Abstract
Reports to date have shown that the SARS-CoV-2 pandemic may have a negative impact on individuals' mental health. The purpose of this study was to assess the relation between ego-resiliency, social support, coronavirus anxiety and trauma effects. The study employed the Polish adaptation of the Coronavirus Anxiety Scale (CAS). It involved 515 individuals aged 18–78. The Polish version of CAS revealed satisfactory internal consistency (α = 0.86). Structural equation modeling indicated that ego-resiliency (the Ego-Resiliency Scale) and social support (the Multidimensional Scale of Perceived Social Support) were correlated and negatively predicted the severity of the novel coronavirus anxiety (CAS). Moreover, the level of anxiety showed positive correlation with negative trauma effects (the short form of the Changes in Outlook Questionnaire). The scores indicate the need for practitioners to focus on interventions which elevate ego-resiliency and perceived social support to improve mental health during the SARS-CoV-2 pandemic.
Keywords: Ego-resiliency, Social support, Coronavirus anxiety, Coronavirus Anxiety Scale, SARS-CoV-2 pandemic, Trauma effects
1. Introduction
A novel type of human coronavirus, SARS-CoV-2 (i.e. 2019-nCov), was detected at the end of 2019 in the city of Wuhan in the Chinese province of Hubei; its genome proved to be 80% similar to the already known SARS virus (Gorbalenya et al., 2020). SARS-CoV-2 is presumed to have originated from bats from which it was transferred onto snakes or pangolins. Eventually, spillover onto humans occurred from (supposedly) market-sold animals (Ji et al., 2020; Lam et al., 2020). According to the World Health Organization (WHO), the reproduction number of the virus is estimated to be at 1–3 (Rabi et al., 2020). SARS-CoV-2 leads to the COVID-19 (Coronavirus Disease 2019) respiratory syndrome (Guan et al., 2020). Approximately 81% of patients are estimated to undergo COVID-19 asymptomatically or to exhibit slight symptoms, such as fever, breathing difficulties, dry cough and muscle pains. In some patients (14%), the disease may be pronounced more acutely, with symptoms such as atypical pneumonia and respiratory problems, or may even assume a critical form (5%). In critical cases, symptoms may include acute respiratory distress syndrome, pulmonary embolism, multiple organ dysfunction syndrome or cytokine storm syndrome (Chen et al., 2020; Huang et al., 2020; Hui et al., 2020; Mehta et al., 2020; Rotzinger et al., 2020). The SARS-CoV-2 virus quickly spread across the globe, with the outbreak escalating rapidly in North America and Europe in March 2020. On March 11, 2020, WHO declared the new coronavirus as a pandemic, which caused many governments to take unprecedented measures, such as imposing limits on businesses (industry and services), closing borders or introducing social isolation. In addition, stores suffered from a shortage of protective masks and disinfectants, while medical professionals on the virus front line worked over 16 h a day, exhibiting signs of fatigue. COVID-19 has been coined the global plague of the 21st century and the pandemic has led to the development of anxiety in people around the world (Bergman et al., 2020; Lai, Ma, et al., 2020; Lee et al., 2020; Lima et al., 2020; Taylor et al., 2020; Wang et al., 2020).
In the past, many studies focused on the consequences of an infectious disease spread on mental health (Taylor, 2019). In the case of the SARS pandemic, the negative effects concerned primarily the experience of post-traumatic stress disorder (PTSD) symptoms and depressive disorders among health professionals and convalescents (Lee et al., 2007; Lu et al., 2006; McAlonan et al., 2007). During the new coronavirus pandemic, most of the scientists' attention turned towards methods of identifying people with SARS-CoV-2, while somewhat neglecting the assessment of mental health needs of people affected by the pandemic (Xiang et al., 2020). One of the key studies on mental functioning during the new coronavirus pandemic is a report by Chinese scientists which showed elevated symptoms of PTSD, anxiety and insomnia among healthcare professionals and their patients (Lai, Ma, et al., 2020). These observations were also confirmed in several subsequent studies – also in general population (Bo et al., 2020; Kim & Su, 2020; Lai, Shih, et al., 2020; Salari et al., 2020; Thakur & Jain, 2020; Xiong et al., 2020; Zhai & Du, 2020). Therefore, it appears necessary to undertake further research (in other populations) in order to grasp the psychological challenges linked to COVID-19 (Asmundson & Taylor, 2020). It should be noted that previous reports concerning the spread of infectious diseases displayed clear links between experienced pandemic (or epidemic) anxiety and reduced mood, elevated stress, suicidal ideation and PTSD symptoms (Chong et al., 2004; Wheaton et al., 2012; Yip et al., 2010). Therefore, it seems that the assessment of SARS-CoV-2 anxiety may serve as an effective indicator of mental function during the novel coronavirus pandemic.
