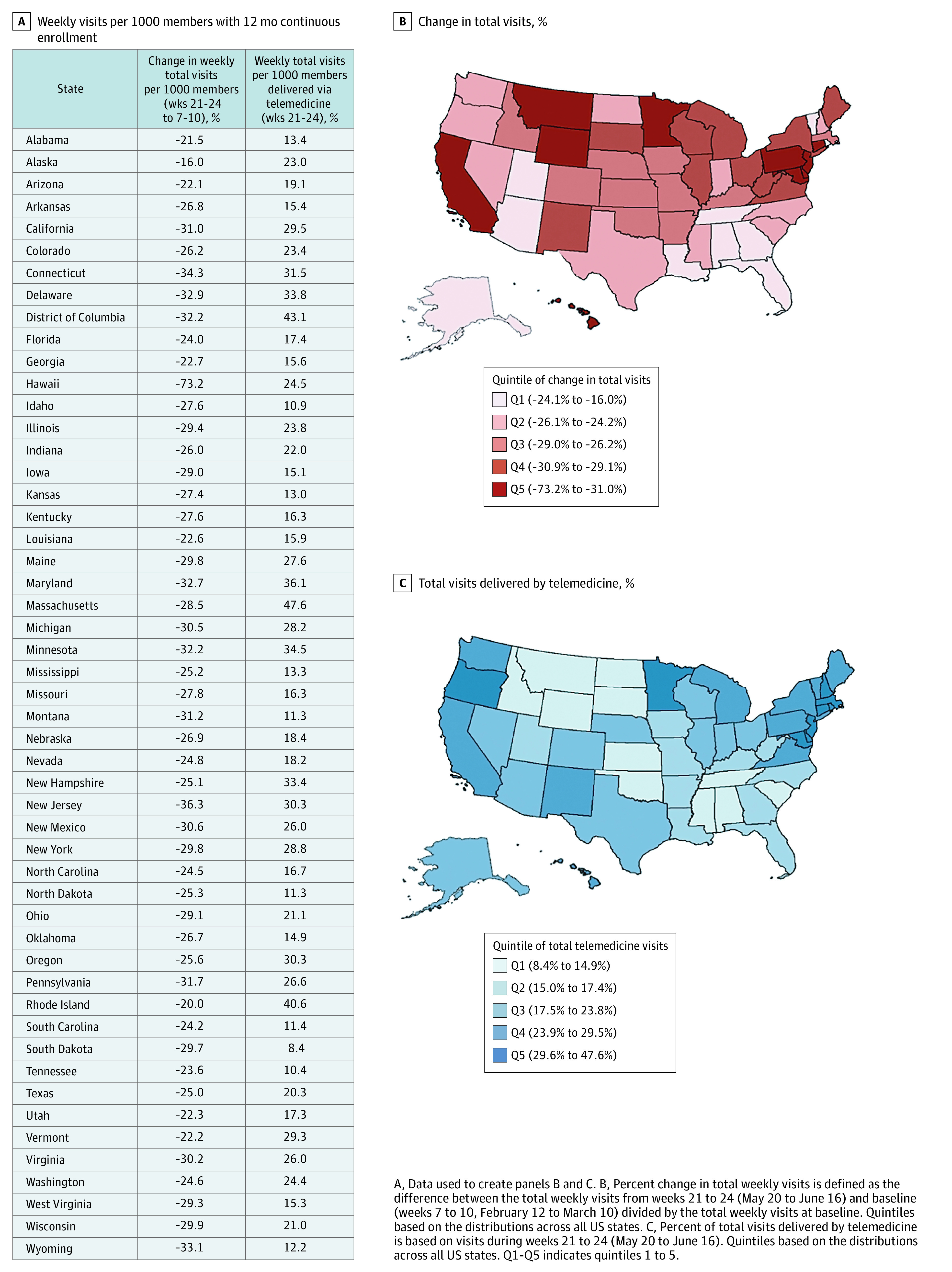
We assessed changes in outpatient visit volume by capturing weekly rates per 1000 enrollees of telemedicine, in-person, and total visits over the study period. For each state, during the final 4 weeks of the study period (May 20 to June 16), we calculated the percent of total weekly visits delivered by telemedicine and the percent change in total weekly visits compared to the 4 week period preceding expansion of telehealth coverage by Medicare (February 12 to March 10).5 The Harvard Medical School institutional review board exempted this study from review and informed consent because all data were deidentified.
