Key Points
Question
What is the association of health care use and outcomes with the loss of a primary care physician?
Findings
In this cohort study of 359 470 Medicare beneficiaries who visited a primary care physician from 2008 to 2017, the loss of a primary care physician was associated with decreased use of primary care; increased use of specialty, urgent, and emergency department care; and increased spending (especially for patients of physicians in solo practice).
Meaning
Interrupting primary care relationships could have a negative association with health outcomes and future engagement with primary care.
Abstract
Importance
Disruptions of continuity of care may harm patient outcomes, but existing studies of continuity disruption are limited by an inability to separate the association of continuity disruption from that of other physician-related factors.
Objectives
To examine changes in health care use and outcomes among patients whose primary care physician (PCP) exited the workforce and to directly measure the association of this primary care turnover with patients’ health care use and outcomes.
Design, Setting, and Participants
This cohort study used nationally representative Medicare billing claims for a random sample of 359 470 Medicare fee-for-service beneficiaries with at least 1 PCP evaluation and management visit from January 1, 2008, to December 31, 2017. Primary care physicians who stopped practicing were identified and matched with PCPs who remained in practice. A difference-in-differences analysis compared health care use and clinical outcomes for patients who did lose PCPs with those who did not lose PCPs using subgroup analyses by practice size. Subgroup analyses were done on visits from January 1, 2008, to December 31, 2017.
Exposure
Patients’ loss of a PCP.
Main Outcomes and Measures
Primary care, specialty care, urgent care, emergency department, and inpatient visits, as well as overall spending for patients, were the primary outcomes. Receipt of appropriate preventive care and prescription fills were also examined.
Results
During the study period, 9491 of 90 953 PCPs (10.4%) exited Medicare. We matched 169 870 beneficiaries whose PCP exited (37.2% women; mean [SD] age, 71.4 [6.1] years) with 189 600 beneficiaries whose PCP did not exit (36.9% women; mean [SD] age, 72.0 [5.0] years). The year after PCP exit, beneficiaries whose PCP exited had 18.4% (95% CI, −19.8% to −16.9%) fewer primary care visits and 6.2% (95% CI, 5.4%-7.0%) more specialty care visits compared with beneficiaries who did not lose a PCP. This outcome persisted 2 years after PCP exit. Beneficiaries whose PCP exited also had 17.8% (95% CI, 6.0%-29.7%) more urgent care visits, 3.1% (95% CI, 1.6%-4.6%) more emergency department visits, and greater spending ($189 [95% CI, $30-$347]) per beneficiary-year after PCP exit. These shifts were most pronounced for patients of exiting PCPs in solo practice, whose beneficiaries had 21.5% (95% CI, −23.8% to −19.3%) fewer primary care visits, 8.8% (95% CI, 7.6%-10.0%) more specialty care visits, 4.4% more emergency department visits (95% CI, 2.1%-6.7%), and $260 (95% CI, $12-$509) in increased spending.
Conclusions and Relevance
Loss of a PCP was associated with lower use of primary care and increased use of specialty, urgent, and emergency care among Medicare beneficiaries. Interrupting primary care relationships may negatively impact health outcomes and future engagement with primary care.
This cohort study uses nationally representative 2008-2017 Medicare billing claims to examine changes in health care use and outcomes among patients whose primary care physician exited the workforce and to directly measure the association of primary care turnover with patients’ health care use and outcomes.
Introduction
Continuity of care, a core principle of high-quality primary care, is associated with improved quality of care1,2,3,4,5 and patient outcomes,6,7,8,9,10 including greater delivery of preventive services and lower rates of hospitalization and emergency department visits, as well as lower costs of care for chronic illness.8,9,10 Based on this evidence, strengthening the relationship between patients and primary care physicians (PCPs) has been a centerpiece of delivery reform efforts targeting high-cost and uncoordinated care. Medicare’s Accountable Care Organization programs revolve around PCPs managing the continuum of patient care, while multiple other Medicare payment demonstrations have focused on enhancing continuity of care through primary care teams, with PCPs as team leaders.11,12
It stands to reason that these benefits may be negated by a disruption in the continuity of care. One such disruption is the loss of a PCP, which may affect patients’ access to care, health outcomes, and coordination of care.13,14,15,16 Many patients lose their PCP every year through mechanisms such as physician relocation, retirement, physician death, noncompete agreements, or insurance coverage changes. In one study of a large Accountable Care Organization, PCP relocation, retirement, or death was the dominant factor associated with the reassignment of approximately one-third of Medicare beneficiaries to a new Accountable Care Organization every year.17 Patients’ potential loss of a PCP will become more relevant as an increasing number of PCPs near retirement; since 1975, the number of practicing physicians older than 65 years has increased by more than 274%.18 Disruptions to patients’ primary care may be particularly relevant for patients of physicians in solo practice: such patients may face larger barriers to reestablishing care once their PCP exits the workforce because they are less likely to have preexisting relationships with other PCPs at the clinic.19
Prior evidence on the loss of a PCP has found mixed results on quality and satisfaction, although this evidence also has methodological limitations.20,21,22,23,24 Most existing studies have focused on populations in single geographical areas or single health systems, while another study24 used only aggregate data on physician turnover within managed care plans. One study examined quality and satisfaction outcomes in a large national sample of patients with exiting PCPs in the Veterans Health Administration health system but did not evaluate patient outcomes, such as emergency department visits or health care use.22 To our knowledge, little existing literature on the loss of PCP continuity has used quasi-experimental methods, such as difference-in-differences or event study designs, to examine health care use or patient outcomes after the loss of a PCP.
To address this evidence gap, we used national data on Medicare beneficiaries from 2008 to 2017 to analyze changes in beneficiary health care use and health outcomes after the loss of a PCP and whether this association differed for beneficiaries of PCPs in solo vs group practices.
Methods
Data Source and Study Population
This cohort study used Medicare administrative claims data for a 20% random sample of continuously enrolled, fee-for-service beneficiaries. For the main study sample as well as subgroup analyses, we included beneficiaries visiting a PCP for at least 1 evaluation and management visit from January 1, 2008, to December 31, 2017. We then limited the study sample to PCPs who treated 30 or more Medicare beneficiaries during a 1-year period and their patients. The institutional review board at the National Bureau of Economic Research approved the study and determined that the study did not meet the definition of human research; therefore, no consent was sought from study participants.
For information on physician characteristics, we linked claims data to the Medicare Data on Provider Practice and Specialty database as well as publicly available National Plan and Provider Enumeration System and Physician Compare data (covering active health care professionals from 2014 to 2018).
Identification of PCPs Who Exited Medicare
We defined PCPs as physicians with a listed specialty of family medicine, general practice, geriatric medicine, internal medicine, preventive medicine, pediatrics (many of whom have board certifications in internal medicine [eMethods 1 in the Supplement]), or obstetrics and gynecology (commonly used as PCPs by women).25 We classified all other physicians as specialists.
