Abstract
Background
Myocardial infarction is an important cause of morbidity and mortality in both men and women. Atypical or the absence of symptoms, more prevalent among women, may contribute to unrecognized myocardial infarctions and missed opportunities for preventive therapies. The aim of this research is to investigate sex‐based differences of undiagnosed myocardial infarction in the general population.
Methods and Results
In the Lifelines Cohort Study, all individuals ≥18 years with a normal baseline ECG were followed from baseline visit till first follow‐up visit (≈5 years, n=97 203). Individuals with infarct‐related changes between baseline and follow‐up ECGs were identified. The age‐ and sex‐specific incidence rates were calculated and sex‐specific cardiac symptoms and predictors of unrecognized myocardial infarction were determined. Follow‐up ECG was available after a median of 3.8 (25th and 75th percentile: 3.0–4.6) years. During follow‐up, 198 women experienced myocardial infarction (incidence rate 1.92 per 1000 persons‐years) compared with 365 men (incidence rate 3.30; P<0.001 versus women). In 59 (30%) women, myocardial infarction was unrecognized compared with 60 (16%) men (P<0.001 versus women). Individuals with unrecognized myocardial infarction less often reported specific cardiac symptoms compared with individuals with recognized myocardial infarction. Predictors of unrecognized myocardial infarction were mainly hypertension, smoking, and higher blood glucose level.
Conclusions
A substantial proportion of myocardial infarctions are unrecognized, especially in women. Opportunities for secondary preventive therapies remain underutilized if myocardial infarction is unrecognized.
Keywords: cohort study, epidemiology, incidence, sex differences, unrecognized myocardial infarction
Subject Categories: Electrocardiology (ECG), Women, Myocardial Infarction, Epidemiology
Nonstandard Abbreviations and Acronyms
- BMI
body mass index
- OR
odds ratio
- CVD
cardiovascular disease
- HDL
high‐density lipoprotein
- LDL
low‐density lipoprotein
- MI
myocardial infarction
Clinical Perspective
What Is New?
The current study reports sex‐specific incidence rates of unrecognized myocardial infarction (MI) in a more contemporary complete adult population with a normal reference ECG.
It was identified that 30% of MI in women remained unrecognized compared with 16% of myocardial infarctions in men, with the greatest difference between women and men among individuals aged ≤60 years.
As compared with individuals with recognized MI, individuals with unrecognized myocardial infarction less often reported specific cardiac symptoms, and predictors of unrecognized MI were mainly hypertension, smoking, and higher blood glucose level.
What Are the Clinical Implications?
Clinicians need to be aware of the high proportion of unrecognized MI, especially in young women.
Reducing the number of unrecognized MI might be challenging but is important as opportunities for secondary preventive therapies will be missed.
Further studies are needed to determine whether screening for unrecognized MI might be of value in terms of outcome and cost‐effectiveness.
Angina pectoris exemplifies the typical manifestation of symptomatic myocardial ischemia. A considerable number of less characteristic symptoms can also indicate ischemia. These less typical symptoms occur more often in women and include dyspnea, nausea, and fatigue.1 These symptoms are more prone to remain unmentioned by the patient, or unnoted or misinterpreted by the doctor, with possible underdiagnoses of myocardial infarction (MI).1 Whether or not recognized, MI increases morbidity and mortality in both men and women,2, 3, 4 with some indications for increased risk among women.3
Earlier studies suggested that up to 64% of MI may not be recognized at their initial presentation.5 Although, absolute numbers of MI have been reported to be higher in men5, 6 the proportion of unrecognized MIs might be larger in women.3, 7
A major shortcoming of previous studies is that many reported the prevalence of unrecognized MI5; prevalence studies are more sensitive to misclassification and have intrinsic limitations in investigating risk factors. Another major limitation of previous reports is the date of ascertainment. It remains questionable whether studies presenting data of decades ago continue to be representative considering disease, treatment (reperfusion therapy), lifestyle and disease risk factors awareness campaigns.8, 9 The more informative data on incidence10 in the general population is sparse and limited to selected samples7, 11, 12 or individuals at increased risk.13, 14 The Lifelines Cohort Study recruited a contemporary adult population (aged ≥18 years) of >150 000 participants in The Netherlands15, 16 and included the systematic collection of serial electrocardiographic evaluations. Here, we aim to determine the sex‐specific incidence rate of unrecognized MI in the Lifelines Cohort Study and describe its sex‐specific association with self‐reported symptoms and other potential predictors.
Methods
Study Design and Subjects
The study design and rationale of the Lifelines Cohort Study were described previously in detail.16 Lifelines is a multi‐disciplinary prospective population‐based 3‐generation cohort study examining the health and health‐related behaviors of 167 729 people living in the North of The Netherlands. Lifelines uses a broad range of investigative procedures in assessing the biomedical, sociodemographic, behavioral, physical, and psychological factors that contribute to the health and disease of the general population, with a special focus on multi‐morbidity and complex genetics. Because of data use agreements with Lifelines, we are unable to make available any data or analysis materials. The Lifelines Cohort Study was approved by the medical ethical committee of the University Medical Center Groningen, The Netherlands. During the baseline visit all participants signed an informed consent form for both the baseline and follow‐up visits, and provided blood and 24‐hour urine samples. Medication use data were collected in a questionnaire and categorized using the general Anatomical Therapeutic Chemical Classification System codes. Participants underwent physical examination and 12‐lead ECG. Between baseline and follow‐up visits, participants were invited to complete 2 follow‐up questionnaires. At the 5‐year follow‐up visit, study personnel collected new blood samples, and systematically conducted physical examinations and 12‐lead ECGs. Participants were asked in the questionnaires (at baseline and follow‐up visit and 2 follow‐up questionnaires) whether they had been hampered by specific symptoms in the past 7 days. For the current study, only participants aged ≥18 years were included.