The experience of anxiety and other mental effects caused by the SARS-CoV-2 pandemic requires the development of intervention methods which can improve the functioning of individuals in the face of a health crisis. Reports thus far have indicated that mental resources such as ego-resiliency and perceived social support can significantly reduce the level of anxiety and mental discomfort (Budge et al., 2013; Crockett et al., 2007; Galatzer-Levy & Bonanno, 2013). Ego-resiliency is considered to be a set of basic personality traits which determines the flexible adaptation of the level of self-control to situational requirements (Block & Kremen, 1996; Letzring et al., 2005). According to researchers, high levels of ego-resiliency are associated with higher emotional adaptability, self-esteem, positive affect and a sense of well-being (Pressman & Cohen, 2005; Tugade & Fredrickson, 2004). Moreover, in the latest studies, negative correlations were observed between individual resilience vs stress intensity and worry during the new coronavirus pandemic (Grossman et al., 2021; Kimhi et al., 2020). The different resiliency and resilience recording stems from the differences in theoretical constructs (see Yang & Danes, 2015). Social support refers to the so-called social network and characterizes the functioning of individuals among other people – it concerns having a spouse, children, friends or neighbors (Buszman & Przybyła-Basista, 2017; Zimet et al., 1988). Numerous reports indicate that social support is strongly linked to positive emotions, plays an important role in maintaining health and supports healing processes (de la Vega et al., 2019; Makabe & Nomizu, 2007; Non et al., 2020). Moreover, researchers observe mutual relations between ego-resiliency and social support (Taylor et al., 2014; Trask-Tate et al., 2010). The impact of the aforementioned resources on the level of anxiety over the novel coronavirus has not yet been studied.
The exposure to stress may also lead to salutogenic outcomes, known as posttraumatic growth (PTG). The construct describes positive trauma effects emerging as a result of attempts made to cope with the stressor – they pertain to changes in the perception of self, in the nature and experience of relationships with others and in one's general philosophy of life (Calhoun & Tedeschi, 2006). Latest studies point to the onset of PTG in individuals experiencing trauma related to COVID-19, as well as to negative relations between PTG and anxiety intensity during the pandemic (Hamam et al., 2021; Tomaszek & Muchacka-Cymerman, 2020).
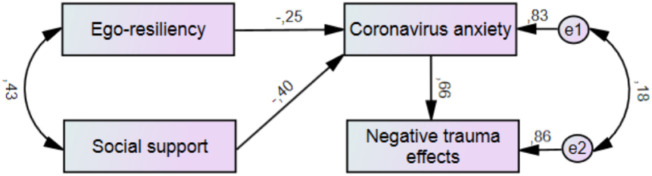
The purpose of this study was to assess the relation between social support, ego-resiliency, coronavirus anxiety and trauma effects. A hypothetical model of the study is presented in Fig. 2. Based on the scientific articles cited so far, we hypothesize that ego-resiliency and social support are correlated and may negatively predict the level of coronavirus anxiety. In addition, we assume that the SARS-CoV-2 anxiety can be positively related to negative trauma effects (PTSD symptoms). For the purpose of this study, a Polish adaptation of the Coronavirus Anxiety Scale (CAS) (Lee, 2020) was used. Positive trauma affects have not been included in the hypothetical model. Measurement of this variable was conducted mainly for the purpose of assessing the discriminant validity of the Polish CAS version. As per theoretical assumptions, PTG develops over time (Calhoun & Tedeschi, 2006). Our study has been conducted within a short time from the onset of the first pandemic wave in Poland.
Fig. 2.
Path model depicting links between ego-resiliency, social support, SARS-CoV-2 anxiety and negative trauma effects (N = 515).
2. Materials and methods
The study was conducted from April 30 to May 7, 2020 via the Internet. The data was collected on the Google Forms platform. The invitation to participate in the study was made available on Facebook and in Google. The study received approval from the Ethics Committee of the Institute of Psychology, Polish Academy of Sciences.
2.1. Participants and procedure
The study involved 515 inhabitants of Poland aged 18–78 (M = 34.64, SD = 11.85), including 298 females (58%). Five percent of participants were subjected to mandatory quarantine due to exposure to SARS-CoV-2, while 7% of the participants had a nasopharyngeal swab taken to diagnose the novel coronavirus infection – all results proved to be negative and, moreover, none of the individuals' relatives contracted the virus either. Participation was anonymous and voluntary. Individuals consented to participate in the study and were informed of the objectives and procedure. The study was targeted only at adults. The study procedure involved filling in questionnaires concerning the novel coronavirus anxiety, trauma effects, ego-resiliency and perceived social support. In addition, participants completed a questionnaire in order to collect basic socio-demographic data. Detailed characteristics of the group in terms of: education, residency and marital status are presented in Table 1 .
Table 1.
Characteristics of the study group (N = 515).
| M (SD) | ||
|---|---|---|
| Age | 34.64 (11.85) | |
| N | % | |
| Sex | ||
| Women | 298 | 58 |
| Men | 217 | 42 |
| Education | ||
| Primary | 3 | 1 |
| Middle school | 5 | 1 |
| Vocational | 13 | 3 |
| Secondary | 342 | 65 |
| Higher | 152 | 30 |
| Residency | ||
| Village | 87 | 17 |
| City up to 100,000 inhabitants | 105 | 20 |
| City from 100,000 to 250,000 inhabitants | 102 | 20 |
| City over 250,000 inhabitants | 221 | 43 |
| Marital status | ||
| Single | 170 | 33 |
| Married | 197 | 38 |
| Informal relationship | 111 | 22 |
| Divorced | 29 | 5 |
| Widow(er) | 8 | 2 |
Key: M = mean, SD = standard deviation, N = number of observations.
