Abstract
Background
Helicobacter cinaedi is rarely identified as a cause of infected aneurysms; however, the number of reported cases has been increasing over several decades, especially in Japan. We report three cases of aortic aneurysm infected by H. cinaedi that were successfully treated using meropenem plus surgical stent graft replacement or intravascular stenting. Furthermore, we performed a systematic review of the literature regarding aortic aneurysm infected by H. cinaedi.
Case presentation
We present three rare cases of infected aneurysm caused by H. cinaedi in adults. Blood and tissue cultures and 16S rRNA gene sequencing were used for diagnosis. Two patients underwent urgent surgical stent graft replacement, and the other patient underwent intravascular stenting. All three cases were treated successfully with intravenous meropenem for 4 to 6 weeks.
Conclusions
These cases suggest that although aneurysms infected by H. cinaedi are rare, clinicians should be aware of H. cinaedi as a potential causative pathogen, even in immunocompetent patients. Prolonged incubation periods for blood cultures are necessary for the accurate detection of H. cinaedi.
Keywords: Helicobacter cinaedi, Infected aneurysm, Japan, Case report
Background
Helicobacter cinaedi is a gram-negative spiral rod that was first discovered in the rectal culture from a man who had had sex with a man with proctitis [1]. H. cinaedi was thought to cause infection only in immunocompromised individuals; however, it has also been observed as a causative pathogen in immunocompetent patients [2–4]. H. cinaedi can cause bacteremia, skin and soft tissue infection, and arterial infection [5, 6].
Although infected (mycotic) aortic aneurysms are not common, they are difficult to treat and are associated with high morbidity and mortality. Mortality has been reported to be greater than 20%, usually attributable to delays in diagnosis and subsequent complications, such as rupture and sepsis [7–9]. Common pathogens include Staphylococcus aureus, Streptococcus pneumoniae, and non-typhoidal Salmonella followed by other gram-negative organisms such as Escherichia coli, Klebsiella, and Pseudomonas spp. [10, 11]. Mycobacterium spp., Treponema palladium, and Chlamydophila spp. have also been reported as causative pathogens, although rarely [12, 13].
Herein, we report three cases of aortic aneurysm infected by H. cinaedi that were successfully treated using meropenem plus surgical stent graft replacement or intravascular stenting. Furthermore, we performed a systematic review of the literature regarding aortic aneurysm infected by H. cinaedi.
Case series
Case 1
A 77-year-old immunocompetent man with a past medical history of hypertension and dyslipidemia presented to our department with a fever up to 38 °C and progressive left pleuritic chest pain for 2 weeks. On admission, the patient was not in acute distress and had a temperature of 37.6 °C, blood pressure of 143/76 mmHg, heart rate of 67/min, respiratory rate of 16/min, and oxygen saturation of 95% on room air. The patient was noted to have coarse crackles over the left lower lobe of the lung and tenderness of the lower abdomen without any rebound or guarding. Laboratory data showed a mildly elevated white blood cell (WBC) count of 8100/μL and C-reactive protein (CRP) of 15.0 mg/dL. Contrast-enhanced computed tomography (CT) chest-abdomen-pelvis examination demonstrated an aneurysm (30 × 42 mm) of the aortic arch with suggestion of a Stanford B dissection involving the descending aorta on a background of abdominal vessel wall thickening (Fig. 1), increased thickness of bilateral common iliac arteries (20 × 25 mm), and a 1 cm diameter low-density area in the spleen, compatible with infected vasculitis and splenic abscess.
Fig. 1.

Sagittal contrast-enhanced CT chest-abdomen-pelvis image demonstrates aorta wall thickening with pseudoaneurysm of the distal aortic arch and suggestion of Stanford type B dissection involving the descending aorta, with abnormal fluid extending to the level of the diaphragm
We initiated ceftriaxone 2 g intravenously (IV) every 24 h, vancomycin IV 1 g every 12 h, and minocycline IV 100 mg every 12 h. Due to the active infection, we opted for conservative management without immediate surgery. Despite empirical antimicrobial therapy, the patient had progressive lower abdominal pain on hospital day 4, and a follow-up CT scan demonstrated enlargement of the aortic arch aneurysm (33 × 49 mm) and worsening aortic dissection. Therefore, total arch replacement was urgently performed on the same day. After surgery, the patient gradually improved. On hospital day 7, gram-negative spiral rods were cultured from blood samples obtained on admission (aerobic bottle, BacT/ALERT [bioMérieux, Inc., Durham, NC]). The empirical therapy was changed to meropenem 1 g IV every 6 h. Final blood culture results revealed H. cinaedi. The minimum inhibitory concentrations (MICs) measured by Etest (bioMérieux) for this strain were as follows: meropenem 0.008 μg/mL, penicillin G > 32 μg/mL, piperacillin/tazobactam 16 μg/mL, cefotaxime > 32 μg/mL, and levofloxacin > 32 μg/mL. Tissue culture of the infected aneurysm was negative. We continued meropenem for 6 weeks after surgery. Follow-up CT revealed resolution of the vasculitis involving the common iliac arteries without evidence of infection. As there are limited data on oral antimicrobials against H. cinaedi, we consulted the data for H. pylori. As faropenem was found to have good antimicrobial action against H. pylori in vitro [14], the patient was discharged on hospital day 46 with oral faropenem. He continued oral faropenem for 1 year, and his general status was stable at a 4-year follow-up.