Definition of Myocardial Infarction
The baseline and corresponding follow‐up ECGs were initially evaluated automatically by the WelchAllyn CardioPerfect (version 1.6.2.1105) software. When automatic evaluation of the ECG was classified as abnormal (possible MI), the ECG was reviewed by an experienced cardiologist to evaluate for the presence of any Q wave in leads V2 to V3 ≥0.02 seconds (s) or QS complex in leads V2 and V3, Q waves ≥0.03s and ≥0.1 mV deep or QS complex in leads I, II, aVL, aVF, or V4 to V6 in any 2 leads of a contiguous lead grouping (I, aVL; V4–V6; II, III, aVF), or R waves ≥0.04s in V1–V2 and R/S ≥1 with a concordant positive T wave in absence of conduction defect.17 An incident unrecognized MI (by both the patient and physician) was defined when a participant had ECG signs corresponding to MI at the follow‐up 5‐year examination in absence of self‐reported history of MI and pathologic ECG signs at the baseline examination. Conversely, a recognized MI was defined when participants answered affirmatively to having experienced a heart attack since the last time they completed the Lifelines questionnaire. When there was no evidence of an infarction (on ECG or questionnaire), participants were randomly selected to generate an age‐ and sex‐classified reference group, with 3 balanced references for each case. ECGs of the referents were evaluated by a cardiologist to confirm whether the ECG was normal. After evaluation of both ECGs for the MI and the reference group, we repeated the matching to have 3 (or 2 when 3 matches was not possible) referents for each confirmed unrecognized MI.
Cardiovascular Risk Factors and Symptoms
We classified the cardiovascular risk factor distribution based on questionnaires, physical examination, and blood biomarkers. The operationalization of these variables has been previously described.16 Self‐reported symptom frequencies were obtained from baseline and follow‐up questionnaires inquiring whether the participant had experienced the item of interest during the past 7 days and considered present if reported in ≥1 days. The Framingham risk score was generated with age, total cholesterol, smoking, high‐density lipoprotein‐cholesterol, systolic blood pressure, self‐reported antihypertensive medication use, and diabetes mellitus.18
Statistical Analysis
Initially, we determined the age‐adjusted sex‐specific incidence rate per 1000 person‐years of unrecognized MI in the general population (Table S1). Thereon, we evaluated the independent predictors (including sex‐specific reported symptoms) of unrecognized MI through a nested case‐referent approach that can be consulted in Figure 1.
Figure 1. Flowchart of the study population.
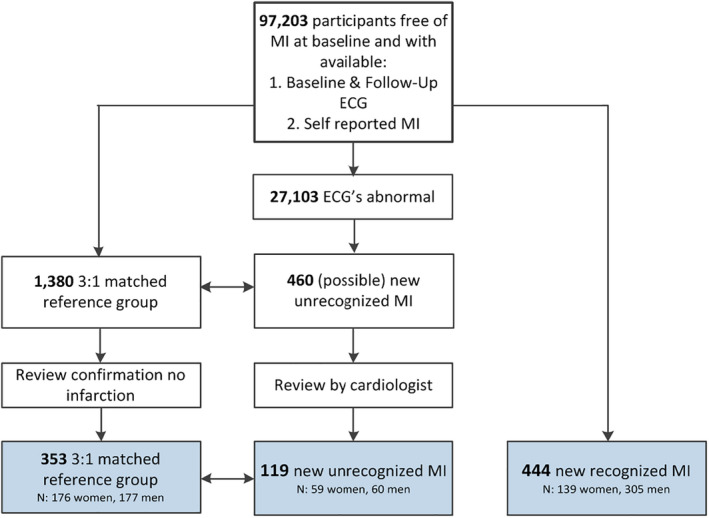
Baseline and follow‐up ECGs were available for 97 203 participants. Among these, 460 ECGs were automatically evaluated as being suspected for an unrecognized myocardial infarction. These individuals were randomly matched with 3 (or if not possible with 2) referents based on age in years at baseline and sex. ECGs of both participants with unrecognized myocardial infarction and the reference group, were reviewed by a cardiologist to validate whether the ECG was pathologic (in case of unrecognized myocardial infarction) or normal (in case of the reference group). MI indicates myocardial infarction.
Additionally, a similar analysis was implemented to evaluate the independent predictors of recognized MI to explore whether the predictors of unrecognized MI differ from those of recognized MI. These and further explorative comparisons between subjects with an unrecognized MI and those with a recognized MI are presented in Tables S2 and S3).