2.2. Measures
For the purpose of this study, the Polish adaptation of CAS (Lee, 2020) was used to assess the severity of clinical symptoms of the novel coronavirus anxiety in the form of 5 self-descriptive statements. The participants express their attitude towards each of the statements on a 5-point Likert scale (0 = “Not at all” to 4 = “Almost everyday”). This measure is computed based on the sum of ratings. The adaptation was conducted with the consent of the author of the original scale. The CAS translation was carried out by two independent translators, followed by a comparison and analysis by a medical terminology specialist. All the adaptation procedures were conducted based on WHO guidelines for cross-cultural research (Juczyński, 2009).
In addition, the study employed:
-
-
the short form of the Changes in Outlook Questionnaire (SF-CiOQ) (Joseph et al., 2006) in its Polish standardization (Skalski, 2019) to assess PTG and the intensity of PTSD symptoms. The questionnaire consists of 10 statements arranged in 2 subscales: positive effects (α = 0.85) and negative effects (α = 0.83). The participants rate each of them on a 6-point Likert scale (1 = “I strongly disagree” to 6 = “I strongly agree”). The score is computed based on the sum of ratings.
-
-
the Ego-Resiliency Scale (ER89) (Block & Kremen, 1996) in its Polish adaptation (Kaczmarek, 2011) to measure ego-resiliency as a set of personality traits. The scale consists of 14 self-descriptive statements (α = 0.78). The participants respond to each of them on a 4-point Likert scale (1 = “I strongly disagree” to 4 = “I strongly agree”). This measure is computed based on the sum of ratings.
-
-
the Multidimensional Scale of Perceived Social Support (Zimet et al., 1988) in its Polish adaptation (Buszman & Przybyła-Basista, 2017) to measure perceived social support networks. The scale consists of 12 self-descriptive statements (α = 0.89). Individuals rate the statements on a 7-point Likert scale (1 = “I strongly disagree” to 7 = “I strongly agree”). The score is computed based on the sum of ratings.
-
-
a survey developed by the authors to collect socio-demographic data (age, sex, marital status, place of residence, exposure to SARS-CoV-2).
2.3. Statistical data analysis
Statistical data analysis was conducted in IBM SPSS Statistics 26 and IBM SPSS Statistics Amos 26. The collected data had a normalized distribution, so it was possible to apply parametric tests (verified using the Kolmogorov-Smirnov test). Confirmatory factor analysis (CFA) was used to assess the factor structure. Pearson's r correlation analysis and structural equation modeling (SEM) were used to determine the relations between the variables. Goodness of fit indexes were used in the CFA and SEM: goodness of fit index (GFI), adjusted GFI (AGFI), Tucker-Lewis index (TLI), confirmatory fit index (CFI) – required value: ratio > 0.90; root mean square error of approximation (RMSEA) – required value: ratio < 0.08; as well as chi-square (X 2)/degrees of freedom (df) – required value: ratio < 2 and statistically insignificant value of test X 2 (MacCallum & Hong, 1997). The significance level was set at p < .05.
3. Results
3.1. Polish adaptation of CAS
The mean values obtained in individual CAS statements, together with standard deviation, as well as the discriminating power of individual items are shown in Table 2 . The strongest symptom of the novel coronavirus anxiety involved paralyzing worry (froze), with reduced appetite (eat) being the least pronounced one.
Table 2.
Mean values obtained from individual CAS statements (N = 515).
| M | SD | % | r | |
|---|---|---|---|---|
| Item 1 (Dizzy) | 0.56 | 1.04 | 16 | 0.71⁎⁎⁎ |
| Item 2 (Sleep) | 0.92 | 1.22 | 28 | 0.83⁎⁎⁎ |
| Item 3 (Froze) | 1.13 | 1.26 | 33 | 0.84⁎⁎⁎ |
| Item 4 (Eat) | 0.51 | 0.98 | 14 | 0.81⁎⁎⁎ |
| Item 5 (Stomach) | 0.57 | 1.03 | 17 | 0.81⁎⁎⁎ |
Key: M = mean, SD = standard deviation, % = percentage of individuals who gave a rating of “at least a few days within the last 2 weeks” or higher (2,3,4 points), r = discriminating power (correlation coefficient with overall CAS score).
p < .001 (level of significance).
The content validity of the Polish CAS adaptation was assessed by competent raters (4 psychologists) as per Lawshe's (1975) method. The content validity ratio (CVR) for each statement exceeded the required value of CVR > 0.75.
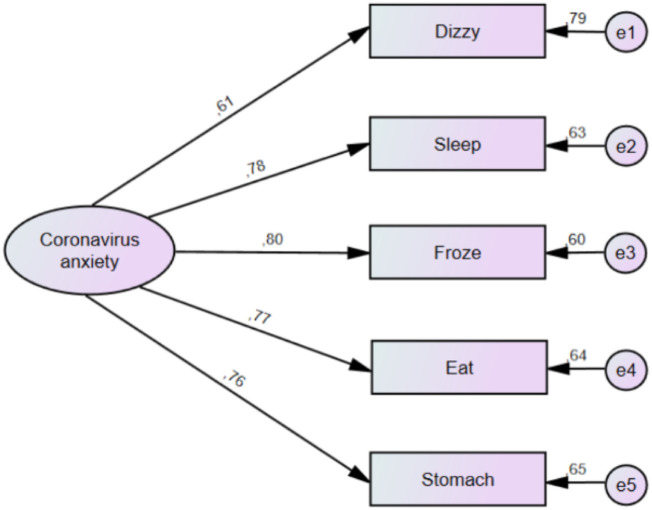
Theoretical validity was assessed using CFA with the maximum likelihood method. The single-factor model returned satisfactory values for the goodness of fit indices: X 2(5) = 1.70, p = .192; X 2 /df ratio = 0.340; GFI = 0.999; AGFI = 0.980; RMSEA = 0.037 (0.000, 0.130; 90% CI); TLI = 0.994; CFI = 0.999. The single-factor CAS structure is depicted in Fig. 1 . Internal reliability was assessed based on Cronbach's alpha which equaled α = 0.86.
