Before COVID-19 became a global pandemic, India was dealing with another, much older epidemic—tuberculosis (TB)—which affected 2.64 million Indians in 2019 and killed nearly 450 000 people in the country.1 That is over 1000 TB deaths every single day, well before COVID-19 entered the picture. In fact, no country has a higher TB burden than India, which accounts for a quarter of the 10 million global TB cases and 1.4 million TB deaths each year.1
Even before the pandemic, the cascade of TB care in India has been leaky,2 with long diagnostic delays,3 complex care pathways,4 poor quality of TB care in public as well as private health sectors2 5 and high TB case fatality.6 7
While the COVID-19 pandemic did not escalate in India until May 2020, by early November, India has reported over 8 million cases of COVID-19, with over 125 000 deaths. As the pandemic continues to escalate, the healthcare system is falling apart under the stress. India’s economy (GDP) contracted by 24% in the April–June period in 2020.8
While the public health system is collapsing under the stress of the growing COVID-19 caseload, the private healthcare system is becoming expensive and challenging to access.9 In both sectors, non-Covid-19 conditions are getting little attention.10 11
When India went into a stringent lockdown on March 25, anecdotal evidence suggested that citizens were having difficulty accessing routine health services.10 A large part of the health administrative machinery had to be diverted in identifying and containing COVID-19 cases, many hospitals were designated as ‘COVID-19 only’ and others restricted routine services for fear of an infected patient causing an outbreak.
Additionally, the complete closure of public and most private transport made travel to health facilities difficult, and horror stories of patients with chronic conditions dying before they could make it to a doctor emerged in the media. Hundreds of thousands of migrants were forced to walk hundreds of miles back to their homes, and they received little by way of medical care. Tests, medicine refills and medical consultations are essential activities for patients but were severely disrupted due to lack of transportation, lockdown measures and an overwhelmed health system.10
Large-scale disruption of TB and general health services
Official data on the extent of health service disruptions have been harder to come by. The National Health Mission’s Health Management Information System (NHM-HMIS),12 an administrative database, aims to collect and publish updated data from over 250 000 health facilities across the country nearly daily. The majority of the NHM-HMIS reporting facilities are in rural areas and are government-run, and their services range from immunisations and the distribution of contraceptives to the treatment of cancer, including all age groups, and both communicable and non-communicable disease treatment.
After the data for March 2020, summarised in an Indian newspaper in late April,10 the NHM-HMIS reported no new data for the next 3 months. In late August, data for April, May and June finally became available, and it laid bare a worrying disruption of all health services.11 In particular, the data show serious disruption in access to the prevention, monitoring and treatment of TB, India’s biggest infectious disease killer.
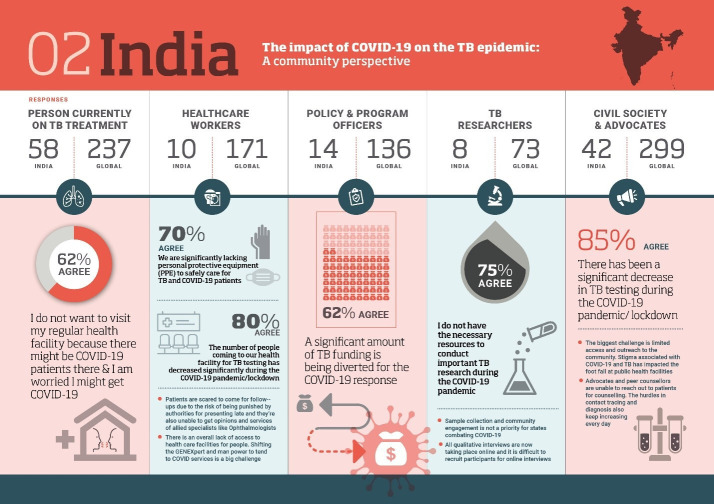
In March 2020, over 260 000 fewer children received the BCG vaccine that provides protection against childhood TB than in January 2020 (figure 1). The decline in April was even sharper—just half as many children received the BCG vaccine in April 2020 as in January 2020. These declines were also evident when the numbers are compared with the same months of the previous year. In May, there was some evidence of an improvement, but the numbers for both May and June were a long way from those earlier in the year or in previous years.
Figure 1.