Case 2
An 85-year-old woman with a past medical history of polymyalgia rheumatica treated with oral prednisolone 5 mg every other day and hypertension presented to our hospital for fever up to 38 °C and epigastric pain for 1 month that had not responded to a short course of oral cefcapene pivoxil. On admission, the patient was not in acute distress with a temperature of 36.9 °C, blood pressure of 158/48 mmHg, heart rate of 60/min, respiratory rate of 18/min, and oxygen saturation of 98% on room air. The patient was noted to have tenderness over the epigastric area but no rebound or guarding. Laboratory data showed an elevated WBC of 10,000/μL, (neutrophils 75%) and CRP of 5.27 mg/dL. Contrast-enhanced CT chest-abdomen-pelvis demonstrated increased wall thickness of the descending aorta (35 × 32 mm) and low attenuation surrounding the aorta, compatible with an infected aortic aneurysm.
We empirically initiated ceftriaxone 2 g IV every 24 h. Her fever subsided and general status gradually improved. On hospital day 5, gram-negative spiral rods were cultured from blood samples obtained at admission (aerobic bottle, BacT/ALERT [bioMérieux]) (Fig. 2). Empirical therapy was changed to meropenem 1 g IV every 6 h. On hospital day 7, 16S rRNA gene sequencing confirmed H. cinaedi. The MICs for this strain tested using the same method as for Case 1 were as follows: meropenem 0.008 μg/mL, ampicillin 32 μg/mL, cefotaxime > 32 μg/mL, and levofloxacin > 32 μg/mL. Follow-up CT on hospital day 17 revealed that the infected aneurysm had diminished (33 × 31 mm). Subsequently, meropenem was switched to oral faropenem on hospital day 44. Follow-up CT on hospital day 62 revealed enlargement of the infected aneurysm (35 × 42 mm). Thereafter, urgent intravascular stenting was performed. After this procedure, the patient improved and was discharged on day 76 without further complications. The patient continued oral faropenem and was clinically stable without any sign of recurrence at the 6-year follow-up.
Fig. 2.
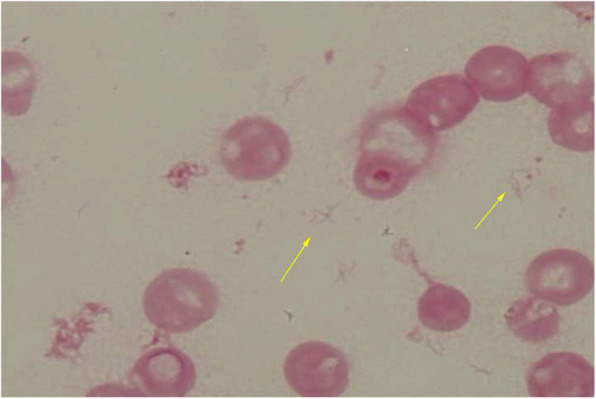
Photomicrograph of Gram stain demonstrates gram-negative spiral rods, which grew on hospital day 5 from blood cultures taken at admission
Case 3
A 72-year-old immunocompetent man with a past medical history of hypertension and benign prostate hypertrophy presented to the emergency room with difficult and painful urination for 10 days and lower abdominal pain for 3 days followed by fever up to 38 °C 1 day prior to admission. On admission, the patient was not in acute distress with a temperature of 37.8 °C, blood pressure of 120/70 mmHg, heart rate of 89/min, respiratory rate of 18/min, and oxygen saturation of 98% on room air. The patient was noted to have tenderness of the lower abdomen without any rebound or guarding. The prostate was elastic, soft, swollen, and tender. Laboratory data showed an elevated WBC of 9800/μL, (neutrophils 78%) and CRP of 18.9 mg/dL. Contrast-enhanced CT chest-abdomen-pelvis demonstrated increased wall thickness of the descending aorta with a wild, multilobulated appearance with focal outpouching (30 × 31 mm) and fat stranding surrounding the aorta (Fig. 3), compatible with an infected aortic aneurysm.