Incidence Rate
The cumulative amount of person‐years was determined in strata according to sex and the individuals’ age at baseline: 18 to 29, 30 to 39, 40 to 49, 50 to 59, 60 to 69, 70 to 79 and ≥80 years. The age‐ and sex‐specific incidence rates per 1000 person‐years follow‐up were calculated as the number of people that developed the event between the baseline and follow‐up assessment. Incidence rates were expressed per 1000 person‐years with corresponding 95% CIs. An age‐ and sex‐standardized incidence rate was calculated for the total Lifelines Cohort Study population. Eventually, this rate was averaged across the weights of the general population of The Netherlands, based on the population distribution by age and sex of adults ≥18 years (13 060 511) in 2010.
Characterizing Symptoms and Predictors of Unrecognized MI
Dichotomous baseline characteristics of individuals with unrecognized MI, recognized MI, and the matched reference group (without infarction) are presented as frequencies and percentages. Continuous variables are summarized by means and SD or medians and 25th and 75th percentiles, as appropriate. The Chi‐square test was used to compare dichotomous variables and differences of continuous variables between groups were evaluated through independent samples t tests or 2‐sample Wilcoxon rank‐sum (Mann–Whitney) tests, as necessary. We examined the interaction of the sex variable by adding product terms of sex and each of the cardiovascular risk factors or blood biomarkers to the logistic regression models. Univariate logistic regression analyses were performed to determine the statistical predictors of unrecognized MI (binary outcome variable representing unrecognized MI versus matched control). Subsequently, a backward‐stepwise multiple logistic regression analysis was performed with cutoff for removal set at significance level 0.10 and significance level at 0.05, to determine the independent predictors of unrecognized MI. As sensitivity analyses, a forward‐stepwise multiple logistic regression was performed, with cutoff for entry set at a significance level 0.05. Variables significantly associated with MI in both the backward‐ and forward‐stepwise model, were considered to be predictors of MI. Similarly, univariate and multiple (backward‐ and forward‐stepwise) logistic regression analyses were performed on unrecognized MI versus recognized MI to explore latent differences between the predictors of unrecognized and recognized MI (Table S3). Two‐sided P<0.05 were considered to be statistically significant. All statistical analyses were performed using Stata version IC 13, StataCorp, College Station, TX.
Results
Baseline and follow‐up ECGs were available for 57 276 women and 39 927 men (Figure 1). Baseline characteristics of women and men with unrecognized MI and the matched reference group are presented in Table 1. Additionally, comparative baseline characteristics of women and men with a recognized MI are presented in Table S2.
Table 1.
Baseline Characteristics of Individuals With Unrecognized Myocardial Infarction and the Reference Group
| Women | Men | Sex | |||||
|---|---|---|---|---|---|---|---|
| Unrecognized MI n=59 | Reference n=176 | P Value | Unrecognized MI n=60 | Reference n=177 | P Value | Interaction P Value | |
| Age, mean±SD | 54.6 (11.1) | 54.5 (11.0) | 0.53 | 56.4 (13.3) | 55.9 (13.0) | 0.59 | 0.94 |
| Anthropometry, mean±SD | |||||||
| BMI, kg/m2 | 27.1 (4.4) | 26.0 (4.7) | 0.14 | 27.1 (4.3) | 26.7 (3.2) | 0.17 | 0.17 |
| Heart rate, BPM | 69 (11) | 69 (11) | 0.88 | 66 (13) | 65 (12) | 0.98 | 0.89 |
| Risk factor, % (n) | |||||||
| Hypertension | 39.0 (23) | 30.7 (54) | 0.24 | 65.0 (39) | 43.5 (77) | 0.004 | 0.24 |
| Hypercholesterolemia | 20.3 (12) | 25.6 (45) | 0.42 | 28.3 (17) | 26.0 (46) | 0.72 | 0.40 |
| Diabetes mellitus | 6.8 (4) | 5.1 (9) | 0.63 | 10.0 (6) | 6.8 (12) | 0.42 | 0.88 |
| Active or former smoker | 64.4 (38) | 55.1 (97) | 0.21 | 73.3 (44) | 54.8 (97) | 0.012 | 0.34 |
| Family health—CVD | 8.5 (5) | 11.4 (20) | 0.55 | 6.7 (4) | 10.7 (19) | 0.36 | 0.80 |
