Abstract
Objective
The lack of precise and inclusive gender, sex, and sexual orientation (GSSO) data in electronic health records (EHRs) is perpetuating inequities of sexual and gender minorities (SGM). We conducted a rapid review on how GSSO documentation in EHRs should be modernized to improve the health of SGM.
Materials and Methods
We searched MEDLINE from 2015 to 2020 with terms for gender, sex, sexual orientation, and electronic health/medical records. Only literature reviews, primary studies, and commentaries from peer-reviewed journals in English were included. Two researchers screened citations and reviewed articles with help from a third to reach consensus. Covidence, Excel, and Atlas-TI were used to track articles, extract data, and synthesize findings, respectively.
Results
Thirty-five articles were included. The 5 themes to modernize GSSO documentation in EHRs were (1) creating an inclusive, culturally competent environment with precise terminology and standardized data collection; (2) refining guidelines for identifying and matching SGM patients with their care needs; (3) improving patient-provider relationships by addressing patient rights and provider competencies; (4) recognizing techno-socio-organizational aspects when implementing GSSO in EHRs; and (5) addressing invisibility of SGM by expanding GSSO research.
Conclusions
The literature on GSSO documentation in EHRs is expanding. While this trend is encouraging, there are still knowledge gaps and practical challenges to enabling meaningful changes, such as organizational commitments to ensure affirming environments, and coordinated efforts to address technical, organizational, and social aspects of modernizing GSSO documentation. The adoption of an inclusive EHR to meet SGM needs is a journey that will evolve over time.
Keywords: sex and gender minorities, documentation practices, electronic health record, electronic medical record, health information standards, rapid review, gender, sex, and sexual orientation
INTRODUCTION
Sexual and gender minorities (SGM) are among the most marginalized and underserved populations in the health system.1 Barriers experienced by SGM include stigma, structural and financial barriers, and a lack of health care provider experience in caring for them.1Furthermore, if an individual is willing to reveal their gender, sex, and sexual orientation (GSSO) to a provider, current electronic health records (EHRs) in most health organizations are unable to store and share this information appropriately.1 The absence of precisely defined and inclusive GSSO concepts, terms, and codes has contributed to the invisibility of SGM in health data sets and EHRs that produce them and to widespread inaccuracies in their use in these systems. As a result, we have little certainty about the specific health needs and long-term health outcomes of SGM.1–3 The challenge is to improve these inadequate structures so GSSO data collected in EHRs can enable safe, inclusive, and affirmative care and eliminate inequities in health data.
There have been efforts to improve the definition, collection, and use of GSSO data in EHRs among health organizations. In 2013, the World Professional Association for Transgender Health published recommendations for EHR developers, vendors, and users with respect to transgender and gender-nonconforming (Note: These terms are evolving; for instance, gender-nonconforming has been replaced by gender-nonbinary and may include a plethora of other genders. Also, some literature assumes transgender includes gender-nonbinary people.) patients.4 In the United States, the Office of the National Coordinator requires EHR vendors to include sexual orientation (SO) and gender identity (GI) data fields as part of the certification process,5 but providers are currently not required to document this information.6 Organizations where GSSO data are collected are often specialized; they include the Fenway Institute,7 Department of Veterans Affairs,8 and PRIDE Study.9 Still, there are variations in current practices,10,11 and many health organizations have yet to implement policies and practices to collect GSSO data due to multiple barriers. They include a lack of organizational will to address an unfamiliar and confusing issue, competing organizational priorities, and the cost of updating existing EHRs with more modern GSSO definitions.12 A lack of standardized GSSO coding schemes has also made it impossible to exchange this information across EHRs13 because of conceptual and practical ambiguity. The enhancement of EHRs to enable safe, inclusive, and affirmative care of SGM is a complex multi-level challenge with numerous barriers that transects every aspect of health care.
In order to understand how to address the challenge of integrating GSSO data into EHRs, we conducted a rapid literature review on how GSSO documentation in EHRs should be modernized. For the purpose of this review, GSSO documentation refers to the principles, approaches, policies, and processes of defining, collecting, organizing, sharing, and using GSSO data.
MATERIALS AND METHODS
Review questions
Our central question for the rapid review was “How should one modernize GSSO documentation in EHRs?” Our specific questions were: (a) What are the current approaches to GSSO documentation in EHRs? (b) What are the current gaps, challenges, and needs? (c) What are the relevant efforts and lessons in modernizing GSSO documentation in EHRs?
Study selection and synthesis
Rapid reviews have gained recognition as a method that supports health care decision-making by allowing for timely review of the literature on topics that require prompt action or that are rapidly evolving.14 Our protocol was developed at the start of the review, informed by published guidance on rapid reviews.14–17 Based on the specified focus and a 4-month time frame, we selected MEDLINE as our search engine, included a hand search of our existing collection, and omitted quality appraisal and bias assessment.14,16 The search strategy was developed in consultation with a health librarian and included search terms and MeSH headings for sex, gender, sexual orientation, and electronic health/medical records (Supplementary Appendix SA).