The study’s main exposure was the exit of a PCP, defined as occurring when a PCP left the workforce entirely (eg, because of retirement, moving to a nonclinical position, or death). We defined the date of exit as the last month a PCP billed Medicare for office-based services with no subsequent Medicare services recorded. To ensure that we could observe a sufficient preperiod, PCPs who practiced at the same practice for less than 2 years before exiting were excluded from the study sample. The study sample also excluded beneficiaries who lost a PCP from 2016 to 2017 because the sample period restricted our ability to follow up with beneficiaries 2 years after PCP exit. As such, the period used to identify PCP exits was from 2010 to 2015 (eMethods 1 and eFigure 1 in the Supplement). We defined PCPs practicing at the same practice for at least 4 years to be nonexiting PCPs. Tax Identification Numbers and 9-digit zip codes defined practices in Medicare claims.
Identification of Control PCPs and Patient Attribution
We matched exiting PCPs to a single nonexiting PCP (1 to 1) using coarsened exact matching, a nonparametric method that matches units either exactly or on “coarsened” bins of characteristics (see eTable 6 in the Supplement for a comparison).26 We chose variables that were not associated with beneficiary outcomes or time-varying characteristics to minimize the potential for regression to the mean.27 We then chose bin sizes to maximize balance between exiting and nonexiting PCPs and to minimize sample attrition. For this application of coarsened exact matching, we matched exiting and nonexiting PCPs exactly on sex, PCP age in 4 bins, practice size in 5 bins, and the monthly number of unique beneficiaries seen in 10 bins (ie, caseload), with all variables defined as of 24 months prior to the departure (eMethods 1 and eTable 1 in the Supplement). We then assigned nonexiting PCPs to a synthetic exit date determined by the exit date of the matched, exiting PCP.
We attributed beneficiaries to PCPs by determining the beneficiaries who visited exiting or nonexiting PCPs 12 to 24 months before the actual or synthetic exit date, respectively (eFigure 3 in the Supplement). Each beneficiary was attributed to the PCP providing the plurality of evaluation and management visits 12 to 24 months before exiting, with ties broken randomly.28 This left a random sample of 359 470 Medicare fee-for-service beneficiaries.
Outcome Measures
First, we measured beneficiaries’ annual rate of outpatient visits to primary care and specialty care physicians, as well as visits to outpatient urgent care centers, defined as outpatient visits with urgent care facility revenue center codes. Second, we measured hospital use, defined as inpatient admissions and emergency department visits, identified by the presence of claims billed with emergency department–specific revenue center codes or place-of-service codes. Third, we assessed changes in medication use using Medicare Part D prescription data to estimate total annual prescription fills signed by primary care and specialty care physicians. We also focused on total prescription fills for a subset of medications for chronic illnesses frequently managed in primary care settings (depression, diabetes, hypertension, and hypercholesterolemia). Fourth, we assessed changes in receipt of preventive care, including influenza vaccination and a composite measure of the total count of preventive screenings for cholesterol, tobacco use, depression, breast cancer, and colorectal cancer.29 Finally, we assessed changes in mortality (using the Medicare Beneficiary Summary File) and total Medicare spending.
Covariates
We obtained beneficiary demographic and enrollment information from Medicare Beneficiary Summary Files. We classified clinical risk with the Elixhauser index using a beneficiary’s entire set of diagnosis codes during the baseline period, defined as 12 to 24 months before PCP exit.30 Primary care physicians were classified as working in solo practices (vs group practices) based on whether the PCP was the only physician (vs one of several) billing under the practice’s associated Tax Identification Number.
Statistical Analysis
To examine the association between PCP exit from Medicare and beneficiaries’ health care use and health outcomes, we conducted a difference-in-differences analysis using multivariable linear regression at the PCP-month level. We compared outcomes for beneficiaries whose PCP exited (exposed beneficiaries) vs a matched sample of beneficiaries whose PCPs did not exit (unexposed beneficiaries), both of whom had respectively assigned exit dates as already described. The key variables in each model were a set of interaction terms between indicators for month or year relative to exit (ie, −24 to 24 months) and an indicator for whether a PCP was in the group that exited. Each of these interaction terms describes the mean differential change in the outcome for patients of PCPs who exited relative to matched control PCPs who did not exit relative to 24 months before exit. To adjust for all observable and unobservable time-invariant differences between exposed and unexposed beneficiaries, all regression models included PCP fixed effects,27 a standard approach with models of panel data.31 Models also included fixed effects for relative month or year. Other controls were not included in the models because they were accounted for in the matching process and by the PCP fixed effects.
Regression analyses were weighted by the size of a PCP’s caseload 12 to 24 months before the departure to give greater weight to PCPs with larger attributed panels. We clustered analyses at the matched PCP pair level to ensure that SEs were asymptotically valid.32 Modeled pretrends of exposed and unexposed beneficiaries’ health care use and health outcomes did not systematically differ prior to PCP exit (eMethods 2 in the Supplement).
We assessed the robustness of findings to alternative specifications and definitions. eTable 7 in the Supplement compares practices with 1, 2 to 4, and ≥5 PCPs, and eTable 8 in the Supplement includes clinics with more than 100 PCPs. Results in eTable 9 in the Supplement are adjusted for the hospital referral region, results in eTable 10 in the Supplement are adjusted for whether the beneficiary resided in an urban or rural location, and results in eTable 11 in the Supplement remove PCP caseload from the match. Additional methods are presented in eMethods 4 in the Supplement. Because spending may be affected by outliers, we also evaluated the sensitivity of spending using log-transformed outcomes (eTable 5 in the Supplement).
Analyses were performed in Stata, version 15 (StataCorp LLC). The 95% CI around reported estimates reflects 0.025 in each tail, or P ≤ .05.
Results
Study Population
Overall, 90 953 PCPs billed services for 30 or more Medicare beneficiaries from 2008 to 2017, of whom 9491 (10.4%) exited Medicare from 2010 to 2015 (eTable 2 in the Supplement). Solo practice PCPs were a mean 6 years older than group practice PCPs and made up 36.6% of all exiting PCPs (3469 of 9491) (eFigure 2 in the Supplement). We matched 5939 exiting PCPs to 5939 nonexiting PCPs, which was 62.6% of all exiting PCPs. In this matched sample, exiting PCPs had 169 870 attributed beneficiaries compared with 189 600 beneficiaries attributed to matched, nonexiting PCPs. The characteristics of the PCPs were well balanced across exiting and matched nonexiting PCPs 24 months before exit (Table 1). The beneficiaries exposed to exiting PCPs were similar to the beneficiaries exposed to nonexiting PCPs in demographic and clinical characteristics, with standardized mean differences of 0.15 or less.