Fig. 1.
Single-factor structure of the Polish CAS version (N = 515).
The convergent and discriminant validity was estimated by assessing the values of correlation coefficients with SF-CiOQ results. The overall CAS score correlated positively with the negative trauma effects subscale (r = 0.53, p < .001), as well as negatively with the positive trauma effects subscale (r = −0.18; p < .001).
Next, the influence of socio-demographic variables on the CAS score was assessed. In this study, age, sex or education did not demonstrate a statistically significant correlation with the level of the novel coronavirus anxiety. The analysis also included: staying in quarantine due to SARS-CoV-2 exposure, collecting swabs in order to diagnose the SARS-CoV-2 infection, as well as the date of CAS measurement – these data had a statistically significant relation with the severity of the coronavirus anxiety. The values of correlation coefficients are presented in Table 4.
Table 4.
Descriptive statistics and correlations (N = 515).
| r |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M(SD) | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | |
| 1. | 3.69 (4.44) | 1 | – | – | – | – | 0.06 | −0.02 | −0.05 | −0.02 | 0.06 | 0.09⁎ | 0.10⁎ | −0.29⁎⁎⁎ |
| 2. | 35.23 (7.02) | −0.43⁎⁎⁎ | 1 | – | – | – | 0.08 | −0.06 | −0.04 | −0.01 | 0.05 | −0.05 | −0.08 | 0.04 |
| 3. | 63.24(17.47) | −0.50⁎⁎⁎ | 0.43⁎⁎⁎ | 1 | – | – | −0.05 | −0.07 | −0.03 | 0.02 | 0.06 | −0.06 | −0.02 | 0.07 |
| 4. | 15.46 (5.39) | −0.18⁎⁎⁎ | −0.12⁎⁎ | −0.15⁎⁎ | 1 | – | −0.08 | 0.08 | −0.09 | 0.02 | −0.01 | −0.03 | 0.04 | 0.08 |
| 5. | 12.95 (5.91) | 0.53⁎⁎⁎ | −0.26⁎⁎⁎ | −0.35⁎⁎⁎ | −0.13⁎⁎ | 1 | −0.07 | −0.04 | 0.05 | 0.01 | −0.07 | 0.04 | 0.03 | −0.07 |
Key: r = correlation coefficient, M = mean, SD = standard deviation, 1. = Coronavirus anxiety, 2. = Ego-resiliency, 3. = Social support, 4. = Positive trauma effects, 5. = Negative trauma effects, 6. = Age, 7. = Sex (0 = female, 1 = male), 8. = Education (0 = below higher, 1 = higher), 9. = Place of residence (0 = village or city up to 100 ths inhabitants, 1 = city over 100 ths inhabitants), 10. = Marital status (0 = single, divorced, window(er), 1 = married or in informal relationship), 11. = Quarantine (0 = no mandatory quarantine, 1 = quarantine), 12. Swab (0 = no nasopharyngeal swab for diagnosing SARS-CoV-2 infection, 1 = swab), 13. Date of CAS measurement.
p < .05.
p < .01.
p < .001 (significance level).
3.2. Standardization
It seems that assessing the novel coronavirus anxiety might benefit from the determination of the intensity of the measured phenomenon. Based on the data obtained from the study group (Table 1), the raw scores were transformed into sten scores, arriving at a population average of 5.50 (SD = 2). Temporary sten scores are presented in Table 3 .
Table 3.
Temporary sten scores for CAS (N = 515).
| RS | Sten |
|---|---|
| – | 1 |
| 0 | 2 |
| 1 | 3 |
| 2 | 4 |
| 3–4 | 5 |
| 5 | 6 |
| 6–7 | 7 |
| 8–11 | 8 |
| 12–15 | 9 |
| 16–20 | 10 |
Key: RS = raw score.
3.3. Mental resources versus anxiety
The mean values obtained in the study together with the standard deviation regarding the controlled variables of coronavirus anxiety, ego-resiliency, social support, as well as positive and negative trauma effects and correlation coefficient values are depicted in Table 4 .
The following statistically significant links have been observed: ego-resiliency versus the novel coronavirus anxiety; social support versus anxiety and ego-resiliency; positive trauma effects versus anxiety, ego-resiliency and social support; as well as negative trauma effects versus anxiety, ego-resiliency, social support and positive trauma effects.