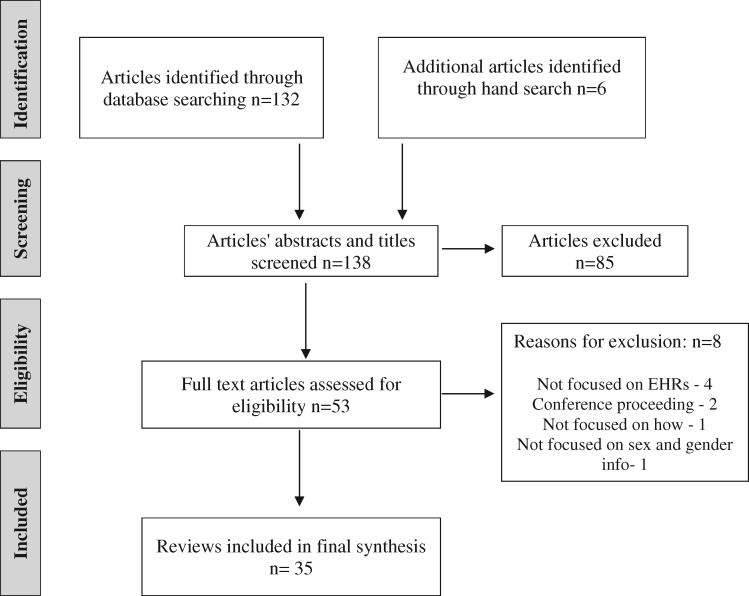
Reviews, primary studies, and commentaries from peer-reviewed journals in English were included. Conference proceedings, non-peer-reviewed articles, and grey literature, such as government and research reports, news articles, user/training manuals, educational materials, and position papers were excluded, as they are the focus of another rapid review currently underway. Citations were screened independently by 2 researchers, and, where disagreements occurred, a third researcher was used to reach consensus. The inclusion and exclusion of studies were tracked using Covidence and data were extracted into Excel. Data were grouped by 1 researcher under the 3 specific questions. Atlas-TI was used by 1 researcher to develop a coding scheme. Further codes were added/refined independently by a second researcher, and 2 others helped validate the outputs to reach consensus (Supplementary Appendix SB). Preliminary results were presented at stakeholder working group meetings18; feedback from these sessions and ongoing synthesis by the research team finalized the analysis. Figure 1 shows the flow diagram of article selection process.
Figure 1.
Flow diagram of article selection.
RESULTS
Characteristics of included articles
Our final selection included 35 peer-reviewed articles with 18 primary studies, 8 reviews, 6 commentaries, and 3 implementation briefs. See Supplementary Appendix SC for article characteristics. There was a predominant focus on the challenges, needs, and strategies to modernize GSSO documentation in EHRs to improve the health of SGM. Both commentaries19–21 and reviews22,23 emphasized the need for inclusive SGM terminology and policy and practice guidance to support clinical care, research innovation, and patient engagement. This need was further demonstrated through a survey on SGM-inclusive policies and practices in breast imaging facilities.24 Several reviews examined transgender patient identification and hormonal therapy guidelines and issues,25–28 and a descriptive study explored identification-related challenges for pathology laboratories.29
The perspectives of SGM patients and health care providers on GI data collection in EHRs30–32 and emergency and inpatient care experiences of transgender and gender-nonconforming patients33,34 were explored through interviews, focus groups, and surveys. EHR efforts for introducing GSSO were examined in a commentary on the SOGI (Note: SOGI and GSSO cover the same concepts of gender [identity], sex [assigned at birth], and sexual orientation. GSSO is used throughout this review unless it is important to mention SOGI as in the Office of National Coordinator mandate in the United States.) mandate in the United States,5 and the need for GSSO and self-identified GI data in EHRs was reinforced in several implementation briefs.7,8,35 Thirteen articles focused on different ways GSSO data can be analyzed in EHR-related SGM research. These included examining the effects of GSSO and sexual partner documentation in EHRs through a pre-post study,36 retrospective studies,10,37,38 and surveys.39,40Text-mining was applied to show how EHR data can be used to identify transgender and nonbinary patients.41–44 Patients’ SOs and their correlation with human immunodeficiency virus risk-assessment45 and intimate partner violence46 were examined in 2 surveys. The methodological gaps and challenges in transgender research and limited evidence-based prevention and care were addressed in a review.47
We synthesized 5 themes in how GSSO documentation in EHRs should be modernized. They were to: (1) create an inclusive and culturally competent environment with precise terminology and standardized data collection; (2) refine guidelines for identifying and matching SGM patients with their care needs; (3) improve patient-provider relationships by addressing patient rights and provider competencies; (4) recognize techno-socio-organizational aspects when modernizing GSSO documentation; and (5) address invisibility of SGM through standardized data and expanded research.
Inclusive environment, precise terminology, and standardized data collection
Need for precise terminology
The growing body of SGM literature has led to a plethora of evolving concepts and terms that have overlapping meanings and can be confusing for those not educated as to their significance. These terms include gender identity, gender expression, and gender role23; gender nonbinary/genderqueer, transsexual, and transgender23; transgender and gender nonconforming8; and lesbian, gay, bisexual, transgender, queer, and/or intersex (LGBTQ/LGBTQI).20 To be inclusive and to improve the health of SGM, it is important to have a precise terminology to facilitate shared understanding of these concepts and terms.20 Examples are the glossary of terms by Madsen et al20 and gender identity definitions by Rosendale et al23 that one can update and track as these concepts, terms, and definitions evolve over time. A proposed SGM terminology based on common terms in the included articles and published terminology48 by 1 of the coauthors (AD) is shown in Table 1.
Table 1.