| Framingham risk—10‐y risk, median (25th and 75th percentiles) | 4 (12–30) | 10 (4–20) | 0.21 | 6 (10–18) | 8 (4–12) | 0.07 | 0.39 |
| Blood biomarkers | |||||||
| Triglycerides, mmol/L | 1.0 (0.7–1.9) | 1.0 (0.7–1.3) | 0.46 | 1.4 (1.0–1.9) | 1.3 (0.9–1.5) | 0.031 | 0.82 |
| Cholesterol, mmol/L | 5.2 (0.9) | 5.5 (1.1) | 0.12 | 5.5 (1.1) | 5.3 (1.0) | 0.34 | 0.07 |
| HDL, mmol/L | 1.6 (0.4) | 1.7 (0.4) | 0.06 | 1.2 (0.3) | 1.3 (0.3) | 0.025 | 0.50 |
| LDL, mmol/L | 3.2 (0.9) | 3.5 (1.0) | 0.13 | 3.6 (1.0) | 3.6 (0.9) | 0.72 | 0.19 |
| Glucose, mmol/L | 5.3 (1.8) | 5.0 (0.7) | 0.017 | 5.7 (1.5) | 5.3 (0.7) | 0.011 | 0.88 |
| HbA1c (%) | 5.7 (0.6) | 5.6 (0.4) | 0.37 | 5.8 (0.7) | 5.7 (0.4) | 0.046 | 0.49 |
| Pharmacotherapy, % (n) | |||||||
| Blood pressure lowering | 36.1 (13) | 31.3 (36) | 0.59 | 52.8 (19) | 48.4 (44) | 0.65 | 0.95 |
| Cholesterol lowering | 8.5 (5) | 7.4 (13) | 0.79 | 15.0 (9) | 14.7 (26) | 0.95 | 0.86 |
| Platelet inhibitors | 3.4 (2) | 1.7 (3) | 0.44 | 11.7 (7) | 7.3 (13) | 0.30 | 0.85 |
| Self‐reported symptoms at baseline or follow‐up, % (n) | |||||||
| Dizziness | 51.7 (30) | 46.8 (81) | 0.52 | 35.6 (21) | 33.0 (58) | 0.71 | 0.86 |
| Chest Pain | 32.8 (19) | 27.9 (48) | 0.48 | 18.6 (11) | 29.0 (51) | 0.12 | 0.10 |
| Nausea | 43.1 (25) | 39.2 (67) | 0.60 | 37.3 (22) | 33.0 (58) | 0.54 | 0.95 |
| Dyspnea | 24.1 (14) | 25.0 (43) | 0.90 | 23.7 (14) | 20.5 (36) | 0.60 | 0.64 |
| Physically weak | 24.1 (13) | 19.2 (30) | 0.45 | 25.5 (12) | 17.4 (25) | 0.22 | 0.71 |
BMI indicates body mass index; BPM, beats per minute; CVD, cardiovascular disease; HDL, high‐density lipoprotein; and LDL, low‐density lipoprotein.
Sex‐Based Differences in Unrecognized and Recognized Myocardial Infarction
During a median follow‐up of 3.8 (25th and 75th percentiles: 3.0–4.6) years, a total of 139 (0.24%) women and 305 (0.76%) men reported to having been diagnosed with an MI. Based on analysis of ECG changes of all participants, another 59 women and 60 men were classified as having an unrecognized MI. A baseline and follow‐up ECG indicative for an unrecognized MI is displayed in Figure S1. Calculating the proportion of unrecognized MI yields 30% (59/198) for women and 16% (60/365) for men (P<0.001). In the age categories of 40 to 49 and 50 to 59 years, the difference in proportions between women and men was greatest (43% versus 17% in the former P=0.001, and 30% versus 11% in the latter, P=0.008). The age distribution of participants with recognized MI and unrecognized MI is displayed in Figure S2.
The incidence rate of recognized MI age‐standardized for the general Dutch population was 1.69 (0.84, 3.19) in women and 2.67 (1.86, 3.95) per 1000 person‐years in men (P<0.001, Figure 2A, Table S1). For unrecognized MI, the general population adjusted incidence rate per 1000 person‐years follow‐up was 0.23 (0.14, 1.45) in women and 0.63 (0.24, 1.52) in men.
Figure 2. Incidence rate and proportion of recognized and unrecognized myocardial infarction in men and women.
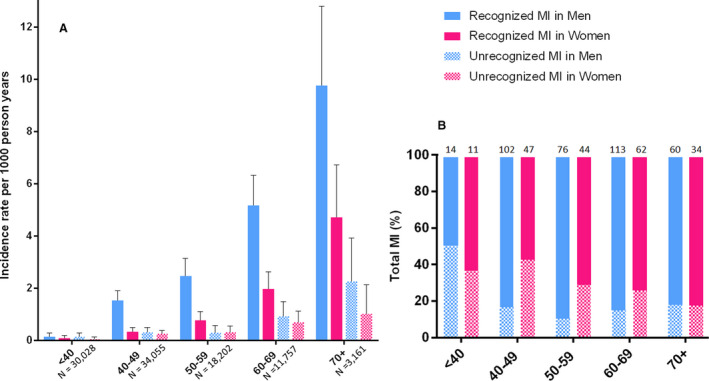
A, Incidence rate with 95% CI of recognized and unrecognized myocardial infarction (MI) in men and women. The number of participants in the age categories is reported below the bars. B, Proportion of recognized and unrecognized MI in men and women. Number of total MIs per sex and age category is reported above the bars. Recognized MI is displayed in plain bars, unrecognized MI in checkered bars. Men are in blue and women in pink. MI indicates myocardial infarction.
Association of Characteristics and Symptoms of Unrecognized Versus Recognized Myocardial Infarction
Compared with referents, individuals with unrecognized MI had a higher prevalence of hypertension (52% versus 37.1%, P=0.004), more frequently smoked (69% versus 55%, P=0.008) and had higher mean blood glucose levels (5.5±1.4 versus 5.1±0.8, P<0.001, Table 1). No significant interactions with sex were found for differences in baseline characteristics in individuals with unrecognized MI versus the reference group.