Results
Among 16 740 365 enrollees, the weekly rate of telemedicine visits increased during the pandemic period, peaking in the week of April 15, 2020, before declining by the week of June 10, 2020 (Figure 1). From the weeks of January 1 to June 10, the rates for telemedicine visits increased from 0.8 to 17.8 visits per 1000 enrollees (increase of 17.0 or 2013% change); in-person visits dropped from 102.7 to 76.3 (decrease of 26.4 or −30.0% change); total visits (telemedicine and in-person visits combined) decreased from 103.5 to 94.1 (−9.1% change).
Figure 1. Trends in In-Person, Telemedicine, and Total (In-Person Plus Telemedicine) Visits per Week During the Pre–COVID-19 and COVID-19 Periods, January 1, 2020, to June 16, 2020a.
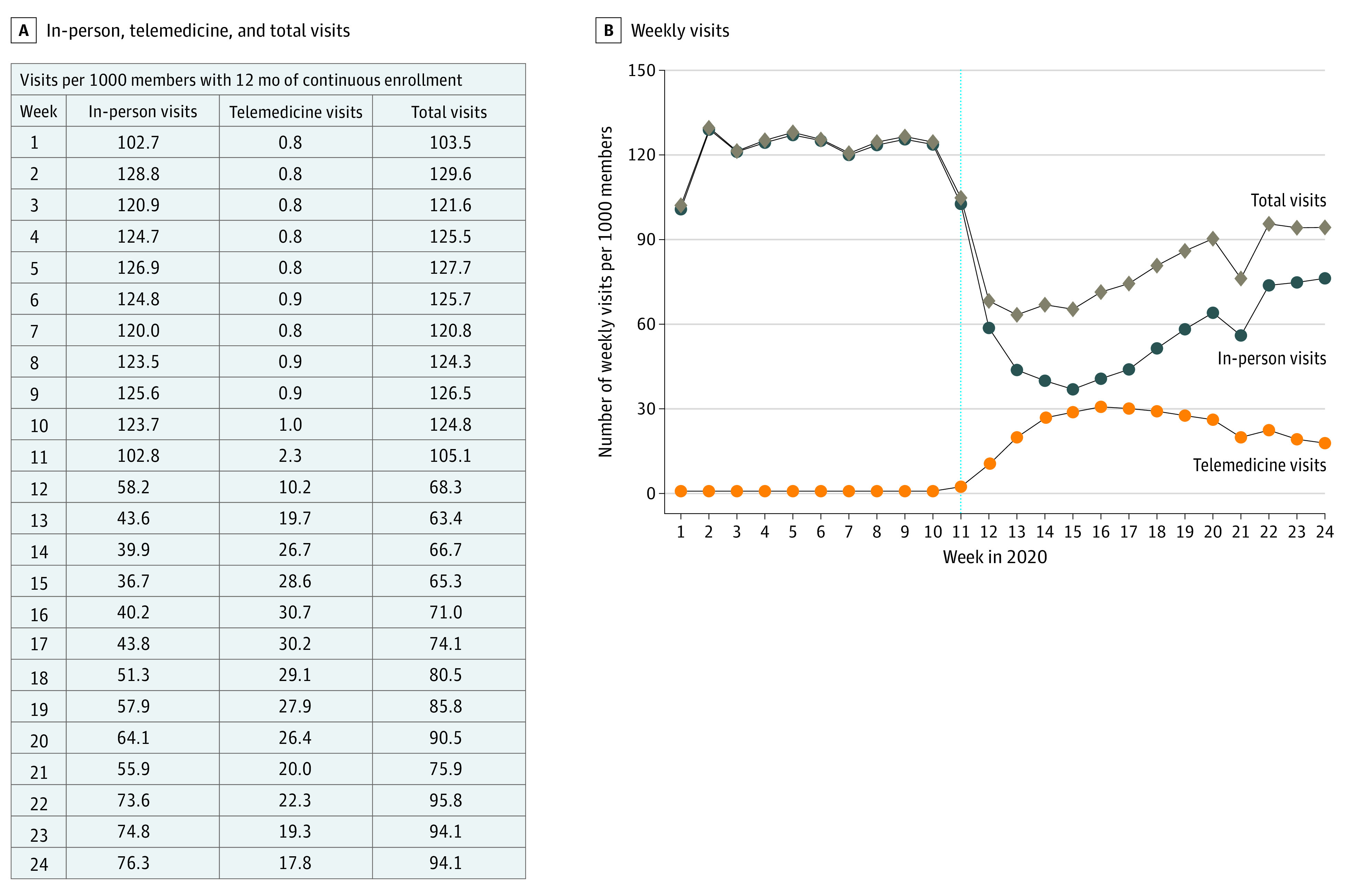
The dotted vertical line in panel B indicates the week of March 17, 2020, (week 11), when Medicare expanded reimbursement for telemedicine visits due to the COVID-19 pandemic.4
aWeek 21 (May 20 to May 26, 2020) includes Memorial Day, a federal holiday in the US. The work week was likely 4 days for many practices resulting in a decrease in visit volume.