Table 1. Characteristics of the Study Population.
| Characteristic | Patients who lost a PCP | Patients who did not lose a PCP | Absolute standardized mean difference |
|---|---|---|---|
| No. of PCPs | 5939 | 5939 | NA |
| No. of Medicare beneficiaries | 169 870 | 189 600 | NA |
| No. of observations | 16 579 457 | 16 579 457 | NA |
| PCP characteristics (2 y prior to PCP exit, matched) | |||
| PCP age, mean (SD), y | 56.8 (12.4) | 55.3 (10.4) | 0.13 |
| Caseload per PCP per mo, meana | 12.1 | 12.1 | 0.01 |
| Female PCPs, % | 25.8 | 25.7 | 0.005 |
| PCPs per practice, % | |||
| 1 (Solo) | 45.7 | 45.7 | 0.0 |
| 2 | 10.5 | 10.5 | 0.0 |
| 3 | 6.7 | 6.7 | 0.0 |
| 4-5 | 10.0 | 10.0 | 0.0 |
| ≥6 | 27.1 | 27.1 | 0.0 |
| Medicare-assigned beneficiary characteristics | |||
| Beneficiary demographics | |||
| Beneficiary age, mean (SD), y | 71.4 (6.1) | 72.0 (5.0) | 0.11 |
| Race, % | |||
| White | 84.0 | 82.7 | 0.05 |
| Black | 9.9 | 9.1 | 0.04 |
| Other | 5.9 | 7.9 | 0.12 |
| Female, % | 37.2 | 36.9 | 0.02 |
| Urban residence, % | 80.9 | 86.3 | 0.15 |
| Beneficiary clinical characteristics | |||
| Elixhauser risk score, mean (SD)b | 2.5 (0.9) | 2.6 (0.8) | 0.05 |
| End-stage kidney disease, % | 1.0 | 1.1 | 0.03 |
| Also enrolled in Medicaid, % | 19.7 | 18.2 | 0.07 |
| Health care use and outcomes 12-24 mo before exit (annual rate per beneficiary) | |||
| Any primary care visit, mean (SD) | 6.0 (3.7) | 6.0 (3.0) | 0.02 |
| Specialty care visits, mean (SD) | 9.6 (5.1) | 9.9 (4.7) | 0.07 |
| Urgent care visits, mean (SD) per 1000 beneficiaries | 9.3 (47.1) | 8.6 (41.7) | 0.02 |
| Emergency department visits, mean (SD) per 100 beneficiaries | 68.9 (65.2) | 61.4 (48.5) | 0.13 |
| Inpatient visits, mean (SD) per 100 beneficiaries | 33.5 (30.5) | 32.8 (26.8) | 0.02 |
| Spending, mean (SD), $ | 7712 (5505) | 7985 (5489) | 0.05 |
| Probability of death, % | 3.6 (1.5) | 3.5 (1.4) | 0.01 |
Abbreviations: PCP, primary care physician; NA, not applicable.
The caseload per PCP per month captured the number of unique Medicare beneficiaries seen by each PCP for any type of visit, regardless of whether the PCP was assigned as the beneficiary’s PCP.
The Elixhauser Risk Index scores patients based on comorbidities and preexisting conditions that are associated with death; scores range from 0 to 12, with higher scores indicating more coexisting conditions and that beneficiaries are of “higher risk.”
Changes in Patterns of Outpatient Care, Prescriptions, and Preventive Care After PCP Exit
In the first year after a PCP’s exit, annual primary care visits decreased 18.4% (95% CI, −19.8% to −16.9%), or −0.97 visits, from a baseline mean of 5.3 visits annually (Figure 1; Table 2). During the same period, specialist visits increased 6.2% (95% CI, 5.4%-7.0%), or 0.6 visits, from a baseline mean of 9.5 visits annually among exposed beneficiaries compared with unexposed beneficiaries. The observed changes in the rates of PCP and specialist visits persisted for 2 years after PCP exit.
Figure 1. Overall Monthly Trends in Outpatient Visits and Prescriptions After Loss of a Primary Care Physician (PCP) .
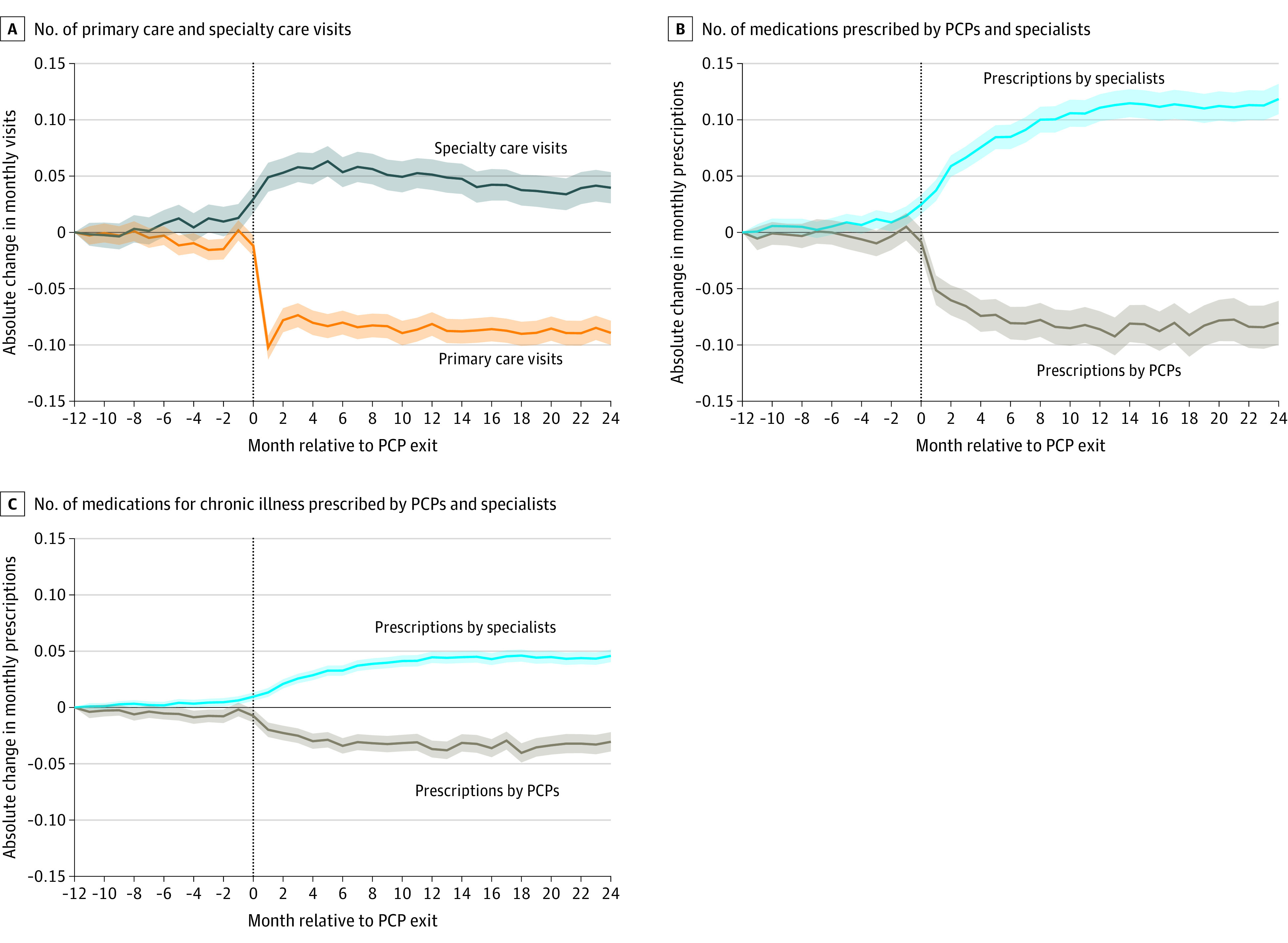
A, Absolute change in monthly primary care and specialty care visits among patients whose PCP exited vs those whose PCP did not exit. B, Absolute change in number of medications prescribed among patients whose PCP exited vs those whose PCP did not exit. C, Absolute change in number of medications prescribed for chronic illness among patients whose PCP exited vs those whose PCP did not exit. Absolute risk differences are relative to 12 months before PCP exit. Exiting PCPs were matched to nonexiting PCPs as described in the Methods. Month 0 (vertical dotted line) includes the last month an exiting PCP was observed practicing. Graphs of outpatient, primary care, specialist, emergency department, and inpatient visit pretrends are shown in eMethods 3 in the Supplement. Overall, beneficiaries had a mean of 0.4 primary care visits, 0.8 specialty visits, 1.5 filled prescriptions, and 0.6 filled prescriptions for chronic illness per month at baseline (Table 2). Shaded areas indicate 95% CIs.