Fig. 3.

Coronal contrast-enhanced CT abdomen image demonstrates irregular wall thickening of the descending aorta having a wild, multilobulated appearance with surrounding soft tissue stranding
We empirically started cefepime 1 g IV every 8 h, vancomycin IV 1 g every 12 h, and minocycline IV 100 mg every 12 h. On hospital day 12, the patient complained of worsening of lower abdominal pain, and a follow-up CT scan revealed enlargement of the aneurysm (36 × 35 mm). He underwent urgent abdominal aorta replacement on the same day. Tissue culture of the abdominal aneurysm was negative; however, 16S rRNA gene sequencing identified H. cinaedi from the tissue. We could not perform the susceptibility testing because H. cinaedi isolates could not be obtained from blood and tissue culture. The empirical therapy was changed to meropenem 1 g IV every 6 h. He was continued on meropenem for 4 weeks after surgical intervention and was discharged on hospital day 47 with oral faropenem. The patient continued oral faropenem for 3 years and was clinically stable without any sign of recurrence at the 5-year follow-up.
Systematic review
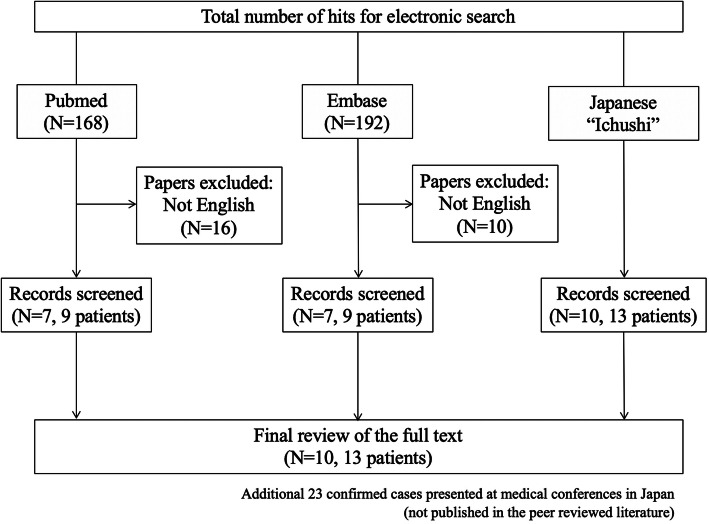
Two authors independently reviewed the titles and abstracts of database records, retrieved full texts for an eligibility assessment, and extracted data from these cases. A literature search was conducted in both the PubMed database (up to November 2019) using the keywords ((cinaedi) AND ((“Vascular Diseases”[Mesh]) OR (aneurysm*[TW]))) OR ((“Aneurysm, Infected”[Mesh]) AND (“Helicobacter”[Mesh] OR “Helicobacter Infections”[Mesh])) and the Embase database using the keywords (cinaedi OR ‘helicobacter cinaedi’/exp) AND (‘infected aneurysm’/exp. OR ‘aortic aneurysm’/exp. OR ‘aneurysm’) (Fig. 4). Knowing that there were several reports in Japanese papers, we have included those published only in Japanese in order to further understand the clinical characteristics of the disease by presenting more confirmed cases. In order to search for articles in Japanese, we used Ichushi, a major Japanese database, using the keywords ((cinaedi/AL)) or (“Helicobacter cinaedi”/TH)) and (((aneurysm [Japanese]/TH or aneurysm/AL)) or ((Vascular diseases [Japanese]/TH or Vascular diseases/AL)) or ((Artery [Japanese]/TH or Artery [Japanese]/AL))).
Fig. 4.
Flow chart depicts the systematic review process of this study
We found ten papers describing thirteen cases of infected aneurysms due to H. cinaedi, all from Japan [6, 15–23]. Additionally, there were twenty-three confirmed cases presented in Japan at medical conferences, though not published in the peer reviewed literature. However, for these cases detailed patient information was not available. The clinical characteristics of the thirteen published cases, including our three cases, are shown in Table 1. Among them, the most common site of infection was the abdominal aorta (at least nine patients). Only two patient received oral corticosteroids; the others were immunocompetent. Regarding management, except for two cases with conservative management, the remaining eleven patients underwent in situ grafting, extra-anatomical bypass, or intravascular stent. Except one patient with fungal infection, all patients were successfully treated without further complications.
Table 1.