Proposed sexual and gender minority terminology
| Term | Definition | Source |
|---|---|---|
| Sex | A person’s status as male, female, or intersex based on biologic and physiologic characteristics. Sexes are usually assigned at birth based on simple visual inspection of the genitals of a newborn baby | Goldman et al48 |
| Sex assigned at birth | Sex assigned and recorded at birth, usually based on simple visual inspection of the genitals of a newborn baby. Also known as birth sex | Goldman et al,48 revised |
| Legal Sex | Sex as defined by legal documents, such as birth certificate, passport, driver’s license, or health care card | Goldstein et al,25 revised |
| Male | Binary category of sex defined by XY chromosomal, gonadal, and anatomic characteristics | Madsen et al,20 revised |
| Female | Binary category of sex defined by XX chromosomal, gonadal, and anatomic characteristics | Madsen et al,20 revised |
| Intersex | A category of sex defined by chromosomal, gonadal, and anatomic characteristics that does not fit into the binary category of male or female | Madsen et al,20 revised |
| Gender | A person’s status as a man or boy, woman or girl, transgender person, nonbinary person, and may include Two-Spirit persons. Genders are usually assigned at birth on the assumption that people born with male genitals will be boys and that people born with female genitals will be girls | Goldman et al48 |
| Administrative gender | A term used in most existing electronic health record systems that refers to either one’s sex or gender recorded and used for administrative purposes such as billing purposes. Also known as legal gender in some EHR systems | Burgess et al,8 revised |
| Man | One of 2 binary categories of gender; typically associated with masculine behaviors and constructs | Madsen et al20 |
| Woman | One of 2 binary categories of gender; typically associated with feminine behaviors and constructs | Madsen et al20 |
| Gender minority | A broad term to describe transgender and nonbinary people whose gender identity or expression differs from what is typically expected | Ehrenfeld et al,42 revised |
| Gender identity | A person’s deeply felt intrinsic sense of their own gender | Goldman et al48 |
| Gender expression | How a person enacts gender in their everyday life. There are many reasons why a person may not feel that it is safe to express their gender identity in certain circumstances. Thus, a person’s gender expression may or may not be a good representation of their gender identity | Goldman et al48 |
| Social/lived gender | The gender in which a person lives their everyday life. A person’s social gender may or may not express their gender identity. Similarly, it may or may not match what would typically be expected on the basis of their sex or gender assigned at birth | Goldman et al48 |
| Cisgender | People whose current sex and gender identities match the ones they were assigned at birth | Goldman et al48 |
| Gender binary | The idea that there are 2, and only 2, genders, men and women, and the expectation that everyone has to be one or the other | Goldman et al48 |
| Nonbinary gender identities | Gender identities adopted by people who reject the idea of gender binary. They may identify as partially a man and partially a woman or identify as sometimes a man and sometimes a woman or identity as some gender other than a man or woman, or as not having a gender at all. They most commonly use the pronouns they/them/their instead of he/him/his or she/her/hers. Some nonbinary people consider themselves to be trans or transgender; some do not because they consider transgender to be part of the gender binary. The shorthand NB (pronounced “enby”) is sometimes used as a descriptor for nonbinary people | Goldman et al48 |
| Gender nonconforming | The extent to which a person’s gender identity or gender expression differs from what is typically expected for people assigned to a particular sex or gender at birth | Goldman et al48 |
| Two-Spirit | An English-language term adopted by North American indigenous peoples to communicate a broad range of identities used in indigenous communities. Each indigenous language has its own specific terms and nuanced cultural meanings. Two-Spirit can encompass any kind of gender identity or sexual orientation other than cisgender and heterosexual. Some people identify only as Two-Spirit. Some people identify as Two-Spirit and lesbian, or gay, or bisexual, or trans, or nonbinary. Only indigenous people should call themselves Two-Spirit | Goldman et al48 |
| Genderqueer | One example of nonbinary gender identity | Madsen et al,20 revised |
| Transgender | An umbrella term used to describe people whose gender identities and/or gender expressions are not what is typically expected for the sex and gender to which they were assigned at birth | Goldman et al48 |
| Transition | Procedures that people use to change from living as the gender they were assigned at birth to living as a gender that better matches their gender identity. People may transition only socially by using methods such as changing their name, clothing and accessories, hairstyles, and/or the ways that they move and speak. Prosthetics, hairpieces/wigs, and/or chest binders may also be used. Transitioning may also involve using hormones and/or surgeries to alter a person’s physical body | Goldman et al48 |
| Transfeminine | Anyone who was assigned male at birth and identifies more as a woman than as a man. Transfeminine people may identify as trans women, as nonbinary, as Two-Spirit, or another currently less common identity | Goldman et al48 |
| Transgender women or trans women | Individuals who were assigned male at birth but who have gender identities as women. They may or may not have undergone any transition. MTF or male-to-female is an older term that is falling out of use | Goldman et al48 |
| Transmasculine | Anyone who was assigned female at birth and identifies more as a man than as a woman. Transmasculine people may identify as trans men, as nonbinary, as Two-Spirit, or another currently less common identity | Goldman et al48 |
| Transgender men or trans men | Individuals who were assigned female at birth but who have gender identities as men. They may or may not have undergone any transition. FTM or female-to-male is an older term that is falling out of use | Goldman et al48 |
| Name used | Name that one prefers to be addressed by that may be different from their legal or given name | Gupta et al,27 revised |
| Pronouns | Words used to describe a person that are appropriate for their gender identity | Goldstein et al,25 revised |
| Organ/Anatomic Inventory | An accurate record of what organs a patient may or may not have (Deutsch as cited in23) | Rosendale et al23 |
| Transgender and gender nonconforming (TGNC) | An umbrella term that refers to people whose gender identities/expressions, or the extent of their gender identifies/expressions, are not what is typically expected for the sex and gender to which they were assigned at birth | Burgess et al,8 revised |
| Sexual and gender minority (SGM) | An umbrella term that encompasses a diverse array of sexual orientations and gender identities, including lesbian, gay, bisexual, and transgender (LGBT) as well as queer/questioning, intersex, and others | Cathcart-Rake et al39 |
| Sexual orientation/Identity | The desire to have sexual relations with someone of the same or different gender identity and/or anatomical sex | Goldstein et al25 |
| LGBTQ/ LGBTQI/ LGBTQIA2+ | Terms referring broadly to the people who identify as lesbian, gay, bisexual, transgender, queer, intersex, asexual, Two-Spirit and other sexual and gender identities that are not cisgender or heterosexual | Madsen et al,20 revised |