Routine BCG immunisation data from India’s National Health Mission’s Health Management Information System (NHM-HMIS) for the January to June 2020 period, in comparison to similar data for 2019. Source: National Health Mission’s Health Management Information System (NHM-HMIS).12
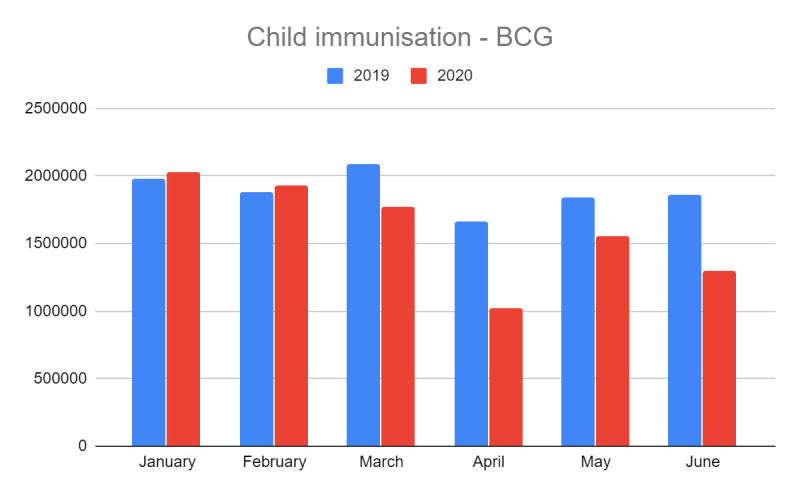
The number of patients with TB registered as being on treatment (captured in the NHM data as ‘DOTS patients’) in April 2020 fell to just half the February levels (figure 2). By June 2020, over 23 000 fewer patients had completed the TB therapy successfully than in January 2020 (figure 2).
Figure 2.
Number of patients with TB registered on DOTS and completed treatment, in India’s National Health Mission’s Health Management Information System (NHM-HMIS) for the January to June 2020 period, in comparison to similar data for 2019. Source: National Health Mission’s Health Management Information System (NHM-HMIS).12 TB, tuberculosis.
Across the country, the number of persons admitted for inpatient treatment fell for many diseases including malaria, dengue and TB.11 In June 2020, the number of people admitted for inpatient TB treatment in these facilities fell to less than a third of the number in June 2019.
Given the scale of administrative disruption, data quality is always a concern, as shown by the reports of the underestimation of COVID-19 deaths in the country.13 While the NHM-HMIS typically includes updated data on the number of facilities reporting this information, the government has not released this data since April onwards, making it difficult to estimate the scale of missed data, if any. However, data from March suggest that unreported data cannot fully explain these numbers—there were in fact more health facilities reporting data in March 2020 than there were in March 2019. Given that the data for April 2020 only confirmed the trend established in March, it is unlikely that the trends in figure 1 can be fully explained by missing data.
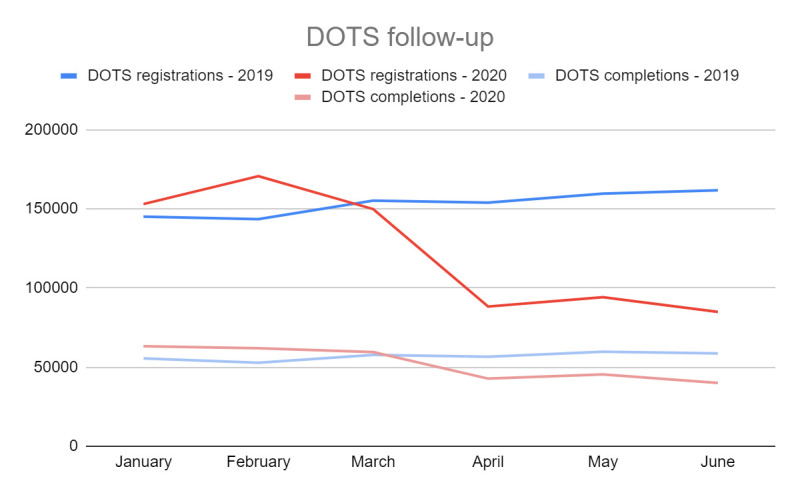
Other official data confirm the NHM trends for TB. Data from the Nikshay database,14 15 India’s national TB case notification system, show that notifications fell most sharply in April, and then revived somewhat in the months after. Figure 3 shows the Nikshay TB case notification data for the April to August 2020 period, in comparison to similar data for 2019. In August 2020, case notifications were down by nearly 50% compared with the same month in 2019. TB notifications declined in both the public and private sectors; at the beginning of the lockdown, the decline was even more severe in the private sector.