Clinical characteristics of cases of aortic aneurysm infected with Helicobacter cinaedi
| No | Case reference | Age (years) | Sex | Published year | Underlying diseases | Chief complaint | Site of infection | Management | Antimicrobial used | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | R. Kakuta | 64 | Male | 2014 | Hypertension | Fever, back pain | Infrarenal abdominal, L common iliac, R internal iliac, and L femoral artery | In situ grafting | Sulbactam/ampicillin 3 g/day and minocycline 100 mg/day for 25 days followed by oral amoxicillin 1500 mg/day and minocycline 200 mg/day | Complete symptom resolution |
| 2 | R. Kakuta | 59 | Male | 2014 | None | Fever, abdominal pain | Infrarenal abdominal aorta | In situ grafting | Piperacillin/tazobactam 4.5 g/day for 28 days followed by oral amoxicillin 1500 mg/day and minocycline 200 mg/day until follow-up visit | Complete symptom resolution |
| 3 | R. Kakuta | 62 | Male | 2014 | History of myocardial infarction | Low back pain | Infrarenal abdominal aorta | In situ grafting | Doripenem, 1.5 g/day for 28 days followed by oral amoxicillin 1500 mg/day and minocycline 200 mg/d, until follow-up visit | Complete symptom resolution |
| 4 | K. Niimi | 60 | Female | 2014 | Rheumatic arthritis on prednisolone, end-stage kidney disease on hemodialysis, MDR-TB | Fever, left inguinal pain | L femoral artery | Resection of the aneurysm and debridement | Ceftazidime 1 g/day for 5 days followed by imipenem-cilastatin 500 mg/day for 10 days, ampicillin/sulbactam 3 g/day for 2 weeks, and oral ampicillin/sulbactam for 1 month | Complete symptom resolution |
| 5 | T. Seto | 39 | Male | 2014 | None | Fever, chest pain | Right coronary artery (pericoronary pseudotumor) | Conservative | Ceftriaxone for 2 weeks | Complete symptom resolution |
| 6 | S. Unosawa | 79 | Male | 2015 | Hypertension | Back pain, left lower quadrant pain | Infrarenal abdominal aorta | In situ grafting with an omental wrapping | Ceftriaxone 2 g/day and gentamicin 120 mg/day, followed by sultamicillin 1250 mg/day | Complete symptom resolution |
| 7 | K. Nishida | 64 | Male | 2015 | None | Low back pain | Infrarenal abdominal aorta, L common iliac artery | In situ grafting | Meropenem and vancomycin for 8 weeks | Complete symptom resolution |
| 8 | M. Akiyama | 49 | Female | 2016 | History of myocardial infarction | Fever, back pain | Abdominal aorta, bilateral common iliac artery | In situ grafting with an omental wrapping | Piperacillin/tazobactam followed by oral amoxicillin, 1500 mg/day, and minocycline 200 mg/day for 3 months | Complete symptom resolution |
| 9 | J. Inagaki | 80 | Male | 2017 | None | Fatigue | Infrarenal abdominal aorta, bilateral common iliac artery | Extra-anatomical bypass | Meropenem and levofloxacin (dose not available) for 6 weeks followed by minocycline and rifampicin for more than 18 months | Complete symptom resolution with continued antimicrobials |
| 10 | K. Kushimoto | 68 | Male | 2017 | Hypertension, hyperuricemia | Fever, chest and back pain | Distal aortic arch, thoracic aorta | In situ grafting with an omental wrapping | Levofloxacin 250 mg/day for 19 days followed by minocycline 200 mg/day | Complete symptom resolution with continued antimicrobials |
| 11 | Y. Kanno | 73 | Male | 2018 | History of abdominal aortic aneurysm, colon polyp | Back pain | Abdominal aorta | Conservative first, followed by in situ grafting 3 months later |
Meropenem 3 g/day and vancomycin 1 g/day for 7 days followed by levofloxacin 500 mg/day for 5 days, and oral sultamicillin 1200 mg/day for 3 months (relapsed) ampicillin/sulbactam 6 g/day for 12 days followed by oral sultamicillin 1200 mg/day (duration not available) |
Complete symptom resolution |
| 12 | Y. Kanno | 72 | Male | 2018 | None | Fever | Thoracic aorta | In situ grafting | Meropenem 3 g/day and vancomycin 1 g/day followed by ampicillin/sulbactam 6 g/day | Deceased (fungal infection) |
| 13 | S. Nakao | 65 | Male | 2018 | None | Fever and right neck pain | R common carotid artery | Conservative |
(1st) Meropenem 6 g/day followed by ceftriaxone 4 g/day for 2 weeks and oral minocycline 200 mg/day for 2 weeks (2nd) Ceftriaxone 4 g/day for 2 weeks followed by oral ampicillin 1.5 g/day and doxycycline 400 mg/day for 6 weeks |
Complete symptom resolution |