Next, SEM was applied using the maximum likelihood method to verify the assumed hypotheses (Fig. 2 ). The model takes into account the possibility of correlation of residual values between coronavirus anxiety and negative trauma effects, as both constructs refer to negative consequences for the individual's psyche due to the SARS-CoV-2 outbreak. A hypothetical model was approved, obtaining satisfactory values for the goodness of fit indices: X 2(1) = 1.06, p = .303, X 2 /df ratio = 1.06; GFI =. 999; AGFI = 0.990; RMSEA = 0.011 (0.000, 0.118; 90% CI); TLI = 0.999; CFI = 1.00.
As per the obtained model, ego-resiliency and social support were statistically significantly correlated. Ego-resiliency and social support were statistically significant predictors of the level of the novel coronavirus anxiety (R 2 = 0.31). The level of anxiety was a statistically significant predictor of the severity of negative trauma effects (R 2 = 0.27 for the entire model). Regression weight indices are presented in Table 5 . Moreover, the following total effects not included in the model were observed: ego-resiliency (β = −0.17) and social support (β = −0.26) were statistically significant predictors of negative trauma effects (p < .001).
Table 5.
Regression weights in the obtained model (N = 515).
| B | SE | β | CR | p | |
|---|---|---|---|---|---|
| Ego-resiliency → Anxiety | −0.16 | 0.03 | −0.25 | −6.30 | <.001 |
| Social support → Anxiety | −0.10 | 0.01 | −0.40 | −9.89 | <.001 |
| Anxiety → Negative trauma effects | 0.88 | 0.09 | 0.66 | 9.75 | <.001 |
Key: B = non-standardized factor, SE = standard error B, β = standardized factor, CR = critical ratio, p = significance level.
4. Discussion
The objective of this study was to assess the link between ego-resiliency, perceived social support, coronavirus anxiety and trauma effects. For the purposes of this article, a Polish CAS adaptation has been introduced.
Throughout validation studies, the Polish CAS version displayed satisfactory psychometric properties. The scale meets the basic requirements for validity and reliability. CAS may be used as a screener of mental function during the coronavirus pandemic in clinical practice and in scientific research. The absolute stability of the scale has not been assessed in this study. We believe that anxiety over the novel coronavirus can change over time or under the influence of interventions.
In this study, nearly every third participant experienced paralyzing worry and reduced appetite in connection with the SARS-CoV-2 pandemic for at least several days during the two weeks prior to participation. The remaining symptoms of coronavirus anxiety proved to be less intense. Moreover, the level of anxiety exhibited a positive relation with the diagnostics for SARS-CoV-2 infection – nasopharyngeal swab (small effect) and a negative link to the date of CAS measurement – the anxiety decreased with time since the outbreak (also small effect). It should be noted that the epidemiological restrictions in Poland have been loosened during the course of the conducted research – hotels, shopping mall stores and libraries were reopened, which could have improved the social mood.
In our study, ego-resiliency and social support were correlated and allowed for predicting the level of anxiety over SARS-CoV-2, as well as the negative trauma effects (PTSD symptoms), which is in line with previous reports (Budge et al., 2013; Chong et al., 2004; Crockett et al., 2007; Galatzer-Levy & Bonanno, 2013; Lee, 2020). It should be stressed that the environmental variable (social support) has proved to be a stronger predictor of anxiety and negative trauma effects than the personality variable (ego-resiliency). This seems understandable, as perceived social support shapes the level of self-esteem, while positive self-esteem can relieve stress and anxiety (Waqas et al., 2016). However, the co-occurrence of both mental resources (environmental and personality variables) is essential for optimal adaptation to the traumatic event and for maintaining mental health (Kim & Yang, 2017). Moreover, as per the assumed hypothetical model, coronavirus anxiety mediated the relation between selected mental resources and negative trauma effects. This observation corresponds to previous reports that anxiety over the spreading infectious disease may be a marker of mental functioning during the pandemic (Chong et al., 2004; Lee, 2020; Wheaton et al., 2012; Yip et al., 2010). All the obtained effects were generally medium or moderate, yet important in our opinion. The scores emphasize the role of ego-resiliency and perceived social support in non-pharmacological alleviation of SARS-CoV-2 anxiety, as well as of negative trauma effects.
The obtained mean values with respect to ego-resiliency, social support and negative trauma effects correspond with the standardization reports for SF-CiOQ, ER89 and MSPSS in the Polish population (Buszman & Przybyła-Basista, 2017; Kaczmarek, 2011; Skalski, 2019). It seems that new technologies have made it considerably easier to maintain social networks despite the mandatory isolation. Our findings underline the need to properly balance between medical gain and psychological effects on mental health during the new coronavirus pandemic. Research so far has shown that single people are more prone to exhibit unease over social isolation and fear of financial problems in connection with COVID-19 (Okruszek et al., 2020). Moreover, the mean value obtained in our study with regard to positive trauma effects (PTG) proved to be lower than in the standardization sample of the Polish version of SF-CiOQ – i.e. 4 sten according to the standards proposed by the author (Skalski, 2019). It is worth noting that PTG is a phenomenon remote in its nature, i.e. it develops over time under the influence of remedial strategies undertaken by an individual (Calhoun & Tedeschi, 2006).
Finally, it should be underlined that the positive trauma effects (PTG) were negatively correlated with ego-resiliency and social support (small effects). It seems that these relations did not stem from direct dependencies, but were moderated by other (not considered) factors, such as restrictions concerning social interactions and limitations on cognitive processing. It is believed that minimizing the importance of a traumatic event by others can lead to withdrawal and avoidance of conversations about stress or trauma which, in turn, limits the ability to achieve PTG (Lepore & Revenson, 2007).