Inclusive and affirming environment
There is a current need to create a welcoming and respectful health care environment that supports all patients. Achieving this requires the adoption of explicit gender-affirming language and policies that encourage inclusion and recognition of civil rights that prohibit sex- and gender-based discrimination. Gender-affirming policies include adhering to standards of care for individuals who are transitioning,18 acknowledging patients by their chosen/affirmed names and pronouns,19,22 and ensuring safe access to washroom facilities in accordance with one’s gender identity.23 Civil rights protections range from access to health care services and completion of birth certificate to requests for partner’s medical information by SGM individuals, partners/spouses, and parents.18
Culturally competent health care staff
An inclusive environment also means having staff that acknowledge diversity and practice culturally competent care for SGM. Health care staff ought to be familiar with SGM terminology, knowledgeable in the unique health needs/challenges of SGM, and be respectful and inclusive in verbal and written communications.18 To achieve cultural competency, regular mandatory institution-wide training programs are needed for all health care staff21 and in formal education curricula for prelicensed health professionals.8,19,23,26 The LGBT advisory council of the Human Rights Campaign promotes cultural competency among health care staff by issuing a Healthcare Equality Index designation to employees who have completed cultural competency training on LGBT issues.21 The patient safety education work group of another organization (Veterans Health Administration) developed training workshops for staff on appropriate ways to collect SOGI data.8
Standardized data collection
Policies and procedures providing direction on what GSSO data should be collected, who should collect the data, when and where they should be collected, and under what circumstances they should be accessed and used are currently inconsistent.18,22–24 Supporting one’s privacy is an essential element to patient trust and to cultivating safe care environments. A survey that involved 144 breast imaging facilities revealed that many do not have explicit policies to consistently document patients’ GI, pronouns, and preferred names; and over half of their intake forms do not ask patients for their GI.24 The need for this information is clear: It can help reduce disparities by improving access to care, guide health risk monitoring and preventive care screening, improve patient-provider communications, and support secondary uses, such as research on policy and health impact.2 Strategies to collect GSSO data include having a standardized data collection process, preferred name and pronouns,18,22 the use of 2-step questions for collecting GI and birth sex,2 and training clinical and nonclinical staff to ask appropriate questions and explain the reasons for collecting this information and its implications.18,22
Identifying and matching SGM patients with unique care needs
Patient identification policies
Existing policies on identifying patients at time of registration and services, such as blood draw, are often based on legal name and appearance matched against recorded sex/gender or on identification labels, such as wristbands.25 For instance, 1 academic health center reported existing policies only allow the use of legal name in blood transfusion and billing.29 Yet a patient’s legal name and/or appearance may not always match the name that a patient uses or one’s lived gender. Although some jurisdictions allow people to change their gender on legal documents, such as driver’s licences, this change may not extend to their health record.29
Sex- and sexuality-based care guidelines
Many clinical and administrative guidelines are based on biological sex that often default to sex assigned at birth and recorded in one’s EHR. This can be an issue when patients update their recorded sex assigned at birth to reflect their current gender.8,27,29Sex-based clinical guidelines for breast cancer screening and pregnancy tests may not account for individuals who identify as trans men.25,27 Administrative billing guidelines for sex-based diagnostic tests may include prostate ultrasound exams that can be denied for reimbursements for trans women.29 There are eligibility guidelines for blood donors, such as sex-specific height and weight criteria in double red blood cell donation, and 12-month blood donation deferral based on recent sexual behaviors of males who have had sex with other males (MSM) or females who have had sex with MSM.29 Although health maintenance guidelines exist for transgender and gender nonbinary patients, it is unclear how widely these recommendations are used in practice.29 The inclusion of an anatomic/organ inventory can improve care and safety of transgender patients to enhance clinical decision-making based on sex-based care guidelines, by neutralizing clinical assumptions about the organs a person has at a given point in time.23
Care of transitioning patients
For patients undergoing gender-affirming surgeries and/or hormonal therapies, monitoring of their progress and health status can be problematic. Laboratory parameters with sex-specific reference ranges such as creatinine, hematocrit, and liver enzyme levels for these patients can be different from expected reference ranges for typical males and females.25,27 The assessment of Pap smears and prostate and breast biopsies from these patients are prone to misinterpretations as their specimens can be impacted by exogenous hormonal therapies.27 Dosage monitoring in transgender patients on hormonal medications need to consider their effect on overall physiology such as renal clearance and lean body mass, which can vary depending on the duration of such therapies.26,28 To improve safety and care, more research is needed to better understand the relationships between various physiologic variables and patients undergoing transition.23,27
Patient and provider perspectives and relationships
Patient perceptions and concerns
While SGM patients appreciate improved staff competencies and GI questions, many report negative experiences and express concerns with involuntary disclosure, privacy violations, access to care, discrimination, and personal safety.31,33,34 Transgender patients have described situations where sensitive gender information has been involuntarily disclosed, misinterpreted or abused, and their safety and care has been compromised.31 SGM patients may avoid emergency care for fear of discrimination, length of wait, and previous negative experiences.34 Although transgender patients will often self-disclose their GI at some point during their health care encounters, they feel it would be helpful for staff to ask them directly during intake.33 Mistakes with deadnaming (addressing a transgender person by the name given at birth and no longer used upon transitioning) and misgendering (using the wrong pronouns or other gender-specific words when referring to or speaking to someone, especially a transgender person) by health care providers are often upsetting for patients, but provider sensitivity in acknowledging mistakes can help ease the distress.33
Provider perceptions and competencies