Comparing individuals with unrecognized MI to those with recognized MI, the prevalence of hypertension (52% versus 60%, P=0.11), diabetes mellitus (8.4% versus 9.5%, P=0.72), smoking (69% versus 71%, P=0.74), and family history of cardiovascular disease, 7.6% versus 12.4%, P=0.14) were comparable (Table S2). The prevalence of hypercholesterolemia was lower in individuals with unrecognized MI compared with recognized MI (24% versus 41%, P=0.001). Sex differences were only seen for total cholesterol and low‐density lipoprotein levels, which were higher in women with recognized MI as compared with men (Table S2).
Frequency of reported symptoms by individuals across the unrecognized MI, recognized MI and reference groups at baseline or follow‐up are presented in Table 1 and Table S2. Compared with individuals with unrecognized MI, individuals with recognized MI more often reported chest pain (women: 53.3% versus 32.8% [P=0.009], men: 54.8% versus 18.6% [P<0.001]) or dyspnea (women: 48.2% versus 24.1% [P=0.002], men: 40.2% versus 23.7% [P=0.017]). Dizziness and nausea were the most commonly reported symptoms in individuals with unrecognized MI (51.7% and 43.1% in women and 35.6% and 37.3% in men, respectively). Notably, compared with referents, individuals with unrecognized MI did not significantly report more symptoms (Table 1). There were no significant interactions between sex and reported symptoms between individuals with recognized MI and the reference group (Table 1). However, a discrete trend towards significance was found for the interaction between sex and chest pain was observed, with a stronger association of chest pain and unrecognized MI in women as compared with men (P for interaction=0.10).
Sex‐Based Predictors of Unrecognized Myocardial Infarction
In the univariate logistic regression analyses of unrecognized MI versus the reference group, body mass index (odds ratio [OR] 1.05, 95% CI, 1.00–1.11), hypertension (OR 1.84, 95% CI, 1.21–2.80), smoking status (OR 1.82, 95% CI, 1.17–2.82), triglycerides (OR 1.37, 95% CI, 1.05–1.80), high‐density lipoprotein (OR 0.48, 95% CI, 0.27–0.84), glucose (OR 1.41, 95% CI, 1.14–1.75), and hemoglobin A1c levels (OR 1.01, 95% CI, 1.01–2.22) were associated with unrecognized MI. The multiple logistic regression analyses documented that only hypertension, smoking status, and blood glucose levels were predictors of unrecognized MI (Table 2). The association between hypertension, smoking status, or blood glucose level and unrecognized MI was not different in men and women (P for interaction=0.24, 0.34 and 0.88, respectively, Table 1).
Table 2.
Univariate and Multiple Logistic Regression Analysis for Predictors of Unrecognized Myocardial Infarction vs the Reference Group
| Univariate Logistic Regression | Multiple Logistic Regression | |||||
|---|---|---|---|---|---|---|
| P Value | Odds Ratio | 95% CI | P Value | Odds Ratio | 95% CI | |
| Anthropometry | ||||||
| BMI | 0.045 | 1.05 | 1.00–1.11 | |||
| Heart rate | 0.93 | |||||
| Risk factor | ||||||
| Hypertension | 0.004 | 1.84 | 1.21–2.80 | 0.004 | 2.05 | 1.26–3.33 |
| Hypercholesterolemia | 0.76 | |||||
| Diabetes mellitus | 0.35 | |||||
| Active or former smoker | 0.008 | 1.82 | 1.17–2.82 | 0.016 | 1.75 | 1.11–1.78 |
| Family health—CVD | 0.28 | |||||
| Blood biomarkers | ||||||
| Triglycerides | 0.020 | 1.37 | 1.05–1.80 | |||
| Cholesterol | 0.67 | |||||
| HDL | 0.011 | 0.48 | 0.27–0.84 | |||
| LDL | 0.41 | |||||
| Glucose | 0.002 | 1.41 | 1.14–1.75 | 0.009 | 1.36 | 1.08–1.72 |
| HbA1c | 0.046 | 1.49 | 1.01–2.22 | |||
BMI indicates body mass index; CVD, cardiovascular disease; HbA1c, hemoglobin A1c; HDL, high‐density lipoprotein; and LDL, low‐density lipoprotein.
Table S3 presents univariate and multiple logistic regression analyses for individuals with unrecognized MI versus recognized MI. Compared with individuals in the youngest age category (<40 years), individuals in a middle age category (50–59 years) had significantly lower odds of unrecognized MI (OR 0.34, 95% CI, 0.13–0.89). In univariate regression analyses, there was a stronger association between low‐density lipoprotein and recognized MI in women as compared with men (P for interaction=0.028, Table S2), and a borderline stronger association between hypercholesterolemia and recognized MI in women compared with men (P for interaction=0.06). However, in multiple regression analyses, these associations did not achieve statistical significance (Table S3).
Discussion
The Lifelines Cohort Study gives the unique opportunity to study the incidence and sex‐based differences of unrecognized MI in a complete contemporary adult population aged ≥18 years. In this population, a substantial part of incident MIs remain undiagnosed. During 3.8 years of follow‐up, 30% of MIs in women remained unrecognized compared with 16% of MIs in men. The higher proportion of incident unrecognized MI in women is in line with most studies investigating older study populations.3, 7, 19 One study investigating the prevalence of unrecognized MI in different ethnicities, did not report a sex difference.20 Using the Lifelines data, we were able ≥ to examine European individuals aged 18 years, and determined that the proportion of unrecognized MI was especially high in European women ≤60 years.