Table 2. Changes in Health Care Use in the First 2 Years After Loss of a Primary Care Physiciana.
| Characteristic | Annual rate, meanb | 1 y After PCP exit | 2 y After PCP exit | ||
|---|---|---|---|---|---|
| Absolute risk difference (95% CI) | Relative change, % (95% CI) | Absolute risk difference (95% CI) | Relative change, % (95% CI) | ||
| Health care use | |||||
| Primary care visits | 5.3 | −1.0 (−1.0 to −0.9) | −18.4 (−19.8 to −16.9) | −1.0 (−1.1 to −0.9) | −18.8 (−20.3 to −17.2) |
| Specialist visits | 9.5 | 0.6 (0.5 to 0.7) | 6.2 (5.4 to 7.0) | 0.4 (0.3 to 0.5) | 4.5 (3.6 to 5.4) |
| Urgent care visits per 1000 | 9.6 | 1.7 (0.6 to 2.9) | 17.8 (6.0 to 29.7) | 0.6 (−0.8 to 2.0) | 6.1 (−8.2 to 20.4) |
| ED visits per 100 | 74.1 | 2.3 (1.2 to 3.4) | 3.1 (1.6 to 4.6) | −0.4 (−1.7 to 0.9) | −0.5 (−2.2 to 1.2) |
| Inpatient visits per 100 | 36.7 | 0.6 (−0.2 to 1.4) | 1.7 (−0.4 to 3.8) | −0.5 (−1.4 to 0.3) | −1.5 (−3.7 to 0.8) |
| Prescription fills | |||||
| All prescriptions | 18.5 | 0.2 (0.04 to 0.3) | 0.9 (0.2 to 1.5) | 0.3 (0.2 to 0.5) | 1.7 (0.8 to 2.5) |
| Prescriptions for chronic illnessc | 6.9 | 0.08 (0.04 to 0.1) | 1.2 (0.6 to 1.9) | 0.2 (0.1 to 0.2) | 2.2 (1.3 to 3.1) |
| Preventive care received | |||||
| Preventive screenings | 1.6 | 0.02 (−0.005 to 0.05) | 1.4 (−0.3 to 3.0) | 0.02 (−0.01 to 0.05) | 1.2 (−0.7 to 3.2) |
| Influenza vaccine, % | 47.7 | −2.6 (−3.2 to −2.0) | −5.5 (−6.7 to −4.2) | −2.0 (−2.6 to −1.4) | −4.2 (−5.4 to −3.0) |
| Spendingd | |||||
| Total spending, $ | 8602 | 189 (30 to 347) | 2.2 (0.4 to 4.0) | −40 (−212 to 133) | −0.5 (−2.5 to 1.5) |
Abbreviations: ED, emergency department; PCP, primary care physician.
Analyses of 5939 exiting PCPs and 5939 nonexiting PCPs, matched as described in the Methods. Data follow patients 2 years after a PCP’s exit, and an observation is at the patient-year level. Main estimates are from the matched difference-in-differences model described in the Methods, with indicators for outcomes 1 and 2 years after departure. Relative percentage changes divide absolute differences by the preperiod mean among exposed patients. Regressions include fixed effects for each PCP-matched pair, cluster at the PCP match level, and weighted by a PCP’s patient load.
Baseline mean is the mean among Medicare beneficiaries with nonexiting PCPs 2 years prior to the synthetically assigned exit.
Prescriptions for chronic illness are total fills for a subset of medications for chronic illness that are frequently managed in primary care settings (depression, diabetes, hypertension, and hypercholesterolemia).
Spending included physician charges, inpatient charges, and emergency department charges.
There was a statistically significant, although small, increase in beneficiaries’ total number of prescriptions and chronic illness medication prescriptions among exposed beneficiaries after a PCP’s exit (0.16 total prescriptions [95% CI, 0.04-0.3] and 0.08 chronic illness medication prescriptions [95% CI, 0.04-0.1]; Table 2). However, totals obscured significant changes in where beneficiaries sought care. The number of prescriptions and chronic medication prescriptions administered by specialists increased, while those administered by PCPs decreased (Figure 1; eTable 3 in the Supplement). For instance, the mean annual number of chronic medications prescribed by PCPs decreased by 0.32 prescriptions (95% CI, −0.38 to −0.27) from a baseline mean of 5.1, a relative decrease of 6.4%, while those administered by specialists increased by 0.44 prescriptions (95% CI, 0.40-0.48) from a baseline mean of 1.9, a relative increase of 23.5%, in the 2 years after PCP exit.
Changes in preventive health services were also observed after the loss of a PCP. Total annual rates of influenza vaccinations decreased by 5.5% (95% CI, −6.7% to −4.2%), or −2.6 percentage points, from a baseline mean of 47.7% among exposed beneficiaries compared with unexposed beneficiaries (Table 2). For the composite preventive screening measure, there was no significant change in the mean annual number of screenings administered among exposed beneficiaries compared with unexposed beneficiaries. However, both influenza vaccination and the composite preventive care measure shifted from PCPs to specialists (influenza vaccinations, −18.6% decrease among PCPs [95% CI, −20.9% to −16.3%] and 40.3% increase among specialists [95% CI, 34.4%-46.2%]; preventive screenings, −7.1% decrease among PCPs [95% CI, −9.1% to -5.0%] and 33.8% increase among specialists [95% CI, 30.5%-37.2%]) (eTable 4 in the Supplement).