| 14 | T. Matsuo | 77 | Male | 2020 | Hypertension | Fever and left chest pain | Aortic arch and bilateral common iliac artery | In situ grafting | Meropenem followed by faropenem 1200 mg/day for 1 year | Complete symptom resolution |
| 15 | T. Matsuo | 85 | Female | 2020 | Polymyalgia rheumatica and hypertension | Epigastric pain | Descending aorta | Intravascular stent | Meropenem followed by faropenem 1200 mg/day | Complete symptom resolution with continued antimicrobials |
| 16 | T. Matsuo | 72 | Male | 2020 | Hypertension and benign prostate hypertrophy | Fever and lower abdominal pain | Bilateral common iliac artery | In situ grafting | Meropenem followed by faropenem 1200 mg/day for 3 years | Complete symptom resolution |
L Left, R Right, MDR-TB Multidrug-resistant tuberculosis
Discussion and conclusions
This is the first systematic review of infected aortic aneurysms caused by H. cinaedi. The mechanisms underlying infected aortic aneurysms remain unknown. However, four main mechanisms have been hypothesized that result in infection of the arterial wall: 1) the development of infected aneurysms secondary to septic microemboli of the vasa vasorum, 2) extension from a contiguous infected focus, 3) hematogenous seeding of the intima during bacteremia originating from a distant infection, and 4) trauma to the arterial wall with contamination [24]. Recently, Araoka et al. reported that bacterial translocation from the intestinal tract could be a route that leads to H. cinaedi bacteremia [25]. The promotion of atherosclerosis by H. cinaedi has also been reported [26, 27]. In our three cases, none had evidence of infection with H. cinaedi at distal sites, extension from a contiguous infected focus, or a history of trauma; therefore, the development of infected aneurysms secondary to septic microemboli of the vasa vasorum or bacterial translocation from the intestinal tract were considered the most likely mechanisms.
There is a lack of data on susceptibility testing, and standard breakpoints of antimicrobial agents for H. cinaedi have not been defined. Previous studies reported that susceptibility testing for H. cinaedi isolates has been conducted using the agar dilution method [28, 29]. Low MIC values were generally reported for H. cinaedi strains for carbapenems, aminoglycosides, and tetracycline (MIC90 ≤ 1 μg/mL) [5, 30], moderate MIC values for ampicillin (MIC90 = 16 μg/mL), cefepime (MIC90 = 8 μg/mL), and ceftriaxone (MIC90 = 8 μg/mL) [5], and high MIC values for erythromycin (MIC90 > 64 μg/mL) [31]. Prior to 2000, low MICs of ciprofloxacin and macrolides were reported for H. cinaedi; however, the majority of H. cinaedi isolates have gained resistance since the early 2000s because of the increased use of these antimicrobials [30]. As the agar dilution method is not available in all institutes, the Etest could be an alternative method; however, it can be inaccurate because of the unclear edges around the growth inhibition zone [5]. Although there are no guidelines for recommended antimicrobial treatment, there has been varied used of beta-lactams such as penicillin, cephalosporin, and carbapenem [2, 32]. Monotherapy versus combination therapy has not been fully investigated. Further studies exploring the antimicrobial susceptibility profiles are warranted.
Except for one case, all of the reviewed cases underwent open repair (OR). OR is considered the gold standard with weak evidence supporting its superiority compared with endovascular aortic repair (EVAR). The optimal treatment of infected aneurysms remains unknown, although an increasing number of trials have reported EVAR as an alternative treatment for infected aortic aneurysms, with improved short-term survival compared with OR without the associated higher incidence of serious infection-related complications or reoperations [33]. In contrast, Luo et al. reported that persistent infection after EVAR does occur and is often fatal without surgical treatment [34]. The choice between OR or EVAR should be weighed against the risks and benefits for each patient.
The optimal duration of antimicrobial therapy for H. cinaedi infection also remains unknown. In addition to IV antimicrobials for at least 6 weeks after surgery, some experts recommend that patients continue oral antimicrobials after discharge for at least 6 months whereas others recommend lifelong therapy [8]. All of our patients continued antimicrobials for at least for 1 year.