Individuals with unrecognized MI are at risk for cardiovascular events21, 22 and mortality23 and identifying these individuals is important for secondary prevention. To date, it is not completely clear why a higher proportion of MIs remain unrecognized in women compared with men. It has been described that lower pain sensitivity is more strongly associated with unrecognized MI in women than in men.24 Also, attitude of patients and general practitioners towards cardiovascular risk may influence perception of pain and symptoms. Women less often relate their chest pain to cardiac disease compared with men.25 Also, public information and medical training of health professionals have focused on recognition of male pattern symptoms, leaving women at greater risk.26 Currently, the impact of cardiovascular disease on the health status of women is gaining more recognition and becomes a focus of public education efforts. A statement by the American Heart Association highlights the importance of sex differences for developing strategies to early recognize MI and to personalize secondary prevention after MI,1 which will hopefully lead to a higher detection rate of MI in women.
Knowledge on sex‐specific symptoms associated with unrecognized MI might be relevant to improve early recognition of MI. In the current study, women and men with unrecognized MI less often reported a typical history of chest pain compared with individuals with recognized MI. This suggests the “atypical” silent nature of unrecognized MI, or an underreporting by the participant when symptoms do not match expectation and are not linked to MI. Compared with the reference group, individuals with unrecognized MI did not report more (cardiovascular) symptoms. It has been described that unrecognized MIs are often smaller and occur more often because of coronary microvascular dysfunction instead of large vessel disease,27 which may contribute to the absence of symptoms in individuals with unrecognized MI. Furthermore, both diabetes mellitus and impaired glucose tolerance forecast unrecognized MI in elderly individuals.28 Diabetic neuropathy is a common complication associated with diabetes mellitus and may lead to the absence of symptoms in individuals with unrecognized MI.28 Interestingly, in a study investigating a population with diabetes mellitus, no sex differences in the prevalence of unrecognized MI were observed.29 It has been reported that men and women with unrecognized MI more often report a history of cardiopulmonary symptoms as compared with referents.30 In the current study, operationalization and quantification of individual symptoms were based on questions inquiring whether the participant had experienced these symptoms during the past 7 days. This may have led to an underestimation of the reported frequency of symptoms and further research is needed for validation of our reported frequencies of symptoms.
Classical cardiovascular risk factors were more prevalent in men and women who developed an unrecognized MI as compared with referents, while there was no difference in preventive medication use between these groups. These findings suggest that individuals with unrecognized MI less often are being identified as at‐risk and aware of their risk. Individuals who are aware of their cardiovascular risk may be more likely to recognize and report symptoms suggestive of MI than those who are unaware. Since secondary prevention of MI is focused on cardiovascular risk factors, individuals with recognized MI have a reduced risk for developing heart failure or a recurrence of MI. In contrast, chances for initiating secondary prevention are missed in those with unrecognized MI. These individuals are at high risk of unpredictable cardiovascular disease and could gain greatly from the use of cardiovascular treatments.
Limitations
Our study has several limitations. First, we used ECG criteria for the diagnosis of unrecognized MI. ECG criteria for diagnosing unrecognized MI have been reported to have low sensitivity.31 However, it is important to note that these previous studies did not use a baseline ECG to compare it against. Our study is based on ECG changes, new Q waves, likely to have a higher sensitivity and specificity although this has not formally been assessed. Based on previous comparisons with ECG and magnetic resonance imaging it is likely that the reported incidence rates of unrecognized MI may be an underestimation. Second, our study is limited to Q‐wave MIs. Using the ECG, we were not able to assess non‐Q MIs as well. Incidences of MI and unrecognized MI may therefore be higher than reported here. Third, lead misplacements tend to occur more often in women than in men because of differences in breast tissue.32 False positive ECG abnormalities indicating a prior septal MI, are therefore more likely to occur in women as compared with men. However, Lifelines research nurses had strict protocols for placing the ECG leads, which minimized the chance of such misplacements. Fourth, self‐reported data on the history of MI were used for differentiating between recognized MI and unrecognized MI. We are not able to validate the questionnaire against hospital data. It has been described that the use of self‐reported data might lead to an underestimation of the disease.33 Fifth, participants of the Lifelines Cohort Study were of European ancestry. The results may therefore not be generalizable to other ethnicities. Sixth, we were not able to replicate the reported findings, since the Lifelines Cohort Study is the only Dutch study covering the contemporary complete adult population. Last, since we used observational data, we are not able to draw conclusions on causality because of potential unmeasured confounding or reverse causality.
Conclusions
The incidence rate of unrecognized MI in the general population is 0.23 in women and 0.63 in men per 1000 person‐years. A substantial proportion of MIs are unrecognized, especially in women (30% in women versus 16% in men). Women and men with unrecognized MI did not report more symptoms compared with the referents. Predictors of unrecognized MI were classical risk factors, including hypertension (OR 2.05, 95% CI, 1.26–3.33), smoking (OR 1.75, 95% CI, 1.11–1.78), and higher blood glucose level (OR 1.36, 95% CI, 1.08–1.72). Opportunities for secondary preventive therapies remain underutilized when MI remains unrecognized.