This study is affected by certain limitations. It was of a cross-sectional nature, therefore it is difficult to pass clear judgment on the causes and effects. None of the participants were infected with SARS-CoV-2 nor were they convalescents – scores in such groups may differ from those of the general population. Moreover, the psychiatric history of the participants was not controlled in the study. Social support was limited only to the perceived support network (e.g. material support was not assessed). Despite these limitations, the study brings new data on the relationship between selected mental resources and the severity of anxiety and trauma effects during a new coronavirus pandemic. In future studies, it would seem interesting to apply experimental techniques – e.g. manipulation of the level of perceived social support, as well as identification of resources conducive to the development of PTG during the SARS-CoV-2 pandemic – including longitudinal studies (PTG may develop over time).
5. Conclusions
This study is one of the first to assess the links between selected mental resources and psychological functioning during the new coronavirus pandemic. For the purposes of this study, a Polish CAS adaptation has been introduced. We were probably the first to demonstrate that ego-resiliency and perceived social support can negatively predict SARS-CoV-2 anxiety and PTSD symptoms (negative trauma effects). In addition, we have confirmed the previous findings that coronavirus anxiety can predict the severity of negative trauma effects. The data obtained have an application value. They can be used in clinical practice and in developing prevention programs.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by The Committee for Ethics in Scientific Research of The Institute of Psychology, Polish Academy of Sciences.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
All authors contributed equally to the manuscript – they planned the study, collected data, conducted statistical analysis and interpretation of data: SS(25%), PU(25%), PD(25%), AK(25%). The first version of the manuscript was prepared by the SS, and then revised and accepted by all authors.
CRediT authorship contribution statement
Sebastian Skalski: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing - original draft. Patrycja Uram: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing - original draft. Paweł Dobrakowski: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing - review & editing. Anna Kwiatkowska: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing - review & editing.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Appendix 1. CAS statements in Polish
Jak często w trakcie ostatnich 2 tygodni doświadczyłeś/aś poniższych zdarzeń?
-
1.
Kręciło mi się w głowie, gdy czytałem/am lub słuchałem/am informacji o koronawirusie.
-
2.
Miałem/am problemy ze snem, ponieważ myślałem/am o koronawirusie.
-
3.
Czułem/am paraliżujący niepokój, gdy myślałem/am lub otrzymywałem/am informacje na temat koronawirusa.
-
4.
Straciłem/am apetyt przez myślenie o koronawirusie lub otrzymywanie informacji na jego temat.
-
5.
Miałem/am mdłości lub inne problemy żołądkowe, gdy myślałem/am lub otrzymywałem/am informacje na temat koronawirusa.
References
- Asmundson G.J.G., Taylor S. Coronaphobia: Fear and the 2019-nCoV outbreak. Journal of Anxiety Disorders. 2020;70 doi: 10.1016/j.janxdis.2020.102196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman Y.S., Cohen-Fridel S., Shrira A., Bodner E., Palgi Y. COVID-19 health worries and anxiety symptoms among older adults: The moderating role of ageism. International Psychogeriatrics. 2020:1–5. doi: 10.1017/S1041610220001258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block J., Kremen A.M. IQ and Ego-resiliency: Conceptual and empirical connections and separateness. Journal of Personality and Social Psychology. 1996;70(2):349–361. doi: 10.1037/0022-3514.70.2.349. [DOI] [PubMed] [Google Scholar]
- Bo H.X., Li W., Yang Y., Wang Y., Zhang Q., Cheung T.…Xiang Y.T. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychological Medicine. 2020 doi: 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budge S.L., Adelson J.L., Howard K.A.S. Anxiety and depression in transgender individuals: The roles of transition status, loss, social support, and coping. Journal of Consulting and Clinical Psychology. 2013;81(3):545–557. doi: 10.1037/a0031774. [DOI] [PubMed] [Google Scholar]
- Buszman K., Przybyła-Basista H. Polska adaptacja the multidimensional scale of perceived social support [Polish adaptation of the multidimensional scale of perceived social support] Polskie Forum Psychologiczne. 2017;22(4):581–599. doi: 10.14656/PFP20170404. [DOI] [Google Scholar]
- Calhoun L., Tedeschi R. In: Handbook of posttraumatic growth: Research & practice. Calhoun L., Tedeschi R., editors. Mahwah; NJ: 2006. The foundations of posttraumatic growth: An expanded framework; pp. 3–23. [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y.…Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. The Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong M.Y., Wang W.C., Hsieh W.C., Lee C.Y., Chiu N.M., Yeh W.C.…Chen C.L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. British Journal of Psychiatry. 2004;185(AUG):127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- Crockett L.J., Iturbide M.I., Torres Stone R.A., McGinley M., Raffaelli M., Carlo G. Acculturative stress, social support, and coping: Relations to psychological adjustment among Mexican American college students. Cultural Diversity and Ethnic Minority Psychology. 2007;13(4):347–355. doi: 10.1037/1099-9809.13.4.347. [DOI] [PubMed] [Google Scholar]