Changes in Spending and Hospital and Urgent Care Use After PCP Exit
In the first year after a PCP’s exit, urgent care visits increased 17.8% (95% CI, 6.0%-29.7%), or 1.7 visits, from a baseline mean of 9.6 visits per 1000 patients annually among exposed beneficiaries compared with unexposed beneficiaries (Table 2). During the same period, emergency department visits increased 3.1% (95% CI, 1.6%-4.6%), or 2.3 visits, from a baseline average of 74.1 visits annually per 100 patients (eFigure 4 and eFigure 5 in the Supplement).
Changes in health care use corresponded to an increase in total Medicare spending of $189 (95% CI, $30-$347) per patient the first year after a PCP’s exit (Table 2). An increase in spending of $189 per beneficiary translates to $46 350 of additional Medicare spending attributable to each exiting PCP annually (based on a mean caseload of 49 Medicare fee-for-service beneficiaries per year in the 20% sample, multiplied by 5 to approximate a 100% sample). Inpatient visits and the probability of death did not significantly change between exposed and unexposed beneficiaries (Table 2; eTable 4 in the Supplement).
Solo vs Group Practices
The overall changes described were larger for patients of exiting PCPs who were in solo practice. For example, compared with beneficiaries who did not lose a PCP, those who did lose a PCP in solo practice experienced larger reductions in primary care visits (−21.5% [95% CI, −23.8% to −19.3%]) than in group practices (−15.7% [95% CI, −17.6% to −13.8%]) (P < .001 for difference in a test of interactions) (Table 3; Figure 2). Specialist visits also increased significantly more for beneficiaries whose exiting PCP was in a solo practice compared with group practice (8.8% [95% CI, 7.6%-10.0%] for solo practice vs 3.9% [95% CI, 2.8%-5.0%] for group practice; P < .001 for difference in a test of interactions). Patients of exiting PCPs in solo practices also had 4.4% more emergency department visits (95% CI, 2.1%-6.7%) vs 2.0% (95% CI, –0.04% to 4.0%) for group practice and $260 (95% CI, $12-$509) increased spending vs $129 (95% CI, –$75 to $333) for group practice. Patients of exiting PCPs in solo practices were also more likely to shift their prescription fills toward specialist physicians (1.5 prescriptions among specialists [95% CI, 1.3-1.6]) vs those with exiting PCPs in group practice (0.87 among specialists [95% CI, 0.76-0.99]) (P < .001 for difference in a test of interactions) (eTable 3 in the Supplement).
Table 3. Changes in Health Care Use in First Year After Loss of a PCP, by PCP’s Practice Sizea.
| Characteristic | Medicare beneficiaries, 1 y after PCP exit | P valueb | |||||
|---|---|---|---|---|---|---|---|
| Solo practice | Group practice | ||||||
| Annual rate, meanc | Absolute risk difference (95% CI) | Relative change, % (95% CI) | Annual rate, meanc | Absolute risk difference (95% CI) | Relative change, % (95% CI) | ||
| Health care use | |||||||
| Primary care visits | 5.3 | −1.1 (−1.3 to −1.0) | −21.5 (−23.8 to −19.3) | 5.2 | −0.8 (−0.9 to −0.7) | −15.7 (−17.6 to −13.8) | <.001 |
| Specialist visits | 10.0 | 0.9 (0.8 to 1.0) | 8.8 (7.6 to 10.0) | 9.1 | 0.4 (0.3 to 0.5) | 3.9 (2.8 to 5.0) | <.001 |
| Urgent care visits per 1000 | 9.8 | 3.3 (1.6 to 5.0) | 34.1 (16.8 to 51.5) | 9.5 | 0.4 (−1.2 to 1.9) | 4.0 (−12.2 to 20.2) | .01 |
| ED visits per 100 | 74.5 | 3.3 (1.6 to 5.0) | 4.4 (2.1 to 6.7) | 73.8 | 1.5 (−0.03 to 3.0) | 2.0 (−0.04 to 4.0) | .12 |
| Inpatient visits per 100 | 36.5 | 0.4 (−0.8 to 1.6) | 1.1 (−2.2 to 4.3) | 36.8 | 0.8 (−0.2 to 1.8) | 2.2 (−0.6 to 5.0) | .61 |
| Prescription fills | |||||||
| All prescriptions | 19.4 | 0.1 (−0.05 to 0.3) | 0.7 (−0.3 to 1.6) | 17.7 | 0.2 (0.03 to 0.3) | 1.0 (0.2 to 1.8) | .71 |
| Prescriptions for chronic illnessd | 7.1 | 0.1 (0.04 to 0.2) | 1.6 (0.6 to 2.7) | 6.8 | 0.06 (−0.002 to 0.1) | 0.9 (−0.03 to 1.7) | .23 |
| Preventive care received | |||||||
| Preventive screenings | 1.6 | 0.03 (−0.01 to 0.07) | 2.0 (−0.5 to 4.4) | 1.6 | 0.01 (−0.02 to 0.05) | 0.9 (−1.5 to 3.2) | .53 |
| Influenza vaccine, % | 46.0 | −1.3 (−2.2 to −0.4) | −2.9 (−4.9 to −1.0) | 49.0 | −3.6 (−4.4 to −2.9) | −7.4 (−9.0 to −5.8) | <.001 |
| Spendinge | |||||||
| Total spending, $ | 8860 | 260 (12 to 509) | 2.9 (0.1 to 5.7) | 8384 | 129 (−75 to 333) | 1.5 (−0.9 to 4.0) | .42 |
Abbreviations: ED, emergency department; PCP, primary care physician.
Analyses of 2713 exiting PCPs and 2713 nonexiting PCPs in solo PCP practices and 3226 exiting PCPs and 3226 nonexiting PCPs in group practices. Table reports analyses for patients 1 year after a PCP’s exit and observations are at the Medicare beneficiary-year level. Main estimates are from the matched difference-in-differences model described in the Methods. We modeled subgroup analyses by whether or not the PCP belonged to a solo or group practice as a formal test of interactions. Relative percentage changes divide absolute differences by the preperiod mean among unexposed patients. Regressions include fixed effects for each PCP-matched pair, cluster at the PCP match level, and weight by a PCP’s patient load.
Based on a test of whether or not solo and group practice estimates are statistically different.
Baseline mean is the mean among Medicare beneficiaries with nonexiting PCPs 2 years prior to the synthetically assigned exit.
Prescriptions for chronic illness are total fills for a subset of medications for chronic illness that are frequently managed in primary care settings (depression, diabetes, hypertension, and hypercholesterolemia).
Spending included physician charges, inpatient charges, and emergency department charges.
Figure 2. Monthly Trends in Outpatient Visits and Prescriptions After Loss of a Primary Care Physician (PCP), by Solo vs Group Practice.