Sources of Funding
The Lifelines Biobank initiative has been made possible by subsidy from the Dutch Ministry of Health, Welfare and Sport, the Dutch Ministry of Economic Affairs, the University Medical Center Groningen (UMCG, The Netherlands), University Groningen and the Northern Provinces of The Netherlands.
Disclosures
None.
Supporting information
Tables S1–S3
Figures S1–S2
(J Am Heart Assoc. 2020;9:e015519 DOI: 10.1161/JAHA.119.015519.)
For Sources of Funding and Disclosures, see page 8.
References
- 1. Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, Lindley KJ, Vaccarino V, Wang TY, Watson KE, et al. Acute myocardial infarction in women: a scientific statement from the American Heart Association. Circulation. 2016;133:916–947. [DOI] [PubMed] [Google Scholar]
- 2. Schelbert EB, Cao JJ, Sigurdsson S, Aspelund T, Kellman P, Aletras AH, Dyke CK, Thorgeirsson G, Eiriksdottir G, Launer LJ, et al. Prevalence and prognosis of unrecognized myocardial infarction determined by cardiac magnetic resonance in older adults. JAMA. 2012;308:890–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zhang ZM, Rautaharju PM, Prineas RJ, Rodriguez CJ, Loehr L, Rosamond WD, Kitzman D, Couper D, Soliman EZ. Race and sex differences in the incidence and prognostic significance of silent myocardial infarction in the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2016;133:2141–2148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Qureshi WT, Zhang ZM, Chang PP, Rosamond WD, Kitzman DW, Wagenknecht LE, Soliman EZ. Silent myocardial infarction and long‐term risk of heart failure: the ARIC Study. J Am Coll Cardiol. 2018;71:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Valensi P, Lorgis L, Cottin Y. Prevalence, incidence, predictive factors and prognosis of silent myocardial infarction: a review of the literature. Arch Cardiovasc Dis. 2011;104:178–188. [DOI] [PubMed] [Google Scholar]
- 6. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, et al.; American Heart Association Statistics Committee, Stroke Statistics Subcommittee . Executive summary: heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133:447–454. [DOI] [PubMed] [Google Scholar]
- 7. de Torbal A, Boersma E, Kors JA, van Herpen G, Deckers JW, van der Kuip DA, Stricker BH, Hofman A, Witteman JC. Incidence of recognized and unrecognized myocardial infarction in men and women aged 55 and older: the Rotterdam Study. Eur Heart J. 2006;27:729–736. [DOI] [PubMed] [Google Scholar]
- 8. Kannel WB, Cupples LA, Gagnon DR. Incidence, precursors and prognosis of unrecognized myocardial infarction. Adv Cardiol. 1990;37:202–214. [DOI] [PubMed] [Google Scholar]
- 9. Sigurdsson E, Thorgeirsson G, Sigvaldason H, Sigfusson N. Unrecognized myocardial infarction: epidemiology, clinical characteristics, and the prognostic role of angina pectoris. The Reykjavik Study. Ann Intern Med. 1995;122:96–102. [DOI] [PubMed] [Google Scholar]
- 10. Noordzij M, Dekker FW, Zoccali C, Jager KJ. Measures of disease frequency: prevalence and incidence. Nephron Clin Pract. 2010;115:c17–c20. [DOI] [PubMed] [Google Scholar]
- 11. McAreavey D, Vidal JS, Aspelund T, Eiriksdottir G, Schelbert EB, Kjartansson O, Cao JJ, Thorgeirsson G, Sigurdsson S, Garcia M, et al. Midlife cardiovascular risk factors and late‐life unrecognized and recognized myocardial infarction detect by cardiac magnetic resonance: ICELAND‐MI, the AGES‐Reykjavik Study. J Am Heart Assoc. 2016;5:e002420 DOI: 10.1161/JAHA.115.002420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nadelmann J, Frishman WH, Ooi WL, Tepper D, Greenberg S, Guzik H, Lazar EJ, Heiman M, Aronson M. Prevalence, incidence and prognosis of recognized and unrecognized myocardial infarction in persons aged 75 years or older: the Bronx Aging Study. Am J Cardiol. 1990;66:533–537. [DOI] [PubMed] [Google Scholar]
- 13. Shlipak MG, Elmouchi DA, Herrington DM, Lin F, Grady D, Hlatky MA; Heart and Estrogen/progestin Replacement Study Research Group . The incidence of unrecognized myocardial infarction in women with coronary heart disease. Ann Intern Med. 2001;134:1043–1047. [DOI] [PubMed] [Google Scholar]
- 14. MacDonald MR, Petrie MC, Home PD, Komajda M, Jones NP, Beck‐Nielsen H, Gomis R, Hanefeld M, Pocock SJ, Curtis PS, et al. Incidence and prevalence of unrecognized myocardial infarction in people with diabetes: a substudy of the Rosiglitazone Evaluated for Cardiac Outcomes and Regulation of Glycemia in Diabetes (RECORD) study. Diabetes Care. 2011;34:1394–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Scholtens S, Smidt N, Swertz MA, Bakker SJ, Dotinga A, Vonk JM, van Dijk F, van Zon SK, Wijmenga C, Wolffenbuttel BH, et al. Cohort Profile: LifeLines, a three‐generation cohort study and biobank. Int J Epidemiol. 2014;44:1172–1180. [DOI] [PubMed] [Google Scholar]