By the last 4 weeks of the study period, May 20 through June 16, there was wide geographic variation in the percent of total visits delivered by telemedicine (ranging from 8.4% in South Dakota to 47.6% in Massachusetts) and the percent change from baseline in total visit rates (ranging from −73.2% in Hawaii to −16.0% in Alaska) (Figure 2). Some states, especially in the South, had a small decline in total visits and lower rates of telemedicine use (ie, Tennessee, −23.6% change in total visits with 10.4% of all visits as telemedicine; Alabama, −21.5% and 13.4%, respectively).
Figure 2. US Geographic Variation in the Percent Change in Total Visits and Percent of Total Visits Delivered by Telemedicine From May 20 to June 16, 2020.
Discussion
In this national study of a commercially insured population, growth in telemedicine use offset roughly two-thirds of the decline in in-person visit volume during the COVID-19 pandemic. Although there was geographic variation in the magnitude of changes, every state experienced a drop in total visits, illustrating the broad scope of deferred care during the first months of COVID-19. Although some deferred care may have represented discretionary care that could be postponed without harm, these results also substantiate concerns that patients may fall behind in chronic illness management or face complications from deferred acute medical issues. This would be consistent with evidence from natural disasters resulting in decreased access to care associated with greater morbidity and mortality not directly related to the disaster itself.6
An important limitation is that results may not generalize to other populations (eg, traditional Medicare or Medicaid). Telemedicine use during the early COVID-19 pandemic only partially offset a drop in total outpatient care.
eAppendix
References
- 1.Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. The impact of the COVID-19 pandemic on outpatient visits: practices are adapting to the new normal. Commonwealth Fund. Published June 25, 2020. Accessed July 15, 2020. https://www.commonwealthfund.org/publications/2020/jun/impact-covid-19-pandemic-outpatient-visits-practices-adapting-new-normal.
- 2.Verma S. Early impact of CMS expansion of Medicare telehealth during COVID-19. Health Aff Blog. Published July 15, 2020. Accessed July 16, 2020. https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/
- 3.OptumLabs . OptumLabs and OptumLabs Data Warehouse (OLDW) Descriptions and Citation. Eden Prairie, MN: n.p., May 2019. PDF. Reproduced with permission from OptumLabs. https://www.optumlabs.com/
- 4.Centers for Medicare & Medicaid Services . President Trump expands telehealth benefits for Medicare beneficiaries during COVID-19 outbreak. Newsroom. Published March 17, 2020. https://www.cms.gov/newsroom/press-releases/president-trump-expands-telehealth-benefits-medicare-beneficiaries-during-covid-19-outbreak.
- 5.Centers for Medicare & Medicaid Services . List of telehealth services. Updated April 30, 2020. Accessed July 15, 2020. https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes.
- 6.Baum A, Barnett ML, Wisnivesky J, Schwartz MD. Association between a temporary reduction in access to health care and long-term changes in hypertension control among veterans after a natural disaster. JAMA Netw Open. 2019;2(11):e1915111-e1915111. doi: 10.1001/jamanetworkopen.2019.15111 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix