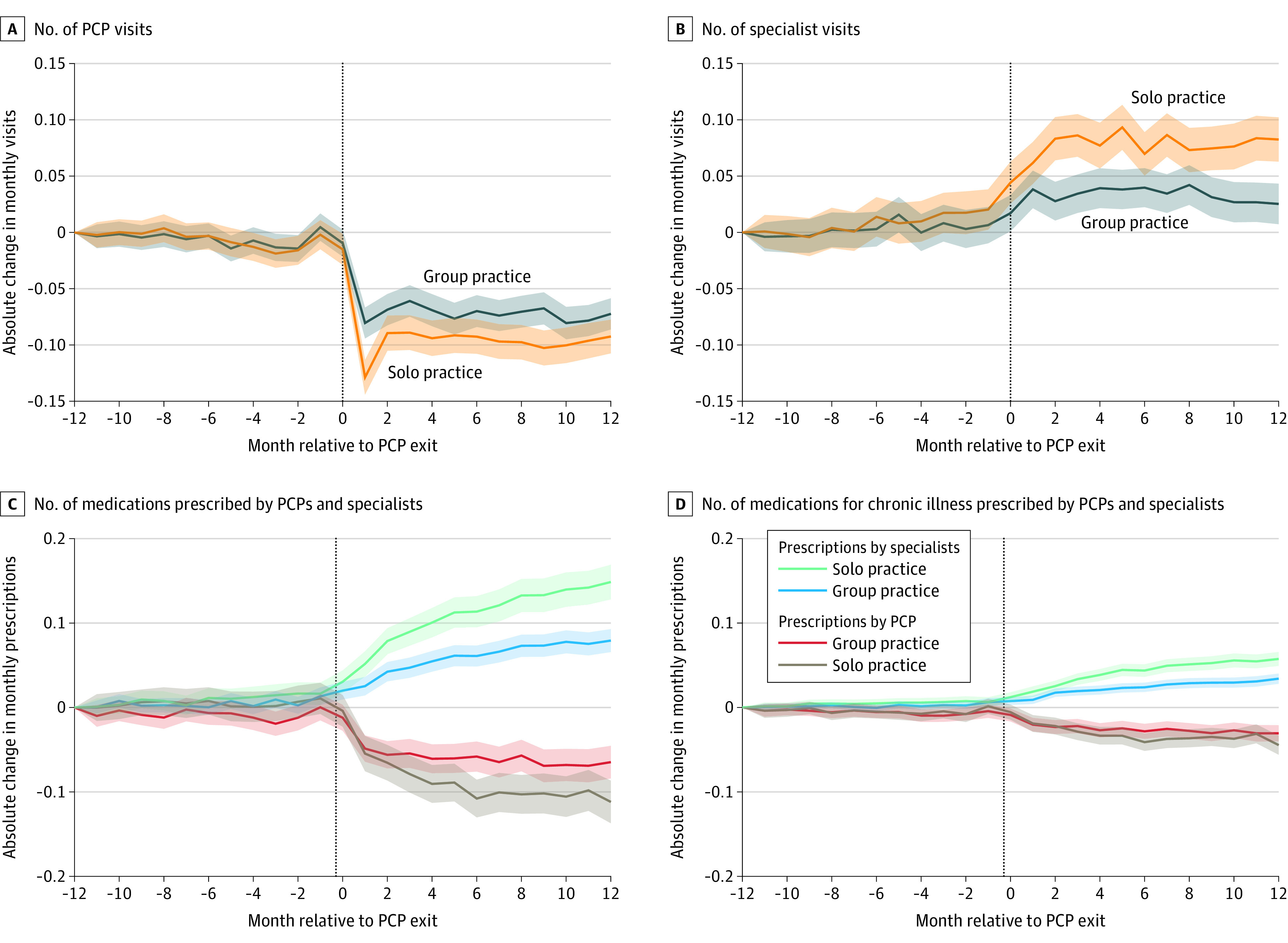
A, Absolute change in monthly PCP visits among patients whose PCP exited vs those whose PCP did not exit, stratified into those in a solo or group PCP practice. B, Absolute change in monthly specialist visits among patients whose PCP exited vs those whose PCP did not exit, stratified into those in a solo or group PCP practice. C, Absolute change in number of medications prescribed among patients whose PCP exited vs those whose PCP did not exit, stratified into those in a solo or group PCP practice. D, Absolute change in number of medications for chronic illness prescribed among patients whose PCP exited vs those whose PCP did not exit, stratified into those in a solo or group PCP practice. Absolute risk differences are relative to 12 months before PCP exit. Exiting PCPs were matched to nonexiting PCPs as described in the Methods. Month 0 (vertical dotted line) includes the last month an exiting PCP was observed practicing. Overall, beneficiaries had a mean of 0.4 primary care visits, 0.8 specialty visits, 1.5 filled prescriptions, and 0.6 filled prescriptions for chronic illness per month at baseline (Table 2). Shaded areas indicate 95% CIs.
Discussion
In this analysis of Medicare beneficiaries who lost a PCP, we found increased use of specialty, urgent, and emergency care and decreased use of primary care in the 2 years after the loss of a PCP compared with beneficiaries who did not lose their PCP. Loss of a PCP was associated with a statistically significant but small increase in the overall number of filled prescriptions and a modest decrease in preventive care services, including influenza vaccination. Overall, outpatient visits, prescriptions, and preventive services shifted from primary to specialty care as patients substituted specialty care for primary care. This shift toward specialty care was especially pronounced for beneficiaries whose PCPs were solo practitioners.
Multiple factors could explain the observed changes in health care use after a PCP’s exit. Increased rates of urgent care and emergency care visits may be a direct consequence of decreased access to care, moving patients to non–primary care settings for urgent issues. It is also possible that patients’ chronic illnesses were exacerbated without a usual source of care to manage health issues in the short term. The shift of outpatient visits, medications, and preventive care to specialist physicians may reflect the fact that the average Medicare beneficiary sees 1 PCP and 2 specialists annually.33 Therefore, beneficiaries could be transferring their care to physicians they already know. This observed change could also imply that many specialists are willing to adopt primary care responsibilities when necessary.
Shifts in outpatient visits and medications toward specialists persisted for 2 years. One interpretation for this result is that, after the loss of a PCP, patients may not actively seek to return to their prior pattern of health care use.34 To the extent that this is a replicable and durable trend, PCP exits may be a mechanism that pushes patients toward specialist-dominated care over time. It is not certain whether more specialist-centered care would have a positive or negative impact over time, although many advocate for a strong primary care–centered system as a key ingredient for successful delivery reform.35,36,37 Given that 10.4% of PCPs exited the workforce during the 4 years in our study sample, this trend could be associated with a meaningful shift away from primary care over a period of 2 to 3 decades.