- de la Vega R., Molton I.R., Miró J., Smith A.E., Jensen M.P. Changes in perceived social support predict changes in depressive symptoms in adults with physical disability. Disability and Health Journal. 2019;12(2):214–219. doi: 10.1016/j.dhjo.2018.09.005. [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy I.R., Bonanno G.A. Heterogeneous patterns of stress over the four years of college: Associations with anxious attachment and ego-resiliency. Journal of Personality. 2013;81(5):476–486. doi: 10.1111/jopy.12010. [DOI] [PubMed] [Google Scholar]
- Gorbalenya A.E., Baker S.C., Baric R.S., de Groot R.J., Drosten C., Gulyaeva A.A.…Ziebuhr J. The species severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nature Microbiology. 2020, April 1;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman E.S., Hoffman Y.S.G., Palgi Y., Shrira A. COVID-19 related loneliness and sleep problems in older adults: Worries and resilience as potential moderators. Personality and Individual Differences. 2021;168 doi: 10.1016/j.paid.2020.110371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W., Ni Z., Hu Y., Liang W., Ou C., He J.…Zhong N. Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamam A.A., Milo S., Mor I., Shaked E., Eliav A.S., Lahav Y. Peritraumatic reactions during the COVID-19 pandemic – The contribution of posttraumatic growth attributed to prior trauma. Journal of Psychiatric Research. 2021;132:23–31. doi: 10.1016/j.jpsychires.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y.…Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui D.S., Azhar E.I., Madani T.A., Ntoumi F., Kock R., Dar O.…Petersen E. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health — The latest 2019 novel coronavirus outbreak in Wuhan, China. International Journal of Infectious Diseases. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji W., Wang W., Zhao X., Zai J., Li X. Cross-species transmission of the newly identified coronavirus 2019-nCoV. Journal of Medical Virology. 2020;92(4):433–440. doi: 10.1002/jmv.25682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph S., Linley P.A., Shevlin M., Goodfellow B., Butler L. Assessing positive and negative changes in the aftermath of adversity: A short form of the changes in outlook questionnaire. Journal of Loss and Trauma. 2006;11:85–99. doi: 10.1080/15325020500358241. [DOI] [Google Scholar]
- Juczyński Z. Pracownia Testów Psychologicznych PTP; Warsaw, Poland: 2009. Narzędzia pomiaru w promocji i psychologii zdrowia [Measurement tools in health promotion and psychology] [Google Scholar]
- Kaczmarek Ł. Kwestionariusz Sprężystości Psychicznej–polska adaptacja Ego Resiliency Scale [Polish adaptation of Ego Resiliency Scale] Czasopismo Psychologiczne. 2011;17:263–265. [Google Scholar]
- Kim H., Yang M.-S. A study on the social support, ego-resiliency and stress coping strategies of school-dropout adolescents. Journal of Digital Convergence. 2017;15(1):23–34. doi: 10.14400/jdc.2017.15.1.23. [DOI] [Google Scholar]
- Kim S.W., Su K.P. Using psychoneuroimmunity against COVID-19. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhi S., Marciano H., Eshel Y., Adini B. Resilience and demographic characteristics predicting distress during the COVID-19 crisis. Social Science and Medicine. 2020;265 doi: 10.1016/j.socscimed.2020.113389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. International Journal of Antimicrobial Agents. 2020;55:105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N.…Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam T.T.Y., Shum M.H.H., Zhu H.C., Tong Y.G., Ni X.B., Liao Y.S.…Guan Y. Identifying SARS-CoV-2 related coronaviruses in Malayan pangolins. Nature. 2020:1–6. doi: 10.1038/s41586-020-2169-0. [DOI] [PubMed] [Google Scholar]
- Lawshe C. A quantitative approach to content validity. Personnel Psychology. 1975;28:563–575. [Google Scholar]
- Lee A.M., Wong J.G., McAlonan G.M., Cheung V., Cheung C., Sham P.C.…Chua S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. The Canadian Journal of Psychiatry. 2007;52(4):233–240. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- Lee S.A. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Studies. 2020;44(7):393–401. doi: 10.1080/07481187.2020.1748481. [DOI] [PubMed] [Google Scholar]
- Lee S.A., Jobe M.C., Mathis A.A., Gibbons J.A. Incremental validity of coronaphobia: Coronavirus anxiety explains depression, generalized anxiety, and death anxiety. Journal of Anxiety Disorders. 2020;74:102268. doi: 10.1016/j.janxdis.2020.102268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepore S.J., Revenson T.A. Social constraints on disclosure and adjustment to cancer. Social and Personality Psychology Compass. 2007;1(1):313–333. doi: 10.1111/j.1751-9004.2007.00013.x. [DOI] [Google Scholar]
- Letzring T.D., Block J., Funder D.C. Ego-control and ego-resiliency: Generalization of self-report scales based on personality descriptions from acquaintances, clinicians, and the self. Journal of Research in Personality. 2005;39(4):395–422. doi: 10.1016/j.jrp.2004.06.003. [DOI] [Google Scholar]
- Lima C.K.T., Carvalho P.M.d.M., Lima I.d.A.A.S., Nunes J.V.A.d.O., Saraiva J.S., de Souza R.I.…Neto M.L.R. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease) Psychiatry Research. 2020;287 doi: 10.1016/j.psychres.2020.112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Y.-C., Shu B.-C., Chang Y.-Y., Lung F.-W. The mental health of hospital workers dealing with severe acute respiratory syndrome. Psychotherapy and Psychosomatics. 2006;75(6):370–375. doi: 10.1159/000095443. [DOI] [PubMed] [Google Scholar]