Regarding the incidence and prevalence of H. cinaedi, all published reports of infected aneurysms caused by H. cinaedi are from Japan. The number of reports of H. cinaedi overall infection, including bacteremia and skin and soft tissue infection, has been increasing over the last 10 years, especially in Japan. It is thought that there are three main reasons for this. First, as H. cinaedi is becoming increasingly recognized in Japan, many institutions are extending the incubation period for blood cultures when clinicians suspect H. cinaedi infection. H. cinaedi usually grows slowly, and one clinical research study from Japan revealed that approximately 50% of H. cinaedi bacteremia would probably have been overlooked had the duration of monitored blood cultures been limited to 5 days [35]. After this report, many institutes extended the incubation period. Another hypothesis is that H. cinaedi may be related to Japanese-specific cultural behaviors such as eating raw fish as sushi and sashimi followed by colonization of H. cinaedi in the intestine. However, this is perhaps less likely given the increasing worldwide popularity of Japanese cuisine. Finally, some institutions have changed blood culture products, moving from BacT/ALERT to BACTEC (BD Diagnostics, Sparks, MD), and this could also be contributing to the increased detection of H. cinaedi [36]. New BacT/ALERT plus bottles that modify the antimicrobial-absorbing materials in the blood culture media could also have contributed to the improved detection [37, 38]. However, the true reason why H. cinaedi infections are increasing in Japan is as yet unknown. As these detections were made using the blood culture system described above for extended cultures and 16S rRNA gene sequencing in tissues, the sensitivity and specificity of the techniques for diagnosis and detection should be analyzed in the future. Furthermore, studies on the true mechanisms of H. cinaedi infections and its incidence and prevalence are warranted.
In summary, aortic aneurysms infected with H. cinaedi are rare and occur in immunocompetent as well as immunocompromised individuals. Clinicians should suspect H. cinaedi as a possible causative pathogen in patients with infected aortic aneurysms and extend the incubation period for blood cultures. The optimal choice of antimicrobials for H. cinaedi, the duration of therapy for infected aneurysms, and the optimal intervention regarding OR versus EVAR should be investigated in further studies.
Acknowledgments
We wish to thank Dr. Kiyofumi Okusu, Department of Microbiology, Tokyo Medical University, for performing the 16S rRNA sequencing and Dr. Emiko Hayashihara, National Institute of Infectious Diseases, for the susceptibility testing identification.
Abbreviations
- H. cinaedi
Helicobacter cinaedi
- WBC
White blood cell
- CRP
C-reactive protein
- CT
Contrast whole trunk computed tomography
- IV
Intravenously
- MIC
Minimum inhibitory concentration
- OR
Open repair
- EVAR
Endovascular aortic repair
- C. trachomatis
Chlamydia trachomatis
Authors’ contributions
The manuscript was seen and approved by all the authors and is not under consideration elsewhere. All the authors contributed to the work in this report. TM collected clinical data and wrote the initial draft of the manuscript. TM and FK performed the systematic review of the literature. NM, AM, AS, JS, DO, KA, MY, JI, KY, YM, YU, and KF supervised and edited the manuscript. The author(s) read and approved the final manuscript.
Funding
There were no sources of funding used in the conception, composition, editing, or submission of this manuscript.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patients in this case report. A copy of written consent is available for the journal.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fennel CL, Totten PA, Quinn TC, Patton DL, Holmes KK, Stamm WE. Characterization of campylobacter-like organisms isolated from homosexual men. J Infect Dis. 1984;149:58–66. doi: 10.1093/infdis/149.1.58. [DOI] [PubMed] [Google Scholar]
- 2.Kitamura T, Kawamura Y, Ohkusu K, Masaki T, Iwashita H, Sawa T, et al. Helicobacter cinaedi cellulitis and bacteremia in immunocompetent hosts after orthopedic surgery. J Clin Microbiol. 2007;45:31–38. doi: 10.1128/JCM.01507-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murata S, Suzuki H, Sakamoto S, Miki T, Rimbara E, Shibayama K, et al. Helicobacter cinaedi-associated vertebral osteomyelitis in an immunocompetent patient. Intern Med. 2015;54:3221–3224. doi: 10.2169/internalmedicine.54.4574. [DOI] [PubMed] [Google Scholar]