Health care providers revealed varying approaches and comfort levels in collecting and documenting GSSO data.32,45 Some feel discomfort and lack of confidence in collecting GI data in the absence of protocols and specific EHR data fields.32 Others noted that they do not routinely inquire about patients’ GI, expect SGM patients to self-disclose their identity, or presume the patient’s GI through mention of gender-affirming treatments.32 Others still are worried that clinical GI questions could offend both cisgender and transgender patients.32 Communication practices between staff about patients’ GI are inconsistent and sometimes done through sticky notes as reminders of a patient’s chosen name, through diagnostic codes to alert others, or through free-text entries in the social history section of the EHR.32
Need for improved interactions
SGM patients have expressed the need for a broader range of gender and birth-assigned sex identifiers and feel they should not have to divulge birth-assigned sex unless needed.30 Health care providers have expressed the need for explicit guidelines and training on when, where, and how to collect and document GSSO data as part of the encounter.32 Both patients and providers believed having an inclusive environment and being respectful during intake and encounter are important.33 Both wanted pronouns, name that the patient uses, and gender identifier in forward-facing displays to improve communication. However, better explanations and safeguard mechanisms are needed for the collection of GI data, as patients and providers have differing opinions on who should collect such data and when they should be collected.30,31
Techno-socio-organizational aspects of EHRs
Technical design
With self-reported SOGI data mandated in the United States as part of stage-3 meaningful use in 2015, vendors have started to include GSSO as distinct data fields in their EHRs.5 Some health organizations have also incorporated preferred/chosen/affirmed name and pronouns as part of the EHR documentation.5 One offers the option of having providers enter GSSO data directly into the EHR after talking with the patient, or allowing patients to complete the questionnaire on their own through an online EHR portal.35 There have been calls to establish an organ inventory to improve clinical decision-making for transgender patients but no EHR examples were found in the included articles.5,8,18 To protect the confidential nature of GSSO data, there were suggestions to treat it as a specific class of information not to be communicated to another provider without the patient’s permission, and the use of mosaic blur to make patient information unreadable to individuals who do not have the need to access certain information.2
Organization and people
Equally important are the socio-organizational aspects that contribute to successful EHR adoption. These include ensuring an inclusive organizational culture that acknowledges diversity, adopts applicable nondiscrimination, privacy, and confidentiality protection mechanisms, trains health care staff on how to collect and use GSSO data, and engages the SGM communities on the importance of collecting these data in EHRs.5 It also includes addressing workflow and work culture issues that can vary across settings.7 For example, 1 organization focused their efforts on developing key messages of how providers could help reduce health disparities if they knew which of their patients were LGBT, involving senior executives and community leaders, providing educational outreach to staff, having different GSSO data entry options for providers and patients, and leveraging the effort to increase patient and community engagement.35
Planning and implementation
Successful examples of GSSO data collection in EHRs included Fenway Health7 and Veterans Affairs.8 Fenway described their process as having: (a) a dedicated team of staff champions, (b) standardized data collection methods, (c) a customized EHR, (d) staff training, (e) patient education on GSSO including how data would be protected, (f) a welcoming environment, (g) pilot data collection with quality improvement to improve the process, and (h) ways to use GSSO data to identify disparities in access, screening, and health outcomes. Veterans Affairs addressed patient safety issues with self-identified GI (SIGI) as some clients had changed their birth sex in the EHR to match with current gender, which created inconsistencies with sex-based EHR rules for health screenings and preventive care. With the implementation of SIGI data fields in their EHR underway, Veterans Affairs (a) created a patient safety education workgroup to disentangle birth sex and SIGI in the EHR, (b) developed SIGI fact sheets with information for patients and staff on the differences between birth sex and SIGI fields, and how they would be used in the EHR, and (c) provided staff training on how to ask and respond to SIGI questions and how to update them.
Addressing needs and directions
Limited data
Thus far, research on GSSO documentation in EHRs covered the use of text-mining to identify SGM, effects of GSSO and sexual partner documentation, correlation of SGM with specific disparities, as well as patient and provider perspectives. For GSSO documentation, the 2-step question had led to increased identification of transgender and gender-nonbinary patients,36,38 but the practice varied across settings.10,37,39,40 For identifying SGM, text-mining algorithms with different combinations of keywords, diagnostic, and billing codes were applied to clinical notes as ways to identify SGM and build lexicons of SGM terms with varying degrees of success.41–44 One organization had missing SOGI data for 77.1% and 62.8% of patients when introduced in the first year,10 while another found their documentation of sexual partner gender at 45%.37 Two studies used survey data in EHRs to examine the correlation of SO with human immunodeficiency virus risk assessment45 and intimate partner violence.46 As explained earlier, patients and providers offered varying perspectives on the collection of this information.30–34
Standardized data for research and evaluation
Reisner et al47 reported existing SGM research suffered from inconsistent use of SGM definitions, lack of prospective observational studies and interventional trials, and limited data on risks and benefits of gender affirmation. The focus was mostly on mental health, substance use and abuse, and sexual health issues, with insufficient attention to evaluating systemic or structural barriers in health care access and utilization and complications from transition treatments. Reisner et al described 4 sampling approaches to SGM research that are general population-, health systems-, clinic-, and venue-based. As seen in our review, the latter 3 approaches are particularly relevant to the study of GSSO documentation in EHRs. The primary studies in our review employed a wide range of research methods and designs. They covered pre-post and retrospective observational studies, cross-sectional surveys, text-mining,41–44 qualitative and mixed methods with interviews, focus groups and surveys, and secondary analysis of EHR records and manual chart reviews.10,36–40
Future needs and directions
Future research should include garnering insights from health organizations based on their experiences with GSSO data collection and use to monitor health and reduce disparities of SGM.7,23 To be inclusive of all gender identities and sexual orientations and behaviors, the SGM terminology must evolve over time, and, when needed,2,20 and it would be beneficial to include revision dates to monitor trends.17 Health organizations should implement and evaluate actions that can improve the experiences of SGM and cultural competencies of health care providers.23 These efforts can help expand our knowledge base of best practice evidence for SGM.23
The 5 themes and review findings are summarized in Table 2.
Table 2.