- 16. van der Ende MY, Hartman MH, Hagemeijer Y, Meems LM, de Vries HS, Stolk RP, de Boer RA, Sijtsma A, van der Meer P, Rienstra M, et al. The LifeLines Cohort Study: prevalence and treatment of cardiovascular disease and risk factors. Int J Cardiol. 2017;228:495–500. [DOI] [PubMed] [Google Scholar]
- 17. White H, Thygesen K, Alpert JS, Jaffe A. Universal MI definition update for cardiovascular disease. Curr Cardiol Rep. 2014;16:492. [DOI] [PubMed] [Google Scholar]
- 18. D'Agostino RBS, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753. [DOI] [PubMed] [Google Scholar]
- 19. Kannel WB. Silent myocardial ischemia and infarction: insights from the Framingham Study. Cardiol Clin. 1986;4:583–591. [PubMed] [Google Scholar]
- 20. Boland LL, Folsom AR, Sorlie PD, Taylor HA, Rosamond WD, Chambless LE, Cooper LS. Occurrence of unrecognized myocardial infarction in subjects aged 45 to 65 years (the ARIC study). Am J Cardiol. 2002;90:927–931. [DOI] [PubMed] [Google Scholar]
- 21. O'Neal WT, Shah AJ, Efird JT, Rautaharju PM, Soliman EZ. Subclinical myocardial injury identified by cardiac infarction/injury score and the risk of mortality in men and women free of cardiovascular disease. Am J Cardiol. 2014;114:1018–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. De Bacquer D, De Backer G, Kornitzer M, Myny K, Doyen Z, Blackburn H. Prognostic value of ischemic electrocardiographic findings for cardiovascular mortality in men and women. J Am Coll Cardiol. 1998;32:680–685. [DOI] [PubMed] [Google Scholar]
- 23. van der Ende MY, Hartman MHT, Schurer RAJ, van der Werf HW, Lipsic E, Snieder H, van der Harst P. Prevalence of electrocardiographic unrecognized myocardial infarction and its association with mortality. Int J Cardiol. 2017;243:34–39. [DOI] [PubMed] [Google Scholar]
- 24. Ohrn AM, Nielsen CS, Schirmer H, Stubhaug A, Wilsgaard T, Lindekleiv H. Pain tolerance in persons with recognized and unrecognized myocardial infarction: a population‐based, cross‐sectional study. J Am Heart Assoc. 2016;5:e003846 DOI: 10.1161/JAHA.116.003846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Granot M, Goldstein‐Ferber S, Azzam ZS. Gender differences in the perception of chest pain. J Pain Symptom Manage. 2004;27:149–155. [DOI] [PubMed] [Google Scholar]
- 26. Kim ES, Menon V. Status of women in cardiovascular clinical trials. Arterioscler Thromb Vasc Biol. 2009;29:279–283. [DOI] [PubMed] [Google Scholar]
- 27. Ohrn AM, Schirmer H, von Hanno T, Mathiesen EB, Arntzen KA, Bertelsen G, Njolstad I, Lochen ML, Wilsgaard T, Bairey Merz CN, et al. Small and large vessel disease in persons with unrecognized compared to recognized myocardial infarction: the Tromso Study 2007–2008. Int J Cardiol. 2018;253:14–19. [DOI] [PubMed] [Google Scholar]
- 28. Stacey RB, Zgibor J, Leaverton PE, Schocken DD, Peregoy JA, Lyles MF, Bertoni AG, Burke GL. Abnormal fasting glucose increases risk of unrecognized myocardial infarctions in an elderly cohort. J Am Geriatr Soc. 2018;67:43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Stiles MC, Seaquist ER, Yale JF, Green JB, Katz LA, Kempainen S, Light LS, Pepper PV, Zhang ZM, Soliman EZ. Is silent myocardial infarction more common in women with type 2 diabetes than in men? J Diabetes Complications. 2012;26:118–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ammar KA, Makwana R, Redfield MM, Kors JA, Burnett JC, Rodeheffer RJ. Unrecognized myocardial infarction: the association with cardiopulmonary symptoms and mortality is mediated via echocardiographic abnormalities of global dysfunction instead of regional dysfunction: the Olmsted County Heart Function Study. Am Heart J. 2006;151:799–805. [DOI] [PubMed] [Google Scholar]
- 31. Sandler LL, Pinnow EE, Lindsay J. The accuracy of electrocardiographic Q waves for the detection of prior myocardial infarction as assessed by a novel standard of reference. Clin Cardiol. 2004;27:97–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rautaharju PM, Park L, Rautaharju FS, Crow R. A standardized procedure for locating and documenting ECG chest electrode positions: consideration of the effect of breast tissue on ECG amplitudes in women. J Electrocardiol. 1998;31:17–29. [DOI] [PubMed] [Google Scholar]
- 33. Molenaar EA, Van Ameijden EJ, Grobbee DE, Numans ME. Comparison of routine care self‐reported and biometrical data on hypertension and diabetes: results of the Utrecht Health Project. Eur J Public Health. 2007;17:199–205. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S3
Figures S1–S2