Figure 3.
Data from Nikshay TB notification system by India’s National TB Elimination Programme on TB for the April to August 2020 period, in comparison to similar data for 2019. Source: Nikshay, Central TB Division, National TB Elimination Programme.14 TB, tuberculosis.
Taking the NHM and Nikshay trends together, there is little doubt that TB services are seriously disrupted in India, and the disruptions extend over several months, rather than just weeks. The pandemic stress, coupled with the pre-existing stigma around TB, has made matters worse for patients. This has severely affected the treatment adherence in some patients, increasing the risk of drug-resistant disease and mortality.
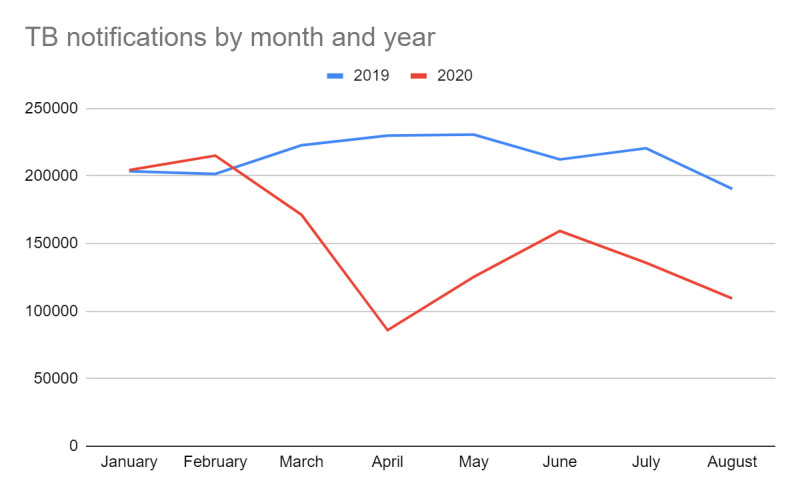
Disruptions to TB services extend well beyond India.16 On 15 September 2020, more than 10 civil society groups and global networks released the results of a large survey done, to document the impact of the COVID-19 pandemic on TB services and stakeholders. The results show that COVID-19 has had an enormous impact on the number of people seeking and receiving healthcare for TB.17 Figure 4 is a summary of the key results for India, from this civil society-led survey.
Figure 4.
Key results for India from a large civil society-led survey on the impact of COVID-19 on the TB epidemic. Source: report on ‘The impact of COVID-19 on the TB epidemic: A community perspective’.17
Now that India is dealing with a large-scale syndemic of TB and COVID-19, we need to anticipate and prevent poor outcomes among TB-affected persons as well as the possibility of increased spread of infection within households and close contacts because social distancing and masking are unlikely to be feasible within families and overcrowded, impoverished communities.
The stigma around TB is well recognised. Stigma around COVID-19 is also emerging as a concern now. People are hesitant to get tested for the fear of being tagged or quarantined. And because TB and COVID-19 have similar symptoms (cough and fever), stigma could delay the diagnosis of both conditions. Underdiagnosis and undernotification of both infections are the norms, not the exception.
Delayed TB diagnosis and treatment might substantially increase TB mortality in the future. A modelling analysis by the Stop TB Partnership and partners suggests that each month of lockdown in India could cause an additional 40 000 deaths over the next 5 years.18 Another model estimate suggests that a 59% reduction in TB case detection between the end March and May 2020 may result in an estimated additional 87 711 TB deaths in 2020.19
How can India tackle the syndemic of TB and COVID-19?
A lot depends on how long service disruptions will continue in India and how quickly essential health services can be ramped up.20 We hope the Indian government will find a way to restart and ramp up all essential health services, especially routine immunisation, TB diagnosis and treatment.20 Some states in India have done better than others in preserving routine health services,21 and other states must learn from their experience.
In September 2020, the National TB Elimination Programme (NTEP) announced a Rapid Response Plan to mitigate the impact of COVID-19 Pandemic on TB Epidemic and NTEP activities.15 The plan includes bi-directional TB-Covid-19 screening, intensified case finding, replacement of sputum smears with rapid molecular testing, home-based sample collection and delivery of TB medicines, and modification of the DOTS approach to include digital adherence technologies, call centres and family members to provide treatment support.