- 4.Shimizu Y, Gomi H, Ishioka H, Isono M. Refractory to treat Helicobacter cinaedi bacteremia with bilateral lower extremities cellulitis in an immunocompetent patient. IDCases. 2016;5:9–11. doi: 10.1016/j.idcr.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kawamura Y, Tomida J, Morita Y, Fujii S, Okamoto T, Akaike T. Clinical and bacteriological characteristics of Helicobacter cinaedi infection. J Infect Chemother. 2014;20:517–526. doi: 10.1016/j.jiac.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 6.Nakao S, Hagiya H, Kimura K, Mitsui T, Oyama A, Hongyo K, et al. Helicobacter cinaedi-associated carotid arteritis. Acta Med Okayama. 2018;72:189–192. doi: 10.18926/AMO/55861. [DOI] [PubMed] [Google Scholar]
- 7.Oderich GS, Panneton JM, Bower TC, Cherry KJ, Rowland CM, Noel AA, et al. Infected aortic aneurysms: aggressive presentation, complicated early outcome, but durable results. J Vasc Surg. 2001;34:900–908. doi: 10.1067/mva.2001.118084. [DOI] [PubMed] [Google Scholar]
- 8.Hsu R-B, Tsay Y-G, Wang S-S, Chu S-H. Surgical treatment for primary infected aneurysm of the descending thoracic aorta, abdominal aorta, and iliac arteries. J Vasc Surg. 2002;36:746–750. doi: 10.1067/mva.2002.126557. [DOI] [PubMed] [Google Scholar]
- 9.Moneta GL, Taylor LM, Yeager RA, Edwards JM, Nicoloff AD, McConnell DB, et al. Surgical treatment of infected aortic aneurysm. Am J Surg. 1998;175:396–399. doi: 10.1016/S0002-9610(98)00056-7. [DOI] [PubMed] [Google Scholar]
- 10.Marques da Silva R, Caugant DA, ERK E, Aas JA, Lingaas PS, Geiran O, et al. Bacterial diversity in aortic aneurysms determined by 16S ribosomal RNA gene analysis. J Vasc Surg. 2006;44:1055–1060. doi: 10.1016/j.jvs.2006.07.021. [DOI] [PubMed] [Google Scholar]
- 11.Brossier J, Lesprit P, Marzelle J, Allaire E, Becquemin J-P, Desgranges P. New bacteriological patterns in primary infected aorto-iliac aneurysms: a single-Centre experience. Eur J Vasc Endovasc Surg. 2010;40:582–588. doi: 10.1016/j.ejvs.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 12.Canaud L, Marzelle J, Bassinet L, Carrié A-S, Desgranges P, Becquemin J-P. Tuberculous aneurysms of the abdominal aorta. J Vasc Surg. 2008;48:1012–1016. doi: 10.1016/j.jvs.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 13.Cruz RP, Marrone LCP, Marrone ACH. Chronic syphilitic aortic aneurysm complicated with chronic aortic dissection. Am J Surg. 2010;200:e64–e66. doi: 10.1016/j.amjsurg.2010.02.017. [DOI] [PubMed] [Google Scholar]
- 14.Ogura K, Mitsuno Y, Maeda S, Hirata Y, Yanai A, Shibata W, et al. Efficacy and safety of faropenem in eradication therapy of Helicobacter pylori. Helicobacter. 2007;12:618–622. doi: 10.1111/j.1523-5378.2007.00551.x. [DOI] [PubMed] [Google Scholar]
- 15.Kakuta R, Yano H, Kanamori H, Shimizu T, Gu Y, Hatta M, et al. Helicobacter cinaedi infection of abdominal aortic aneurysm, Japan. Emerg Infect Dis. 2014;20:1942–1945. doi: 10.3201/eid2011.140440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Unosawa S, Niino T. An infected abdominal aortic aneurysm caused by Helicobacter cinaedi. Ann Vasc Dis. 2015;8:318–320. doi: 10.3400/avd.cr.15-00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nishida K, Iwasawa T, Tamura A, Lefor AT. Infected abdominal aortic aneurysm with Helicobacter cinaedi. Case Rep Surg. 2016;2016:1396568. doi: 10.1155/2016/1396568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akiyama M, Hayatsu Y, Sakatsume K, Fujiwara H, Shimizu T, Akamatsu D, et al. Graft placement with an omental flap for ruptured infective common iliac aneurysm in a patient with a continuous flow left ventricular assist device: alternative surgical approach avoiding driveline injury and pathogen identification by 16S ribosomal DNA. J Artif Organs. 2016;19:383–386. doi: 10.1007/s10047-016-0916-7. [DOI] [PubMed] [Google Scholar]
- 19.Niimi K, Ichihara T, Sasaki M. A case of mycotic deep femoral artery aneurysm due to Helicobacter cinaedi bacteremia. J Jpn Coll Angiol. 2014;54:51–55. doi: 10.7133/jca.14-00001. [DOI] [Google Scholar]
- 20.Seto T, Takano T, Ichimura H. Pericoronary pseudotumor caused by Helicobacter cinaedi. Int Heart J. 2014;55:463–465. doi: 10.1536/ihj.14-018. [DOI] [PubMed] [Google Scholar]
- 21.Inagaki M, Tokui T, Maze Y. Six cases of infected abdominal aortic aneurysm. Jpn J Cardiovasc Surg. 2017;46:17–20. doi: 10.4326/jjcvs.46.17. [DOI] [Google Scholar]