- MacCallum R.C., Hong S. Power analysis in covariance structure modeling using GFI and AGFI. Multivariate Behavioral Research. 1997;32(2):193–210. doi: 10.1207/s15327906mbr3202_5. [DOI] [PubMed] [Google Scholar]
- Makabe R., Nomizu T. Social support and psychological and physical states among Japanese women with breast cancer before and after breast surgery. Oncology Nursing Forum. 2007;34(4):883–889. doi: 10.1188/07.ONF.883-889. [DOI] [PubMed] [Google Scholar]
- McAlonan G.M., Lee A.M., Cheung V., Cheung C., Tsang K.W.T., Sham P.C.…Wong J.G.W.S. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Canadian Journal of Psychiatry. 2007;52(4):241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. The Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Non A.L., Román J.C., Clausing E.S., Gilman S.E., Loucks E.B., Buka S.L.…Kubzansky L.D. Optimism and social support predict healthier adult behaviors despite socially disadvantaged childhoods. International Journal of Behavioral Medicine. 2020;27(2):200–212. doi: 10.1007/s12529-020-09849-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okruszek L., Aniszewska-Stańczuk A., Piejka A., Wiśniewska M., Żurek K. 2020. Safe but lonely? Loneliness, mental health symptoms and COVID-19. (Manuscript Submitted for Publication) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pressman S.D., Cohen S. Does positive affect influence health? Psychological Bulletin. 2005;131:925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- Rabi F.A., Al Zoubi M.S., Kasasbeh G.A., Salameh D.M., Al-Nasser A.D. SARS-CoV-2 and coronavirus disease 2019: What we know so far. Pathogens. 2020;9(3) doi: 10.3390/pathogens9030231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotzinger D.C., Beigelman-Aubry C., von Garnier C., Qanadli S.D. Pulmonary embolism in patients with COVID-19: Time to change the paradigm of computed tomography. Thrombosis Research. 2020;190:58–59. doi: 10.1016/j.thromres.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M.…Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization and Health. 2020;16 doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skalski S. New perspective questionnaire to measure positive and negative trauma effects. Polish adaptation of the short form of the changes in outlook questionnaire. Annales Universitatis Mariae Curie-Skłodowska, Sectio J – Paedagogia-Psychologia. 2019;32(3):317. doi: 10.17951/j.2019.32.3.307-317. [DOI] [Google Scholar]
- Taylor S. Newcastle upon Tyne. Cambridge Scholars Publishing; UK: 2019. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. COVID stress syndrome: Concept, structure, and correlates. Depression and Anxiety. 2020;37(8):706–714. doi: 10.1002/da.23071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor Z.E., Doane L.D., Eisenberg N. Transitioning from high school to college. Emerging Adulthood. 2014;2(2):105–115. doi: 10.1177/2167696813506885. [DOI] [Google Scholar]
- Thakur V., Jain A. COVID 2019-suicides: A global psychological pandemic. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.04.062. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Tomaszek K., Muchacka-Cymerman A. Thinking about my existence during COVID-19, I feel anxiety and awe—The mediating role of existential anxiety and life satisfaction on the relationship between PTSD symptoms and post-traumatic growth. International Journal of Environmental Research and Public Health. 2020;17(19):7062. doi: 10.3390/ijerph17197062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trask-Tate A., Cunningham M., Lang-DeGrange L. The importance of family: The impact of social support on symptoms of psychological distress in African American girls. Research in Human Development. 2010;7(3):164–182. doi: 10.1080/15427609.2010.504458. [DOI] [Google Scholar]
- Tugade M.M., Fredrickson B.L. Resilient individuals use positive emotions to bounce back from negative emotional experiences. Journal of Personality and Social Psychology. 2004;86:320–333. doi: 10.1037/0022-3514.86.2.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waqas A., Naveed S., Bhuiyan M.M., Usman J., Inam-ul-Haq A., Cheema S.S. Social support and resilience among patients with burn injury in Lahore, Pakistan. Cureus. 2016 doi: 10.7759/cureus.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton M.G., Abramowitz J.S., Berman N.C., Fabricant L.E., Olatunji B.O. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognitive Therapy and Research. 2012;36(3):210–218. doi: 10.1007/s10608-011-9353-3. [DOI] [Google Scholar]
- Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L.…McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Danes S.M. Resiliency and resilience process of trepreneurs in new venture creation. Entrepreneurship Research Journal. 2015;5(1):1–30. doi: 10.1515/erj-2013-0076. [DOI] [Google Scholar]
- Yip P.S.F., Cheung Y.T., Chau P.H., Law Y.W. The impact of epidemic outbreak. Crisis. 2010;31:86–92. doi: 10.1027/0227-5910/A000015. [DOI] [PubMed] [Google Scholar]
- Zhai Y., Du X. Loss and grief amidst COVID-19: A path to adaptation and resilience. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet G.D., Dahlem N.W., Zimet S.G., Farley G.K. The multidimensional scale of perceived social support. Journal of Personality Assessment. 1988;52(1):30–41. doi: 10.1207/s15327752jpa5201_2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.