We applaud this rapid response plan and call for its full and rapid implementation. But we are yet to see data on whether NTEP has been allocated sufficient funds by the Indian government to fully implement the rapid response plan. With the Indian economy shrinking and with the ongoing diversion of funds to COVID-19 response, we worry that TB funding will decrease, rather than increase.16
The first pressing priority is to catch-up on all the missed patients—actively find over half a million persons with TB who were missed during the past 6 months and offer them TB treatment. Precision public health approaches for TB have shown that employed men who problem-drink and smoke are a prime target for interventions in urban India.22 Reducing delays in care seeking in this group of ‘missing men’23 is critical for catching up on TB case notifications.
There are several innovative apps now available for COVID-19, and some of them could be repurposed to also nudge people with TB symptoms to seek care, for increasing TB notifications and for contact tracing for both TB and COVID-19. This might also help with real-time data dashboards and geospatial trackers on TB, just as we have several dashboards and trackers for COVID-19.
Even as existing molecular platforms such as GeneXpert and TrueNAT are being repurposed for COVID-19 testing, it is critical to not stop TB testing. In particular, the TB programme must continue running the Xpert MTB/RIF TB test bacause this test is critical for early detection of drug-resistant TB.24
There are now digital X-rays with artificial-intelligence solutions that can rapidly screen for both TB and COVID-19. In urban India, X-rays are widely available and could be used to triage people with respiratory symptoms.
Novel sample collection methods should be tried out for both COVID-19 and TB, including drive-by sample collection sites, at-home collection, collection via community health workers and engagement of neighbourhood private laboratories. The national TB helpline should be strengthened, and patients should have a choice of texting, calling, emailing or engaging through social media—whatever is convenient to them.
In fact, India has announced a plan for bi-directional screening, with COVID-19 screening of all diagnosed patients with TB and TB screening for all Covid-19-positive patients.15 This plan, however, will require substantially higher capacity for molecular testing and serious financial investment, given the massive numbers of TB and COVID-19 cases in the country. If approximately 200 000 notified patients with TB need COVID-19 testing every month and if approximately 100 000 new patients with COVID-19 are being reported every day, the numbers add up to millions of TB and COVID-19 molecular tests each month. Because COVID-19 testing is much harder to access than TB testing, it is critical to make sure that COVID-19 testing does not become a bottleneck for accessing TB testing services.
There is tremendous innovation ongoing to develop and deploy rapid antigen tests for COVID-19 as molecular testing capacity is scarce in many settings.25 If rapid tests can be developed and rolled out so quickly for COVID-19, there is no reason to think it cannot be done for TB.
Where possible, treatment support could be done remotely using telemedicine and digital adherence technologies such as 99DOTS, smart pillboxes and video DOT.26 Medicine vending machines and e-pharmacies that can deliver medicines to homes of patients are other approaches worth trying. Community-based groups, including TB survivors, are closer to patients than government staff and could be engaged to provide patient support via WhatsApp, FaceBook and mobile phones.
Because injectable TB drugs are very challenging during this crisis, it is important to adopt the WHO-recommended all-oral, shorter drug regimens for drug-resistant TB. To avert a big increase in paediatric TB, it is important to increase BCG vaccination coverage and catch up on all the missed BCG and other vaccinations in the past 6 months.
Infection control has received tremendous attention during this pandemic, including widespread use of personal protection equipment, use of face masks, safe disposal of sputum and physical distancing. Greater use of such infection control measures can help reduce TB transmission.
Malnutrition is a huge driver of the TB epidemic in India, and India’s economic collapse during COVID-19 is pushing millions into extreme poverty and worsening malnutrition. Addressing these key social determinants of TB will be critical for ending TB in India.27 Experts have suggested enhanced food rations through India’s public distribution system, as well as direct cash transfers to the poor as a way of dealing with this immediate crisis.19 The pandemic has demonstrated the critical importance of sick pay as a safety net. All patients with TB in India deserve sick pay to help them get through the long and difficult treatment period.
In the longer term, we endorse the suggestions of Bhargava and colleagues27 who argue that TB elimination in India will need ‘a pro-poor model of patient-centred care inclusive of nutritional, psychosocial and financial support, universal health coverage and social protection; and convergence with multisectoral efforts to address poverty, undernutrition, unsafe housing and indoor pollution’.