- 22.Kushimoto K, Yonekura R, Umesue M. Infected thoracic aortic aneurysm caused by Helicobacter cinaedi. Ann Vasc Dis. 2017;10(2):139–142. doi: 10.3400/avd.cr.16-00126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kanno Y, Shimizu R, Takei Y. Helicobacter cinaedi from infected aortic aneurysm, 2 cases reports. Jpn J Vasc Surg. 2018;27:273–276. [Google Scholar]
- 24.Bennett JE, Dolin R, Blaser MJ. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 8. Elsevier Saunders: Philadelpha; 2014. [Google Scholar]
- 25.Araoka H, Baba M, Okada C, Kimura M, Sato T, Yatomi Y, et al. First evidence of bacterial translocation from the intestinal tract as a route of Helicobacter cinaedi bacteremia. Helicobacter. 2018;23:e12458. doi: 10.1111/hel.12458. [DOI] [PubMed] [Google Scholar]
- 26.Khan S, Okamoto T, Enomoto K, Sakashita N, Oyama K, Fujii S, et al. Potential association of Helicobacter cinaedi with atrial arrhythmias and atherosclerosis. Microbiol Immunol. 2012;56:145–154. doi: 10.1111/j.1348-0421.2012.00421.x. [DOI] [PubMed] [Google Scholar]
- 27.Khan S, Rahman HNA, Okamoto T, Matsunaga T, Fujiwara Y, Sawa T, et al. Promotion of atherosclerosis by Helicobacter cinaedi infection that involves macrophage-driven proinflammatory responses. Sci Rep. 2015;4:4680. doi: 10.1038/srep04680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kiehlbauch JA, Brenner DJ, Cameron DN, Steigerwalt AG, Makowski JM, Baker CN, et al. Genotypic and phenotypic characterization of Helicobacter cinaedi and Helicobacter fennelliae strains isolated from humans and animals. J Clin Microbiol. 1995;33:2940–2947. doi: 10.1128/JCM.33.11.2940-2947.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tee W, Street AC, Spelman D, Munckhof W, Mijch A. Helicobacter cinaedi bacteraemia: varied clinical manifestations in three homosexual males. Scand J Infect Dis. 1996;28:199–203. doi: 10.3109/00365549609049078. [DOI] [PubMed] [Google Scholar]
- 30.Rimbara E, Mori S, Matsui M, Suzuki S, Wachino JI, Kawamura Y, et al. Molecular epidemiologic analysis and antimicrobial resistance of Helicobacter cinaedi isolated from seven hospitals in Japan. J Clin Microbiol. 2012;50:2553–2560. doi: 10.1128/JCM.06810-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuijper EJ, Stevens S, Imamura T, De Wever B, Claas ECJ. Genotypic identification of erythromycin-resistant Campylobacter isolates as Helicobacter species and analysis of resistance mechanism. J Clin Microbiol. 2003;41:3732–3736. doi: 10.1128/JCM.41.8.3732-3736.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matsumoto T, Goto M, Murakami H, Tanaka T, Nishiyama H, Ono E, et al. Multicenter study to evaluate bloodstream infection by Helicobacter cinaedi in Japan. J Clin Microbiol. 2007;45:2853–2857. doi: 10.1128/JCM.00465-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sörelius K, Wanhainen A, Furebring M, Björck M, Gillgren P, Mani K, et al. Nationwide study of the treatment of mycotic abdominal aortic aneurysms comparing open and endovascular repair. Circulation. 2016;134:1822–1832. doi: 10.1161/CIRCULATIONAHA.116.024021. [DOI] [PubMed] [Google Scholar]
- 34.Luo C-M, Chan C-Y, Chen Y-S, Wang S-S, Chi N-H, Wu I-H. Long-term outcome of endovascular treatment for mycotic aortic aneurysm. Eur J Vasc Endovasc Surg. 2017;54:464–471. doi: 10.1016/j.ejvs.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 35.Araoka H, Baba M, Kimura M, Abe M, Inagawa H, Yoneyama A. Clinical characteristics of bacteremia caused by Helicobacter cinaedi and time required for blood cultures to become positive. J Clin Microbiol. 2014;52:1519–1522. doi: 10.1128/JCM.00265-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miyake N, Chong Y, Nishida R, Nagasaki Y, Kibe Y, Kiyosuke M, et al. A dramatic increase in the positive blood culture rates of Helicobacter cinaedi: the evidence of differential detection abilities between the Bactec and BacT/Alert systems. Diagn Microbiol Infect Dis. 2015;83:232–233. doi: 10.1016/j.diagmicrobio.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 37.Doern CD, Mirrett S, Halstead D, Abid J, Okada P, Reller LB. Controlled clinical comparison of new pediatric medium with adsorbent polymeric beads (PF plus) versus charcoal-containing PF medium in the BacT/Alert blood culture system. J Clin Microbiol. 2014;52:1898–1900. doi: 10.1128/JCM.00175-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kirn TJ, Mirrett S, Reller LB, Weinstein MP. Controlled clinical comparison of BacT/Alert FA plus and FN plus blood culture media with BacT/Alert FA and FN blood culture media. J Clin Microbiol. 2014;52:839–843. doi: 10.1128/JCM.03063-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.