Summary of the 5 themes and review findings
| Themes | Findings |
|---|---|
| Inclusive environment, precise terminology, and standardized data collection |
|
| Identifying and matching SGM patients with unique care needs |
|
| Patient and provider perspectives and relationships |
|
| Techno-socio-organizational aspects of EHRs |
|
| Addressing needs and directions |
|
DISCUSSION
Contributions and implications
This review contributes to the SGM literature in several ways. First, the incorporation of GSSO data into EHRs is not just a technical endeavor but a journey that involves the complex interplay of various techno-socio-organizational dynamics. Others have emphasized on this aspect, such as the best practice guidelines for collecting GSSO data by Fenway49 and gender diversity guidance for laboratory services by the Institute for Quality Management in Healthcare.50 Second, the 5 themes provide a snapshot of the current state of knowledge in modernizing GSSO documentation in EHRs for SGM. These findings are consistent with those in literature. Examples include current end user EHR practices in GI data collection by Deutsch et al,11 barriers to quality health care for the transgender population by Roberts and Fantz,1 patient and provider perspectives on the risks and benefits of collecting GSSO data by Maragh-Bass et al,51 and the need for uniform GSSO standards in EHRs by Moscoe.52
Third, the proposed SGM terminology can promote shared understanding of the evolving SGM concepts, terms, and definitions. The importance of precise terminology is emphasized by Pedersen53 as a way to improve communication with the gender diverse community in diagnostic imaging departments. It is also reflected in the review by Collin on the prevalence of transgender populations based on how it is defined,54 the need for accurate data to estimate the size of the transgender and gender diverse populations by Zhang et al,55 and familiarity with the SGM terminology to ensure safe and appropriate care by Safer and Tangpricha.56 Fourth, the EHR-related efforts and strategies described in this review can guide future EHR planning and implementation to advance the inclusion and health of SGM. The efforts by Callahan et al,35 Burgess et al,8 and Grasso et al7 to incorporate GSSO data into their organizations are exemplary cases for others to follow and addressed the call by Nguyen and Lau57 to standardize GSSO documentation in EHRs. Collectively, these examples can help build the knowledge base on EHR adoption efforts and their impact on the inclusion and health of SGM.
Limitations
This rapid review has limitations. The review covered only peer-reviewed English articles in MEDLINE from the last 5 years. It was possible relevant studies in other languages or databases were missed. The 5-year limit was for expediency, so important studies from earlier periods would have been omitted. The synthesis and derived themes were subjective and could be biased. The review collated a large number of articles and findings, which made it difficult to include exhaustive detail on all reported efforts and issues. Most included articles were from western countries, so other cultures were not represented, such as Two-Spirit and Hijra from Indigenous and South Asian communities. Efforts were made to overcome these limitations. They included independent article selection and extraction by multiple researchers and stakeholder feedback to reduce bias, as well as articles from earlier periods to compare and validate the findings and build on previous work.
CONCLUSION
This rapid review showed that the literature on GSSO documentation in EHRs is growing. While this trend is encouraging, there are still knowledge gaps and practical challenges, such as organizational commitments to ensure affirming, culturally competent environments that enable meaningful changes as well as coordinated efforts to address the technical design, organizational and social, and planning and implementation aspects of modernizing GSSO documentation. The adoption of an inclusive EHR is a journey as we continue to learn about and address the health needs and outcomes of SGM.
GLOSSARY OF TERMS
CIHR- Canadian Institutes of Health Research
EHRs- electronic health records
GI- gender identity
GSSO- gender, sex, and sexual orientation
LBGT- lesbian, gay, bisexual, transgender
LGBTQ- lesbian, gay, bisexual, transgender, queer
LGBTQI- lesbian, gay, bisexual, transgender, queer, intersex
LGBTQIA2+ lesbian, gay, bisexual, transgender, queer, intersex, asexual, two-spirit, and other sexual and gender identities
MEDLINE- Medical Literature Analysis and Retrieval System Online, or MEDLARS Online
MSM- males who have sex with males
PRIDE- Personal Rights In Defense and Education. (RQ Note: Sometimes PRIDE is used an acronym and sometimes not. Many organizations use it without knowing that it was originally created as an acronym)
SGM- sexual and gender minorities
SIGI- self-identified GI
SO- sexual orientation
SOGI- sexual orientation and gender identity
TGNC- transgender and gender nonconforming
FUNDING
This study was funded by the Canadian Institutes for Health Research (CIHR) Institute for Gender and Health, 2019-09-27 Planning and Dissemination Grant–Institute Community Support.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting or revising the presented work, gave approval of the submitted manuscript, and agreed to be accountable for ensuring the integrity of the manuscript. FL and MA drafted the manuscript, and all co-authors reviewed and revised it. FL, MA, KD, and RQ extracted the data, prepared the tables, and validated the outputs. MA created the initial coding schemes, FL revised them, and KD and RW further refined them. AD created and FL refined the terminology table.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
We are indebted to members of the Infoway Sex and Gender Working Group members and stakeholder organizations and groups who have generously volunteered their time to contribute to this important work. Individuals who have provided feedback on draft versions of this paper include Zander Keig, Andrea MacLean, Erin Pichora, Finnie Flores, Janine Kaye, Sanya Palli, and Shannon O’Connor.
CONFLICT OF INTERESTS STATEMENT
None declared.