Lastly, the pandemic has clearly exposed major fragility in India’s underfunded public health system and an unregulated, potentially exploitative private health system. India cannot achieve its true potential by spending just 1.5% of its Gross Domestic Product (GDP) on health. India needs to strengthen the public health system while simultaneously regulating and engaging with the private health sector to deliver quality, affordable care.28 In particular, engagement of the private health sector is critical for TB as nearly half of India’s TB cases are managed by private providers.29 30 Without leveraging both sectors, India cannot meet the surging health needs of over 1.3 billion people.
Acknowledgments
The authors used publicly available data (already reported in the media) for displaying the impact of COVID-19 on tuberculosis services. No patient data were obtained or analysed, and no ethics approvals were sought.
Footnotes
Handling editor: Seye Abimbola
Twitter: @paimadhu
Contributors: SR, SR and MP conceived the analysis. SR collected and verified the data. SR and MP wrote the initial draft. All authors revised and approved the final version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: MP is on the editorial board of BMJ Global Health. He has no financial or industry conflicts.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article.
References
- 1.World Health Organization Global tuberculosis report 2020. Geneva: WHO, 2020: 1–232. [Google Scholar]
- 2.Subbaraman R, Nathavitharana R, Satyanarayana S, et al. The Tuberculosis Cascade of Care in India’s Public Sector: Recent Estimates and Gaps in Knowledge. PLoS Med 2016;13:e1002149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sreeramareddy CT, Qin ZZ, Satyanarayana S, et al. Delays in diagnosis and treatment of pulmonary tuberculosis in India: a systematic review. Int J Tuberc Lung Dis 2014;18:255–66. 10.5588/ijtld.13.0585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mistry N, Rangan S, Dholakia Y, et al. Durations and delays in care seeking, diagnosis and treatment initiation in uncomplicated pulmonary tuberculosis patients in Mumbai, India. PLoS One 2016;11:e0152287. 10.1371/journal.pone.0152287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kwan A, Daniels B, Saria V, et al. Variations in the quality of tuberculosis care in urban India: a cross-sectional, standardized patient study in two cities. PLoS Med 2018;15:e1002653. 10.1371/journal.pmed.1002653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huddart S, Svadzian A, Nafade V, et al. Tuberculosis case fatality in India: a systematic review and meta-analysis. BMJ Glob Health 2020;5:e002080. 10.1136/bmjgh-2019-002080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pai M, Correa N, Mistry N, et al. Reducing global tuberculosis deaths-time for India to step up. Lancet 2017;389:1174–6. 10.1016/S0140-6736(17)30790-0 [DOI] [PubMed] [Google Scholar]
- 8.The Economist India’s economy shrinks by a quarter as covid-19 gathers pace, 2020. Available: https://www.economist.com/asia/2020/09/03/indias-economy-shrinks-by-a-quarter-as-covid-19-gathers-pace [Accessed 10 Oct 2020].
- 9.Thiagarajan K. Covid-19 exposes the high cost of India's reliance on private healthcare. BMJ 2020;370:m3506. 10.1136/bmj.m3506 [DOI] [PubMed] [Google Scholar]
- 10.Rukmini S. How covid-19 response disrupted health services in rural India. live MINT, 2020. Available: https://www.livemint.com/news/india/how-covid-19-response-disrupted-health-services-in-rural-india-11587713155817.html [Accessed 6 Sept 2020].
- 11.Rukmini S. COVID-19 Disrupted India’s Routine Health Services. IndiaSpend, 2020. Available: https://www.indiaspend.com/covid-19-disrupted-indias-routine-health-services/ [Accessed 6 Sept 2020].
- 12.Ministry of Health and Family Welfare; Government of India Health management information system (HMIS), a digital initiative under national health mission (NHM), 2020. Available: https://hmis.nhp.gov.in/#!/ [Accessed 6 Sept 2020].
- 13.Chatterjee P. Is India missing COVID-19 deaths? Lancet 2020;396:657. 10.1016/S0140-6736(20)31857-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Central TB Division Ministry of health and family welfare; government of India. Nikshay, a web enabled patient management system for TB control under the National tuberculosis elimination programme. New Delhi: Government of India, 2020. https://reports.nikshay.in/Reports/TBNotification [Google Scholar]
- 15.Central TB Division; Ministry of Health & Family Welfare; Government of India Rapid response plan to mitigate impact of COVID-19 pandemic on TB epidemic and national TB elimination program (NTEP) activities in India, 2020. Available: https://tbcindia.gov.in/showfile.php?lid=3551 [Accessed 13 Sept 2020].