For beneficiaries who lost a PCP in solo practice, the rate of primary care visits decreased 27.0% more than beneficiaries whose exiting PCP was in a group practice. The vulnerability of beneficiaries with solo PCPs is especially relevant given that PCPs in solo practice comprised one-third of the study sample and given that their mean age was 6 years older than group PCPs, implying that solo PCPs will be retiring at an increased rate. This finding suggests that an underappreciated feature of group practices may be their capacity to take on a departing PCP’s patients and therefore maintain better continuity of care under certain conditions, such as when a PCP nears retirement. More robust infrastructure at larger practices (eg, advanced electronic health record systems), procedures that internally transfer patients to replacement PCPs (eg, informing patients of their replacement PCP by letter or telephone), different care patterns (eg, group practices, some of which may contain specialty physicians within those practices, may refer to specialists at a higher rate than solo PCPs), or preexisting relationships between patients and remaining PCPs (eg, providing care in teams) may explain why patients in larger practices have more stable patterns of care with transition to replacement PCPs.23,38,39 These observations suggest that interventions that focus on transitioning information and relationships to a new primary care team in advance of PCP exit may be able to mitigate the decrease in primary care engagement after solo PCP exit and other potential negative consequences.
Limitations
This study has several limitations. First, the findings may not be generalizable to other insured populations besides individuals insured by Medicare. Second, we were unable to observe the reason for a PCP’s exit, which may be associated with patient outcomes in certain circumstances. Third, patients were assigned to PCPs 2 years before PCP exit to limit bias due to sorting around the exit period (eg, PCPs may transition sicker patients to new PCPs before healthier patients). As a result, patients who started seeing a PCP less than 1 year before that PCP exited were excluded from analyses. These restrictions are unlikely to affect our findings because they were applied to both exiting and nonexiting PCPs, but they could still limit the generalizability of the findings. Fourth, there may be limitations in the definitions used to classify PCPs. Fifth, PCPs in the solo practice category may have included small practices in which only patients of 1 PCP were sampled in the data’s 20% sampling frame.
Conclusions
Among Medicare beneficiaries, the loss of a PCP was associated with reduced primary care use in the 2 years after the loss as well as increased use of specialty, urgent, and emergency care. These results suggest that interrupting primary care relationships could diminish not only patients’ health outcomes but also patients’ future engagement with primary care.
eMethods 1. Data Details
eMethods 2. Estimating Equations and Identification
eMethods 3. Additional Results
eMethods 4. Sensitivity Analyses
eTable 1. Cut-off Values for Matching Bins
eTable 2. Breakdown of Departures
eTable 3. Prescription Outcomes 2 Years After PCP Exit
eTable 4. Other Outcomes 2 Years After PCP Exit
eTable 5. Changes in Utilization by Practice Size of Exiting PCP by Year
eTable 6. Balance Table for Unmatched Exiting and Staying PCPs and All Visiting Beneficiaries
eTable 7. Changes in Utilization After PCP Exit by Year, by Tercile of Practice Size
eTable 8. Changes in Utilization After PCP Exit by Year, Including all Clinics with 100+ PCPs
eTable 9. Changes in Utilization After PCP Exit by Year, Controlling for Hospital Referral Region (HRR)
eTable 10. Changes in Utilization After PCP Exit by Year, Matching on Urban/Rural
eTable 11. Changes in Utilization After PCP Exit by Year, Not Matching on Caseload
eFigure 1. Data Restriction and Matching Strategy
eFigure 2. Histograms of PCP Age
eFigure 3. Probability of Visiting Assigned PCP
eFigure 4. Raw Plots
eFigure 5. Pre-Period and Event Plots per Patient, Relative to t = −12
References
- 1.Rodriguez KL, Bayliss NK, Alexander SC, et al. . Effect of patient and patient-oncologist relationship characteristics on communication about health-related quality of life. Psychooncology. 2011;20(9):935-942. doi: 10.1002/pon.1829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chanfreau-Coffinier C, Washington DL, Chuang E, et al. . Exploring the association of care fragmentation and patient ratings of care quality: a mediation analysis of women veterans’ experience with VA care. Health Serv Res. 2019;54(4):816-826. doi: 10.1111/1475-6773.13153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodriguez HP, Rogers WH, Marshall RE, Safran DG. The effects of primary care physician visit continuity on patients’ experiences with care. J Gen Intern Med. 2007;22(6):787-793. doi: 10.1007/s11606-007-0182-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mainous AG III, Kern D, Hainer B, Kneuper-Hall R, Stephens J, Geesey ME. The relationship between continuity of care and trust with stage of cancer at diagnosis. Fam Med. 2004;36(1):35-39. [PubMed] [Google Scholar]
- 5.Katz DA, McCoy K, Sarrazin MV. Does improved continuity of primary care affect clinician-patient communication in VA? J Gen Intern Med. 2014;29(suppl 2):S682-S688. doi: 10.1007/s11606-013-2633-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Starfield B Is primary care essential? Lancet. 1994;344(8930):1129-1133. doi: 10.1016/S0140-6736(94)90634-3 [DOI] [PubMed] [Google Scholar]
- 7.Rosenblatt RA, Wright GE, Baldwin LM, et al. . The effect of the doctor-patient relationship on emergency department use among the elderly. Am J Public Health. 2000;90(1):97-102. doi: 10.2105/AJPH.90.1.97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nyweide DJ, Anthony DL, Bynum JPW, et al. . Continuity of care and the risk of preventable hospitalization in older adults. JAMA Intern Med. 2013;173(20):1879-1885. doi: 10.1001/jamainternmed.2013.10059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hussey PS, Schneider EC, Rudin RS, Fox DS, Lai J, Pollack CE. Continuity and the costs of care for chronic disease. JAMA Intern Med. 2014;174(5):742-748. doi: 10.1001/jamainternmed.2014.245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wasson JH, Sauvigne AE, Mogielnicki RP, et al. . Continuity of outpatient medical care in elderly men: a randomized trial. JAMA. 1984;252(17):2413-2417. doi: 10.1001/jama.1984.03350170015011 [DOI] [PubMed] [Google Scholar]
- 11.Khullar D, Burke GC, Casalino LP. Can small physician practices survive? sharing services as a path to viability. JAMA. 2018;319(13):1321-1322. doi: 10.1001/jama.2017.21704 [DOI] [PubMed] [Google Scholar]