REFERENCES
- 1. Roberts TK, Fantz CR. Barriers to quality health care for the transgender population. Clin Biochem 2014; 47 (10–11): 983–7. [DOI] [PubMed] [Google Scholar]
- 2. Bosse JD, Leblanc RG, Jackman K, Bjarnadottir RI. Benefits of implementing and improving collection of sexual orientation and gender identity data in electronic health records. Comput Inform Nurs 2018; 36 (6): 267–74. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academies Press (US; ); 2011. [PubMed] [Google Scholar]
- 4. Deutsch MB, Green J, Keatley J, et al. Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group. J Am Med Inform Assoc 2013; 20 (4): 700–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cahill SR, Baker K, Madeline MA, Deutsch MB, Keatley J, Makadon HJ. Inclusion of sexual orientation and gender identity in stage 3 meaningful use guidelines: a huge step forward for LGBT health. LGBT Health 2016; 3 (2): 100–2. [DOI] [PubMed] [Google Scholar]
- 6. Woebkengberg J. Capturing Sexual Orientation/Gender Identity Data through HIT. 2018. In: journal.adhima.org. 2019 - [about 2 screens]. https://journal.ahima.org/capturing-sexual-orientation-gender-identity-data-through-hit/ Accessed May 27, 2020
- 7. Grasso C, McDowell MJ, Goldhammer H, Keuroghlian AS. Planning and implementing sexual orientation and gender identity data collection in electronic health records. J Am Med Inform Assoc 2019; 26 (1): 66–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Burgess C, Kauth MR, Klemt C, Shanawani H, Shipherd JC. Evolving sex and gender in electronic health records. Fed Pract 2019; 36 (6): 271–7. [PMC free article] [PubMed] [Google Scholar]
- 9. Lunn MR, Lubensky M, Hunt C, et al. A digital health research platform for community engagement, recruitment and retention of sexual and gender minority adults in a national longitudinal cohort study—the PRIDE Study. J Am Med Inform Assoc 2019; 26 (8–9): 737–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Grasso C, Goldhammer H, Funk D, et al. Required sexual orientation and gender identity reporting by US health centers: first-year data. Am J Public Health 2019; 109 (8): 1111–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Deutsch MB, Keatley J, Sevelius J, Shade SB. Collection of gender identity data using electronic medical records: survey of current end-user practices. J Assoc Nurses AIDS Care 2014; 25 (6): 657–63. [DOI] [PubMed] [Google Scholar]
- 12. Deutsch MB, Buchholz D. Electronic health records and transgender patients—practical recommendations for the collection of gender identity data. J Gen Intern Med 2015; 30 (6): 843–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.HL7. The Gender Harmony Project. 2019. https://confluence.hl7.org/display/VOC/The+Gender+Harmony+Project Accessed May 27, 2020
- 14. Haby MM, Chapman E, Clark R, Barreto J, Reveiz L, Lavis JN. What are the best methodologies for rapid reviews of the research evidence for evidence-informed decision making in health policy and practice: a rapid review. Health Res Policy Sys 2016; 14 (1): 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kaltenthaler E, Cooper K, Pandor A, Martyn-St. James M, Chatters R, Wong R. The use of rapid review methods in health technology assessments: 3 case studies. BMC Med Res Methodol 2016; 16 (1): 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kelly SE, Moher D, Clifford TJ. Quality of conduct and reporting in rapid reviews: an exploration of compliance with PRISMA and AMSTAR guidelines. Syst Rev 2016; 5 (1): 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tricco A, Antony J, Zarin W, et al. A scoping review of rapid review methods. BMC Med 2015; 13 (1): 224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Canada Health Infoway. Sex and Gender Working Group. https://infocentral.infoway-inforoute.ca/en/collaboration/wg/sex-gender Accessed May 27, 2020
- 19.AHIMA Work Group. Improved patient engagement for LGBT populations: Addressing factors related to sexual orientation/gender identity for effective health information management. Journal of AHIMA 2017; 88 (3): 34–9. [PubMed] [Google Scholar]
- 20. Madsen TE, Bourjeily G, Hasnain M, et al. Sex- and gender-based medicine: the need for precise terminology. Gender and the Genome 2017; 1 (3): 122–8. [Google Scholar]
- 21. Rosa W, Fullerton C, Keller R. Equality in healthcare: the formation and ongoing legacy of an LBGT advisory council. LGBT Health 2015; 2 (4): 292–6. [DOI] [PubMed] [Google Scholar]
- 22. Donald C, Ehrenfeld JM. The opportunity for medical systems to reduce health disparities among lesbian, gay, bisexual, transgender, and intersex patients. J Med Syst 2015; 39 (11): 178. [DOI] [PubMed] [Google Scholar]
- 23. Rosendale N, Goldman S, Ortiz G, Haber LA. Acute clinical care for transgender patients: a review. JAMA Intern Med 2018; 178 (11): 1535–43. [DOI] [PubMed] [Google Scholar]
- 24. Goldberg JE, Moy L, Rosenkrantz A. Assessing transgender patient care and gender inclusivity of breast imaging facilities across the United States. J Am Coll Radiol 2018; 15 (8): 1164–72. [DOI] [PubMed] [Google Scholar]
- 25. Goldstein Z, Corneil TA, Greene DN. When gender identity doesn’t equal sex recorded at birth: the role of the laboratory in providing effective healthcare to the transgender community. Clin Chem 2017; 63 (8): 1342–52. [DOI] [PubMed] [Google Scholar]
- 26. Bishop BM. Pharmacotherapy considerations in the management of transgender patients: a brief review. Pharmacotherapy 2015; 35 (12): 1130–9. [DOI] [PubMed] [Google Scholar]
- 27. Gupta S, Imborek KL, Krasowski MD. Challenges in transgender healthcare: the pathology perspective. Lab Med 2016; 47 (3): 180–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Webb AJ, McManus D, Rouse GE, Vonderheyde R, Topal JE. Implications for medication dosing for transgender patients: a review of the literature and recommendations for pharmacists. Am J Health Syst Pharm 2020; 77 (6): 427–33. [DOI] [PubMed] [Google Scholar]