- 16.Pai M. Tuberculosis and Covid-19: fighting a deadly Syndemic, 2020. Available: https://www.forbes.com/sites/madhukarpai/2020/09/26/tuberculosis-and-covid-19-fighting-a-deadly-syndemic/#480c876624c5 [Accessed 10 Oct 2020].
- 17.ACTION; Global Coalition of TB Activists; Global TB Caucus; KANCO; McGill International TB Centre; Results; Stop TB Partnership; TB People; TB PPM Learning Network; We are TB The impact of COVID-19 on the TB epidemic: a community perspective, 2020. Available: https://spark.adobe.com/page/xJ7pygvhrIAqW/ [Accessed 13 Sept 2020].
- 18.Stop TB Partnership; Imperial College; Avenir Health; Johns Hopkins University; USAID The potential impact of the Covid-19 response on tuberculosis in high-burden countries: a modelling analysis. Geneva: Stop TB Partnership, 2020. http://www.stoptb.org/assets/documents/news/Modeling%20Report_1%20May%202020_FINAL.pdf [Google Scholar]
- 19.Bhargava A, Shewade HD. The potential impact of the COVID-19 response related lockdown on TB incidence and mortality in India. Indian J Tuberc 2020. 10.1016/j.ijtb.2020.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vasquez NA, Pande T, Heitkamp P, et al. Ensuring continuity of tuberculosis care during the covid-19 crisis. BMJ opinion 2020, 2020. Available: https://blogs.bmj.com/bmj/2020/06/25/ensuring-continuity-of-tuberculosis-care-during-the-covid-19-crisis/ [Accessed 6 Sept 2020].
- 21.Dreze J, Paikra VK. The uneven decline of health services across states during Lockdown, 2020. Available: https://thewire.in/health/covid-19-lockdown-health-services-decline [Accessed 10 Oct 2020].
- 22.Helfinstein S, Engl E, Thomas BE, et al. Understanding why at-risk population segments do not seek care for tuberculosis: a precision public health approach in South India. BMJ Glob Health 2020;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chikovore J, Pai M, Horton KC, et al. Missing men with tuberculosis: the need to address structural influences and implement targeted and multidimensional interventions. BMJ Glob Health 2020;5. 10.1136/bmjgh-2019-002255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Albert H, Nathavitharana RR, Isaacs C, et al. Development, roll-out and impact of Xpert MTB/RIF for tuberculosis: what lessons have we learnt and how can we do better? Eur Respir J 2016;48:516–25. 10.1183/13993003.00543-2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization Global partnership to make available 120 million affordable, quality COVID-19 rapid tests for low- and middle-income countries. Geneva: WHO, 2020. https://www.who.int/news-room/detail/28-09-2020-global-partnership-to-make-available-120-million-affordable-quality-covid-19-rapid-tests-for-low-and-middle-income-countries [Google Scholar]
- 26.Subbaraman R, de Mondesert L, Musiimenta A, et al. Digital adherence technologies for the management of tuberculosis therapy: mapping the landscape and research priorities. BMJ Glob Health 2018;3:e001018. 10.1136/bmjgh-2018-001018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bhargava A, Bhargava M, Juneja A. Social determinants of tuberculosis: context, framework, and the way forward to ending TB in India. Expert Rev Respir Med 2020:1–17. 10.1080/17476348.2021.1832469 [DOI] [PubMed] [Google Scholar]
- 28.Pai M, Das J. How can India address big surge for health care after coronavirus lockdown? Devex, 2020. Available: https://www.devex.com/news/opinion-how-can-india-address-big-surge-for-health-care-after-coronavirus-lockdown-97382 [Accessed 6 Sept 2020].
- 29.Stallworthy G, Dias HM, Pai M. Quality of tuberculosis care in the private health sector. J Clin Tuberc Other Mycobact Dis 2020;20:100171. 10.1016/j.jctube.2020.100171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization & Stop TB Partnership Public-Private mix for TB prevention and care: a roadmap, 2018. Available: http://www.who.int/tb/publications/2018/PPMRoadmap/en/ [Accessed 2 Dec 2018].