- 12.Sessums LL, McHugh SJ, Rajkumar R. Medicare’s vision for advanced primary care: new directions for care delivery and payment. JAMA. 2016;315(24):2665-2666. doi: 10.1001/jama.2016.4472 [DOI] [PubMed] [Google Scholar]
- 13.Friedberg MW, Hussey PS, Schneider EC. Primary care: a critical review of the evidence on quality and costs of health care. Health Aff (Millwood). 2010;29(5):766-772. doi: 10.1377/hlthaff.2010.0025 [DOI] [PubMed] [Google Scholar]
- 14.McWilliams JM, Chernew ME, Dalton JB, Landon BE. Outpatient care patterns and organizational accountability in Medicare. JAMA Intern Med. 2014;174(6):938-945. doi: 10.1001/jamainternmed.2014.1073 [DOI] [PubMed] [Google Scholar]
- 15.Hausman N, Lavetti K Physician practice organization and negotiated prices: evidence from state law changes. Working paper. Published August 31, 2019. Accessed September 5, 2019. http://kurtlavetti.com/NCA_price_vc.pdf
- 16.Lavetti K, Simon C, White W. The impacts of restricting mobility of skilled service workers: evidence from physicians. J Hum Resoures. 2020;55(3):1025-1067. doi: 10.3368/jhr.55.3.0617-8840R5 [DOI] [Google Scholar]
- 17.Hsu J, Price M, Spirt J, et al. . Patient population loss at a large pioneer accountable care organization and implications for refining the program. Health Aff (Millwood). 2016;35(3):422-430. doi: 10.1377/hlthaff.2015.0805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Medical Association Competency and the Aging Physician: Report 5 of the Council on Medical Education (A-15). American Medical Association; 2015. [Google Scholar]
- 19.Sabety AS The value of service sector relationships in health care. Harvard working paper. Published April 4, 2020. Accessed April 10, 2020. https://www.adriennesabety.com/research
- 20.Misra-Hebert AD, Kay R, Stoller JK. A review of physician turnover: rates, causes, and consequences. Am J Med Qual. 2004;19(2):56-66. doi: 10.1177/106286060401900203 [DOI] [PubMed] [Google Scholar]
- 21.Ruhe M, Gotler RS, Goodwin MA, Stange KC. Physician and staff turnover in community primary care practice. J Ambul Care Manage. 2004;27(3):242-248. doi: 10.1097/00004479-200407000-00008 [DOI] [PubMed] [Google Scholar]
- 22.Pereira AG, Kleinman KP, Pearson SD. Leaving the practice: effects of primary care physician departure on patient care. Arch Intern Med. 2003;163(22):2733-2736. doi: 10.1001/archinte.163.22.2733 [DOI] [PubMed] [Google Scholar]
- 23.Reddy A, Pollack CE, Asch DA, Canamucio A, Werner RM. The effect of primary care provider turnover on patient experience of care and ambulatory quality of care. JAMA Intern Med. 2015;175(7):1157-1162. doi: 10.1001/jamainternmed.2015.1853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Plomondon ME, Magid DJ, Steiner JF, et al. . Primary care provider turnover and quality in managed care organizations. Am J Manag Care. 2007;13(8):465-472. [PubMed] [Google Scholar]
- 25.Leader S, Perales PJ. Provision of primary-preventive health care services by obstetrician-gynecologists. Obstet Gynecol. 1995;85(3):391-395. doi: 10.1016/0029-7844(94)00411-6 [DOI] [PubMed] [Google Scholar]
- 26.Ho DE, Imai K, King G, Stuart EA. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Political Analysis. 2007; 15(3):199-236. doi: 10.1093/pan/mpl013 [DOI] [Google Scholar]
- 27.Daw JR, Hatfield LA. Matching in difference-in-differences: between a rock and a hard place. Health Serv Res. 2018;53(6):4111-4117. doi: 10.1111/1475-6773.13017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pollack CE, Hussey PS, Rudin RS, Fox DS, Lai J, Schneider EC. Measuring care continuity: a comparison of claims-based methods. Med Care. 2016;54(5):e30-e34. doi: 10.1097/MLR.0000000000000018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Medicare & Medicaid Services Medicare preventive services. Updated August 2020. Accessed January 12, 2018. https://www.cms.gov/Medicare/Prevention/PrevntionGenInfo/medicare-preventive-services/MPS-QuickReferenceChart-1.html
- 30.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. doi: 10.1097/00005650-199801000-00004 [DOI] [PubMed] [Google Scholar]
- 31.Angrist JD, Pischke JS. Mostly Harmless Econometrics: An Empiricist's Companion. Princeton University Press; 2009. [Google Scholar]
- 32.Abadie A, Spiess J. Robust post-matching inference. Harvard University working paper. Published January 2019. Accessed September 1, 2019. https://scholar.harvard.edu/files/spiess/files/robust.pdf
- 33.Pham HH, Schrag D, O’Malley AS, Wu B, Bach PB. Care patterns in Medicare and their implications for pay for performance. N Engl J Med. 2007;356(11):1130-1139. doi: 10.1056/NEJMsa063979 [DOI] [PubMed] [Google Scholar]
- 34.Pincavage AT, Ratner S, Prochaska ML, et al. . Outcomes for resident-identified high-risk patients and resident perspectives of year-end continuity clinic handoffs. J Gen Intern Med. 2012;27(11):1438-1444. doi: 10.1007/s11606-012-2100-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502. doi: 10.1111/j.1468-0009.2005.00409.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Phillips RL Jr, Bazemore AW. Primary care and why it matters for U.S. health system reform. Health Aff (Millwood). 2010;29(5):806-810. doi: 10.1377/hlthaff.2010.0020 [DOI] [PubMed] [Google Scholar]
- 37.Bindman A Primary care for all. JAMA. 2019;322(17):1641-1642. doi: 10.1001/jama.2019.16630 [DOI] [PubMed] [Google Scholar]
- 38.Audet AM, Doty MM, Peugh J, Shamasdin J, Zapert K, Schoenbaum S. Information technologies: when will they make it into physicians’ black bags? MedGenMed. 2004;6(4):2. [PMC free article] [PubMed] [Google Scholar]
- 39.Pincavage AT, Lee WW, Beiting KJ, Arora VM. What do patients think about year-end resident continuity clinic handoffs? a qualitative study. J Gen Intern Med. 2013;28(8):999-1007. doi: 10.1007/s11606-013-2395-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods 1. Data Details
eMethods 2. Estimating Equations and Identification
eMethods 3. Additional Results
eMethods 4. Sensitivity Analyses
eTable 1. Cut-off Values for Matching Bins
eTable 2. Breakdown of Departures
eTable 3. Prescription Outcomes 2 Years After PCP Exit
eTable 4. Other Outcomes 2 Years After PCP Exit
eTable 5. Changes in Utilization by Practice Size of Exiting PCP by Year
eTable 6. Balance Table for Unmatched Exiting and Staying PCPs and All Visiting Beneficiaries
eTable 7. Changes in Utilization After PCP Exit by Year, by Tercile of Practice Size
eTable 8. Changes in Utilization After PCP Exit by Year, Including all Clinics with 100+ PCPs
eTable 9. Changes in Utilization After PCP Exit by Year, Controlling for Hospital Referral Region (HRR)
eTable 10. Changes in Utilization After PCP Exit by Year, Matching on Urban/Rural
eTable 11. Changes in Utilization After PCP Exit by Year, Not Matching on Caseload
eFigure 1. Data Restriction and Matching Strategy
eFigure 2. Histograms of PCP Age
eFigure 3. Probability of Visiting Assigned PCP
eFigure 4. Raw Plots
eFigure 5. Pre-Period and Event Plots per Patient, Relative to t = −12