- 29. Imborek KL, Nisly NL, Hesseltine MJ, et al. Preferred names, preferred pronouns and gender identity in the electronic medical record and laboratory information systems: is pathology ready? J Pathol Inform 2017; 8: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Dunne MJ, Raynor LA, Cottrell EK, Pinnock W. Interviews with patients and providers on transgender and gender nonconforming health data collection in the electronic health record. Transgend Health 2017; 2 (1): 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Thompson HM. Patient perspectives on gender identity data collection in electronic health records: an analysis of disclosure, privacy and access to care. Transgend Health 2016; 1 (1): 205–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nadler LE, Ogden SN, Scheffey KL, Cronholm PF, Dichter ME. Provider practices and perspectives regarding collection and documentation of gender identity. J Homosex 2019: 1–13. doi: 10.1080/00918369.2019.1667162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Acosta W, Qayyum Z, Turban JL, van Schalkwyk G. Identify, engage, understand: supporting transgender youth in an inpatient psychiatric hospital. Psychiatr Q 2019; 90 (3): 601–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Samuels EA, Tape C, Garber N, Bowman S, Choo EK. “Sometimes you feel like the freak show”: a qualitative assessment of emergency care experiences among transgender and gender-nonconforming patients. Ann Emerg Med 2018; 71 (2): 170–82. [DOI] [PubMed] [Google Scholar]
- 35. Callahan EJ, Sitkin N, Ton H, Eidson-Ton WS, Weckstein J, Latimore D. Introducing sexual orientation and gender identity into the electronic health record: one academic health center’s experience. Acad Med 2015; 90 (2): 154–60. [DOI] [PubMed] [Google Scholar]
- 36. Tordoff DM, Morgan J, Dombrowski JC, Golden MR, Barbee LA. Increased ascertainment of transgender and non-binary patients using a 2-step versus 1-step gender identity intake question in an STD clinical setting. Sex Transm Dis 2019; 46 (4): 254–9. [DOI] [PubMed] [Google Scholar]
- 37. Nguyen GT, Yehia BR. Documentation of sexual partner gender is low in electronic health records: observations, predictors, and recommendations to improve population health management in primary care. Popul Health Manag 2015; 18 (3): 217–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Vance SR Jr, Mesheriakova VV. Documentation of gender identity in an adolescent and young adult clinic. J Adolesc Health 2017; 60 (3): 350–2. [DOI] [PubMed] [Google Scholar]
- 39. Cathcart-Rake EJ, Zemla T, Jatoi A, et al. Acquisition of sexual orientation and gender identity data among NCI community oncology research program practice groups. Cancer 2019; 125 (8): 1313–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Guss CE, Inwards-Breland DI, Ozer E, Vance SR Jr. Experiences with querying gender identity across seven adolescent medicine sites. J Adolesc Health 2018; 63 (4): 506–8. [DOI] [PubMed] [Google Scholar]
- 41. Bjarnadottir RI, Bockting Q, Yoon S, Dowding DW. Nurse documentation of sexual orientation and gender identity in home healthcare. Comput Inform Nurs 2019; 37 (4): 213–21. [DOI] [PubMed] [Google Scholar]
- 42. Ehrenfeld JM, Gottlieb KG, Beach LB, Monahan SE, Fabbri D. Development of a natural language processing algorithm to identify and evaluate transgender patients in electronic health record systems. Ethn Dis 2019; 29(Suppl 2): 441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Roblin D, Barzilay J, Tolsma D, et al. A novel method for estimating transgender status using electronic medical records. Ann Epidemiol 2016; 26 (3): 198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Blosnich JR, Cashy J, Gordon AJ, et al. Using clinician text notes in electronic medical record data to validate transgender-related diagnosis codes. J Am Med Inform Assoc 2018; 25 (7): 905–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Joore IK, Geerlings SE, Brinkman K, van Bergen J, Prins JM. The importance of registration of sexual orientation and recognition of indicator conditions for an adequate HIV risk-assessment. BMC Infect Dis 2017; 17 (1): 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Valentine SE, Peitzmeier SM, King DS, et al. Disparities in exposure to intimate partner violence among transgender/gender nonconforming and sexual minority primary care patients. LGBT Health 2017; 4 (4): 260–7. [DOI] [PubMed] [Google Scholar]
- 47. Reisner SL, Deutsch MB, Bhasin S, et al. Advancing methods for US transgender health research. Curr Opin Endocrinol Diabetes Obes 2016; 23 (2): 198–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Goldman M, Butler-Foster T, Lapierre D, O’Brien SF, Devor A. Trans people and blood donation. Transfusion 2020; 60 (5): 1084–92. [DOI] [PubMed] [Google Scholar]
- 49.Fenway Institute. Ready, Set, Go! Guidelines and Tips for Collecting Patient Data on Sexual Orientation and Gender Identity. Boston: National LGBT Health Education Centre; 2018. https://www.lgbthealtheducation.org/publication/ready-set-go-guidelines-tips-collecting-patient-data-sexual-orientation-gender-identity/ Accessed May 27, 2020 [Google Scholar]
- 50.Institute for Quality Management in Healthcare. Care Considerations for Inclusion of Gender Diversity within Medical Laboratory Services. Toronto: Centre for Education; 2019. https://iqmh.org/Portals/0/Docs/Resources/Education/White%20Paper%20-%20Care%20Considerations%20for%20Inclusion%20of%20Gender%20Diversity%20Within%20Medical%20Laboratory%20Services.pdf Accessed May 27, 2020 [Google Scholar]
- 51. Maragh-Bass AC, Torain M, Adler R, et al. Risks, benefits, and importance of collecting sexual orientation and gender identity data in healthcare settings: a multi-method analysis of patient and provider perspectives. LGBT Health 2017; 4 (2): 141–52. [DOI] [PubMed] [Google Scholar]
- 52. Moscoe GB. Beyond the Binary: A Proposal for Uniform Standards for Gender Identity and More Descriptive Sex Classifications in Electronic Medical Records [thesis on the Internet]. Portland, OR: Oregon Health & Science University; 2014. 10.6083/M4HQ3XNJ Accessed May 27, 2020 [DOI] [Google Scholar]
- 53. Pedersen V. Improving communication with the gender diverse community diagnostic imaging departments. Radiography 2018; 24(Suppl 1):S3–6. [DOI] [PubMed] [Google Scholar]
- 54. Collin L, Reisner SL, Tangpricha V, Goodman M. Prevalence of transgender depends on the case definitions: a systematic review. J Sex Med 2016; 13 (4): 613–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Zhang Q, Goodman M, Adams N, et al. Epidemiological considerations in transgender health: a systematic review with focus on higher quality data. International Journal of Transgenderism 2020; 21 (2): 125–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Safer JD, Tangpricha V. Care of the transgender patient. Ann Intern Med 2019; 171 (10): 775. [DOI] [PubMed] [Google Scholar]
- 57. Nguyen A, Lau BD. Collecting sexual orientation and gender identity information: filling the gaps in sexual and gender minority health. Med Care 2018; 56 (3): 205–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.